Abstract
Background
Developmental care practices across pediatric cardiac intensive care units (CICUs) have not previously been described.
Purpose
To characterize current developmental care practices in North American CICUs.
Methods
A 47-item online survey of developmental care practices was developed and sent to 35 dedicated pediatric CICUs. Staff members who were knowledgeable about developmental care practices in the CICU completed the survey.
Findings/Results
Completed surveys were received from 28 CICUs (80% response rate). Eighty-nine percent reported targeted efforts to promote developmental care, but only 50% and 43% reported having a developmental care committee and holding developmental rounds, respectively. Many CICUs provide darkness for sleep (86%) and indirect lighting for alertness (71%), but fewer provide low levels of sound (43%), television restrictions (43%), or designated quiet times (21%). Attempts to cluster care (82%) and support self-soothing during difficult procedures (86%) were commonly reported, but parental involvement in these activities is not consistently encouraged. All CICUs engage in infant holding, but practices vary on the basis of medical status and only 46% have formal holding policies.
Implications for Practice
Implementation of developmental care in the CICU requires a well-planned process to ensure successful adoption of practice changes, beginning with a strong commitment from leadership and a focus on staff education, family support, value of parents as the primary caregivers, and policies to increase consistency of practice.
Implications for Research
Future studies should examine the short- and long-term effects of developmental care practices on infants born with congenital heart disease and cared for in a pediatric CICU.
Keywords: cardiac intensive care, cardiac nursing, child development, congenital heart defects, developmental care, postnatal development
BACKGROUND AND SIGNIFICANCE/LITERATURE REVIEW
Medical and surgical advancements have dramatically decreased mortality rates for infants with congenital heart disease (CHD).1 Surviving infants with complex forms of CHD present significant management challenges to their parents and caregivers in the pediatric cardiac intensive care unit (CICU). Many require cardiac surgery in the first days or weeks following birth, often returning to the CICU with a mediastinal incision, artificial airway with mechanical ventilation, and peripheral, central, or intracardiac catheters. Postoperatively, these infants are at risk for low cardiac output, malignant arrhythmias, multiorgan dysfunction, and infection.2 Neurobehaviorally, they are often hypersensitive and difficult to calm and feed.3,4 Studies suggest that brain development is structurally delayed in infants with certain forms of complex CHD,5 which could contribute to poor feeding skills and other challenges in regulatory functioning. Many infants with CHD will go on to exhibit neurodevelopmental (ND) deficits, including developmental delays, learning disabilities, and behavior problems, requiring special education and mental health services.6
Length of perioperative CICU and hospital stay are robust predictors of ND outcomes for infants with CHD,7,8 highlighting the importance of early hospital experiences for later functioning. While multiple medical factors likely contribute to increased length of stay and ND risk,6 including disease severity and complexity of surgical intervention, these factors are not easily modified. One potentially modifiable variable is the environment of the critical care unit, which may be adapted to promote optimal development during this sensitive period.9 Current medical care in the CICU necessitates that infants are exposed to developmentally unexpected and unpleasant stimuli, including bright lights, high sound levels, and frequent stressful and painful interventions, all in the face of significantly diminished positive experience. While the CICU is necessary for the assurance of survival, the excessive and unexpected environmental and negative tactile stimulation are potentially detrimental to the fragile brain’s organization and development.10
Developmental care in the neonatal intensive care unit (NICU) has been shown to improve ND and psychosocial outcomes for preterm infants and their families and is widely agreed to be best practice for vulnerable high-risk infants.11 Developmental care is a broad category of interventions designed to individualize care and minimize stress of infants to maximize neurologic development. Elements of developmental care include control of external stimuli (vestibular, auditory, visual, tactile), regulatory infant support, clustering of care activities, providing consistent caregivers such as primary nursing, positioning support, feeding/oral motor interventions, nonpharmacologic comfort measures, and family-integrated care that cultivates parents’ capacity to observe, understand, and respond to their infants’ states and behavioral cues to promote more optimal infant regulatory functioning. Within family-integrated care, parents are an integral part of the healthcare team and are incorporated into every possible aspect of their child’s care.12 Research suggests that providing a developmentally appropriate and consistent care environment in which parents are in control and support their infants’ physiologic and psychologic needs may lead to improved infant outcomes along with reduced parent stress and anxiety.13 Developmental and family-integrated care strategies have also been combined to form comprehensive programs, such as the “Newborn Individualized Developmental Care and Assessment Program,”14 which has been associated with enhanced brain structure and function, shorter intensive care and hospital stays, better weight gain, and improved behavioral outcomes that endure beyond infancy and into school age.15–18
Individualized, family-integrated, and developmentally supportive care during both preoperative and postoperative periods may be helpful in promoting behavioral organization and optimal neurodevelopment in infants with CHD. However, implementation of developmental care, a theory-guided rather than procedurally driven approach, is especially challenging in an acute and intensive care setting such as a CICU, which is often oriented to standards, protocols, and strictly enforced rules and caregiving routines. In the critical and high-stress environment of the CICU where staff often must balance competing priorities of managing high-risk technologies and providing life-saving interventions, developmental care practices may be perceived as less important or vital in the caregiving routine. Implementing developmental care practices in a CICU requires a thoughtful and well-planned process to ensure successful adoption of practice changes, beginning with a strong commitment from leadership and a focus on staff education as well as family support, parent education, and value of parents as the primary caregivers.9 Although developmental care practices are implemented to varying degrees in many North American CICUs, no data have been published on developmental care interventions for infants with CHD across CICUs. The purpose of this study was to characterize current developmental care practices in North American pediatric CICUs to inform future best practice recommendations and identification of education and resources necessary to promote developmental care in the CICU setting. This study addressed the following questions: (1) What developmental care practices are currently implemented in North American pediatric CICUs? (2) What aspects of developmental care are most easily applied to care in the CICU? and (3) What specific barriers impact the implementation of CICU developmental care practices? There has been a recent shift toward providing postoperative care within a dedicated CICUs versus a general pediatric intensive care unit (PICU),19 and the presence of a CICU is used as a measure of quality in ranking US pediatric heart surgery programs.20 This study focused exclusively on centers in which cardiac critical care is provided within a dedicated pediatric CICU, as the culture and environment of these settings are likely to differ from a general PICU or NICU, given the more targeted patient population and complexity of care.
METHODS
Design
This article reports the results of a cross-sectional, descriptive study of developmental care practices in North American pediatric CICUs.
Sample
Thirty-five cardiac centers in North America with a dedicated pediatric CICU were identified and sent an online survey regarding CICU developmental care practices. Centers in which cardiac critical care is provided within a PICU or NICU were excluded. Survey recipients were asked to identify one staff member from their center who was knowledgeable about developmental care practices in the pediatric CICU and willing to complete the survey. To maintain anonymity of survey respondents, identifying information about respondents was not obtained.
Instruments
A 47-item electronic survey of CICU developmental care practices was developed by the authors (see Supplemental Digital Content 1, http://links.lww.com/ANC/A12, for a text document containing survey items). Survey domains included hospital information, developmental education/rounding, environmental adaptations, implementation of infant care (including positioning, restraints, and sedation), infant holding, and developmental support for preschool and school-aged children. The majority of items were multiple choice with an “other (please specify)” response option. Fifteen items prompted an open-ended response. The survey required 15 to 20 minutes to complete.
Statistical Analysis
Multiple-choice survey data were analyzed using descriptive statistics (frequencies, percentages). Themes within the open-ended data were structured by the survey tool.
Procedures
Survey responses were recorded in SurveyMonkey and reviewed by the first author for accuracy and completion. Hospital name was obtained to ensure a single response per CICU but was removed and replaced with a unique study number by the first author prior to data analysis. This study was reviewed by the Nemours Institutional Review Board and was determined to meet the criteria for exempt research without the requirement for documentation of informed consent.
RESULTS
Site Characteristics
One survey response per center was obtained from 28 cardiac centers with a dedicated pediatric CICU (80% response rate). Six were located in the Northeast, 7 in the Southeast, 7 in the Midwest, 3 in the Southwest, 4 in the West, and 1 in Canada. Three survey respondents indicated that their CICU had 10 or fewer beds, 12 indicated that their CICU had 11 to 20 beds, and 13 indicated that their CICU had 21 to 30 beds.
Developmental Education/Rounding
Twenty-five CICUs (89%) reported targeted efforts to promote developmental care practices in the CICU setting, but only 14 (50%) reported having a dedicated task force/committee. Twelve CICUs (43%) hold regularly scheduled developmental rounds, typically occurring on a weekly basis, taking place at the bedside for at least a portion of the time, and involving parent participation consistently or sometimes. Providers most often involved in developmental rounds include occupational therapists (92%), speech/feeding therapists (83%), physical therapists (75%), nurses (75%), nurse practitioners/physician assistants (75%), and child life specialists (75%). Physicians (50%), social workers (42%), psychologists (25%), lactation consultants (25%), and music therapists (25%) are less often involved. Many CICUs reported the use of developmental education and bedside guidance to promote developmental care, but also noted challenges including lack of funding, time, staff, and support for developmental education. See Table 1 for survey respondent comments regarding best practices and barriers related to education and implementation of developmental care.
TABLE 1.
Survey Respondent Comments Regarding Best Practices and Barriers Related to Developmental Care
| Survey Domain | Best Practices | Barriers/Challenges |
|---|---|---|
Developmental education/rounding
|
Formal training
|
Limited time/resources
|
Environmental adaptations
|
Regulation of light and sound
|
Environment
|
Implementation of care and restraint/sedation use
|
Support for self-soothing
|
Inconsistent practices
|
Infant holding
|
Preventing/overcoming negative events
|
Inconsistent practices
|
Abbreviations: CICU, cardiac intensive care unit; DC, developmental care; NICU, neonatal intensive care unit; OT, occupational therapy; PT, physical therapy.
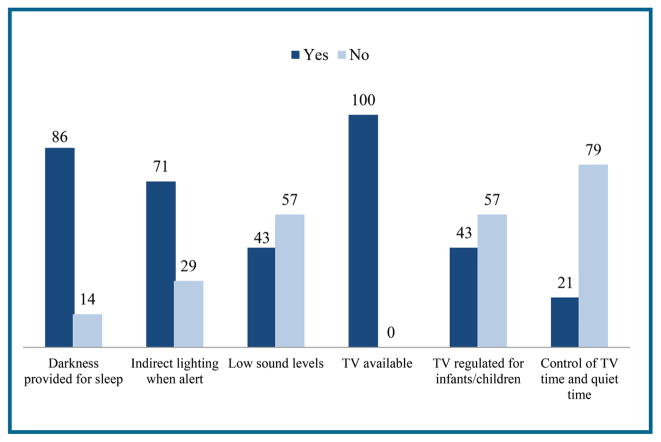
Environmental Adaptations
Pediatric CICUs reported differing environmental adaptations and supports (Figure 1 and Table 1). Many provide darkness for sleep (86%) and indirect lighting for alertness (71%), but fewer provide consistently low levels of sound (43%). Challenges were reported in providing quiet and dim environments for critically ill infants who require frequent medical interventions and caregiving. All CICUs reported the use of television at the bedside with less than half implementing television restrictions or regulations (43%). Even fewer CICUs implement designated quiet times or hours without television (21%). Discussion with families regarding developmentally appropriate television use and modeling of these behaviors were reported as inconsistent in the CICU.
FIGURE 1.
Environmental adaptations. Amounts are represented as percentages. N = 28.
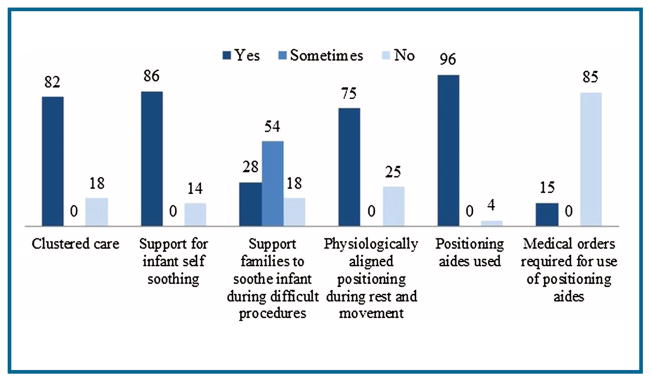
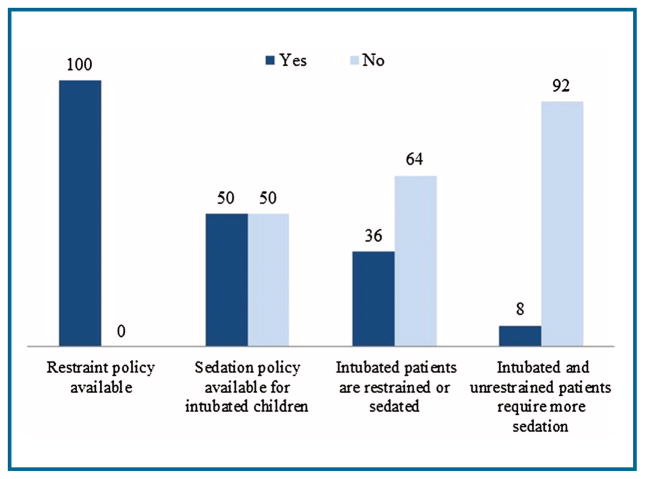
Implementation of Infant Care
Most CICUs reported consistent attempts to cluster infant care to allow opportunities for rest (82%). However, this was noted to be challenging because of frequent interruptions for procedures and even contraindicated at times for a medically complex infant. Only 28% of CICUs reported that they consistently attempt to engage and support parents in soothing their infants during difficult procedures. Fifty-four percent of CICUs sometimes provide support to parents to soothe their infants, but these efforts often depended on parents’ comfort level and the complexity of the procedure. Many CICUs reported striving for individualized physiologically aligned positioning during rest and movement (75%) and most use positioning support for containment like bendy bumpers, rolled blankets, or pillows (96%) (Figure 2). All CICUs reported a policy for patient restraint, but only half have a sedation policy for intubated children. Thirty-six percent of CICUs reported that intubated patients are either sedated or restrained. Open-ended survey responses report inconsistency in sedation and restraint practices (Figure 3 and Table 1).
FIGURE 2.
Implementation of developmentally based infant care. Amounts are represented as percentages. N = 28.
FIGURE 3.
Restraint and sedation use. Amounts are represented as percentages. N = 28.
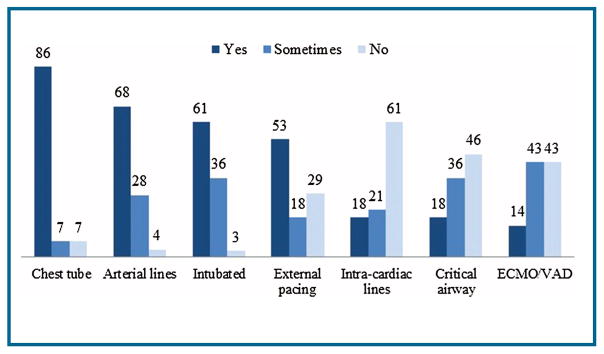
Infant Holding
All CICUs reported engaging in infant holding, with 57% encouraging kangaroo/skin-to-skin holding. Most CICUs reported allowing holding when infants have less invasive medical devices such as chest tubes. However, medical complications such as critical airways and devices such as intracardiac lines and pacing wires present challenges to holding (Figure 4). Concerns for infant stability and nursing comfort in holding a fragile infant were noted. Only 46% reported having a formal policy for infant holding. Open-ended survey responses indicated that most CICUs engage in holding while on a ventricular assist device but not on extracorporeal membrane oxygenation unless at the end of life. Sixty-one percent of CICUs responded that they do not engage in holding with intracardiac lines, but close to 20% of these CICUs also noted that intra-cardiac lines are often removed quickly after surgery and therefore do not interfere with holding. For the CICUs responding “sometimes” to holding questions, open-ended responses indicated that holding is performed “rarely,” “probably not,” or only after meeting certain criteria such as physical review or end of life. Thirty-nine percent of CICUs reported adverse events associated with infant holding, but noted that these events have not usually limited holding practices and have instead resulted in increased education for the medical team and family regarding proper holding techniques.
FIGURE 4.
Infant holding. Amounts are represented as percentages. N = 28. ECMO, extra-corporeal membrane oxygenation; VAD, ventricular assist device.
Developmental Support for Preschool and School-aged Children
While 96% of CICUs reported providing some form of developmental support for preschool-aged and school-aged children, challenges in providing developmental care within such a broad age range were noted. Developmental care support for preschool-aged and school-aged children is often provided by child life specialists, physical therapists, occupational therapists, speech/feeding therapists, and hospital-based schoolteachers/tutors. Less frequently, developmental support for this age group is provided via music therapy, art therapy, pet therapy, psychology consultation, or volunteer program. Several CICUs noted having a unit-based playroom, developmentally appropriate toys, and computer/video game access for preschool-aged and school-aged children.
DISCUSSION
A growing body of evidence suggests that brain development may be influenced by the quality of care provided to infants, including sensory stimulation, physical and emotional closeness to caregivers, and sedation use.15–18,21, 22 The survey results described in this study recorded developmental care practices within varying sized CICUs across the United States and Canada. Survey responses indicated that developmental care practices vary within and across CICUs and noted both strengths and unique challenges in CICU developmental care. Areas of strength included knowledge of and targeted efforts to promote developmental care for both infants and older children, adjustments to light, attempts to cluster care and facilitate self-regulation, and the use of positioning aides to support physically well-aligned positioning. However, care practices are reportedly inconsistent, with particular challenges described in the ability to regulate sound and television use, reduce the use of sedation and restraints, engage in infant holding, and fully integrate families into the care of the infant.
Implications for Practice
The results of this survey highlight areas of opportunity for change. Implementation must include a well-planned process to ensure successful adoption of practice changes, beginning with a strong commitment from leadership including time and resources allocated to developmental care, policies and guidelines for developmental care, and a focus on education for all staff from the nurse at the bedside to the therapist and physician. Parent education and support of parents as the primary caregivers are also imperative for the adoption of developmental care. Formation of a developmental care committee and consistent developmental rounding with participation from both staff and parents are important mechanisms through which to promote practice change. Including staff from a variety of disciplines in developmental committees and rounding can provide a richer and broader perspective on child and family functioning and practice change.
Basic tenets of developmental care can be incorporated, no matter how sick an infant is. However, concerns for physiologic and medical status were often identified as barriers to implementing developmental care. CICU nurses must partner with the interdisciplinary team to advocate for best practice guidelines regarding developmental care to decrease inconsistencies in practice. While most CICUs reported targeted efforts to promote developmental care, in many cases these have not been formalized. Policies specifically around infant holding, sedation use, and infant positioning would be helpful for families, patients, and staff. Most units identified the need for additional education and allocation of resources in support of developmental care. However, only half of CICUs have a formal developmental task force/committee and less than half hold regularly scheduled developmental rounds. In addition, physicians are not consistently involved in developmental rounds, which is an area in need of improvement, as physician engagement and support for developmental care initiatives are crucial for their ongoing success. Social workers and psychologists are also not often involved in developmental rounds and thus a mental health professional may not be available to address the psychosocial needs of the family that could impact development and provide recommendations to support the family.
A critical component of developmental care involves approaching the infant from within the context of a family unit and incorporating parents into every possible aspect of their child’s care. Based on survey responses, parents are not consistently included in developmental care practices in the CICU, such as developmental rounding and soothing the infant during difficult procedures. Programs to promote staff acceptance and encouragement of parental involvement in all aspects of the infant’s care in the hospital setting are imperative. Nurses and other staff can partner with parents to read and understand the infant’s behavioral cues within the hospital environment and medical staff should encourage parents to respond to the infant’s cues with developmentally supportive care, including nonnutritive sucking with a pacifier or at the breast, gentle touch, holding, or kangaroo care. Parents can also find encouragement through parent group programs, including parent-to-parent support with a focus on coping along with developmental care education. Given research indicating that parental role alteration contributes to anxiety for mothers whose infants are being cared for in a pediatric CICU23 and that maternal mental health may influence infant developmental and behavioral outcomes,24–26 it is clinically important to support families and provide interventions that reduce separation of family and infant. Supporting parents as valuable members of their infant’s care team may help prevent parental depression and anxiety and promote positive child outcomes.13
While acknowledging the challenges in feeding a child with CHD, the American Heart Association promotes pumping of breast milk within hours after birth and breastfeeding when oral feeding is introduced, as breastfed babies with CHD tend to have more consistent weight gain than bottle-fed babies.27 Meeting with a lactation consultant within the hospital setting is also recommended by the American Heart Association. Despite this, involvement of lactation consultations in developmental rounding was reported to be limited. Kangaroo care and nonnutritive sucking at the breast may also assist the promotion of breastfeeding for infants with CHD. Bedside nurses and lactation support can assist mothers in holding their infants skin-to-skin and allow for infants to latch onto the breast when displaying feeding cues.
Implications for Future Research
This study aimed to characterize CICU developmental care practices but did not explore their relation to short- or long-term outcomes. Future studies are needed to examine the impact of developmental care practices on ND and medical outcomes of infants born with CHD and cared for in a pediatric CICU. Research is also needed to inform best practice guidelines regarding CICU developmental care, including empirical investigations of negative and positive events associated with infant holding, strategies to enhance the parental role and promote parental involvement in developmental care, and approaches to staff training and education. This study should be replicated in PICUs, as they continue to care for large numbers of infants with CHD in a setting where developmental care practices are critical.
Limitations
This study focused exclusively on North American cardiac centers with a dedicated pediatric CICU and results may not be generalizable to the care of infants with CHD in a PICU or NICU or to pediatric CICUs outside of North America. Only 80% of identified pediatric CICUs responded to the survey. Although these CICUs represented a wide range of geographic regions and sizes, it is possible that results may have differed somewhat had all of the CICUs responded. In addition, it is possible that some centers with a “dedicated” pediatric CICU were not identified, such as those that have recently transitioned to a dedicated CICU model. Survey responses may differ depending on the role of the respondent in the CICU and his or her general perspectives on or prior experiences with developmental care. Unfortunately, the anonymous nature of this survey did not allow examination of responses by profession or other characteristics of the respondent. The survey was developed by the authors for the purposes of this study and psychometric properties are not available at this time. In addition, some important aspects of developmental care were not included in the survey, such as the use of single family rooms, precluding a complete characterization of developmental care practices in the CICU.
CONCLUSIONS
Given a growing literature supporting the use of developmental care for high-risk infants,15–18,21, 22 professionals delivering care in the pediatric CICU should be informed and knowledgeable about these practices and provide opportunities for individualized, family-integrated, and developmentally supportive care. Those responsible for CICU staff development and training are also encouraged to learn about developmental training and support. Despite the increasing availability of the Newborn Individualized Developmental Care and Assessment Program and other types of developmental training and systems consultation, developmental care is a new endeavor for the CICU and is not practiced consistently. Many CICU professionals continue to encounter significant systems, financial, and time-based barriers, along with the perception that developmental care may not be appropriate or necessary for infants in the CICU. Yet, there appears to be an increasing awareness of the importance of individualized developmental care and support to engage in selected aspects of developmental care. Evidence from premature neonates, which are a comparable group with similar early risks, suggests that developmentally supportive and family-integrated care in the ICU can have positive short- and long-term benefits for children and their families. Modifying the CICU model of care to further incorporate developmental care practices has the potential to improve ND outcomes and child and family quality of life.
WhatThis Study Adds.
Description of current developmental care practices in North American pediatric cardiac intensive care units (CICUs)
Understanding of strengths and challenges in implementing developmental care in the CICU
Discussion of the important role of the parent for developmental care in the CICU
Summary of Recommendations for Practice and Research.
| What we know: |
|
| What needs to be studied: |
|
| What we can do today: |
|
Acknowledgments
The authors thank the staff members who took the time to complete the survey on developmental care practices. Dr. Sood’s work on this project was supported by an Institutional Development Award (IDeA) from the National Institute of General Medical Sciences of the National Institutes of Health under grant U54-GM104941 (PI: Binder-Macleod). Dr Medoff-Cooper has funding from NIH/National Institute of Nursing Research (R01 NR002093) and Clinical and Translational Science Award (CTSA) program (MO1-RR00240; UL1-RR-024134). Dr Butler’s work on this project was supported by funding from the Kenrose Kitchen Table Foundation.
Footnotes
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s Web site (www.advancesin-neonatalcare.org).
Data collection and management was conducted at Nemours/Alfred I. duPont Hospital for Children.
No conflicts of interest were declared.
References
- 1.Khairy P, Ionescu-Ittu R, Mackie AS, et al. Changing mortality in congenital heart disease. J Am Coll Cardiol. 2010;56:1149–1157. doi: 10.1016/j.jacc.2010.03.085. [DOI] [PubMed] [Google Scholar]
- 2.Tweddell JS, Hoffman GM. Postoperative management in patients with complex congenital heart disease. Semin Thorac Cardiovasc Surg Pediatr Card Surg Annu. 2002;5:187–205. doi: 10.1053/pcsu.2002.31499. [DOI] [PubMed] [Google Scholar]
- 3.Massaro AN, Glass P, Brown J, et al. Neurobehavioral abnormalities in newborns with congenital heart disease requiring open-heart surgery. J Pediatr. 2011;158:678–681. e2. doi: 10.1016/j.jpeds.2010.11.060. [DOI] [PubMed] [Google Scholar]
- 4.Hartman DM, Medoff-Cooper B. Transition to home after neonatal surgery for congenital heart disease. MCN Am J Matern Child Nurs. 2012;37:95–100. doi: 10.1097/NMC.0b013e318241dac1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Licht DJ, Shera DM, Clancy RR, et al. Brain maturation is delayed in infants with complex congenital heart defects. J Thorac Cardiovasc Surg. 2009;137:529–537. doi: 10.1016/j.jtcvs.2008.10.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Marino BS, Lipkin PH, Newburger JW, et al. Neurodevelopmental outcomes in children with congenital heart disease: evaluation and management: a scientific statement from the American Heart Association. Circulation. 2012;126:1143–1172. doi: 10.1161/CIR.0b013e318265ee8a. [DOI] [PubMed] [Google Scholar]
- 7.Newburger JW, Sleeper LA, Bellinger DC, et al. Early developmental outcome in children with hypoplastic left heart syndrome and related anomalies: the single ventricle reconstruction trial. Circulation. 2012;125:2081–2091. doi: 10.1161/CIRCULATIONAHA.111.064113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Newburger J, Wypij D, Bellinger D, et al. Length of stay after infant heart surgery is related to cognitive outcome at age 8 years. J Pediatr. 2003;143:67–73. doi: 10.1016/S0022-3476(03)00183-5. [DOI] [PubMed] [Google Scholar]
- 9.Torowicz D, Lisanti AJ, Rim JS, et al. A developmental care framework for a cardiac intensive care unit: a paradigm shift. Adv Neonatal Care. 2012;12:S28–S32. doi: 10.1097/ANC.0b013e318265aeef. [DOI] [PubMed] [Google Scholar]
- 10.Anand KJ, Scalzo FM. Can adverse neonatal experiences alter brain development and subsequent behavior? Biol Neonate. 2000;77:69–82. doi: 10.1159/000014197. [DOI] [PubMed] [Google Scholar]
- 11.Kenner C, McGrath J, editors. Developmental Care of Newborns and Infants: Guide for Health Professionals. 2. Philadelphia, PA: Mosby; 2010. [Google Scholar]
- 12.O’Brien K, Bracht M, Macdonell K, et al. A pilot cohort analytic study of family integrated care in a Canadian neonatal intensive care unit. BMC Pregnancy Childbirth. 2013;13(suppl 1):S12. doi: 10.1186/1471-2393-13-S1-S12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jiang S, Warre R, Qiu X, et al. Parents as practitioners in preterm care. Early Hum Dev. 2014;90:781–785. doi: 10.1016/j.earlhumdev.2014.08.019. [DOI] [PubMed] [Google Scholar]
- 14.Als H. Program Guide—Newborn Individualized Developmental Care and Assessment Program (NIDCAP): An Education and Training Program for Health Care Professionals. Boston, MA: Children’s Medical Center Corporation; 1986. revised 2008 (11th revision) [Google Scholar]
- 15.Als H, Duffy FH, McAnulty GB, et al. Early experience alters brain function and structure. Pediatrics. 2004;113:846–857. doi: 10.1542/peds.113.4.846. [DOI] [PubMed] [Google Scholar]
- 16.McAnulty G, Duffy FH, Kosta S, et al. School age effects of the Newborn Individualized Developmental Care and Assessment Program for preterm infants with intrauterine growth restriction: preliminary findings. BMC Pediatr. 2013;13:25. doi: 10.1186/1471-2431-13-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Als H, Duffy FH, McAnulty G, et al. NIDCAP improves brain function and structure in preterm infants with severe intrauterine growth restriction. J Perinatol. 2012;32:797–803. doi: 10.1038/jp.2011.201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Als H, Duffy FH, McAnulty GB, et al. Is the Newborn Individualized Developmental Care and Assessment Program (NIDCAP) effective for preterm infants with intrauterine growth restriction? J Perinatol. 2011;31:130–136. doi: 10.1038/jp.2010.81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Burstein DS, Rossi AF, Jacobs JP, et al. Variation in models of care delivery for children undergoing congenital heart surgery in the United States. World J Pediatr Congenit Heart Surg. 2010;1:8–14. doi: 10.1177/2150135109360915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.US News and World Report. [Accessed September 20, 2015];US News and World Report’s America’s best children’s hospitals. www.rti.org/besthospitals.
- 21.Buehler DM, Als H, Duffy FH, et al. Effectiveness of individualized developmental care for low-risk preterm infants: behavioral and electrophysiological evidence. Pediatrics. 1995;96:923–932. [PubMed] [Google Scholar]
- 22.Fleisher BE, VandenBerg K, Constantinou J, et al. Individualized developmental care for very-low-birth-weight premature infants. Clin Pediatr (Phila) 1995;34:523–529. doi: 10.1177/000992289503401003. [DOI] [PubMed] [Google Scholar]
- 23.Lisanti AJ. Maternal Stressors and Stress Response in a Pediatric Cardiac Intensive Care Unit. Widener University School of Nursing Digital Dissertation; 2014. [Google Scholar]
- 24.McCusker CG, Doherty NN, Molloy B, et al. A controlled trial of early interventions to promote maternal adjustment and development of infants born with severe congenital heart disease. Child Care Health Dev. 2010;36:110–117. doi: 10.1111/j.1365-2214.2009.01026.x. [DOI] [PubMed] [Google Scholar]
- 25.Kikkert HK, Middelburg KJ, Hadders-Algra M. Maternal anxiety is related to infant neurological condition, paternal anxiety is not. Early Hum Dev. 2010;86:171–177. doi: 10.1016/j.earlhumdev.2010.02.004. [DOI] [PubMed] [Google Scholar]
- 26.Re J, Franich-Ray C, Menahem S, et al. Infant withdrawal following cardiac surgery—treat mother’s distress. Heart Lung Circ. 2011;20:S236. [Google Scholar]
- 27.American Heart Association. [Accessed May 2, 2015];Feeding tips. http://www.heart.org/HEARTORG/Conditions/CongenitalHeartDefects/CareTreatmentforCongenitalHeartDefects/Feeding-Tips_UCM_307735_Article.jsp.