Abstract
The Affordable Care Act (ACA) shifted the focus in medical care from quantity to quality. This qualitative systematic review determined the key skills to be an effective physician leader after the implementation of the ACA and to compare them to the key skills identified prior to its implementation. A qualitative systematic review collects qualitative data and can be analyzed in a number of ways, including thematic analysis that constructs themes from the pooled data. A systematic literature search on leadership skills for physicians resulted in 26 papers. Thematic analysis was used to categorize the data presented in each paper. The results from these 26 papers were then compared to a similar paper published prior to the implementation of the ACA. Teamwork and team-building, communication, and self-awareness skills were mentioned the most often. The percentage of papers mentioning teamwork and team-building skills (61.5%) was significantly greater than the percentage (25%) reported prior to the implementation of the ACA (p≤0.04). With the shift towards quality of patient care, healthcare workers at all levels should strive to work as a team to provide the best quality of care at all stages of patient care.
Keywords: Physician education, Health system reform, National health insurance, Leadership
The Affordable Care Act (ACA), implemented in 2010, was one of the most drastic changes in the US healthcare system since the emergence of private medical insurance in 1929, and Medicare/ Medicaid in the 1960s.1 One of the major changes in healthcare administration caused by the ACA is an expansion in the shift away from pay-per-service care and towards pay-for-performance care. The first pay-for-performance initiative was Medicare's Physician Group Practice (PGP) demonstration running for three years from 2005 through 2008, which established incentives for improving quality of care and cost efficiency.2 Pay-for-performance contracts mandate quality measures such as hospital readmission rates, patient satisfaction scores, mortality rates, early elective delivery rates, and catheter-associated urinary tract infection rates.3 The ACA includes the hospital readmission reduction program (HRRP) in which hospitals receive reduced Medicare payments for having high readmission rates. Studies examining the effects of the HRRP have shown that the hospital readmission rates, particularly for acute myocardial infarctions, have decreased since the implementation of the ACA.4 Payers provide financial incentives to hospitals for reducing readmission rates, thereby placing increased importance on the quality of care over traditional pay-per-service models.5 Furthermore, healthcare institutions are encouraged to work towards the triple aim put forth by the Institute for Healthcare Improvement for improved population health, improved patient experience of care, and lowered costs, which places further emphasis on the quality of care delivered.6
These changes have spurred demand for physician leaders.7 One outward result of this increase in demand is the emergence of the position of chief experience officer, or CXO, at healthcare institutions.8 A CXO is an executive in charge of the overall experiences and services of an institution and, in a healthcare setting, primarily focuses on patient satisfaction. A recent study of 300 hospital CEOs found that hospitals with physician CEOs provided better quality care than those with non-physician CEOs.9 Furthermore, a 2015 survey found that 63% of CEOs were seeking to recruit healthcare professionals with the right skill-set to become executives and 53% indicated they were planning to hire in the next year.7 As the demand for physician leaders rises, new leadership education programs for up-and-coming physicians have emerged.10-12 In addition, the number of joint degree MD/MBA programs that teach business principles alongside clinical skills has grown, with six programs in 1993 to 33 in 2002.13
The emergence of programs training physician leaders is critical for the progress and improvement of physician leaders over time. Our healthcare system needs to replenish physician leaders to ensure a ready supply of replacement leaders. Other general qualities of a leader have been described as the ability to direct the activities of a group toward a shared goal, influence group activities, and cope with change.14 Although many different types of effective leadership have been proposed and described, these general goals remain the same. In 2008, shortly before the implementation of the ACA, a review was published analyzing the key competencies needed to be an effective physician leader.15 The author found six core domains of necessary competence for successful physician leaders: communication, knowledge of healthcare, technical knowledge and skills, problem-solving prowess, emotional intelligence, and commitment to lifelong learning. The changes in healthcare administration influenced by the ACA and the related emphasis on the quality of care may have caused changes in the area of physician leadership, resulting in an alteration in these core domains. This systematic review aims to determine whether the skills considered to be the most important for physician leadership have changed in recent years since the implementation of the ACA. We hypothesize that skills necessary for team-based medicine will be emphasized more in newer publications than before the ACA was introduced.
Methods
We followed the Cochrane's guide for how to conduct a qualitative systematic review.16 Articles publishing primary qualitative research on physician leadership were collected in a step-wise fashion (by title, abstract, and full text). We then did a thematic analysis which resulted in the construction of 19 suggested skill groups for physician leaders.
Literature search
Using the PubMed electronic database, we searched for articles published from January 2009 to September 2016 containing both the phrase “physician” and “leader” along with the MeSH terms “physician executives”, “physicians”, “physician's role”, or “leadership.” The initial search returned 153 articles. The date range was chosen because drafting for the ACA began in 2009. There is a possibility that earlier pay-for-performance initiatives, such as the aforementioned PGP demonstration added a confounding factor to our results. However, previous initiatives were smaller in scale whereas the ACA expanded on these making pay-for-performance applicable to all healthcare settings. After analyzing the abstracts for papers that reported primary, qualitative data with physician leadership as a theme in addition to being published in the U.S., 46 articles remained. Articles were considered primary, qualitative data if they reported on a qualitative study such as a survey-based or observational study, contained interviews or quotes from physician executives or leaders, contained a case report, or were a narrative by a physician leader on his or her personal experiences. We chose to only analyze articles published in the U.S. because of our emphasis on the effect of the ACA on healthcare leadership. Further data analysis that extracted the reported skills necessary to become a successful physician leader left 26 articles that were used in the final analysis.17-42 Figure 1 shows the search strategy flow diagram.
Figure 1.
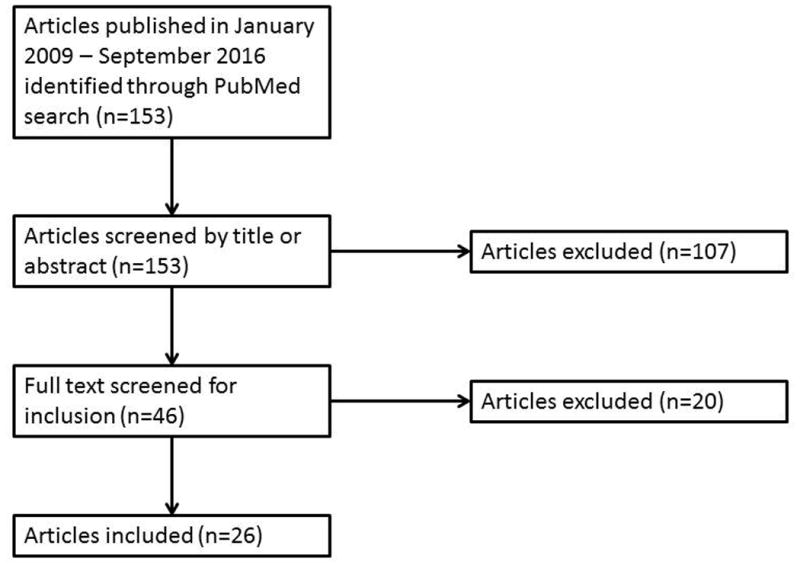
A search strategy flow diagram.
Thematic analysis
Skills helpful or important to physician leadership mentioned in each paper were extracted and then grouped together. If a skill was mentioned two or more times it was given its own group, and skills that were only mentioned once were put into a category called “other.” Nineteen skill groups were found, and these were then categorized into five overarching areas of competency (interpersonal skills, personal characteristics, business and law knowledge, self-awareness, managerial skills, and other) (Figure 2). Finally, current literature was compared to previous literature by grouping skills into the same six core domains found in the 2008 article by Stoller.15 These six core domains were not used universally throughout our analysis because we first wanted to determine what core domains would emerge when analyzing only the current literature. “Technical knowledge and skills” included knowledge of operations, finance and accounting, information technology and systems, human resources, strategic planning, legal issues in healthcare, and public policy. “Knowledge of healthcare” included knowing about reimbursement strategies, legislation and regulation, quality assessment, and management. “Problem-solving prowess” included organizational strategy and project management. Emotional intelligence included the ability to evaluate oneself and others, and the ability to manage oneself in the context of a group. “Communication skills” included leading change in groups and in individual encounters, including negotiation and conflict resolution. “A commitment to lifelong learning” was not further defined in the Stoller paper. In addition, the appendix of the Stoller paper catalogued 16 papers with details of leadership skills that were used in the thematic analysis to develop the six core domains. We compared the number of papers that mentioned teamwork in the Stoller paper to the 26 publications in our analysis.
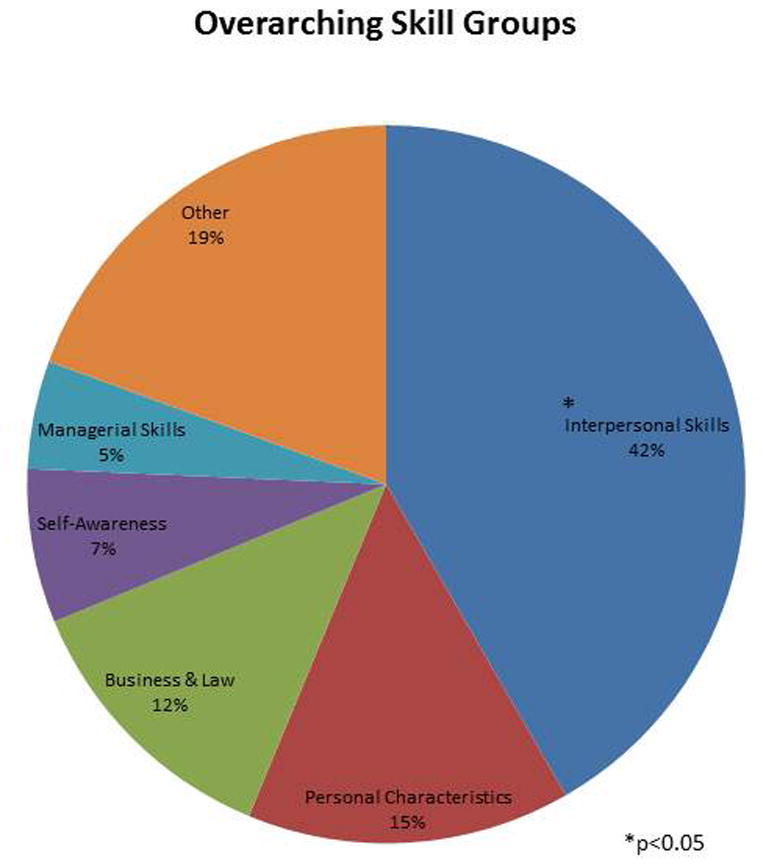
Figure 2.
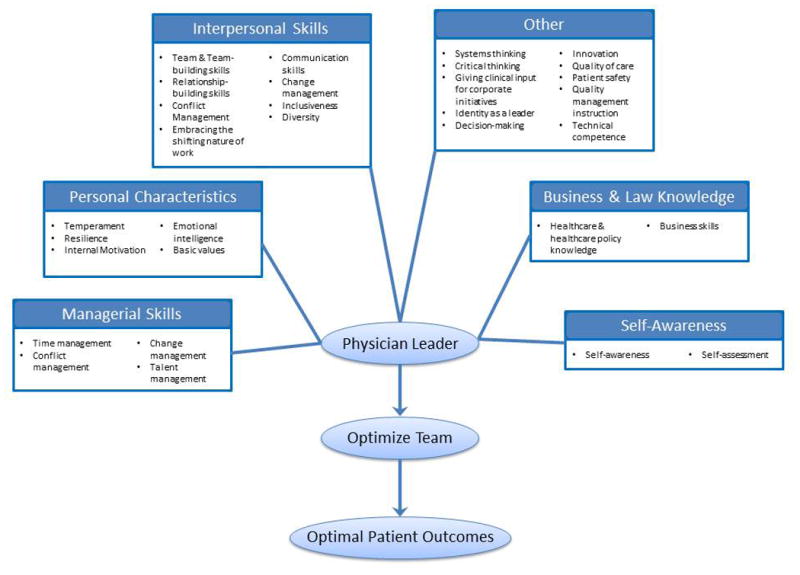
A conceptual model showing the percentage of skills falling under each overarching skill group. The interpersonal skill group was larger than all other groups, not including “other,” with p<0.01.
Statistics
We used Pearson's chi-squared tests to test for significant differences in proportions. Significance was considered at p<0.05.
Results
A total of 19 different detailed skill groups were identified in our analysis of 26 papers mentioning 138 individual skills. Team and team-building skills were cited most often with 61.5% (16/26) of the papers mentioning these skills, comprising 14.9% (21/138) of all skills mentioned. Communication skills were the second largest group with 57.7% (15/26) of papers mentioning them, comprising 12.8% (18/138) of all skills mentioned. These were the only two skills that were mentioned by 13 or more of the articles. The next most-cited skill was self-awareness, in 38.5% (10/26) of the papers. We found that communication skills and team and team-building skills were mentioned in significantly more papers than any other category except for self-awareness (p≤0.03) (Figure 3). There were no significant differences in the number of papers that mentioned any skills apart from communication, self-awareness, and team and team-building. In terms of overall skills stated, communication and team and team-building skills were also mentioned significantly more often than any other skills except for self-awareness (p≤0.04).
Figure 3.
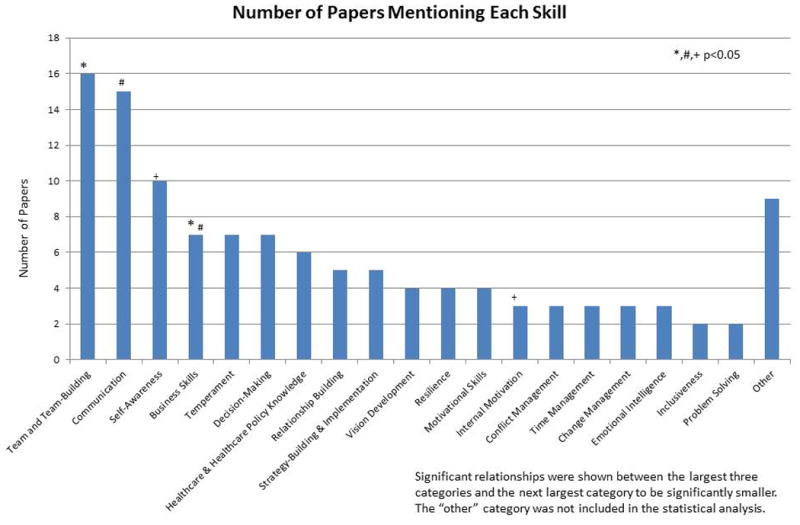
A bar graph depicting the number of papers mentioning skills within each group. Significant relationships were shown between the largest three categories and the next largest category to be significantly smaller. The “other” category was not included in the statistical analysis.
Figure 4 illustrates the distribution of papers when categorized according to Stoller's 6 core domains. In the 16 papers analyzed by Stoller, communication skills were mentioned most often, followed by knowledge of healthcare, technical knowledge and skills, problem-solving prowess, emotional intelligence, and a commitment to lifelong learning. In our 26 papers, communication skills were again mentioned most often, followed by technical knowledge and skills, emotional intelligence, knowledge of healthcare, problem-solving prowess, and a commitment to lifelong learning. Significantly fewer papers published in 2009 or later mentioned “problem-solving prowess” or problem-solving in general compared to papers published earlier (p=0.006). This was the only domain with a significant difference in proportions.
Figure 4.
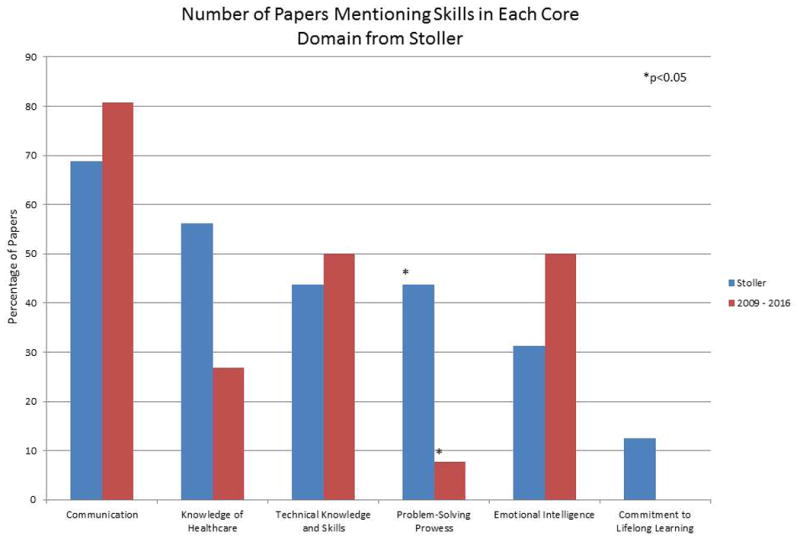
A bar graph comparing the number of papers mentioning skills in each of the core domains outlined by Stoller in 2008.
We compared the number of papers mentioning team and team-building skills between our analysis and Stoller's because it was our largest skill group and was not one of the 6 core domains determined by Stoller. 25% (4/16) of the papers analyzed by Stoller mentioned team skills compared to a significantly larger portion, 61.5% (16/26), of papers published in 2009 or later (p=0.02).
In a comparison of overarching skill groups (Figure 5), interpersonal skills represented 42% (60/138) of all skills mentioned. The next largest category was personal characteristics (15%, 21/138), followed by business and law (12%, 18/138), self-awareness (7%, 10/138), and managerial skills (5%, 7/138). The proportion of skills falling under “interpersonal skills” was significantly greater than any other category with a p-value<0.01 compared to each of the other skill groups. Excluding the “other” group, the remaining groups were not significantly different from each other.
Figure 5.
A graph showing the proportion of skills mentioned that fall into each of the overarching skill groups found in our thematic analysis.
Discussion
In 2010, about a month before the ACA was passed, the American College of Surgeons released a statement on the importance of teamwork and asserted that teamwork at all stages of patient care was necessary to achieve the best outcomes.43 Furthermore, team-based care is more important for success in the pay-for-performance care that is encouraged by the ACA. Rather than rewarding clinicians and other healthcare workers for only services and procedures rendered to the patient, the ACA rewards improved outcomes and other aspects of care such as transitions through hospitalization and surgery that rely on team-based care.44 Therefore, it is not surprising that the biggest difference between our review and the 2008 review is the importance of the team and team-building skill group. Although these skills were barely noted in the previous review, we found this group of skills to be the one most often mentioned and emphasized in the current literature.
The emergence of the emphasis of teamwork and team-building in recent literature on physician leadership indicates that hospitals and clinicians are attempting to transition to more team-centered care since the implementation of the ACA. Team-based care focuses on delivering effective and efficient care in a balanced way targeted at producing excellent patient outcomes.45 Surgeons, rather than focusing entirely on procedures in the operating room, also work with nurses and other staff to ensure that the patient receives optimal, personal care before and after the procedure. As one of the more drastic shifts in healthcare administration since the ACA, these results indicate that clinicians and administrators are both embracing the move towards team-based care as well as searching out resources to train up-and-coming healthcare workers in a more team-centered approach. Furthermore, the focus on teamwork as an essential skill for healthcare leaders indicates that team-based care should continue to be a central focus as healthcare organizations continue to make changes in response to the ACA.
In addition to teamwork, emotional intelligence, including self-awareness, continues to be essential skills for physician leaders. Emotional intelligence is the ability to understand and manage emotions in oneself and in others.46 It has been posited that emotional intelligence plays an essential role in leadership,46 and, in the more team-based environment that healthcare is moving towards, emotional intelligence and self-awareness will continue to become even more important. Emotional intelligence has been found to be linked to interpersonal and communication skills, which supports compassionate and empathetic patient care, improved medical knowledge, better coping with organizational pressures, improved teamwork, and improved doctor-patient communication.47 Leaders with greater emotional intelligence scores are more likely to discern patients' desires and more effectively motivate and critiquing members of their team, leading to more overall improvement and patient satisfaction. For example, in a situation when a patient is nervous about an upcoming surgical procedure, a surgeon with high emotional intelligence will pick up on this, sit down with the patient, and attempt to assuage his or her fears, whereas a surgeon with low emotional intelligence is more likely to ignore or never pick up on the patient's apprehension. Emotional intelligence is considered to be partially innate, but studies have shown that it can be improved with training,48 and many programs that aim to develop physician leaders focus, at least in part, on improving emotional intelligence.49,50
The combination of these skill groups, particularly self-awareness, communication skills, and team and team-building skills made up a large portion of the interpersonal skills we found to be mentioned most in the literature that we analyzed. The interpersonal skill group was significantly larger than any of the other overarching skill groups and comprised 42% of all stated skills. These skills were emphasized substantially more often than business and law skills, which included knowledge of healthcare laws and policies. In the Stoller article, the differences between the number of papers discussing communication skills versus those mentioning technical knowledge and skills (including business knowledge) or healthcare knowledge and skills was not significant. In addition, we found that significantly fewer articles published from 2009 onwards mentioned problem-solving skills. One possibility for the increased emphasis on interpersonal skills over knowledge and individual skill in more recent years is that, in a team-based setting, it is more important to be able to tap into the group's combined intelligence.
By tapping into group intelligence, the group can cover for individual weaknesses in business skills or knowledge. The team can be made up of a leader who has the strongest skills in communication, teamwork, and inspiring change and, in the case of a physician, has the most patient experience. The surgeon may have some knowledge of healthcare law and business skills including accounting, but may not have the same level of understanding as someone who dedicated their education to business and administrative subjects. However, he or she has knowledge and understanding of the complex issues and relationships physicians have with each other, with their staff, and with their patients that can then be used to improve the efficiency and efficacy of the team as a whole. Additionally, an efficient team can use these skills to improve outcomes of quality initiatives and other projects that indirectly improve patient outcomes.
By conducting a thorough search of articles published since 2009 and performing a thematic analysis, we were able to pinpoint the skills emphasized for physician leaders since the implementation of the ACA. Further research can be conducted to quantify how these skills affect patient experience using metrics to determine if there is a significant connection between this shift in physician leadership and patient experience. Once these skills and the level of their influence on patient outcomes are identified, the conversation can move on to the development of these skills and improvement of existing programs on physician leadership. The Stoller paper also looked at five physician leadership programs. They found that all five of their programs included a segment on teamwork and team-building, but only one in five focused on emotional intelligence or 360° feedback.15 All five discussed both financial and business knowledge.15 Our results would indicate that focus on teamwork should continue with an increased focus on emotional intelligence and self-awareness. In other words, interpersonal skills should be the main focus of any leadership development programs because they far outweigh any other skill group in our analysis. Group work, team exercises, and coaching can all be used to improve interpersonal skills. Furthermore, team exercises can lead to improvement of a surgical team's nontechnical skills which are correlated with the performance of technical skills.51 Therefore, investing in leadership training focusing on interpersonal skills may not only improve physician leadership but directly enhance clinical care as well. The ACA, as one of the biggest healthcare policy changes in US history, was bound to lead to changes in healthcare administration. Our findings show that physicians need to be actively engaged with other physicians, nurses, and other staff in order to become successful leaders. Programs and seminars that focus on improving physician leadership should focus more on effective communication, teamwork, and emotional intelligence than ever before with slightly less importance placed on business principles. Although business principles remain important, recent publications would suggest that well-developed interpersonal skills play a larger role in obtaining better patient results. Additionally, the healthcare community should continue to encourage the creation of dual degree MD/MBA and physician leadership programs in order to create a steady supply of leaders with a set of skills optimized for patient care under the ACA.
Acknowledgments
Indication of Funding Source: Research reported in this publication was supported by the National Institute of Arthritis and Musculoskeletal and Skin Diseases of the National Institutes of Health under Award Number 2 K24-AR053120-06. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
References
- 1.Zinner MJ, Loughlin KR. The evolution of health care in America. Urol Clin N Am. 2009;36:1–10. doi: 10.1016/j.ucl.2008.08.005. [DOI] [PubMed] [Google Scholar]
- 2.Kautter J, Pope GC, Trisolini M, Grund S. Medicare physician group practice demonstration design: quality and efficiency pay-for-performance. Health Care Financ Rev. 2007;29:15–29. [PMC free article] [PubMed] [Google Scholar]
- 3.Caveney BJ. Pay-for-Performance Incentives: Holy Grail or Sippy Cup? N C Med J. 2016;77:265–8. doi: 10.18043/ncm.77.4.265. [DOI] [PubMed] [Google Scholar]
- 4.Mellor J, Daly M, Smith M. Does It Pay to Penalize Hospitals for Excess Readmissions? Intended and Unintended Consequences of Medicare's Hospital Readmissions Reductions Program. Health Econ. 2016 doi: 10.1002/hec.3382. [DOI] [PubMed] [Google Scholar]
- 5.Kocher RP, Adashi EY. Hospital readmissions and the Affordable Care Act: paying for coordinated quality care. JAMA. 2011;306:1794–5. doi: 10.1001/jama.2011.1561. [DOI] [PubMed] [Google Scholar]
- 6.Barry JY, McCrary HC, Kent S, Saleh AA, Chang EH, Chiu AG. The Triple Aim and its implications on the management of chronic rhinosinusitis. Am J Rhinol Allergy. 2016;30:344–50. doi: 10.2500/ajra.2016.30.4348. [DOI] [PubMed] [Google Scholar]
- 7.Ostermeier L. Clinical Executives: The Rise of Healthcare's New Leader. B E Smith White Paper. 2015 [Google Scholar]
- 8.Carlson B. The Rise of the Chief Experience Officer. Physician Leadersh J. 2015;2:16–21. [PubMed] [Google Scholar]
- 9.Goodall AH. Physician-leaders and hospital performance: is there an association? Soc Sci Med. 2011;73:535–9. doi: 10.1016/j.socscimed.2011.06.025. [DOI] [PubMed] [Google Scholar]
- 10.Ackerly DC, Sangvai DG, Udayakumar K, et al. Training the next generation of physician-executives: an innovative residency pathway in management and leadership. Acad Med. 2011;86:575–9. doi: 10.1097/ACM.0b013e318212e51b. [DOI] [PubMed] [Google Scholar]
- 11.Clyne B, Rapoza B, George P. Leadership in Undergraduate Medical Education: Training Future Physician Leaders. R I Med J (2013) 2015;98:36–40. [PubMed] [Google Scholar]
- 12.Paller MS, Becker T, Cantor B, Freeman SL. Introducing residents to a career in management: the Physician Management Pathway. Acad Med. 2000;75:761–4. doi: 10.1097/00001888-200007000-00025. [DOI] [PubMed] [Google Scholar]
- 13.Larson DB, Chandler M, Forman HP. MD/MBA programs in the United States: evidence of a change in health care leadership. Acad Med. 2003;78:335–41. doi: 10.1097/00001888-200303000-00021. [DOI] [PubMed] [Google Scholar]
- 14.Al-Sawai A. Leadership of healthcare professionals: where do we stand? Oman Med J. 2013;28:285–7. doi: 10.5001/omj.2013.79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stoller JK. Developing physician-leaders: key competencies and available programs. J Health Adm Educ. 2008;25:307–28. [PubMed] [Google Scholar]
- 16.The Cochrane Collaboration; 2011. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0. [updated March 2011] Available from www.handbook.cochrane.org. [Google Scholar]
- 17.Aranda R, Tilton S. Myers-Briggs personality preferences may enhance physician leadership success in non-clinical jobs. Physician Exec. 2013;39:14–6. 8, 20. [PubMed] [Google Scholar]
- 18.Birk S. The future of physician leadership: physician leaders and the changing healthcare landscape. Healthc Exec. 2013;28:8–10. 2–4, 6. [PubMed] [Google Scholar]
- 19.Birk S. Creating a culture of ‘we’ investing in physician leaders. Healthc Exec. 2014;29:10–2. 4–6, 8. [PubMed] [Google Scholar]
- 20.Buell JM. Physician leadership development: a strategic imperative for integrated healthcare delivery. Healthc Exec. 2012;27:18–20. 2–3. 6 passim. [PubMed] [Google Scholar]
- 21.Dine CJ, Kahn JM, Abella BS, Asch DA, Shea JA. Key elements of clinical physician leadership at an academic medical center. J Grad Med Educ. 2011;3:31–6. doi: 10.4300/JGME-D-10-00017.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Garfield J. Leading Change: What Is Being Asked of Physician Leaders? Physician Leadersh J. 2015;2:46–9. [PubMed] [Google Scholar]
- 23.Grady CM. Can complexity science inform physician leadership development? Leadersh Health Serv (Bradf Engl) 2016;29:251–63. doi: 10.1108/LHS-12-2015-0042. [DOI] [PubMed] [Google Scholar]
- 24.Gustafson C. Mark Hertling, SVP Lieutenant General, US Army (Ret.): A Voice at the Table-Training Physician Leaders. Integr Med (Encinitas) 2016;15:54–9. [PMC free article] [PubMed] [Google Scholar]
- 25.Hayes C, Yousefi V, Wallington T, Ginzburg A. Case study of physician leaders in quality and patient safety, and the development of a physician leadership network. Healthc Q. 2010;13 doi: 10.12927/hcq.2010.21969. Spec No:68-73. [DOI] [PubMed] [Google Scholar]
- 26.Hemker RA, Solomon LA. Building a Physician Culture for Healthcare Transformation: A Hospital's Leadership Challenge. Front Health Serv Manage. 2016;32:3–14. [PubMed] [Google Scholar]
- 27.Howard J, Shaw EK, Felsen CB, Crabtree BF. Physicians as inclusive leaders: insights from a participatory quality improvement intervention. Qual Manag Health Care. 2012;21:135–45. doi: 10.1097/QMH.0b013e31825e876a. [DOI] [PubMed] [Google Scholar]
- 28.Long T, Katz MC, Hass D. Young Physicians' Leadership Curriculum: A Novel Approach to Creating Future Physician Leaders and Health Policy Advocates. Conn Med. 2015;79:41–3. [PubMed] [Google Scholar]
- 29.Malloy E, Butt S, Sorter M. Physician leadership and quality improvement in the acute child and adolescent psychiatric care setting. Child Adolesc Psychiatr Clin N Am. 2010;19:1–19. doi: 10.1016/j.chc.2009.08.008. table of contents. [DOI] [PubMed] [Google Scholar]
- 30.Neal JM. Congratulations, New Physician Leader… You're No Longer Special. Physician Leadersh J. 2015;2:50–3. [PubMed] [Google Scholar]
- 31.Nowill DP. Lessons of experience: Key events and lessons learned of effective chief medical officers at freestanding children's hospitals. J Healthc Manag. 2011;56:63–79. discussion -80. [PubMed] [Google Scholar]
- 32.Pradarelli JC, Jaffe GA, Lemak CH, Mulholland MW, Dimick JB. A leadership development program for surgeons: First-year participant evaluation. Surgery. 2016;160:255–63. doi: 10.1016/j.surg.2016.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Quinn JF. The affect of vision and compassion upon role factors in physician leadership. Front Psychol. 2015;6:442. doi: 10.3389/fpsyg.2015.00442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Quinn JF, Perelli S. First and foremost, physicians: the clinical versus leadership identities of physician leaders. J Health Organ Manag. 2016;30:711–28. doi: 10.1108/JHOM-05-2015-0079. [DOI] [PubMed] [Google Scholar]
- 35.Revere L, Robinson A, Schroth L, Mikhail O. Preparing academic medical department physicians to successfully lead. Leadersh Health Serv (Bradf Engl) 2015;28:317–31. doi: 10.1108/LHS-03-2014-0023. [DOI] [PubMed] [Google Scholar]
- 36.Satiani B, Sena J, Ruberg R, Ellison EC. Talent management and physician leadership training is essential for preparing tomorrow's physician leaders. J Vasc Surg. 2014;59:542–6. doi: 10.1016/j.jvs.2013.10.074. [DOI] [PubMed] [Google Scholar]
- 37.Shanafelt TD, Gorringe G, Menaker R, et al. Impact of organizational leadership on physician burnout and satisfaction. Mayo Clin Proc. 2015;90:432–40. doi: 10.1016/j.mayocp.2015.01.012. [DOI] [PubMed] [Google Scholar]
- 38.Swensen S, Kabcenell A, Shanafelt T. Physician-Organization Collaboration Reduces Physician Burnout and Promotes Engagement: The Mayo Clinic Experience. J Healthc Manag. 2016;61:105–27. [PubMed] [Google Scholar]
- 39.Throgmorton C, Mitchell T, Morley T, Snyder M. Evaluating a physician leadership development program - a mixed methods approach. J Health Organ Manag. 2016;30:390–407. doi: 10.1108/JHOM-11-2014-0187. [DOI] [PubMed] [Google Scholar]
- 40.Van Gorder M, Kearns D, Hong P. The Need for Physician Leadership Training: A Survey of the American Society of Pediatric Otolaryngology Members. Physician Leadersh J. 2015;2:70–5. [PubMed] [Google Scholar]
- 41.Warde CM, Vermillion M, Uijtdehaage S. A medical student leadership course led to teamwork, advocacy, and mindfulness. Fam Med. 2014;46:459–62. [PubMed] [Google Scholar]
- 42.Williams B. PLC: training the next generation of physician leaders. Tenn Med. 2009;102:27–9. [PubMed] [Google Scholar]
- 43.Statement on high-performance teams. American College of Surgeons; 2010. [Accessed October 21, 2016]. [PubMed] [Google Scholar]
- 44.Shock LP. Team-Based Care Offers a New World of Value. N C Med J. 2016;77:273–4. doi: 10.18043/ncm.77.4.273. [DOI] [PubMed] [Google Scholar]
- 45.Al-Touby SS. Functional results-oriented healthcare leadership: a novel leadership model. Oman Med J. 2012;27:104–7. doi: 10.5001/omj.2012.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.George JM. Emotions and leadership: The role of emotional intelligence. Hum Relat. 2000;53:1027–55. [Google Scholar]
- 47.Arora S, Ashrafian H, Davis R, Athanasiou T, Darzi A, Sevdalis N. Emotional intelligence in medicine: a systematic review through the context of the ACGME competencies. Med Educ. 2010;44:749–64. doi: 10.1111/j.1365-2923.2010.03709.x. [DOI] [PubMed] [Google Scholar]
- 48.Bamberger E, Genizi J, Kerem N, et al. A pilot study of an emotional intelligence training intervention for a paediatric team. Arch Dis Child. 2016 doi: 10.1136/archdischild-2016-310710. [DOI] [PubMed] [Google Scholar]
- 49.Erdman MK, Bonaroti A, Provenzano G, Appelbaum R, Browne M. Street Smarts and a Scalpel: Emotional Intelligence in Surgical Education. J Surg Educ. 2016 doi: 10.1016/j.jsurg.2016.09.004. [DOI] [PubMed] [Google Scholar]
- 50.Farver CF, Smalling S, Stoller JK. Developing leadership competencies among medical trainees: five-year experience at the Cleveland Clinic with a chief residents' training course. Australas Psychiatry. 2016;24:499–505. doi: 10.1177/1039856216632396. [DOI] [PubMed] [Google Scholar]
- 51.Rao R, Dumon KR, Neylan CJ, et al. Can Simulated Team Tasks be Used to Improve Nontechnical Skills in the Operating Room? J Surg Educ. 2016 doi: 10.1016/j.jsurg.2016.06.004. [DOI] [PubMed] [Google Scholar]


