Abstract
Accurate measurement of cytokine concentrations is a powerful and essential approach to the study of inflammation. The enzyme-linked immunosorbent assay (ELISA) is a simple, low-cost analytical tool that provides both the specificity and sensitivity required for the study of cytokines in vitro or in vivo. This communication describes a systematic approach to develop an indirect sandwich ELISA to detect and quantify cytokines, or other biomarkers, with accuracy and precision. Also detailed is the use of sequential ELISA assays to analyze multiple cytokines from samples with limited volumes. Finally, the concept of a multiplex ELISA is discussed with considerations given to cost and additional time required for development.
Keywords: Cytokines, Sandwich ELISA, Sequential ELISA, Multiplex ELISA, Antibodies
1. Introduction
Cytokines are a cornerstone of any study that deals with inflammation, whether it is an in vitro cell culture system or an in vivo animal model (1). The cytokine profile as a whole and the relative abundance of one cytokine, and the endogenous inhibitors, define an inflammatory process that is in motion (2). Cytokines may be used to describe the nature of the insult, infection, or injury (3), and may even be used to stage the disease process (4). These studies revolve around the ability to detect, quantify, and discriminate a single cytokine from a multitude of biomolecules present in any given sample. One such method that is routinely used is the indirect sandwich enzyme-linked immunosorbent assay (ELISA).
The ELISA exploits the specificity of antibodies (Abs) and uses them to capture and quantify an analyte of interest from a given volume of sample, and it does this with remarkable sensitivity (pg/mL or ~0.5 pM for a 15 kDa protein) (5).
There are four basic steps involved in an indirect sandwich ELISA. (1) Capturing analyte from sample with capture antibody. (2) Detecting captured analyte with detection antibody (also specific for captured analyte) that is labeled with biotin. (3) Detection amplification with streptavidin that has been conjugated with an enzyme, in most instances horseradish peroxidase (HRP). Each streptavidin molecule has multiple HRP molecules attached, and each detection antibody has multiple biotins attached. Alternatively, detection antibodies may be directly conjugated to HRP, thereby eliminating an incubation step, but at the cost of sensitivity. (4) Substrate addition and signal measurement via optical density (OD) with a microplate reader.
After each incubation step throughout the assay, unbound reactants are washed away. Also, due to the binding properties of the microplates used, the plates must be blocked with an inert protein, after coating with capture antibody, in order to prevent non-specific binding (NSB) of the sample.
This simple method can be expanded to measure several analytes from a single aliquot of sample via the sequential ELISA (6). In this instance, a single sample is removed from one ELISA plate and then incubated in a separate plate, since the first plate should have only captured the cytokine detected by the antibody used for capturing the cytokine. An alternative to the sequential ELISA is the multiplex ELISA, which offers a more rapid and cost-effective alternative to sequential analysis. In this approach, multiple capture antibodies, with differing specificities, are printed into a single well in a microplate. Each printed “spot” of antibody is exclusive from the others (see Subheading 3.5, Fig. 4). In this manner, it is possible to measure 17, or more, analytes from a single sample all at once.
Fig. 4.
Example array of “Printed Capture Antibodies for the Multiplex ELISA”.
This chapter details the steps involved in developing an ELISA by way of checkerboard titrations of antibodies, as well as selecting the optimal blocking buffer and diluent via dose–response curve analysis. Also discussed is the use of a spike-recovery method to determine if cross-reactivity or loss of analyte exists between the separate ELISAs used in the sequential ELISA format. Finally, the multiplex ELISA is given consideration in terms of the principle, determination of cross-reactivity, and cost efficiency compared to the standard ELISA.
2. Materials and Equipment
2.1. Standard and Sequential ELISA
Matched antibody pairs: Monoclonal for capture and either mono- or polyclonal biotinylated antibody for detection.
Recombinant proteins for cytokine standards.
- Blocking buffers: There are several different blocking buffers. Trial and error must be used to determine the optimal buffer.
- 2% (w/v) Bovine Serum Albumin (BSA) (Sigma Chemical Company, St Louis, MO) in 1× phosphate-buffered saline (PBS; 120 mM sodium chloride, 1.2 mM sodium phosphate monobasic, 2.8 mM potassium chloride, 8.8 mM sodium phosphate dibasic, pH 7.4).
- Blocker™ Blotto in TBS (Pierce, Rockford, IL).
- Blocker™ Casein in PBS (Pierce).
- Superblock® Blocking Buffer in PBS (Pierce).
- Dilution buffer.
- 10% blocking buffer, 0.1% BSA, and 0.005% Tween-20 in 1× PBS.
- Standard dilution buffer: 1× PBS, 0.005% Tween-20 (Pierce), and 2% (v/v) fetal calf serum (FCS).
Wash buffer: 1× PBS with 0.05% Tween-20, pH7.4.
Streptavidin-conjugated HRP (SA–HRP) diluted 1:20,000 in 1× PBS, 0.1% BSA, and 0.005% Tween-20.
Substrate: 1% 3, 3′,5,5′-tetramethylbenzidine (TMB) dissolved in DiMethyl Sulfoxide (DMSO), diluted 1:100 in 0.1 M sodium acetate (pH 6.0) and 0.005% hydrogen peroxide (H2O2). Do not add in the H2O2 until just prior to the use of the substrate. It is suggested to freeze aliquots of TMB. WARNING: TMB is a known carcinogen.
1.5 N sulfuric acid.
96-well Microtiter plates: High binding capacity (Nunc Immunoplate, Neptune, NJ) (see Note 1).
96-well deep-well polypropylene for storage of diluted samples (source plate).
96-well microtiter plates, nonbinding, for making of standards.
Multichannel pipette and single-channel pipettes.
Automatic plate washer.
MicroPlate optical density scanner that can read between 450 and 600 nm.
2.2. Multiplex Materials and Equipment
All materials listed in 2.1 are required, except for the following: 1.5 N sulfuric acid, MicroPlate reader, substrate (TMB), SA–HRP, all dilution and blocking buffers listed.
Blocking buffer: May be specific for the imaging system used for analysis. This analysis uses the Odyssey blocking buffer from Li-Cor.
Dilution buffer: 1:2 dilution of the Odyssey blocking buffer with 1× PBS, pH 7.4.
Streptavidin-conjugated infrared (IR) dye: This is applicable for the Li-Cor scanning system, see below, but may be applicable to other systems as well.
Microarray printer: This is used to “print” capture antibody onto the bottom of the well of the microplate. This communication is based on our experience with a noncontact spotter, the Perkin Elmer Piezorray.
Detection/imaging system: A system with high resolution is needed to resolve and detect the signal from the individual prints (150 nm diameter) in each well. We use a Li-Cor scanner which can also be used for other assays. This detects the infrared fluorescence of each spotted cytokine which can then be quantified using various software packages.
Automatic plate washer: An automatic plate washer is especially important for this multiplex assay. If manually washing, any contact of pipette tips to the spots in the well could result in a failed assay or even false-positive or -negative results.
3. Methods
3.1. Optimizing Antibody Concentrations (the Checkerboard)
Day #1: Dilute the capture antibodies in a suitable volume of PBS to make four dilutions as shown in Fig. 1 (use the manufacturer’s suggested dilution as a starting point).
Coat a 96-well high-binding microplate with 50 µL/well of the appropriate dilution of capture Ab. Figure 1 shows the layout with the proper dilutions. Tap plate gently to ensure complete coverage of the well bottom. Incubate plate overnight at 4°C.
Day #2: Wash the coated plate with an automatic plate washer (five washes, 250 µL/wash, 15-s soaks between washes, repeat for all wash steps, see Note 2). After the last wash is complete, invert and tap the plate on a paper towel to remove excess liquid. (Once wash buffer is emptied from the plate, it is important to work quickly so that the plate does not dry.)
Add blocking buffer, 150 µL/well, and incubate for 1 h at ambient temperature on an orbital shaker (all subsequent incubations are at ambient temperature on an orbital shaker unless noted otherwise).
Using dilution buffer, prepare a suitable volume of high, medium, low, and zero standards, as shown in Fig. 1. (Standard values in Fig. 1 are only examples; however, a three-log range between high and low is usually sufficient.)
After the plate has been blocked, wash and tap the plate.
Add 50 µL/well of each standard to the plate, as depicted in Fig. 1. Incubate for 2 h (see Note 3).
Prepare a suitable volume of three dilutions of biotinylated detection Ab as shown in Fig. 1.
Wash plate, and then add 50 µL/well of biotinylated detection Ab as shown in Fig. 1. Incubate for 2 h.
Prepare a suitable volume of dilute SA–HRP as normal. (If necessary, two dilutions of SA–HRP can be analyzed here as well by adding two different dilutions to alternating rows of the plate; see Note 4.)
Wash plate. Add SA–HRP, 50 µL/well, as shown in Fig. 1. Incubate for 30 min.
Wash plate: Add TMB substrate, 100 µL/well, and incubate in the dark without shaking for 20–30 min. Periodic measurements at 590 nm should be performed to determine when to stop the reaction. The high standards, for each antibody titration, should have an OD590 of at least 0.4–0.5 prior to stopping color development (see Note 5). It is important to protect TMB substrate from light in order to limit nonenzyme-mediated substrate catalysis (see Note 6 for troubleshooting color development).
Stop the reaction with 1.5 N sulfuric acid, 100 µL/well, and tap plate with hand to gently mix the solutions. The solution should turn yellow.
Scan plate with plate reader at 465 and 590 nm and use the delta OD (OD465−OD590) as the OD data point.
To determine the optimal antibody concentrations, compare the signal-to-noise ratio for each antibody pairing by dividing the OD of each standard by the OD of its corresponding zero standard, i.e.: for Fig. 1, divide the average OD of column 2, rows A and B, by the average OD of column 4, rows A and B. The antibody dilution pairs that yield the highest overall ratios for each standard represent the optimal antibody concentrations (see Note 7). It is highly recommended to use a spreadsheet to simplify the calculation process.
Fig. 1.
The checkerboard titration plate map: Capture and detection antibodies are titrated against each other over a three-log range of standard concentrations. All parameters are assayed in duplicate wells.* An additional titration for strep:HRP may be examined by alternating strep:HRP dilutions across rows.
3.2. Determining the Optimal Blocking and Dilution Buffer for the Sample Matrix (the Dose–Response)
Certain sample matrices, such as serum, plasma, or tissue homogenates, may produce high nonspecific background (NSB) levels of interference which may affect the range, precision, and accuracy of the assay. Often, the blocking and dilution buffers used can exacerbate or diminish the level of NSB that a sample or the antibodies used impart on the assay. These effects are important to account for when selecting the blocking/dilution buffer, and the extent to which the sample should be diluted. The actual matrix dilutions to test are also dependent upon the sensitivity of the assay and the prevalence of the analyte in the sample. A dose–response test example is provided in Fig. 2.
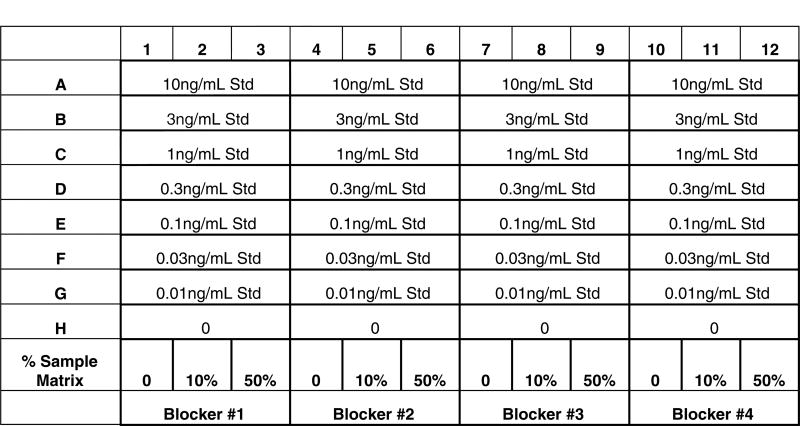
Fig. 2.
Dose–response plate map: Each standard conc., in its respective buffer with or without sample matrix, is loaded into a single well.
The optimal buffer choice is that which yields the least amount of difference in OD between the 0, 10, and 50% sample matrix + standards for the entire range tested. For visual comparison, it may help to plot standard concentrations (x-axis) against ODs (y-axis). A brief procedure is listed below.
Coat a 96-well plate with capture Ab using the optimal concentration determined from the checkerboard (Subheading 3.1) and incubate overnight at 4°C.
Wash plate and divide the plate into 4 three-column sections. Add different blocking buffers (i.e.: Blotto, Casein, Superblock, or Lab Blocking Buffer) to separate sections as shown in Fig. 2. Incubate for 1 h.
Prepare stocks of each dilution buffer at 0, 10, and 50% sample matrix concentrations (v/v). Dilute the recombinant standard with each stock solution prepared and add them to the plate as shown in Fig. 2. Incubate for 2 h.
Prepare the detection Ab in each dilution buffer (without sample matrix!) using the optimal dilution determined in Subheading 3.1. Add to plate as depicted in Fig. 2.
Add SA–HRP, TMB, and sulfuric acid in the appropriate sequence and read as normal.
Again, the optimal buffer system contains the smallest differences between the dilution buffer + standards and the dilution buffer + standards + sample matrix.
3.3. Determining an Analyte’s Concentration in a Given Sample (the Standard ELISA)
All the basic ELISA steps covered in the previous section apply here for analyte quantification. Expounded upon herein are the construction, modeling, and evaluation of a standard curve.
ELISAs have a dose–response curve shape that is sigmoidal; therefore, linear curve fitting models are inappropriate. The fourparameter logistic (4PL) fit is generally acknowledged to be the reference model of choice for ELISAs (7). As the name suggests, the 4PL model calculates on the basis of four parameters:
The lower, minimum asymptote, where the OD from decreasing concentrations of standard approaches that of the zero standard
The slope factor
The inflection point, or IC50, where the concavity of the sigmoidal curve changes
The upper maximum asymptote, where increasing standard concentration results in minimal to no net increase in OD
The 4PL model calculates f(x) = D + ((A−D)/(1 + ((x/C) ^ B))).
There are numerous commercial software packages that perform the calculations. Also, analysis software is usually available from the manufacturer of the plate reader.
Standard curve: An eight-point standard curve, including the blank, is usually sufficient for sample analysis. The high standard concentration, used in the checkerboard stage of development, is a good point from which to start the standard curve. Typically, threefold serial dilutions are made, beginning from the highest standard. All standards, including the blank, are assayed in duplicate.
Curve evaluation: A good curve is symmetrical and sigmoidal in shape with both upper and lower asymptotes (see Note 8), and a top OD within the linear range of the plate reader (see Note 8).
Sample ODs should fall within the steeper area of the curve for the most accurate quantitation. If the sample OD is on or near the top plateau of the curve, the samples should be assayed again, but at a higher dilution in order to place them in the steep portion. If the sample OD is at the lower end of the curve, determine if the sample can be run more concentrated based off the results of the dose–response data generated in Subheading 3.2.
Ultimately, the users should define the range of acceptable accuracy for their curve by preparing standards of known concentrations that differ from those used in the curve, and treating these samples as unknowns. The calculated value should be within 80–120% of the expected value. This process is frequently referred to as “spike and recovery.”
3.4. The Sequential ELISA
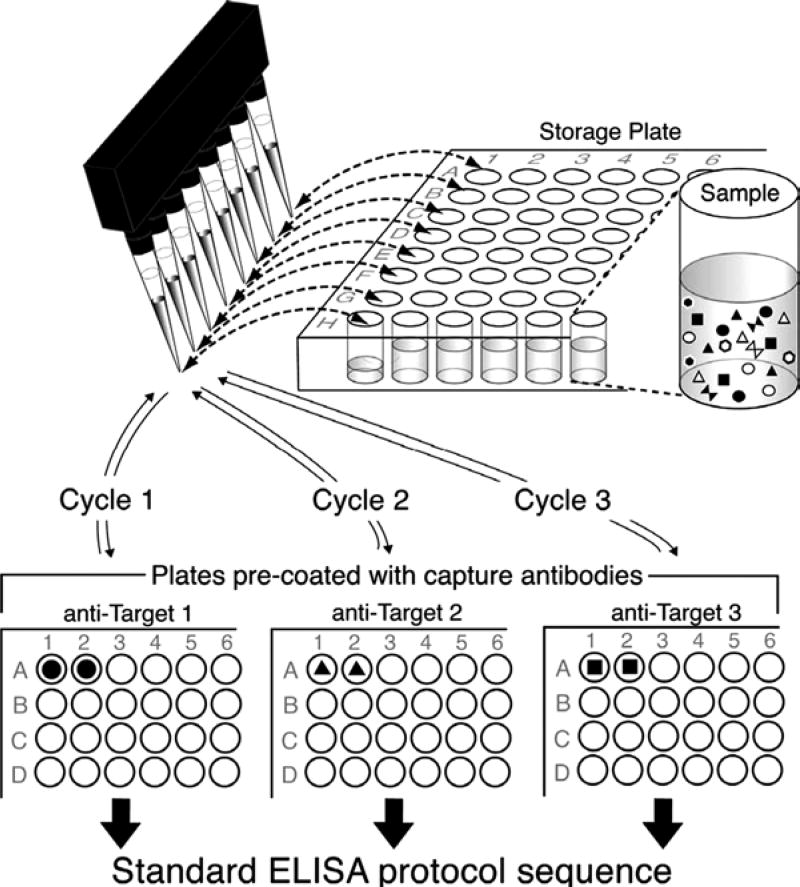
This method uses the same protocol as the standard ELISA; however, the same samples can be run, sequentially, on multiple cytokine ELISA plates. This is particularly useful when the amount of sample available is limited.
A word of caution: Prior to assaying samples, it should be determined if there is cross-reactivity between the different ELISAs. To determine this, perform a spike and recovery, in which a known amount of each protein to be tested is spiked into a normal control sample and tested in the sequential ELISA format. An acceptable recovery range is 80–120%. Furthermore, samples should only be sequentially assayed in the same order as for which the spike–recovery performance was determined.
Coat the various cytokine ELISA plates as normal.
Wash only one plate, block, and add standard and samples as normal.
During the second hour of sample/standard incubation for the first plate, wash and block the second plate.
Before washing the first plate, transfer the samples from the first plate back to the source plate, as shown in Fig. 3, and then wash the plate as normal. Add detection Ab to the first plate and the standard and samples to the second plate, as shown in Table 1.
Wash the first plate and add the SA–HRP. Transfer the samples from the second plate back to the source plate and wash the second plate. Then, add detection Ab to the second plate. We have measured up to three separate cytokines using the sequential ELISA (see Note 9).
Fig. 3.
A conceptual Illustration of the sequential ELISA. After the samples are subjected to one ELISA for cytokine 1, they are transferred back to a source plate for storage until they are used in the ELISA for cytokine 2, so on and so forth. The steps after the sample incubation are as normal for the particular ELISA adapted from ref. 6.
Table 1.
Schematic depicting the time arrangement of a simplified sequential ELISA protocol of exemplary targets analyzed in three subsequent cycles
| Time (h) | Previous day capture incubation overnight | ||
|---|---|---|---|
| Regular ELISA cycle # 1 | Sequential ELISA cycle # 2 | Sequential ELISA cycle # 3 | |
| 0.0 | Blocking | ||
| 1.0 | Samples | ||
| 2.0 | Incubation | Blocking | |
| 3.0 | Detection ⇒TRANSFER SAMPLESa | TO CYCLE # 2 ⇒Samples | |
| 4.0 | Incubation | Incubation | Blocking |
| 5.0 | Streptavidin–HRP | Detection ⇒TRANSFER SAMPLESa | TO CYCLE # 3 ⇒Samples |
| 5.5 | TMB | Incubation | Incubation |
| 6.0 | Reading | Incubation | Incubation |
| 7.0 | Streptavidin–HRP | Detection ⇒REMOVE AND STORE SAMPLESb | |
| 7.5 | TMB | Incubation | |
| 8.0 | Reading | Incubation | |
| 9.0 | Streptavidin–HRP | ||
| 9.5 | TMB | ||
| 10.0 | Reading | ||
Samples are removed and transferred to the storage plate (master mix) before washing and detection step
Samples are removed before washing, transferred to the master mix, and stored overnight at 4°C for consecutive cycles
3.5. The Multiplex ELISA
Two possible ways to measure multiple analytes from one sample include the cytometric bead array (CBA) and the multiplex ELISA. The CBA is a flow cytometry-based method in which specialized beads are coated with specific antibodies to the analytes of interest. Commercial kits are available that can provide measurement of up to 30 proteins from 25 to 50 µL of sample. If one desires, beads may be purchased without specific antibodies attached. This allows the user to customize the assay according to need. The general method is as such: Beads are conjugated in various intensities with a dye which fluoresces strongly within a specific channel filter (i.e., FL3). This creates distinct populations for data acquisition. Next, each specific population of these beads is coated with a specific capture antibody for the target of interest. Samples are then incubated with the “capture beads,” followed by incubation with a detection antibody conjugated to a fluorophore that emits light into a different filter channel than that of the capture bead (i.e., FL2). The FL2 fluorescence is in direct proportion to the amount of analyte present while the FL3 fluorescence indicates the specific analyte present (8). This method uses less sample volume than a single ELISA; however, the cost may be prohibitive because the user is required to buy kits. The multiplex ELISA is another way to measure multiple analytes from one sample and is further discussed below.
Due to the nature of the multiplex ELISA, specialized equipment is required. This necessitates a sizable initial investment; however, because of the high throughput and reduced labor, the cost per assay is substantially lower. There are significant differences in the printing apparatuses between manufacturers of the specialized equipment; as such, this section covers general considerations in developing a multiplex ELISA.
Due to the similarities between the standard single ELISA and the multiplex, similar optimization techniques can be used to develop the assay. The checkerboard described in Subheading 3.1 can be used to determine the optimal concentrations of antibodies and standards for the multiplex assay. In this instance, however, the standard and detection Ab must be added to each well as a cocktail because in each well there is essentially multiple, simultaneous ELISAs occurring (see Fig. 4 for illustration and Table 2 for list of analytes in the multiplex).
Table 2.
Example layout for the multiplex array in Fig. 4
| IL-1β | IL-1β | IL-1β | IL-1β | IL-1rα | IL-1rα | IL-1rα | IL-1rα |
| IL-2 | IL-2 | IL-2 | IL-2 | IL-4 | IL-4 | IL-4 | IL-4 |
| IL-5 | IL-5 | IL-5 | IL-5 | IL-6 | IL-6 | IL-6 | IL-6 |
| IL-10 | IL-10 | IL-10 | IL-10 | IL-12 | IL-12 | IL-12 | IL-12 |
| IL-13 | il13 | il13 | il13 | IFN-γ | IFN-γ | IFN-γ | IFN-γ |
| Mip-2 | Mip-2 | Mip-2 | Mip-2 | Mip1α | Mip1α | Mip1α | Mip1α |
| Rantes | Rantes | Rantes | Rantes | Eotaxin | Eotaxin | Eotaxin | Eotaxin |
| Eotaxin2 | Eotaxin2 | Eotaxin2 | Eotaxin2 | Mcp-1 | Mcp-1 | Mcp-1 | Mcp-1 |
| Tnf-α | Tnf-α | Tnf-α | Tnf-α | Tnf sr1 | Tnf sr1 | Tnf sr1 | Tnf sr1 |
| Tnf sr2 | Tnf sr2 | Tnf sr2 | Tnf sr2 | IL-17 | IL-17 | IL-17 | IL-17 |
| Icam | Icam | Icam | Icam |
3.5.1. General Method
The ELISA plates must first be printed with the capture antibody specific for the cytokines of interest. Again, the printing process is specific to the printer used, and the manufacturer’s recommendations should be followed.
Incubate the printed plates overnight at 4°C (see Note 10).
Block the plate with 150 µL/well of blocking buffer for 1 h.
Standard cocktail preparation: Using dilution buffer, mix each recombinant cytokine of interest into a heterogeneous cocktail. A 16-point standard curve (including the blank) that begins at 50,000 pg/mL/cytokine followed by twofold serial dilutions is sufficient (i.e.: dilutions of 1×, 2×, 4×, n×., 16,384×, or, 50,000–3.05 pg/mL).
Incubate standards, samples, and the detection Ab cocktail as with the standard ELISA procedure. For the sake of simplicity, dilute all detection Abs into the cocktail at the same concentration.
After the detection cocktail incubation is complete, wash the plate and add the streptavidin dye conjugate diluted in dilution buffer, 50 µL/well, and incubate for 30 min in the dark (see Note 11).
Wash the plate and dry thoroughly by spinning upside down in a centrifuge.
Inspect surface of plate for fingerprints or other optical obstructions. If necessary, clean the bottom of the plate and then place into the scanner.
Scan and analyze as suggested by the specific system used.
3.5.2. Cross-Reactivity Determination
As with the sequential ELISA, cross-reactivity poses a potential problem in a multiplex assay and the issue should be addressed prior to analyzing a sample. An experimental approach to determine the presence of cross-reactivity is listed in Table 3.
Table 3.
Determination of cross-reactivity for multiplex ELISA
| Capture | Standard | Detection | Assessment | |
|---|---|---|---|---|
| 1 | Capture | Complete standard cocktail | Complete detection cocktail | Ensures that Ab pairs provide signal |
| 2 | Capture | Complete standard cocktail | Ab of interest absent from cocktail | Ensures that other detection Abs do not interact with std of interest |
| 3 | Capture | std of interest absent from cocktail | Ab of interest absent from cocktail | Ensures that other std Abs and other det. Abs do not interact with capture of interest |
| 4 | Capture | std of interest absent from cocktail | Complete detection cocktail | Ensures that capture does not interact with any detection Abs or other stds |
| 5 | Capture | Only std of interest | Only Ab of interest | Ensures that Ab pairs work well and multiplex assay works as well |
3.5.3. Cost Comparison
An obvious advantage of the multiplex versus the standard ELISA is the greater amount of data generated from a single sample and within the same window of time. Less obvious is the money saved using the multiplex approach. The comparison is not straightforward and varies from lab to lab. Without regards to specialized equipment, the multiplex is more expensive than a standard ELISA on a per plate basis. However, when compared using a data per sample basis, the multiplex becomes more cost-efficient than the standard ELISA.
For example, our lab has found that it is more cost-effective to use the multiplex when measuring seven cytokines or more. This takes into account the cost of antibodies, technician time, and overhead costs (see Table 4 for an example comparison). To be most efficient, samples that require 7+ cytokine measurements are stored until there are enough samples to fill an entire plate.
Table 4.
Example cost comparison between multiplex and single cytokine ELISA. Costs are for analysis of 17 cytokines. Up to 40 samples/plate may be assayed
| Multiplex | Single | |
|---|---|---|
| Antibody costs | ||
| Capture | $17.28 | $72.00 |
| Standard | $0.81 | $2.00 |
| Detection | $41.04 | $91.20 |
|
| ||
| Consumables’ costs | ||
| Pipette tips | $2.00 | $40.00 |
| Clean room wipes | $0.20 | $0.00 |
| Plates | $4.00 | $68.00 |
| IR dye | $0.27 | $0.00 |
| Odyssey blocking buffer | $5.72 | $0.00 |
| Buffers | $0.50 | $40.00 |
| HRP | $0.00 | $2.00 |
| TMB | $0.00 | $8.80 |
| Total costs | $71.82 | $324.00 |
Footnotes
In general, high binding plates (>400 ng/cm2) work best for ELISAs, but may result in higher background readings. If the high background cannot be resolved through titration, one should consider the use of medium binding plates (250 ng/cm2).
It is acceptable, but cumbersome, to manually wash the plates with a multichannel pipette. It is not advisable to use a squirt bottle for washing because wash fluid from one well can spill into another, skewing results. Additionally, it is possible to leave the plates soaking in wash buffer for up to an hour; however, it is recommended that this is determined empirically for your ELISAs.
Any length of time may be used for each incubation so long as the incubation times used in the checkerboarding step of development are used going forward. It is likely that shorter incubation times will require an increased concentration of reactants. For instance, our lab has a standard IL-6 ELISA assay that takes 6+ hours to complete. We also have a rapid IL-6 ELISA that can be performed in less than 90 min and is useful when a rapid value is necessary (9).
The optimal dilution for SA–HRP typically remains the same across different cytokine ELISAs. This needs to be determined only once.
There is a linear relationship between the OD590 and the ΔOD(10). An OD590 of 0.4–0.5 translates to a ΔOD of ~ 1.2–1.6 (see Note 7).
There are several reasons why a plate may turn uniformly blue or not change color at all. Uniform color development across the plate may be due to the following: (1) User coated with biotinylated detection Ab instead of unlabeled capture antibody. (2) The biotinylated antibody has degraded causing NSB. (3) Too much capture and/or detection antibody was used. This is especially true in the initial stages of development (checkerboard), when the amount of antibody to be used is unknown. Lack of color development usually indicates a problem with the capture antibody or HRP conjugate. If all wells with standards turn blue too quickly, but the zero standard remains clear, repeat the ELISA with a more dilute standard range.
The optimal dilution of antibody may not have the highest signal-to-noise ratio for the top standard when compared to other dilutions. The signal:noise of the low and mid standard should guide your selection. This is because the OD of the top standard is likely representative of saturation of the system (either the capture or the detection Ab is not in excess to standard). What is important, however, is that the top standard has an OD around 1.5 or higher. ODs above 1.5–1.7 are unreliable for quantitative measurements in many plate readers (11), but they are a good starting point for the top standard. If the OD of the top standard does not reach this area, the range of the standard curve is decreased. If raising the concentration of standard does not increase the OD, it is likely that either the capture or detection antibodies are limiting.
The upper asymptote is a result of the standard being in excess to the capture or detection antibodies. It is important that this asymptote does not exceed the linear range of the plate reader being used. Decreasing capture or detection antibody concentrations decrease the maximum OD observed; however, there may be a trade-off in sensitivity of the ELISA. If sensitivity cannot be sacrificed, it is advisable to investigate the five-parameter logistic (5PL) fit model as an alternative to the 4PL. The 5PL can better handle curves with asymmetries such as those that may come from not achieving an upper or lower asymptote. Regardless of which curve model is selected, the OD of the standards must be within the linear range of the plate reader.
Samples can be stored overnight at 4°C to continue the sequential ELISAs the next day, since each additional plate adds 2 hours to the time devoted to the assay.
Printed plates may be stored for up to 6 months at 4°C. It is recommended to determine the stability of the printed plates under the conditions in your lab.
As with many fluorophores, exposure to ambient light may result in photobleaching. Care should be taken to limit the exposure of the IR dye to light.
References
- 1.Feghali CA, Wright TM. Cytokines in acute and chronic inflammation. Front Biosci. 1997;2:d12–26. doi: 10.2741/a171. [DOI] [PubMed] [Google Scholar]
- 2.Sokol H, Pigneur B, Watterlot L, et al. Faecalibacterium prausnitzii is an anti-inflammatory commensal bacterium identified by gut microbiota analysis of Crohn disease patients. Proc Natl Acad Sci USA. 2008;105:16731–16736. doi: 10.1073/pnas.0804812105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Polpitiya AD, McDunn JE, Burykin A, et al. Using systems biology to simplify complex disease: immune cartography. Crit Care Med. 2009;37:S16–21. doi: 10.1097/CCM.0b013e3181920cb0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.De Santo C, Arscott R, Booth S, et al. Invariant NKT cells modulate the suppressive activity of IL-10-secreting neutrophils differentiated with serum amyloid A. Nat Immunol. 2010;11:1039–1046. doi: 10.1038/ni.1942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.DeForge LE, Remick DG. Sandwich ELISA for detection of picogram quantities of interleukin-8. Immunol Invest. 1991;20:89–97. doi: 10.3109/08820139109054928. [DOI] [PubMed] [Google Scholar]
- 6.Osuchowski MF, Remick DG. The repetitive use of samples to measure multiple cytokines: the sequential ELISA. Methods (San Diego, Calif) 2006;38:304–311. doi: 10.1016/j.ymeth.2005.11.009. [DOI] [PubMed] [Google Scholar]
- 7.Findlay JWA, Dillard RF. Appropriate calibration curve fitting in ligand binding assays. AAPS Journal. 2007;9(2):E260–E267. doi: 10.1208/aapsj0902029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Morgan E, Varro R, Sepulveda H, et al. Cytometric bead array: a multiplexed assay platform with applications in various areas of biology. Clin Immunol. 2004;110:252–266. doi: 10.1016/j.clim.2003.11.017. [DOI] [PubMed] [Google Scholar]
- 9.Nemzek JA, Siddiqui J, Remick DG. Development and optimization of cytokine ELISAs using commercial antibody pairs. J Immunol Methods. 2001;255:149–157. doi: 10.1016/s0022-1759(01)00419-7. [DOI] [PubMed] [Google Scholar]
- 10.Natarajan S, Remick DG. The ELISA Standard Save: Calculation of sample concentrations in assays with a failed standard curve. J Immunol Methods. 2008;336:242–245. doi: 10.1016/j.jim.2008.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Crowther JR. The ELISA guidebook. Methods in molecular biology (Clifton, NJ) 2000;149(III–IV):1–413. doi: 10.1385/1592590497. [DOI] [PubMed] [Google Scholar]