Abstract
The aim of this study is to investigate and compare how 12-weeks of Tai Chi Chuan and Baduanjin exercise can modulate brain structure and memory function in older adults. Magnetic Resonance Imaging(MRI) and memory function measurements (Wechsler Memory Scale-Chinese revised, WMS-CR)were applied at both the beginning and end of the study. Results showed that both Tai Chi Chuan and Baduanjin could significantly increase grey matter volume (GMV) in the insula, medial temporal lobe (MTL), and putamen after 12-weeks of exercise. No significant differences were observed in grey matter volume (GMV) between the Tai Chi Chuan and Baduanjin groups. We also found that compared to healthy controls, Tai Chi Chuan and Baduanjin significantly improved visual reproduction subscores on the WMS-CR. Baduanjin also improved mental control, recognition, touch and comprehension memory subscores of the WMS-CR compared to the control group. Memory quotient (MQ)and visual reproduction subscores were both associated with GMV increases in the putamen and hippocampus. Our results demonstrate the potential of Tai Chi Chuan and Baduanjin exercise for the prevention of memory deficits in older adults.
Keywords: Tai Chi Chuan, Baduanjin, mind-body exercise, memory, aging, voxel-based morphometry
1. Introduction
The average age of the world population is on the rise. By the year 2050, an estimated 21.1% (>2 billion) of the world’s population will be over the age of 60 [1]. As the population grows older, age-related diseases such as cognitive impairment present huge challenges to society [2]. Age-related memory loss, characterized by alterations affecting memory, is very common in older adults [3,4]. Previous studies indicate that memory dysfunctions are some of the first cognitive symptoms in mild cognitive impairment and Alzheimer’s disease (AD) [5].
In addition, previous neuroimaging studies have shown that aging is associated with reductions in brain volume, corticalthickness and white-matter integrity at various brain regions [6]. For instance, in a five-year longitudinal study of structural brain images in older adults, investigators [7] found both cross-sectional and longitudinal declines in brain volume, as well as in brain regions associated with cognition and memory, such as the prefrontal cortex, hippocampus, caudate, and cerebellum. Newberg et al. reported that an 8-week meditation program can improve neuropsychological function such as verbal fluency and logical memory in people with age-associated memory impairment and MCI. Functional neuroimaging changes have also shown significant increases in baseline CBF ratios in the prefrontal, superior frontal, and superior parietal cortices [8]. Additionally, Khalsa et al. demonstrated that Kirtan Kriya (KK), an easy, cost effective meditation technique, can significantly improve memory in people with subjective cognitive decline or mild cognitive impairment [9].
Current pharmaceutical treatments for the prevention of age-related memory and cognitive decline are far from satisfactory [10–12]. For instance, several large epidemiologic studies have failed to find a significant association between the use of nonsteroidal anti-inflammatory drugs and the development of AD [13]. In randomized drug trials in which patients received 25 mg of rofecoxibor placebo daily for up to 4 years, rofecoxib did not exhibit significant benefits in terms of reducing conversion to clinical AD [14]. In addition, it has been reported that a clinical trial on mild cognitive impairment using galantamine was terminated early due to the increased mortality in individuals receiving the experimental drug [15]. Thus, effective pharmacological treatments to prevent aging and cognitive decline are yet to be developed.
As a result, alternative low-cost, non-pharmacological methods are necessary and arising as promising treatments for preventing cognitive decline. Accumulating evidence suggests that physical activity and mental training exercises may decrease the risk of developing age-related memory deficits [10,16–19], as well as increase grey and white matter volume in older adults [16,17,19–24].
Recently, Tai Chi Chuan, a mind-body exercise combining low to moderate intensity slow movements, deep breathing and mental concentration, has drawn the attention of the public and researchers alike [25–27]. Tai Chi Chuan has several components, including physical, cognitive and social, which are believed to aid in maintaining cognition in older adults [28]. In a previous study [29], Zhang and colleagues compared the effects of 18 months of swimming, running, square dancing, and Tai Chi Chuan on cognitive function and emotion in older adults. They found that all of the physical intervention groups showed improvements in cognition and emotion, with the Tai Chi Chuan exercise group demonstrating the most robust effect [30]. Studies have shown that cardiovascular fitness plays an important role in the relationship between exercise and cognition [31]. Erickson and colleagues found that higher fitness levels and physical activity are associated with greater volume of the prefrontal cortex and the hippocampus in older adults [24]. However, Tai Chi Chuan is not acardiovascular exercise, thus the increases in physical activity from practicing Tai Chi Chuan may not be associated with improvements in cognition, and other factors such as social interaction may also play a role in Tai Chi Chuan’s effect on cognitive improvement [30], further supporting the assertion that the beneficial effects of Tai Chi Chuan and physical exercise are due to different underlying mechanisms.
The social component of Tai Chi Chuan, that is, practicing Tai Chi Chuan in a group, also seems to be an important factor in the effectiveness of Tai Chi Chuan on reducing the cognitive aging process [32,33]. A longitudinal population-based study of aging and dementia in Sweden found that social interactions were important for the prevention of cognitive decline [34]. Similarly, in a community-based study, researchers also found that a rich social network had a protective effect against dementia. Compared with married people living with a spouse, single people and those living alone had an increased risk of developing dementia [35].
Despite the individual significance of the social and physical components of Tai Chi Chuan, the multimodal nature of Tai Chi Chuan seems to be crucial in preventing cognitive decline and memory loss [28,36–43]. For instance, Mortimer and colleagues [44] compared the effects of Tai Chi Chuan to walking, social interaction, and no intervention on brain volume and cognition in older adults. They found that after 40 weeks of intervention, significant increases in brain volume were observed in the Tai Chi Chuan and social intervention groups compared to the no intervention group. The Tai Chi group also showed improvements in the Mattis Dementia Rating Scale score, the Trail Making Test (TMT) Parts A and B, the Auditory Verbal Learning Test, and verbal fluency. The social interaction group showed improvements in fewer neuropsychological indices than the Tai Chi group, and no significant differences in improvements were observed between the walking and no intervention groups.
In addition to Tai Chi Chuan, Baduanjin is another popular mind-body exercise [45]. Baduanjin exercise consists of 10 postures (including the beginning and ending posture), and is also a low-intensity exercise that can improve range of motion, strength, and general health [46]. Both Tai Chi Chuan and Baduanjin are considered multi-component interventions that integrate physical, psychosocial, emotional, spiritual, and behavioral elements. The only difference between the two exercises is the complexity; unlike Tai Chi Chuan, Baduanjin involves eight simple fixed movements of the arms with almost no movement of the legs. Due to the simplicity of Baduanjin, at least for beginners, it is easy for individuals to integrate the body movements with other techniques such as breathing.
Memory is a complicated brain function, which involves information encoding, storage and retrieval. Literature suggests that an expansive brain network is involved in different types and aspects of memory [47]. Previous literature demonstrates that mind-body exercises such as Tai Chi Chuan can modulate and improve verbal memory [38], working memory [48], and memory retrieval processes [49]. However, very few studies have investigated if Tai Chi Chuan and Baduanjin can improve global memory function, as well as how these exercises can modulate different subtypes and aspects of memory [30].
In a previous study, we used this dataset to investigate how Tai Chi Chuan and Baduanjin exercise modulates different aspects of cognition and memory using the Wechsler Memory Scale - Chinese Revision (WMS-CR), and resting state functional connectivity changes at the hippocampus [50] and dorsal lateral prefrontal cortex [51]. In this manuscript, we focus on whether Tai Chi Chuan and Baduanjin exercise can modulate different brain structures as measured by voxel-based morphometry (VBM). We also investigate how Tai Chi Chuan and Baduanjin can regulate the WMS-CR subscores, as well as the association between the GMV changes and WMS-CR score changes.
2. Methods
2.1. Study participants
The Ethics Committee of the Affiliated Rehabilitation Hospital, Fujian University of Traditional Chinese Medicine approved all study procedures. The experiment was performed in accordance with approved guidelines. This study was registered in the Chinese Clinical Trial Registry (ChiCTR, http://www.chictr.org, ChiCTR-IPR-15006131). We recruited healthy volunteers aged 50–70 at the Sports Center Community, in Gulou District, Fuzhou City, China. All participants provided written informed consent.
Inclusion criteria for the participants were: (1) 50 to 70 years old; (2) have not participated in regular physical exercise for at least 1 year (regular physical exercise lasting for more than 3 months with a frequency of 3 to 4 times per week and at least 30 minutes per session); (3) right-handed; (4) provided informed consent.
Exclusion criteria were: (1) have a history of stroke; (2) have suffered from severe cerebrovascular disease, musculoskeletal system diseases, or other sports injury related contraindications; (3) score of < 24 on the cognitive screening by the Chinese version of Mini-Mental State Exam (MMSE) [52]; (4) Beck Depression Inventory(BDI-II) [53] scores ≥14.
2.2. Experimental design
Two cohorts of participants were simultaneously and independently recruited from the same community. Printed leaflets, brochures, and community recruitment stations were used to recruit participants. In one cohort, participants were recruited and randomized to the Tai Chi Chuan or control group. In another cohort, participants were recruited and randomized to the Baduanjin or control group. We decided to choose two cohorts of participant to avoid the potential cross practice of Tai Chi Chuan and Baduanjin, so that participants were aware of only one exercise option. The two cohorts started and ended the interventions at the same time. In each cohort, the randomized treatment assignments were sealed in opaque envelopes and were opened individually for each patient who agreed to be in the study. Study staff was blinded to group randomizations.
2.3. Intervention
2.3.1. Tai Chi Chuan exercise group
The Tai Chi Chuan exercise was based on Yang-style 24-form [54]. The participants in the Tai Chi Chuan group received 12-weeks of Tai Chi Chuan exercise training at a frequency of 5 days per week for 60 minutes per day. Each session included: 1) 10 min of warm-up (for example weight shifting, arm swinging, gentle stretches of the neck)and a review of Tai Chi Chuan principles; 2) 30 min of Tai Chi Chuan exercises; 3) 10 min of breathing techniques, and 4) 10 min of relaxation.
2.3.2. Baduanjin exercise group
The training scheme of Baduanjin was in accordance with the Health Qigong - Baduanjin published by the General Administration of Sport of China [55]. The participants in the Baduanjin group received 12-weeks of Baduanjin exercise training at a frequency of 5 days per week for 60 minutes per day. Each session included: 1) 10 min of warm-up (for example arm swinging and gentle stretches of the neck) and a review of Baduanjin principles; 2) 30 min of Baduanjin exercises; 3) 10 min of breathing techniques, and 4) 10 min of relaxation.
Two professional instructors at Fujian University of Traditional Chinese Medicine with more than 5 years of training guided the Tai Chi Chuan and Baduanjin exercises. Participants learned the movements and postures from the instructors. In addition, two staff members were assigned to each training site to monitor participation in the Tai Chi Chuan and Baduanjin exercise training.
2.3.3. Control group
Participants in the control group received basic health education at the start of the study, and were instructed to maintain their original physical activity habits during the following 12-week period. They were also provided free Tai Chi Chuan or Baduanjin training after participation in the study.
2.4. MRI Data Acquisition and analysis
2.4.1. MRI data acquisition
All MRI scans were applied using a 3.0 Tesla GE scanner (General Electric, Milwaukee, WI, USA) with an 8-channel phased-array head coil. The T1-weighted structural images were acquired with a Magnetization-prepared rapid gradient echo sequence (MPRAGE). The scanning parameters were as follows: Echo time (TE) = min, flip angle = 15 degree, slice thickness= 1mm, field of view=240 mm, 164 contiguous slices.
2.4.2. VBM analysis
VBM [56,57] was performed using Statistical Parametric Mapping (SPM12) (Welcome Department of Cognitive Neurology, University College, London, UK) running under a MATLAB suite (Math works, Inc., Natick, Massachusetts). First, all images were checked for artifacts, structural abnormalities and pathologies. Then, the images were segmented into grey matter (GM), white matter and cerebrospinal fluid (CSF), and normalized using the high dimensional DARTEL algorithm [58]. Subsequently, a group specific template was created to reduce variability between participants. The template was then used to normalize the images into the standard Montreal Neurological Institute (MNI) space using the “DARTEL Normalize to MNI Space” program, utilizing the “preserve amount” option to retain the volumetric data of the original images. Finally, spatial smoothing was performed with an isotropic Gaussian kernel of 8mm full-width at half maximum [59,60].
Group analysis was applied using a random effects model. We first compared the pre-treatment regional grey matter volume (GMV) differences between the Tai Chi Chuan, Baduanjin and control groups using a one-way ANOVA. Then we performed second level analyses using a full factorial design module in SPM12 (http://www.fil.ion.ucl.ac.uk/spm/doc/manual.pdf) to explore the differences between the different groups. There were two factors included in the analysis, the first factor had three levels (Tai Chi Chuan group, Baduanjin group and the control group) and the second factor had two levels (pre-treatment and post-treatment). Age (year), gender, and education (year) were also included in the model as covariates. Similar to a previous study [61], an absolute threshold of 0.1 was used for masking. Total intracranial volume was obtained by summing up the overall volumes of GM, white matter, and CSF. A threshold of voxelwise p < 0.001 (uncorrected) and p< 0.05 family-wise error corrected at cluster level was applied for all the analyses.
In addition, to explore the association between the GMV changes, MQ changes and WMS-CR subscore changes that displayed significant differences in the above analyses, we extracted the average GMV values of the significantly overlapped clusters (Tai Chi Chuan vs Control, Baduanjin vs Control) and performed a multiple regression analysis including age, gender, and education as covariates.
2.5. Behavioral outcomes and statistical analysis
Behavioral outcomes were measured with the Wechsler Memory Scale-Chinese Revised (WMS-CR) [62,63]. The WMS-CR is a neuropsychological test that measures an individual’s ability to learn and remember verbal and visual information. It is designed to assess global memory function as measured by memory quotient (MQ), as well as memory function subscores (mental control, picture recognition, visual reproduction, associative learning, touch, comprehension memory, digit span) [63]. In this study, we focused on the subscores of the WMS-CR since the modulation effect of Tai Chi Chuan and Baduanjin on the MQ has been published in a previous study [64].
All measurements were taken at week 0 and week 12, and assessed by two blinded and licensed WMS-CR specialists. In this study, we applied the MQ as a primary behavioral outcome measure, and used the eight subscores of the WMS-CR as secondary outcome measures.
SPSS 18.0 Software (SPSS Inc., Chicago, IL, USA) was applied for data analysis. One-way ANOVA and Chi square tests were used to compare baseline characteristics of the participants among the Tai Chi Chuan, Baduanjin and control groups. During the analysis, we combined all controls from the two cohorts of participants to increase power. ANCOVA analysis was applied to compare the change of the subscores across the three groups respectively. The age (years), gender, and education (years) were also included in the model as covariates. To explore the difference between-groups, the post-hoc analysis (Sidak correct) was applied. We also applied Bonferroni’s correction to adjust the p value for multiple subscore comparisons; a p value of 0.0063(0.05/8) was applied.
3. Results
102 older adults were recruited for this study. Of the 90 participants who passed screening and finished baseline scans, 62 (21 in the Tai Chi Chuan group, 16 in the Baduanjin group, 25 in the control group) completed all study procedures. Four participants dropped out of the Tai Chi Chuan group (1 due to movement, 1 due to contraindications to the MRI scan, 2 due to scheduling conflicts). Nine participants dropped out of the Baduanjin group (8 due to scheduling conflicts, 1 due to contraindications to the MRI scan). Fifteen participants dropped out of the control group (11 due to scheduling conflicts, 4 due to inability to adhere to the second scan). One additional participant in the control group was excluded from the data analysis due to a technical issue during the post-treatment MRI scan. The flowchart of this study can be found in the Supplemental Figure 1. The baseline characteristics of participants who dropped out are shown in supplemental Table 1. There were no significant difference in demographics and baseline memory function between the control and treatment groups among those who were dropped from the study (supplemental Table 1).
To explore whether Tai Chi Chuan and Baduanjin dropouts differed, we re-compared the dropouts with those who were included in the analyses using an independent t-test (supplemental Table 2, Table 3, Table 4). There were no significant differences between the subjects included in the analyses and the dropouts in the Tai Chi Chuan, Baduanjin and control groups in terms of age, gender, education, MQ and the sub-components of memory (mental control, picture, recognition, visual reproduction, associative learning, touch, comprehension memory and digit span) (p<0.05).
3.1. Baseline Characteristics of the Participants
Baseline characteristics and BDI/MMSE scores of included participants are listed in Table 1. There were no significant differences in age, gender, average years of education, MMSE and BDI-II scores between the three groups. The average attendance rates in the Tai Chi Chuan group were 95%, ranging from 88% to 100%. The average attendance rates in the Baduanjin group were 97%, ranging from 92% to 100%. The physical activity of participants in the control group was also orally asked at the end of the study, and no participants reported significant changes in their daily activity.
Table 1.
Demographics of the study participants for PP analysis.
| Characteristics | Control (n=24) | Tai Chi Chuan (n=21) | Baduanjin (n=16) | P value |
|---|---|---|---|---|
| Age(y)* Mean (95%CI) |
60.16(58.28; 62.06) | 62.38(60.31; 64.45) | 62.18(60.16; 64.21) | 0.180 |
| Average years of education(y)* Mean (95%CI) |
8.37(6.83; 9.92) | 9.61(8.24; 11.00) | 9.06(7.67; 10.46) | 0.430 |
| Female n(%)** | 18.00(75.00%) | 13.00(61.90%) | 10.00(62.50%) | 0.580 |
| BDI* Mean (95%CI) |
7.60(6.13;9.07) | 7.19(5.49;8.89) | 8.40(6.50;10.30) | 0.609 |
| MMSE* Mean (95%CI) |
27.20(26.39;28.01) | 27.67(26.79;28.55) | 27.87(27.15;28.59) | 0.485 |
P values were calculated with one-way analysis of variance,
P value was calculated with the use of the chi-square test.
The subscores of the Wechsler Memory Scale (WMS-CR) and general memory function as indicated by the memory quotient (MQ) are shown in Table 2. There were no significant differences between the three groups at baseline (pre-treatment). ANCOVA analysis demonstrated that the Tai Chi Chuan group showed a significant increase in their visual reproduction subscore compared with the control group after Bonferroni correction(0.0063). The Baduanjin group showed significant increases in mental control, recognition, visual reproduction touch, and comprehension memory subscores compared with the control group following Bonferroni correction (0.0063).
Table 2.
Comparison of WMS-CR subscores among the three groups using ANCOVA analysis.
| Characteristics (post-pre) | Tai Chi Chuan (n=21) | Baduanjin (n=16) | Control (n=24) | Tai ChiChuan vs Control | Baduanjin vs Control | Baduanjin vs TaiChi Chuan | |||
|---|---|---|---|---|---|---|---|---|---|
| Mean (SD) | Mean (SD) | Mean (SD) | P | Effect size | P | Effect size | P | Effect size | |
| Mental control | 5.38(5.55) | 7.13(5.10) | 0.00(7.14) | 0.012 | 0.841 | 0.002* | 1.149 | 0.813 | 0.328 |
| Picture | 1.19(3.16) | 2.56(2.37) | 0.13(3.13) | 0.395 | 0.337 | 0.033 | 0.875 | 0.509 | 0.490 |
| Recognition | 2.76(2.77) | 4.00(1.97) | −0.21(3.62) | 0.007 | 0.921 | <0.001* | 1.445 | 0.561 | 0.516 |
| Visual reproduction | 2.33(2.08) | 2.44(3.52) | −0.83(3.32) | 0.001* | 1.141 | 0.001* | 0.956 | 1.000 | 0.038 |
| Associative learning | 0.71(4.26) | 0.00(3.71) | −0.88(3.42) | 0.288 | 0.412 | 0.716 | 0.247 | 0.919 | 0.177 |
| Touch | 0.95(3.22) | 4.75(2.52) | 0.29(3.37) | 0.822 | 0.200 | <0.001* | 1.499 | 0.002* | 1.314 |
| Comprehension memory | 3.14(2.41) | 5.00(2.76) | 1.29(4.51) | 0.066 | 0.512 | 0.001* | 0.992 | 0.361 | 0.718 |
| Digit span | 3.38(3.85) | 2.19(3.51) | 0.25(4.12) | 0.042 | 0.785 | 0.347 | 0.507 | 0.786 | 0.323 |
denotes a significant difference based on corrected Bonferroni’s adjustment of p<0.0063 value.
3.2 VBM analysis results
To explore the baseline difference of GMV, we first applied a comparison between all groups using a one-way ANOVA analysis. No significant differences were observed between the baseline of the Tai Chi Chuan group, Baduanjin group and control group. VBM analysis on GMV changes before and after Tai Chi Chuan and Baduanjin exercise are shown in Table 3. After 12-weeks of the designated exercise, we observed significant GMV increases in the Tai Chi Chuan group compared to the control group at the left insula, left putamen, left parahippocampus/hippocampus, left amygdala, and left inferior temporal. We also found significant GMV increases at the left insula, left hippocampus, left amygdala, bilateral putamen in the Baduanjin group compared to the control group. No significant differences were observed between Tai Chi Chuan and Baduanjin groups.
Table 3.
Regionalgrey matter volume differences between groups (post-treatment - pre-treatment).
| Brain regions | Cluster size | Peak score | MNI peak coordinates(mm) | |||
|---|---|---|---|---|---|---|
| X | Y | Z | ||||
| Tai ChiChuan>Control | Left insula/putamen/parahippocampus/hippocampus/amygdala/inferior temporal gyrus | 1518 | 4.82 | −30 | 2 | −12 |
| Baduanjin>Control | Left insular/hippocampus/Amygdala/putamen | 3912 | 5.33 | −26 | 6 | −5 |
| Right putamen | 1272 | 4.12 | 32 | 5 | −11 | |
| Tai Chi Chuan>Baduanjin | No brain region above the threshold | |||||
| Baduanjin>Tai Chi Chuan | No brain region above the threshold | |||||
| Control>Tai Chi Chuan | No brain region above the threshold | |||||
| Control>Baduanjin | No brain region above the threshold | |||||
L, left; R, right.
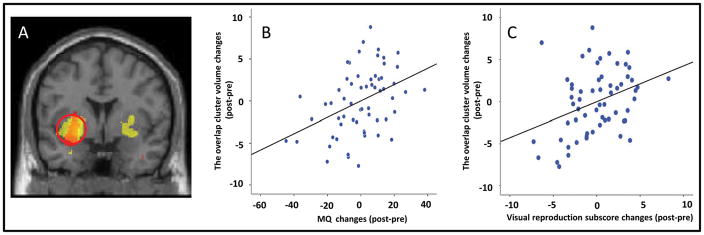
To investigate the association between the GMV changes, MQ changes and WMS-CR visual reproduction subscore changes (the only subscores that showed a significant difference in both Tai Chi Chuan and Baduanjin groups when compared with the control group), we extracted the average GMV values of the significantly overlapped clusters (left putamen and left hippocampus) and performed a multiple regression analysis including age, gender and education as covariates. We found a significant positive association between the GM increase at the overlapped cluster and the corresponding MQ increase (p = 0.002, r=0.406) (Fig 1B)) across all participants. In addition, a significant positive association was found between the GMV increase (left hippocampus and left putamen) and the corresponding visual production subscore increase(p = 0.007, r=0.349) (Fig 1C) across all participants.
Figure 1.
A. Increased gray matter volume in Tai Chi Chuan and Baduanjin groups compared with the control group. Red indicates increased GMV in the Tai Chi Chuan group compared with the control group after 12-weekof training; Yellow indicates increased GMV in theBaduanjin group compared with the control group after 12-weekof training. B. C.Scatter plots show thesignificant association between GMV increases and improvements in MQ scores and visual reproduction corrected for age, gender and education. L: left.
4. Discussion
We investigated the modulation effect of 12-weeks of Tai Chi Chuan and Baduanjin exercise on GMV, and differenttypes and aspects of memory. The results showed that compared with the control group, both Tai Chi Chuan and Baduanjingroups showed significantly increased GMV at the medial temporal lobe (MTL), putamen, and insula. We also found that both Tai Chi Chuan and Baduanjin improved the visual reproduction subscore compared with the control group, and Baduanjin also improved mental control, recognition, touch and comprehension memory subscores compared with the control group. Finally, we found a positive association between memory improvement and GMV increases at the left putamen and hippocampus across all participants.
In this study, we found significant GMV increases at the left medial temporal lobe (MTL), including the parahippocampus, hippocampus, and amygdala afterTai Chi Chuan and Baduanjin practice. The MTL, including the hippocampus and adjacent parahippocampal, perirhinal, and entorhinal cortices, are vital for memory processing [65–68]. Studies suggest that the MTL is involved in the retrieval and encoding of memory [69]. A number of brain imaging studies have also shown that age-related memory deficits often a result of a loss of MTL volume [70–72]. Studies suggest that a decrease in grey matter volume in the MTL may contribute to subsequent cognitive decline and conversion from mild cognitive impairment to AD [73], and that the preservation of GMV may be important for maintaining memory function [67].
In a previous study, Bugg and colleagues found that low levels of exercise were associated with age-related decreases in the volume of the MTL, while higher levels of exercise were associated with greater superior frontal lobe volume in older adults [74]. Erickson and colleagues found that after one year of moderate-intensity exercise(3 days/week), individual’s spatial memory and hippocampal volume significantly increased as compared with the control group [16]. Niemannand colleagues found that increases in motor fitness and regular exercise increased hippocampal volume in older adults [75]. As a further support of our findings, we found that Tai Chi Chuan exercise significantly enhanced the resting state functional connectivity between the hippocampus and medial prefrontal cortex (mPFC) [76]. Li and colleagues also found that a multimodal intervention including cognitive training, Tai Chi Chuan exercise, and group counseling improved the resting-state connectivity between the mPFC and MTL[77].
We also found that the left parahippocampal volume increased in the Tai Chi Chuan group compared to the control group. Previous studies showed that the parahippocampal cortex is associated with many cognitive processes, including visuospatial processing and episodic memory [78]. Our results are consistent with these previous findings [79], which found that compared with controls, long-term Tai Chi Chuan practitioners (average 14 years of exercise) showed significantly thicker cortices in the temporal gyrus relative to the control group.
Significant GMV increases in the putamen were observed in both Tai Chi Chuan and Baduanjin groups as compared with the control group. Accumulating evidence suggests the role of the putamen in movement related functions [80–82], executive functions, working memory[83,84], and the learning of associations between stimuli, responses, and outcomes. The contribution of the putamen in cognition may be due to the existence of circuits connecting the basal ganglia to non-motor regions in the frontal lobe[85]that are associated with a variety of cognitive functions [86]. In our study, we found a positive correlation between GMV changes in the putamen and both the MQ and visual reproduction subscore changes after12-weeks of Tai Chi Chuan and Baduanjin practice. We speculate that the putamen may play a key role linking mind-body exercises to improve cognitive function. Specifically, we speculate Tai Chi Chuan and Baduanjin may first modulate the motor related network of the putamen, then strengthen the circuits connecting the putamen to memory related regions such as frontal lobe.
We also found GMV increases in the insula after Tai Chi Chuan and Baduanjin exercise. The insula is a brain structure involved in cognitive, affective, and regulatory functions, including interceptive awareness and emotional responses [87,88]. Studies report that the insula is a crucial hub of many human brain networks that play important roles in memory processes [89,90]. Tang and colleagues [91] found that five days of integrative body mind training increased brain activity in the ventral left insula, anterior cingulate cortex, and striatum. Previous studies showed that both yoga [92], meditation [93,94] and physical exercise[95,96] may also increasecortical thickness of the insula [97–99]. Our result is consistent with these previous findings suggesting an important role of the insula in the modulation effect of Tai Chi Chuan and Baduanjin exercise.
In this study, we found 12-weeks of both Tai Chi Chuan and Baduanjin practice (5 days/per week) increased MTL volume, although there was no significant difference between the two. Despite this, the GMV increase evoked by Baduanjin was more expansive. This result is also consistent with the behavioral outcomes, i.e. both Tai Chi Chuan and Baduanjin improved the visual reproduction subscore compared with the control group, but Baduanjin also improved mental control, recognition, touch and comprehension memory subscores compared with controls. We speculate this may due to the fact that the Tai Chi Chuan is a complicated exercise, and therefore 12-weeksof intervention may not be a sufficient amount oftime to demonstrate all of the positive effects of Tai Chi Chuan exercise in Tai Chi Chuan naïve older adults. Longer trials with a larger sample size are needed to test this hypothesis.
Since both Tai chi and Baduanjin focus on the body positions during exercise, we hypothesize they will be efficient in improving spatial related memory function, as demonstrated by the significant improvement in visual reproduction subscores. Nevertheless, our results also suggest the two may work through multiple mechanisms related to the mind-body interaction including meditation, exercise, and social interaction [100–102], the mechanisms underlying Tai Chi Chuan and Baduanjin exercise may differ. Compared with Tai Chi Chuan which requires a considerable degree of dynamic balance and complexity, Baduanjin exercise is much simpler, therefore, it is easier for participants to concentrate on the coordination of both the body and mind. Due to their low physical intensity, both are well suited for older adults that have been advised not to participate in intense exercise. However, Baduanjin may be more appropriate for those with cognitive impairment due to its relative simplicity.
There are several limitations in this study. First, the sample size was relatively small, therefore a future study with a larger sample size is needed to further confirm the findings of our study. Secondly, both Tai Chi Chuan and Baduanjin are considered mind-body exercises. We do not know whether physical activity, mental exercise, or a combination of the two are crucial for memory improvement and brain volume changes in the Tai Chi Chuan and Baduanjin groups. Literature suggests that both body and mind exercises are important, and our study corroborates with these claims. In a previous study, Erickson and colleagues [16] found significant hippocampal volume increases and spatial memory improvements after one year of exercise. Our study showed that 12-weeks of Tai Chi Chuan and Baduanjin exercise can significantly improve memory function and increase GMV in the MTL. We speculate that the combination of physical activity and mental exercise could be more effective than physical activity or mental exercise alone. Future studies investigating the effects of exercise, meditation, Tai Chi Chuan and Baduanjin separately are needed. Finally, we only used basic health education as a control. A more comparable control condition such as a mild to moderate exercise regimen may be needed to validate our findings.
In summary, we found that 12-weeks of intensive group Tai Chi Chuan or Baduanjin exercise can modulate global memory, as well as improve specific types and aspects of memory function. The brain mechanisms underlying the effects of both Tai Chi Chuan and Baduanjin seem to be slightly different, although both increase GMV at the MTL, putamen and insular, which are regions essential for memory and cognition. Our results imply that Tai Chi Chuan and Baduanjin might be effective methods for delay in memory decline.
Supplementary Material
Acknowledgments
This scientific work was supported by the Special Scientific Research Fund of Public Welfare Profession of China (Grant No. 201307004), Ministry of Science and Technology and Ministry of Finance of the People’s Republic of China to Jing Tao, Fujian Rehabilitation Tech Co-innovation Center (Grant No. X2012007-Collaboration) to Jing Tao. It is also supported by National Rehabilitation Research Center of Traditional Chinese Medicine, Fujian provincial rehabilitation industrial institution. Jian Kong is supported by R01AT006364, R01 R01AT008563, R21AT008707, and P01 AT006663 from NIH/NCCIH.
Footnotes
Disclosure statement
All authors declare no conflict of interest.
References
- 1.Sander M, Oxlund B, Jespersen A, Krasnik A, Mortensen EL, Westendorp RGJ, Rasmussen LJ. The challenges of human population ageing. Age Ageing. 2015;44:185–187. doi: 10.1093/ageing/afu189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Heese K. Ageing, dementia and society - an epistemological perspective. Springerplus. 2015;4:135. doi: 10.1186/s40064-015-0910-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vera-Cuesta H, Vera-Acosta H, Leon-Benito O, Fernandez-Maderos I. Prevalence and risk factors of age-related memory disorder in a health district. Rev Neurol. 2006;43:137–142. [PubMed] [Google Scholar]
- 4.Wang M, Gamo NJ, Yang Y, Jin LE, Wang X-J, Laubach M, Mazer JA, Lee D, Arnsten AFT. Neuronal basis of age-related working memory decline. Nature. 2011;476:210–3. doi: 10.1038/nature10243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McKhann G, Knopman DS, Chertkow H, Hymann B, Jack CR, Kawas C, Klunk W, Koroshetz W, Manly J, Mayeux R, Mohs R, Morris J, Rossor M, Scheltens P, Carrillo M, Weintrub S, Phelphs C. The diagnosis of dementia due to Alzheimer’s disease: Recommendations from the National Institute on Aging- Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011;7:263–269. doi: 10.1016/j.jalz.2011.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Goh JO, Park DC. Neuroplasticity and cognitive aging: The scaffolding theory of aging and cognition. Restor Neurol Neurosci. 2009;27:391–403. doi: 10.3233/RNN-2009-0493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Raz N, Lindenberger U, Rodrigue KM, Kennedy KM, Head D, Williamson A, Dahle C, Gerstorf D, Acker JD. Regional brain changes in aging healthy adults: General trends, individual differences and modifiers. Cereb Cortex. 2005;15:1676–1689. doi: 10.1093/cercor/bhi044. [DOI] [PubMed] [Google Scholar]
- 8.Newberg AB, Wintering N, Khalsa DS, Roggenkamp H, Waldman MR. Meditation effects on cognitive function and cerebral blood flow in subjects with memory loss: a preliminary study. J Alzheimers Dis. 2010;20:517–26. doi: 10.3233/JAD-2010-1391. [DOI] [PubMed] [Google Scholar]
- 9.Khalsa DS. Stress, meditation, and Alzheimer’s disease prevention: Where the evidence stands. J Alzheimer’s Dis. 2015;48:1–12. doi: 10.3233/JAD-142766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gard T, Hölzel BK, Lazar SW. The potential effects of meditation on age-related cognitive decline: A systematic review. Ann N Y Acad Sci. 2014;1307:89–103. doi: 10.1111/nyas.12348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gaitán Ab, Garolera Mbc, Cerulla Nd, Chico Gd, Rodriguez-Querol M, Canela-Soler Jf. Efficacy of an adjunctive computer-based cognitive training program in amnestic mild cognitive impairment and Alzheimer’s disease: A single-blind, randomized clinical trial. Int J Geriatr Psychiatry. 2013;28:91–99. doi: 10.1002/gps.3794. [DOI] [PubMed] [Google Scholar]
- 12.Newberg AB, Wintering N, Khalsa DS, Roggenkamp H, Waldman MR. Meditation effects on cognitive function and cerebral blood flow in subjects with memory loss: a preliminary study. J Alzheimers Dis. 2010;20:517–26. doi: 10.3233/JAD-2010-1391. [DOI] [PubMed] [Google Scholar]
- 13.Etminan M, Gill S, Samii A. Effect of non-steroidal anti-inflammatory drugs on risk of Alzheimer’s disease: systematic review and meta-analysis of observational studies. BMJ. 2003;327:128. doi: 10.1136/bmj.327.7407.128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Thal LJ, Ferris SH, Kirby L, Block Ga, Lines CR, Yuen E, Assaid C, Nessly ML, Norman Ba, Baranak CC, Reines Sa. A randomized, double-blind, study of rofecoxib in patients with mild cognitive impairment. Neuropsychopharmacology. 2005;30:1204–15. doi: 10.1038/sj.npp.1300690. [DOI] [PubMed] [Google Scholar]
- 15.National Institute for Health and Clinical Excellence. Donepezil, galantamine, rivastigmine, and memantine for the treatment of Alzheimer’s Disease. Natl Inst Heal Clin Excell. 2011:1–84. [Google Scholar]
- 16.Erickson KI, Voss MW, Prakash RS, Basak C, Szabo A, Chaddock L, Kim JS, Heo S, Alves H, White SM, Wojcicki TR, Mailey E, Vieira VJ, Martin Sa, Pence BD, Woods Ja, McAuley E, Kramer AF. Exercise training increases size of hippocampus and improves memory. Proc Natl Acad Sci U S A. 2011;108:3017–3022. doi: 10.1073/pnas.1015950108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Makizako H, Shimada H, Doi T, Park H, Yoshida D, Suzuki T. Six-minute walking distance correlated with memory and brain volume in older adults with mild cognitive impairment: a voxel-based morphometry study. Dement Geriatr Cogn Dis Extra. 2013;3:223–32. doi: 10.1159/000354189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Killgore WDS, Olson EA, Weber M. Physical exercise habits correlate with gray matter volume of the hippocampus in healthy adult humans. Sci Rep. 2013;3:3457. doi: 10.1038/srep03457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Varma VR, Chuang Y-F, Harris GC, Tan EJ, Carlson MC. Low-intensity daily walking activity is associated with hippocampal volume in older adults. Hippocampus. 2014 doi: 10.1002/hipo.22397. i, n/a-n/a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Voss MW, Heo S, Prakash RS, Erickson KI, Alves H, Chaddock L, Szabo AN, MaileyWójcicki ELRT, White SM, Gothe N, Edward McAuley BPS, Krame AF. The influence of aerobic fitness on cerebral white matter integrity and cognitive function in older adults: Results of a one- year exercise intervention. 2013;34:2972–2985. doi: 10.1002/hbm.22119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hayes SM, Hayes JP, Cadden M, Verfaellie M. A review of cardiorespiratory fitness-related neuroplasticity in the aging brain. Front Aging Neurosci. 2013;5:31. doi: 10.3389/fnagi.2013.00031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Xu J, Vik A, Groote IR, Lagopoulos J, Holen A, Ellingsen O, Håberg AK, Davanger S. Nondirective meditation activates default mode network and areas associated with memory retrieval and emotional processing. Front Hum Neurosci. 2014;8:86. doi: 10.3389/fnhum.2014.00086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yin S, Zhu X, Li R, Niu Y, Wang B, Zheng Z, Huang X, Huo L, Li J. Intervention-induced enhancement in intrinsic brain activity in healthy older adults. Sci Rep. 2014;4:7309. doi: 10.1038/srep07309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Erickson KI, Leckie RL, Weinstein AM. Physical activity, fitness, and gray matter volume. Neurobiol Aging. 2014;35(Suppl 2):S20–8. doi: 10.1016/j.neurobiolaging.2014.03.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Club J. A Randomized Trial of Tai Chi for Fibromyalgia 1. N Engl J Med. 2010;1:743–754. doi: 10.1056/NEJMoa0912611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yeh GY, Wang C, Wayne PM, Phillips RS. The effect of Tai Chi exercise on blood pressure: A systematic review. Prev Cardiol. 2008;11:82–89. doi: 10.1111/j.1751-7141.2008.07565.x. [DOI] [PubMed] [Google Scholar]
- 27.Wang C, Schmid CH, Rones R, Kalish R, Yinh J, Goldenberg DL, Lee Y, McAlindon T. A randomized trial of tai chi for fibromyalgia. N Engl J Med. 2010;363:743–54. doi: 10.1056/NEJMoa0912611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chang JY, Tsai PF, Beck C, Hagen JL, Huff DC, Anand KJ, Roberson PK, Rosengren KSBL. The effect of tai chi on cognition in elders with cognitive impairment. Medsurg Nurs. 2011;20:63–70. [PMC free article] [PubMed] [Google Scholar]
- 29.Zhang X, Ni X, Chen P. Study about the effects of different fitness sports on cognitive function and emotion of the aged. Cell Biochem Biophys. 2014;70:1591–6. doi: 10.1007/s12013-014-0100-8. [DOI] [PubMed] [Google Scholar]
- 30.Fong D-Y, Chi L-K, Li F, Chang Y-K. The benefits of endurance exercise and Tai Chi Chuan for the task-switching aspect of executive function in older adults: an ERP study. Front Aging Neurosci. 2014;6:1–11. doi: 10.3389/fnagi.2014.00295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kramer aF, Hahn S, Cohen NJ, Banich MT, McAuley E, Harrison CR, Chason J, Vakil E, Bardell L, Boileau Ra, Colcombe a. Ageing, fitness and neurocognitive function. Nature. 1999;400:418–419. doi: 10.1038/22682. [DOI] [PubMed] [Google Scholar]
- 32.Yau MK. Tai Chi exercise and the improvement of health and well-being in older adults. Med Sport Sci. 2008;52:155–165. doi: 10.1159/000134296. [DOI] [PubMed] [Google Scholar]
- 33.Matthews MM, Williams HG. Can Tai chi enhance cognitive vitality? A preliminary study of cognitive executive control in older adults after A Tai chi intervention. J S C Med Assoc. 2008;104:255–7. [PubMed] [Google Scholar]
- 34.Wang H-X. Late-Life Engagement in Social and Leisure Activities Is Associated with a Decreased Risk of Dementia: A Longitudinal Study from the Kungsholmen Project. Am J Epidemiol. 2002;155:1081–1087. doi: 10.1093/aje/155.12.1081. [DOI] [PubMed] [Google Scholar]
- 35.Fratiglioni L, Wang HX, Ericsson K, Maytan M, Winblad B. Influence of social network on occurrence of dementia: a community-based longitudinal study. Lancet. 2000;355:1315–9. doi: 10.1016/S0140-6736(00)02113-9. [DOI] [PubMed] [Google Scholar]
- 36.Fong DY, Chi LK, Li F, Chang YK. The benefits of endurance exercise and Tai Chi Chuan for the task-switching aspect of executive function in older adults: An ERP study. Front Aging Neurosci. 2014;6 doi: 10.3389/fnagi.2014.00295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wells RE, Phillips RS, Schachter SC, McCarthy EP. Complementary and alternative medicine use among US adults with common neurological conditions. J Neurol. 2010;257:1822–1831. doi: 10.1007/s00415-010-5616-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chan AS, Ho YC, Cheung MC, Albert MS, Chiu HFK, Lam LCW. Association between mind-body and cardiovascular exercises and memory in older adults. J Am Geriatr Soc. 2005;53:1754–1760. doi: 10.1111/j.1532-5415.2005.53513.x. [DOI] [PubMed] [Google Scholar]
- 39.Lam LCW, Chau RCM, Wong BML, Fung AWT, Tam CWC, Leung GTY, Kwok TCY, Leung TYS, Ng SP, Chan WM. A 1-Year Randomized Controlled Trial Comparing Mind Body Exercise (Tai Chi) With Stretching and Toning Exercise on Cognitive Function in Older Chinese Adults at Risk of Cognitive Decline. J Am Med Dir Assoc. 2012;13 doi: 10.1016/j.jamda.2012.03.008. [DOI] [PubMed] [Google Scholar]
- 40.Tsai P-F, Chang JY, Beck C, Kuo Y-F, Keefe FJ. A pilot cluster-randomized trial of a 20-week Tai Chi program in elders with cognitive impairment and osteoarthritic knee: effects on pain and other health outcomes. Pain Symptom Manag. 2013;45:660–669. doi: 10.1016/j.jpainsymman.2012.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wayne PM, Walsh JN, Taylor-Piliae RE, Wells RE, Papp KV, Donovan NJ, Yeh GY. Effect of tai chi on cognitive performance in older adults: Systematic review and meta-analysis. J Am Geriatr Soc. 2014;62:25–39. doi: 10.1111/jgs.12611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Zheng G, Lan X, Li M, Ling K, Lin H, Chen L, Tao J, Li J, Zheng X, Chen B, Fang Q. Effectiveness of Tai Chi on physical and psychological health of college students: Results of a randomized controlled trial. PLoS One. 2015;10 doi: 10.1371/journal.pone.0132605. no pagination. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Chang YK, Nien YH, Tsai CL, Etnier JL. Physical activity and cognition in older adults: The potential of Tai Chi Chuan. J Aging Phys Act. 2010;18:451–472. doi: 10.1123/japa.18.4.451. [DOI] [PubMed] [Google Scholar]
- 44.Mortimer JA, Ding D, Borenstein AR, Decarli C, Guo Q, Wu Y, Zhao Q, Chu S. Changes in brain volume and cognition in a randomized trial of exercise and social interaction in a community-based sample of non-demented chinese elders. J Alzheimer’s Dis. 2012;30:757–766. doi: 10.3233/JAD-2012-120079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Li M, Fang Q, Li J, Zheng X, Tao J, Yan X, Lin Q, Lan X, Chen B, Zheng G, Chen L. The effect of Chinese traditional exercise-Baduanjin on physical and psychological well-being of college students: A randomized controlled trial. PLoS One. 2015;10 doi: 10.1371/journal.pone.0130544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Zheng G, Huang M, Li S, Li M, Xia R, Zhou W, Tao J, Chen L. Effect of Baduanjin exercise on cognitive function in older adults with mild cognitive impairment: study protocol for a randomised controlled trial. BMJ Open. 2016;6:e010602. doi: 10.1136/bmjopen-2015-010602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Miyashita Y. Cognitive memory: cellular and network machineries and their top-down control. Science. 2004;306:435–440. doi: 10.1126/science.1101864. [DOI] [PubMed] [Google Scholar]
- 48.Kim THM, Pascual-Leone J, Johnson J, Tamim H. The mental-attention Tai Chi effect with older adults. BMC Psychol. 2016;4:29. doi: 10.1186/s40359-016-0137-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Tsang WWN, Kwok JCY, Hui-Chan CWY. Effects of aging and Tai Chi on a finger-pointing task with a choice paradigm. Evidence-based Complement Altern Med. 2013;2013 doi: 10.1155/2013/653437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Tao Jing, Jiao Liu NE. increased hippocampus–Medial Prefrontal cortex resting-state Functional connectivity and Memory Function after Tai chi chuan Practice in elder adults. Front Aging Neurosci. 2016;8:1–9. doi: 10.3389/fnagi.2016.00025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Tao J. Tai Chi Chuan and Baduanjin practice modulates functional connectivity of the cognitive control network in older adults. Sci Rep. 2017 doi: 10.1038/srep41581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Zhang MY, Katzman R, Salmon D, Jin H, Cai GJ, Wang ZY, Qu GY, Grant I, Yu E, Levy P. The prevalence of dementia and Alzheimer’s disease in Shanghai, China: impact of age, gender, and education. Ann Neurol. 1990;27:428–37. doi: 10.1002/ana.410270412. [DOI] [PubMed] [Google Scholar]
- 53.Beck A, Steer R, Brown G. BDI-II, Beck depression inventory: manual 1996 [Google Scholar]
- 54.China National Sports Commission. Simplified Taijiquan. 1983. [Google Scholar]
- 55.Health Qigong Management Center of General Administration of Sport of China. Health qigong--Baduanjin. People’s Sports Publishing House of China; Beijing: 2003. [Google Scholar]
- 56.Ashburner J, Friston KJ. Voxel-based morphometry--the methods. Neuroimage. 2000;11:805–821. doi: 10.1006/nimg.2000.0582. [DOI] [PubMed] [Google Scholar]
- 57.Good CD, Johnsrude IS, Ashburner J, Henson RN, Friston KJ, Frackowiak RS. A voxel-based morphometric study of ageing in 465 normal adult human brains. Neuroimage. 2001;14:21–36. doi: 10.1006/nimg.2001.0786. [DOI] [PubMed] [Google Scholar]
- 58.Ashburner J. A fast diffeomorphic image registration algorithm. Neuroimage. 2007;38:95–113. doi: 10.1016/j.neuroimage.2007.07.007. [DOI] [PubMed] [Google Scholar]
- 59.Grabe HJ, Wittfeld K, Hegenscheid K, Hosten N, Lotze M, Janowitz D, Völzke H, John U, Barnow S, Freyberger HJ. Alexithymia and brain gray matter volumes in a general population sample. Hum Brain Mapp. 2014;35:5932–5945. doi: 10.1002/hbm.22595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Van der Velde J, Van Tol MJ, Goerlich-Dobre KS, Gromann PM, Swart M, De Haan L, Wiersma D, Bruggeman R, Krabbendam L, Aleman A. Dissociable morphometric profiles of the affective and cognitive dimensions of alexithymia. Cortex. 2014;54:190–199. doi: 10.1016/j.cortex.2014.02.017. [DOI] [PubMed] [Google Scholar]
- 61.Kalmady SV, Venkatasubramanian G, Shivakumar V, Gautham S, Subramaniam A, Jose DA, Maitra A, Ravi V, Gangadhar BN. Relationship between interleukin-6 gene polymorphism and hippocampal volume in antipsychotic-naïve schizophrenia: Evidence for differential susceptibility? PLoS One. 2014;9 doi: 10.1371/journal.pone.0096021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Wechsler D. Wechsler Memory Scale-Revised. Psychological Corporation; New York: 1987. [Google Scholar]
- 63.Gong Y, wang Dj. Handbook of Wechsler Memory Scale-Revised. Changsha; China: 1989. [Google Scholar]
- 64.Tao J, Liu J, Egorova N, Chen X, Sun S, Xue X, Huang J, Zheng G, Wang Q, Chen L, Kong J. Increased hippocampus-medial prefrontal cortex resting-state functional connectivity and memory function after Tai Chi Chuan practice in elder adults. Front Aging Neurosci. 2016;8 doi: 10.3389/fnagi.2016.00025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Pergola G, Suchan B. Associative learning beyond the medial temporal lobe: many actors on the memory stage. Front Behav Neurosci. 2013;7:162. doi: 10.3389/fnbeh.2013.00162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Lech RK, Suchan B. The medial temporal lobe: Memory and beyond. Behav Brain Res. 2013;254:45–49. doi: 10.1016/j.bbr.2013.06.009. [DOI] [PubMed] [Google Scholar]
- 67.Wixted JT, Squire LR. The medial temporal lobe and the attributes of memory. Trends Cogn Sci. 2011;15:210–217. doi: 10.1016/j.tics.2011.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Sidhu MK, Stretton J, Winston GP, McEvoy AW, Symms M, Thompson PJ, Koepp MJ, Duncan JS. Memory network plasticity after temporal lobe resection: A longitudinal functional imaging study. Brain. 2016;139:415–430. doi: 10.1093/brain/awv365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Takehara-Nishiuchi K, McNaughton BL. Spontaneous changes of neocortical code for associative memory during consolidation. Science. 2008;960:960–963. doi: 10.1126/science.1161299. [DOI] [PubMed] [Google Scholar]
- 70.Head D, Rodrigue KM, Kennedy KM, Raz N. Neuroanatomical and cognitive mediators of age-related differences in episodic memory. Neuropsychology. 2008;22:491–507. doi: 10.1037/0894-4105.22.4.491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Ward AM, Mormino EC, Huijbers W, Schultz AP, Hedden T, Sperling RA. Relationships between default-mode network connectivity, medial temporal lobe structure, and age-related memory deficits. Neurobiol Aging. 2015;36:265–272. doi: 10.1016/j.neurobiolaging.2014.06.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Rajah MN, Kromas M, Han JE, Pruessner JC. Group differences in anterior hippocampal volume and in the retrieval of spatial and temporal context memory in healthy young versus older adults. Neuropsychologia. 2010;48:4020–4030. doi: 10.1016/j.neuropsychologia.2010.10.010. [DOI] [PubMed] [Google Scholar]
- 73.Ferreira LK, Diniz BS, Forlenza OV, Busatto GF, Zanetti MV. Neurostructural predictors of Alzheimer’s disease: a meta-analysis of VBM studies. Neurobiol Aging. 2011;32:1733–41. doi: 10.1016/j.neurobiolaging.2009.11.008. [DOI] [PubMed] [Google Scholar]
- 74.Bugg JM, Head D. Exercise moderates age-related atrophy of the medial temporal lobe. Neurobiol Aging. 2011;32:506–514. doi: 10.1016/j.neurobiolaging.2009.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Niemann C, Godde B, Voelcker-Rehage C. Not only cardiovascular, but also coordinative exercise increases hippocampal volume in older adults. Front Aging Neurosci. 2014;6:1–24. doi: 10.3389/fnagi.2014.00170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Tao J, Liu J, Egorova N, Chen X, Sun S, Xue X, Huang J, Zheng G, Wang Q, Chen L, Kong J. Increased hippocampus–medial prefrontal cortex resting state functional connectivity and memory function after Tai Chi Chuan practice in elder adults. Front Aging Neurosci. 2016 doi: 10.3389/fnagi.2016.00025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Li R, Zhu X, Yin S, Niu Y, Zheng Z, Huang X, Wang B, Li J. Multimodal intervention in older adults improves resting-state functional connectivity between the medial prefrontal cortex and medial temporal lobe. Front Aging Neurosci. 2014;6:39. doi: 10.3389/fnagi.2014.00039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Kinnavane L, Amin E, Horne M, Aggleton JP. Mapping parahippocampal systems for recognition and recency memory in the absence of the rat hippocampus. Eur J Neurosci. 2014;40:3720–34. doi: 10.1111/ejn.12740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Wei GX, Xu T, Fan FM, Dong HM, Jiang LL, Li HJ, Yang Z, Luo J, Zuo XN. Can Taichi Reshape the Brain? A Brain Morphometry Study. PLoS One. 2013;8 doi: 10.1371/journal.pone.0061038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Lorey B, Pilgramm S, Bischoff M, Stark R, Vaitl D, Kindermann S, Munzert J, Zentgraf K. Activation of the Parieto-Premotor Network Is Associated with Vivid Motor Imagery—A Parametric fMRI Study. PLoS One. 2011;6:e20368. doi: 10.1371/journal.pone.0020368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Kovács G, Raabe M, Greenlee MW. Neural correlates of visually induced self-motion illusion in depth. Cereb Cortex. 2008;18:1779–1787. doi: 10.1093/cercor/bhm203. [DOI] [PubMed] [Google Scholar]
- 82.Cairo TA, Liddle PF, Woodward TS, Ngan ETC. The influence of working memory load on phase specific patterns of cortical activity. Cogn Brain Res. 2004;21:377–387. doi: 10.1016/j.cogbrainres.2004.06.014. [DOI] [PubMed] [Google Scholar]
- 83.Sefcsik T, Nemeth D, Janacsek K, Hoffmann I, Scialabba J, Klivenyi P, Ambrus GG, Haden G, Vecsei L. The role of the putamen in cognitive functions — A case study. Learn Percept. 2011;1:215–227. [Google Scholar]
- 84.Arsalidou M, Duerden EG, Taylor MJ. The centre of the brain: Topographical model of motor, cognitive, affective, and somatosensory functions of the basal ganglia. Hum Brain Mapp. 2013;34:3031–3054. doi: 10.1002/hbm.22124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Middleton Fa, Strick PL. Basal-ganglia “projections” to the prefrontal cortex of the primate. Cereb Cortex. 2002;12:926–935. doi: 10.1093/cercor/12.9.926. [DOI] [PubMed] [Google Scholar]
- 86.Stuss DTKRT. Principles of frontal lobe function. Oxford University Press; 2013. [Google Scholar]
- 87.Craig ADB. How do you feel — now? The anterior insula and human awareness. 2009;10 doi: 10.1038/nrn2555. [DOI] [PubMed] [Google Scholar]
- 88.Menon V, Uddin LQ. Saliency, switching, attention and control: a network model of insula function. Brain Struct Funct. 2010;214:655–67. doi: 10.1007/s00429-010-0262-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Levens SM, Phelps EA. Insula and orbital frontal cortex activity underlying emotion interference resolution in working memory. J Cogn Neurosci. 2010;22:2790–2803. doi: 10.1162/jocn.2010.21428. [DOI] [PubMed] [Google Scholar]
- 90.Xie C, Bai F, Yu H, Shi Y, Yuan Y, Chen G, Li W, Chen G, Zhang Z, Li S-J. Abnormal insula functional network is associated with episodic memory decline in amnestic mild cognitive impairment. Neuroimage. 2012;63:320–7. doi: 10.1016/j.neuroimage.2012.06.062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Tang Y-Y, Ma Y, Fan Y, Feng H, Wang J, Feng S, Lu Q, Hu B, Lin Y, Li J, Zhang Y, Wang Y, Zhou L, Fan M. Central and autonomic nervous system interaction is altered by short-term meditation. Proc Natl Acad Sci U S A. 2009;106:8865–70. doi: 10.1073/pnas.0904031106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Villemure C, Čeko M, Cotton VA, Bushnell MC. Neuroprotective effects of yoga practice: age-, experience-, and frequency-dependent plasticity. Front Hum Neurosci. 2015;9:281. doi: 10.3389/fnhum.2015.00281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Froeliger BE, Garland EL, Modlin La, McClernon FJ. Neurocognitive correlates of the effects of yoga meditation practice on emotion and cognition: a pilot study. Front Integr Neurosci. 2012;6:48. doi: 10.3389/fnint.2012.00048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Hölzel BK, Carmody J, Vangel M, Congleton C, Yerramsetti SM, Gard T, Lazar SW. Mindfulness practice leads to increases in regional brain gray matter density. Psychiatry Res. 2011;191:36–43. doi: 10.1016/j.pscychresns.2010.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Peters J, Dauvermann M, Mette C, Platen P, Franke J, Hinrichs T, Daum I. Voxel-based morphometry reveals an association between aerobic capacity and grey matter density in the right anterior insula. Neuroscience. 2009;163:1102–1108. doi: 10.1016/j.neuroscience.2009.07.030. [DOI] [PubMed] [Google Scholar]
- 96.Rayhan RU, Stevens BW, Raksit MP, Ripple Ja, Timbol CR, Adewuyi O, VanMeter JW, Baraniuk JN. Exercise challenge in Gulf War Illness reveals two subgroups with altered brain structure and function. PLoS One. 2013;8:e63903. doi: 10.1371/journal.pone.0063903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Eyre HA, Acevedo B, Yang H, Siddarth P, Van Dyk K, Ercoli L, Leaver AM, Cyr NS, Narr K, Baune BT, Khalsa DS, Lavretsky H. Changes in Neural Connectivity and Memory Following a Yoga Intervention for Older Adults: A Pilot Study. J Alzheimer’s Dis. 2016;52:673–684. doi: 10.3233/JAD-150653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Innes KE, Selfe TK. Meditation as a therapeutic intervention for adults at risk for Alzheimer’s disease—Potential benefits and underlying mechanisms. Front Psychiatry. 2014;5 doi: 10.3389/fpsyt.2014.00040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Innes KE, Selfe TK, Khalsa DS, Kandati S. Effects of Meditation versus Music Listening on Perceived Stress, Mood, Sleep, and Quality of Life in Adults with Early Memory Loss: A Pilot Randomized Controlled Trial. J Alzheimer’s Dis. 2016;52:1277–1298. doi: 10.3233/JAD-151106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Kang D-H, Jo HJ, Jung WH, Kim SH, Jung Y-H, Choi C-H, Lee US, An SC, Jang JH, Kwon JS. The effect of meditation on brain structure: cortical thickness mapping and diffusion tensor imaging. Soc Cogn Affect Neurosci. 2013;8:27–33. doi: 10.1093/scan/nss056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Wells RE, Yeh GY, Kerr CE, Wolkin J, Davis RB, Tan Y, Spaeth R, Wall RB, Walsh J, Kaptchuk TJ, Press D, Phillips RS, Kong J. Meditation’s impact on default mode network and hippocampus in mild cognitive impairment: a pilot study. Neurosci Lett. 2013;556:15–9. doi: 10.1016/j.neulet.2013.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Hölzel BK, Ott U, Gard T, Hempel H, Weygandt M, Morgen K, Vaitl D. Investigation of mindfulness meditation practitioners with voxel-based morphometry. Soc Cogn Affect Neurosci. 2008;3:55–61. doi: 10.1093/scan/nsm038. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.