Abstract
Aims
This study aims to investigate resting-state functional connectivity (rs-fc) of the right frontoparietal network (rFPN) between migraineurs and healthy controls (HCs), and how the rFPN rs-fc can be modulated by effective treatment.
Methods
One hundred patients and forty-six matched HCs were recruited. Migraineurs were randomized to verum acupuncture, sham acupuncture, and waiting list groups. Resting state fMRI data was collected before and after longitudinal treatments.
Results
Independent component analysis found that migraineurs showed decreased outside-network rs-fc with the bilateral precuneus for rFPN, a key node in the default mode network, compared with HCs. After treatment (real and sham), outside-network rs-fc with the precuneus for rFPN was significantly reduced. This reduction was associated with headache intensity relief. To explore the role of the precuneus in acupuncture modulation, we performed a seed-based rs-fc analysis using the precuneus as a seed and found that the precuneus rs-fc with key regions in the reward system, cognitive control, and descending pain modulatory systems is significantly enhanced after treatment.
Conclusion
Our results suggest that migraineurs were associated with abnormal rFPN rs-fc. An effective treatment, such as acupuncture, may relieve symptoms by strengthening the cognitive adaption/coping process. Elucidation of the adaption/coping mechanism may open a new window for migraine management.
Keywords: Acupuncture, Migraine without aura, fMRI, Independent component analysis, Frontoparietal network, resting state functional connectivity
Introduction
Migraine, a disabling chronic brain disorder, has become an important public healthcare and social issue due to its high prevalence, large medical burden1, disabling effects2, and serious reduction in quality of life3. Nevertheless, many questions regarding its pathophysiology remain unclear. An improved understanding of the mechanisms underlying migraine and the modulation effect of treatment will open new and promising avenues for discovery of its causes as well as the development of new therapeutic methods.
Despite its high prevalence and social burden, treatments for migraine are far from satisfactory4. Previous studies showed that acupuncture may achieve its therapeutic effect by enhancing human body’s self-regulation/healing process; and both verum or sham acupuncture, can significantly relieve migraine headache intensity and frequency5,6. Although the mechanism underlying acupuncture is complex, studies have demonstrated that nonspecific effects (including attention, cognition and expectation) play an important role7. As a result, acupuncture treatment can be used as an effective treatment to investigate the neural physiopathology of migraine.
Recently, investigators have recently begun to explore the functions of individual brain regions of interest as well as neural networks of migraineurs8,9,10,11,12 and found that the brain structure and function of migraineurs differs significantly from that of healthy individuals. These differences can be embodied in their reaction to pain, light and smell, or as an adaptive response to repeated pain (stressor) attacks13,14.
More recently, accumulating evidence has suggested that resting state functional connectivity (rs-fc) may be a valuable tool for understanding brain networks15. One such brain network is the right frontoparietal network (rFPN), which plays an important role in cognitive control and top-down modulation16, and has been reliably identified by independent component analysis (ICA)17. Previous studies suggested that pain and cognition interact reciprocally, i.e., pain can negatively influence cognitive performance, while cognition can significantly modulate our pain experience18,19. In particular, studies have shown that migraineurs are associated with impaired rFPN rs-fc20,21.
Thus, this study aims to investigate the rFPN resting-state functional connectivity (rs-fc) between migraine patients (during the interictal period when they were free from headache symptoms) and matched healthy controls (HC), as well as how longitudinal acupuncture, an effective treatment, can modulate rFPN rs-fc in migraineurs. We hypothesize that migraineurs will be associated with altered rFPN rs-fc to adapt/cope with repeated headache attacks, an effective non-pharmacological treatment that can further modulate the adaptation/coping process.
Materials and Methods
Participants
The Ethics Committee of the 1st Teaching Hospital of Chengdu University of Traditional Chinese Medicine approved all study procedures. The experiment was performed in accordance with approved guidelines. This study was then registered on clinicaltrial.gov (NCT01152632, June 27, 2010). Patients (n=100) and healthy controls (n=46) were enrolled from the outpatient department of the 3rd Teaching Hospital, local advertisements or the Chengdu University of Traditional Chinese Medicine campus. All participants signed a written consent. The recruitment started in June 2011 and ended in November 2013.
Migraine without aura (MwoA) patients
Migraineur inclusion criteria was as follows: 1) 17–45 years (to improve demographic homogeneity) old and right-handed, 2) matched the diagnosis of MwoA based on the International Classification of Headache Disorders, 2nd Edition ICHD-II MwoA criteria22, 3) had not received any prophylactic headache medicine or acupuncture treatment in the past 3 months, 4) had a migraine duration of at least 6 months, and 5) had at least one headache attack per month in the past 3 months. Exclusion criteria included: 1) alcohol or drug abusers, 2) pregnant or lactating women, 3) suffered from psychiatric, neurologic, cardiovascular, respiratory or renal illnesses, 4) had any other type of headache or a history of head trauma with loss of consciousness, 5) magnetic resonance imaging (MRI) contraindications such as claustrophobia, and 6) acupuncture contraindications such as excessive bleeding.
Healthy controls
Right-handed HCs between 17–45 years, free from headache and other chronic pain conditions, were recruited for this study as controls. Each subject underwent a review of medical history evaluation, physical examination, hepatic function, renal function, and routine analysis of blood, urine, and stool to exclude organic disease carriers. Individuals with abnormal test results or a history of head trauma with loss of consciousness, pregnancy or lactation were excluded.
Study Design
The total observation period for MwoA patients in this study was 8 weeks. After screening, all MwoA patients were randomized into 5 groups: verum acupuncture (VA) groups 1, 2, 3 (VA1, VA2, VA3), a sham acupuncture group (SA) and the waiting list (WT) group. All patients were blinded with the group allocation. In this study, we included three verum acupuncture prescriptions to better represent different acupoint selection strategies23. Weeks 1–4 were the baseline phase during which patients recorded baseline headache diaries. Weeks 5–8 were the intervention phase during which patients in treatment groups received verum or sham acupuncture. All patients continued recording headache diaries during this treatment period. In addition, MRI scans were applied at the end of the 4th and 8th weekends for the migraine patients. All MwoA patients were migraine-free for at least 72 hours at the time of the MRI scan. HCs received only the baseline MRI scan (Figure 1).
Figure 1.
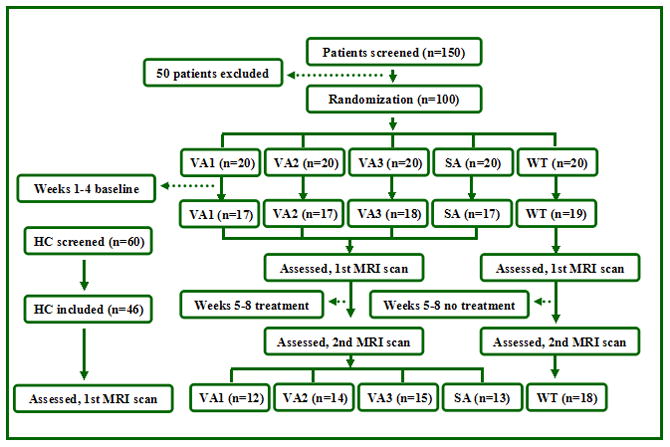
Study flow chart. HC, healthy controls; MRI, magnetic resonance image; n, number; VA, verum acupuncture; SA, sham acupuncture; WT, waiting list.
Interventions
Two licensed acupuncturists administered all acupuncture treatments. Acupoint and non-acupoint selection were similar to those in our previous RCT studies6. Acupoints selected in VA1 included Yanglingquan (GB34), Qiuxu (GB40) and Waiguan (SJ5). VA2 acupoints included Xiyangguan (GB33), Diwuhui (GB42) and Sanyangluo (SJ8). VA3 acupoints included Zusanli (ST36), Chongyang (ST42) and Pianli (L16). SA acupoints included non-acupoints 1, 2, 3 (NAP1, NAP2 and NAP3) (Figure 2).
Figure 2.
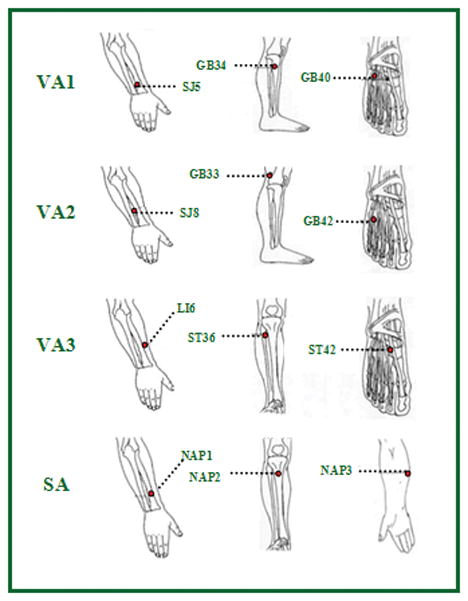
Acupoint locations. GB, Gallbladder meridian; LI, Large intestine meridian; NAP, non acupoints; SA, sham acupuncture; SJ, Sanjiao meridian; ST; Stomach meridian; VA, verum acupuncture; WT, waiting list.
All acupoints and non-acupoints were punctured bilaterally using disposable needles. The needles were inserted perpendicularly at a penetration of 5 to 15 mm and were gently twisted, lifted, and thrust at an even amplitude, force, and speed to acquire deqi sensation24 (deqi sensation is a complex feeling including soreness, numbness, heaviness, distention or dull pain at the site of needle placement) in all treatment groups. The MwoA patients in acupuncture groups received 20 treatments (30 min each) over a 4-week period: once per day for five weekdays followed by a two-day break. Acupuncture or sham acupuncture treatment was not performed on HCs and migraines in the waiting list group.
MwoA patients were instructed and agreed not to take any regular medications for migraine treatment. In cases of severe pain, ibuprofen (300 mg per capsule with sustained release) was allowed as a rescue medication.
Outcome Measures
The clinical outcomes included: headache intensity (visual analogue scale (VAS) of 0–10) and frequency (number of migraines separated by pain-free intervals of at least 48 hours) in the past month obtained from the headache diary. The metrics obtained were consistent with the guidelines of the IHS for Clinical Trials in Migraine25. In addition, the Self-rating anxiety scale (SAS) and Self-rating depression scale (SDS) were applied to assess the MwoA patients’ emotional status26,27.
MRI data acquisition
MRI data was acquired with a 3.0T magnetic resonance scanner (Siemens 3.0T Trio Tim, Munich, Germany) with an 8-channel head coil at the West China Hospital MRI center. Prior to the functional run, a high-resolution structural image for each subject was acquired using a three-dimensional MRI sequence with a voxel size of 1 mm3 employing an axial fast spoiled gradient recalled sequence (TR=1900ms; TE=2.26ms; data matrix, 256×256; field of view, 256×256mm2). The BOLD resting-state functional images were obtained with echo-planar imaging (30 continuous slices with a slice thickness of 5mm; TR=2000ms; TE=30ms; flip angle, 90°; total volumes, 180; matrix size, 64×64; field of view, 256×256mm2). Subjects were instructed to stay awake and remain motionless during the scan with their eyes closed.
Data Analysis
Clinical data analysis
The clinical variables were analyzed using SPSS16.0 software (SPSS Inc, Chicago, IL). A threshold of p < 0.05 (2-tailed) was applied. Continuous variables were presented as the mean (standard deviation) with 95% confidence intervals (CI). Categorical variables were described as n (percentage). χ2 was applied for categorical variables comparisons. For continuous variables, a paired-t test was applied for within-group comparisons, two-sample t-tests were applied for two-group comparisons, and one-way ANOVA was applied when there were more than three groups.
Independent Component Analysis for resting state fMRI data
Resting state data was processed using FSL (FMRIB Software Library) and AFNI following the same processing steps (pipeline) described previously17. Previous studies suggested ICA as a reliable method for analyzing resting state functional connectivity, particularly the attention and control network28,29.
Preprocessing of functional images included removal of non-brain structures, motion correction, temporal bandpass filtering at 0.01 to 0.1 Hz, spatial smoothing (6 mm full-width at half-maximum Gaussian kernel), and 8-parameter nuisance signal extraction. Similar to previous study17, to co-register fMRI images to a standard space, functional images were first registered to each individual’s high-resolution T1 anatomical scan and further registered to the MNI152 template using affine transformations with 12 degrees of freedom30,31.
Probabilistic independent component analysis (PICA) at low dimensionality (20 components) was performed (MELODIC, FSL32) to derive the group’s (n=190) resting state networks. Spatial correlations between our group-level networks and the template networks derived from 1414 healthy subjects17 were calculated. The group-derived network that showed the highest spatial overlap with the rFPN in the template network was assigned to the rFPN.
Then, a dual-regression33 analysis was applied. Using the rFPN as spatial regressors in a general linear model (GLM), we were able to extract the temporal dynamics associated with each spatial map. The resulting time courses served as temporal regressors in a GLM to generate subject-specific maps of the whole brain for each subject. Finally, group analyses were performed using whole-brain subject-specific network maps from the second GLM. The results represent the strength of the rs-fc for each voxel with the rFPN. A two-sample t-test and paired t-test were applied to compare the between-group and within-group differences.
In addition, we also applied multiple regression analyses on migraine patients to explore the association between baseline functional connectivity and the corresponding migraine intensity as measured by VAS, as well as the association between pre- and post-treatment functional connectivity changes and corresponding VAS changes in all treatment groups including age, gender, disease duration, SAS and SDS as non-interest covariates. For all analysis, cluster correction threshold at Z > 2.3, P < .05 was applied.
Seed based functional connectivity
Using ICA analysis, we found that the precuneus plays an important role in the modulation of acupuncture. To further explore the modulation process, we performed a seed based rs-fc analysis using the precuneus as a seed. The fMRI data was preprocessed using Data Processing Assistant for Resting-State fMRI (DPARSF) software (available at: http://rfmri.org/DPARSF). The fMRI images were slice timing and head-motion corrected, coregistered to the respective structural images for each subject, segmented, regressed out 6 rigid body motion, white matter, and CSF signal, normalized using structural image unified segmentation, and then re-sampled to 3-mm cubic voxels. After linear detrending, data was filtered using a typical temporal bandpass (0.01–0.08 Hz) to remove low frequency noise (including slow scanner drifts) and influences of higher frequencies reflecting cardiac and respiratory signals. We removed frames with FD > 0.5 mm (‘scrubbing’), one time point before ‘bad’ time points and two time points after ‘bad’ time points were deleted. Finally, the data was smoothed using a full width half maximum of 6 mm.
Functional connectivity analysis for individual subjects was carried out in DPARSF by applying a seed-region approach using the right precuneus (2, −62, 50, 3mm) so that the coordinate represents the peak of the overlap cluster observed in ICA results. Next, the averaged time course was obtained from the seed and correlation analysis was performed in a voxel-wise manner to generate the FC map. The correlation coefficient map was converted into a Fisher-Z map using Fisher’s r-to-z transform by calling functions in REST to improve normality. Group analysis was calculated with a random effect model using SPM8. We first compared the rs-fc difference between MwoA patients and healthy controls using two sample t-tests. Then, we compared the changes of rs-fc difference (post-treatment minus pre-treatment) between acupuncture (verum + sham) groups (AG) and waiting-list group in factorial design module in SPM8.. A threshold of voxel-wise p < 0.005 (uncorrected) and p < 0.05 family wise error (FWE) corrected at cluster level was applied for all the analyses.
Results
One hundred and fifty patients were screened, of which 100 patients were recruited for this study. Forty-six age and gender matched HCs were also recruited. Eighty-eight patients participated in the first fMRI scan and 81 patients participated in the second. Seven patients did not participate in the second fMRI scan due to scheduling conflicts (2 in VA1, 2 in VA2, 1 in VA3, and 2 in SA). Of the 81 patients who participated in the two MRI scans, 9 patients were excluded from data analysis due to incomplete scans (lack of resting state MRI or T1 anatomy, 3 in V1, 1 in V2, 2 in V3, 2 in SA and 1 patient in the waiting list group) (Figure 1).
The baseline characteristics
We found no statistical difference among VA1, VA2, VA3, SA and waiting list groups in age, sex, weight, height, duration of disease, headache intensity (VAS score), headache frequency, SAS and SDS (P > 0.05). There is no statistical difference in age, gender, weight and height between MwoA patients and HCs (Table 1).
Table 1.
Baseline characteristics of MwoA patients (subjects finished the two scans with completed data) in different groups and healthy controls.
| Characteristics | VA1, n=12 | VA2, n=14 | VA3, n=15 | SA, n=13 | WT, n=18 | P value * | MwoA, n=72 | HC, n=46 | P value ** |
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| Female n(%) | 10 (83.3%) | 10 (71.4%) | 12 (80.0%) | 11 (84.6%) | 14 (77.8%) | 0.925 | 57 (79.2%) | 36 (78.3%) | 0.907 |
|
| |||||||||
| Age (y) | 21.75 | 20.93 | 20.87 | 21.38 | 21.61 | 0.605 | 21.30 | 21.24 | 0.789 |
| Mean (95%CI) | (20.70; 22.80) | (19.74; 22.12) | (19.89; 21.85) | (20.75; 22.02) | (20.54; 22.68) | (20.89; 21.73) | (20.98; 21.50) | ||
|
| |||||||||
| Height (cm) | 159.0 | 161.93 | 159.1 | 157.9 | 162.3 | 0.390 | 160.22 | 161.11 | 0.493 |
| Mean (95%CI) | (154.50; 163.40) | (157.52; 166.24) | (155.13; 163.01) | (154.84; 161.00) | (157.91; 166.76) | (158.49; 161.96) | (158.49; 161.96) | ||
|
| |||||||||
| Weight (kg) | 52.50 | 55.21 | 50.17 | 50.23 | 53.95 | 0.375 | 52.49 | 51.13 | 0.335 |
| Mean (95%CI) | (48.09; 56.91) | (49.23; 61.20) | (47.64; 52.70) | (45.96; 54.50) | (49.01; 58.88) | (50.56; 54.42) | (49.33; 52.93) | ||
|
| |||||||||
| Duration (mo) | 61.67 | 69.57 | 62.27 | 58.69 | 64.73 | 0.140 | - | - | - |
| Mean (95%CI) | (44.38; 78.95) | (56.10; 100.19) | (42.79; 82.54) | (34.29; 64.63) | (58.52; 95.81) | ||||
|
| |||||||||
| Headache intensity | 5.33 | 5.32 | 5.80 | 5.46 | 5.58 | 0.799 | - | - | - |
| Mean (95%CI) | (4.46; 6.20) | (4.77; 5.87) | (5.20; 6.40) | (4.52; 6.40) | (5.14; 6.03) | ||||
|
| |||||||||
| Headache frequency | 5.75 | 7.50 | 5.73 | 6.00 | 4.50 | 0.164 | - | - | - |
| Mean (95%CI) | (3.89; 7.61) | (5.61; 9.39) | (3.58; 7.88) | (4.04; 7.96) | (3.07; 5.93) | ||||
|
| |||||||||
| SAS score | 44.63 | 44.86 | 47.02 | 47.21 | 47.10 | 0.885 | - | - | - |
| Mean (95%CI) | (39.74; 49.51) | (40.36; 49.35) | (41.69; 52.34) | (42.23; 52.20) | (41.92; 52.26) | ||||
|
| |||||||||
| SDS score | 42.13 | 48.98 | 44.80 | 45.06 | 46.88 | 0.516 | - | - | - |
| Mean (95%CI) | (35.01; 49.24) | (43.97; 53.99) | (38.22; 51.38) | (39.25; 50.86) | (42.01; 51.74) | ||||
HC, healthy controls; MwoA, migraine without aura; VA, verum acupuncture; SA, sham acupuncture group; SAS, self-rating anxiety scale; SDS, self-rating depression scale; WT, waiting list;
χ2 test applied for gender comparison, one-way ANOVA applied for the rest comparisons, among VA1, VA2, VA3, SA and WT groups;
χ2 test was applied for gender comparison, two-sample t test applied for the rest comparisons, between MwoA and HC.
The clinical outcomes
Compared with the baseline condition, all three verum acupuncture groups (VA1, VA2, and VA3) showed improvement in headache intensity and headache frequency (P < 0.05) after treatment. Participants in the sham acupuncture group only showed improvement in SAS and SDS (P < 0.05) and a trend for headache intensity (p = 0.083) (Table 2). As expected, we found no significant differences among the VA1, VA2, VA3, and sham acupuncture groups in headache intensity, headache frequency, SAS and SDS improvement (P > 0.05), which is consistent with previously published meta-analysis reports34,35, indicating that the specific effect of acupuncture treatment as compared with sham is only moderate. Because both verum and sham acupuncture treatments reduced the headache intensity in migraine patients we merged all acupuncture groups (AG) and found that AG showed significantly greater improvements than the waiting list group in headache intensity and frequency improvement (P < 0.05) (Table 2). Since the aim of this study is to use acupuncture treatment as a mediator to investigate the neural mechanism of migraine development; thus, we merged all acupuncture treatment groups (verum and sham) in the following rs-fc analyses to investigate the modulation effect of an effective treatment.
Table 2.
Clinical outcomes before and after treatment in different groups. AG, acupuncture group including both verum acupuncture and sham acupuncture; VA, verum acupuncture; SA, sham acupuncture group; SAS, self-rating anxiety scale; SDS, self-rating depression scale; WT, waiting list. Pair-t test was applied for comparisons in each group.
| Outcome measures | VA1, n=12 | VA2, n=14 | VA3, n=15 | SA, n=13 | WT, n=18 | AG, n=54 |
|---|---|---|---|---|---|---|
|
| ||||||
| Headache intensity | ||||||
| Mean (95%CI) | ||||||
|
| ||||||
| Baseline | 5.33 | 5.32 | 5.80 | 5.46 | 5.58 | 5.49 |
| (4.46; 6.20) | (4.77; 5.87) | (5.20; 6.40) | (4.52; 6.40) | (5.14; 6.03) | (5.15; 5.83) | |
|
| ||||||
| End of treatment | 3.25 | 3.57 | 2.87 | 4.19 | 5.53 | 3.45 |
| (2.39; 4.11) | (2.83; 4.31) | (2.01; 3.72) | (3.34; 5.04) | (4.69; 6.36) | (3.06; 3.85) | |
|
| ||||||
| P value | 0.003 | 0.000 | 0.000 | 0.083 | 0.869 | 0.000 |
|
| ||||||
| Headache frequency | ||||||
| Mean (95%CI) | ||||||
|
| ||||||
| Baseline | 5.75 | 7.50 | 5.73 | 6.00 | 4.50 | 6.26 |
| (3.89; 7.61) | (5.61; 9.39) | (3.58; 7.88) | (4.04; 7.96) | (3.07; 5.93) | (5.34; 7.18) | |
|
| ||||||
| End of treatment | 3.92 | 5.93 | 4.20 | 6.15 | 8.17 | 5.06 |
| (2.37; 5.46) | (4.38; 7.47) | (2.42; 5.98) | (4.03; 8.27) | (5.81; 10.52) | (4.21; 5.90) | |
|
| ||||||
| P value | 0.014 | 0.021 | 0.013 | 0.895 | 0.001 | 0.003 |
|
| ||||||
| SAS score | ||||||
| Mean (95%CI) | ||||||
|
| ||||||
| Baseline | 44.63 | 44.86 | 47.02 | 47.21 | 47.10 | 46.00 |
| (39.74; 49.51) | (40.36; 49.35) | (41.69; 52.34) | (42.23; 52.20) | (41.92; 52.26) | (43.71; 48.23) | |
|
| ||||||
| End of treatment | 38.13 | 41.45 | 37.98 | 37.37 | 41.39 | 38.76 |
| (31.15; 45.10) | (37.12; 45.78) | (32.61; 43.36) | (33.09; 41.64) | (37.83; 44.94) | (36.36; 41.17) | |
|
| ||||||
| P value | 0.055 | 0.117 | 0.005 | 0.019 | 0.017 | 0.000 |
|
| ||||||
| SDS score | ||||||
| Mean (95%CI) | ||||||
|
| ||||||
| Baseline | 42.13 | 48.98 | 44.80 | 45.06 | 46.88 | 45.35 |
| (35.01; 49.24) | (43.97; 53.99) | (38.22; 51.38) | (39.25; 50.86) | (42.01; 51.74) | (42.51; 48.20) | |
|
| ||||||
| End of treatment | 40.63 | 42.68 | 39.15 | 37.56 | 41.18 | 40.01 |
| (32.17; 49.08) | (37.07; 48.28) | (33.41; 44.89) | (32.06; 43.06) | (36.57; 45.80) | (37.14; 42.88) | |
|
| ||||||
| P value | 0.518 | 0.040 | 0.023 | 0.049 | 0.066 | 0.000 |
Independent Component Analysis results
As expected, ICA analysis including all subjects/scans have produced a right frontoparietal network, which mainly covers the right DLPFC, VLPFC, bilateral inferior/superior parietal lobules, MPFC, insula and left cerebellum (Figure 3). This component is consistent with findings from previous studies36.
Figure 3.
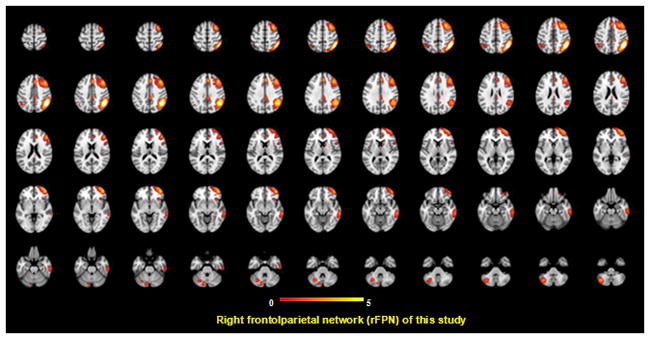
rFPN revealed by independent component analysis in this study.
Compared with healthy controls, MwoA patients showed significant decreased outside-network rs-fc with the bilateral precuneus, lingual gyrus, middle temporal gyrus, and superior temporal gyrus; left fusiform and secondary somatosensory cortex (S2); right cerebellum, inferior occipital gyrus, inferior temporal gyrus and cuneus for rFPN (Figure 4 and Table 4); no abnormal intra-network functional connectivity for rFPN was found. Regression analysis showed that the outside-network rs-fc with the bilateral precuneus, and left superior frontal gyrus and intra-network rs-fc within rACC/MPFC for rFPN were positively associated with migraine headache intensity (VAS) at the baseline. The outside-network rs-fc with the right inferior temporal gyrus for rFPN was negatively associated with headache intensity (Figure 4 and Table 4).
Figure 4.
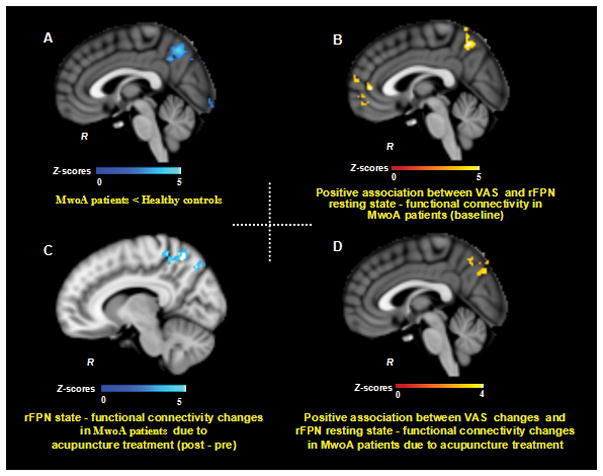
rFPN resting state functional connectivity (rs-fc) results. 4A. MwoA showed reduced rFPN rs-fc with the precuneus at baseline compared with HC; 4B. fFPN rs-fc between the precuneus and MPFC/rACC was associated with headache VAS at baseline; 4C. The reduced rFPN rs-fc with the precuneus due to acupuncture treatment (verum + sham); 4D. The greater reduction of rFPN rs-fc with the right precuneus was associated with greater headache intensity relief. A threshold of Z > 2.3, P < 0.05 was applied. AG, acupuncture groups; HC, healthy controls; MwoA, migraine without aura; R, right side; rFPN, right frontoparietal network; VAS, visual analogue scale.
Table 4.
The rFPN resting state functional connectivity (ICA). AG, acupuncture groups; G, gyrus; HC, healthy controls; Inf, inferior; L, left side; MwoA, migraine without aura; Mid, middle; PCC, posterior cingulate cortex; R, right side; rFPN, right frontoparietal network; Sup, superior; SII, secondary somatosensory cortex; VAS, visual analogue scale
| rFPN resting state functional connectivity differences between MwoA patients and healthy controls at baseline | Association between VAS and rFPN resting state functional connectivity in MwoA patients at baseline | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Contrast | Voxels | Brain Region | MNI (x, y, z) | Z | Contrast | Voxels | Brain Region | MNI (x, y, z) | Z | ||||
|
|
|
||||||||||||
| HC>MwoA | 884 | L/R Precuneus | −6 | −58 | 46 | 4.12 | Positive | 358 | L/R precunues | 4 | −60 | 54 | 3.78 |
|
|
|
||||||||||||
| 595 | L SII | −54 | −32 | 22 | 4.17 | 349 | L Sup Frontal G | −14 | 68 | 10 | 4.14 | ||
|
|
|
||||||||||||
| 689 | L Lingual G | −10 | −98 | −16 | 4.54 | 191 | R/L pgACC/mPFC | −4 | 44 | 0 | 3.54 | ||
|
|
|||||||||||||
| 829 | L Fusiform G/Mid/Sup Temporal G | −46 | −52 | −10 | 4.48 | ||||||||
|
|
|||||||||||||
| 426 | R Lingual/Cuneus | 18 | −84 | 4 | 4.17 | ||||||||
|
|
|||||||||||||
| 1086 | R Sup/Mid/Inf Tempotal G | 38 | −74 | −4 | 4.57 | ||||||||
|
|
|||||||||||||
| 273 | R Cerebellum | 40 | −40 | −28 | 4.72 | ||||||||
|
|
|
||||||||||||
| MwoA>HC | No brain region above the threshold | Negative | 162 | R Inf Temporal G | 52 | −14 | −32 | 4.22 | |||||
|
|
|
||||||||||||
| Changes of rFPN resting state functional connectivity in MwoA patients before and after acupuncture treatment | Association between VAS changes (post minus pre) and corresponding rFPN functional connectivity changes in MwoA patients | ||||||||||||
| Contrast | Voxels | Brain Region | MNI (x, y, z) | Z | Contrast | Voxels | Brain Region | MNI (x, y, z) | Z | ||||
|
|
|
||||||||||||
| Pre>Post | 569 | R Precuneus | 22 | −62 | 40 | 4.02 | Positive | 212 | L/R Precuneus | −2 | −70 | 34 | 3.39 |
|
|
|
||||||||||||
| 195 | L Mid Frontal G | −38 | 34 | 14 | 3.59 | 268 | R Postcentral G | 14 | −34 | 72 | 3.87 | ||
|
|
|
||||||||||||
| Post>Pre | 183 | R/L dorsal PCC | 10 | −38 | 24 | 3.74 | Negative | No brain region above the threshold | |||||
Paired t-tests showed that after longitudinal treatment (real and sham), the outside-network rs-fc with the right precuneus and intra-network rs-fc within left middle frontal gyrus for rFPN was significantly reduced; the outside-network rs-fc with the bilateral posterior cingulate cortex (PCC) for rFPN was significantly increased (Figure 4 and Table 4). Regression analysis showed that after treatment, the decrease of outside-network rs-fc with the bilateral precuneus, right paracentral gyrus and postcentral gyrus for rFPN was positively associated with a decrease in headache intensity (Figure 4 and Table 4).
In waiting list group, we found the intra-network rs-fc within the left inferior frontal gyrus (peak MNI coordinates: −52, 30, 8, cluster size 351) and bilateral MPFC (peak MNI coordinates: 0, 44, 28, cluster size 273) for rFPN was significantly reduced; the outside-network rs-fc with the middle temporal gyrus/angular gyrus (peak MNI coordinates: −52, −68, 38, cluster size 208) for rFPN was significantly increased in MwoA patients (second time–first time). The comparison between the acupuncture treatment (real and sham) (post minus pre-treatment) and the waiting list group showed a significant difference at the left cerebellum (peak MNI coordinates: −6, −46, −30, cluster size 163) and right middle frontal gyrus (peak MNI coordinates: 38, 6, 46, cluster size 123). In addtion, we also compared sham acupuncture group and waiting list group. The comparison between the sham group (post minus pre-treatment) and the waiting list group showed a significant difference at the left precentral gyrus (peak MNI coordinates:42, −4, 60, cluster size 523) and left insula (peak MNI coordinates: 46, −8, 12, cluster size 122).
Seed-based rs-fc analysis results
We found that the right precuneus plays an important role in pathophysiology of migraine, specifically that: 1) reduced outside-network rs-fc with the right precuneus for rFPN in MwoA patients as compared with healthy controls; 2) outside-network rs-fc with right precuneus for rFPN was associated with headache intensity in baseline MwoA patients; and 3) the decrease of outside-network rs-fc with the right precuneus for rFPN was positively associated with a decrease in headache intensity due to acupuncture treatment. To further explore the role of the right precuneus in the pathology of migraine and its role in treatment, we applied a functional connectivity analysis using the peak of the overlapped cluster at right precuneus (2, −62, 50, 3mm) as the seed. We found that compared with HCs, MwoA patients showed reduced right precuneus rs-fc with the left precuneus, supramarginal gyrus and inferior temporal gyrus. After longitudinal acupuncture treatment (verum + sham), MwoA patients showed increased right precuneus rs-fc with the bilateral rACC/MPFC, ventral striatum, middle/inferior occipital gyrus, cuneus, DLPFC and cerebellum, and left VLPFC and right superior temporal gyrus (Figure 5, Table 4).
Figure 5.
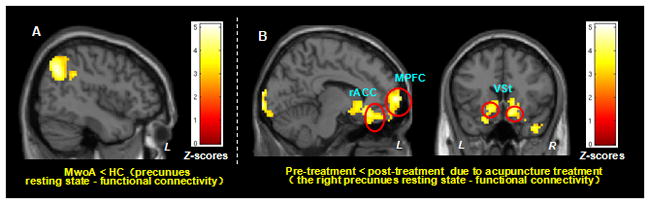
Precuneus resting state functional connectivity (rs-fc) results. 5A. MwoA showed reduced precuneus rs-fc with the supramarginal gyrus and inferior temporal gyrus, compared with HC. 5B. MwoA patients showed increased right precuneus rs-fc with the bilateral rACC/MPFC, ventral striatum, DLPFC and VLPFC, due to acupuncture treatment (verum + sham). A threshold of Voxelwise P < 0.005 and p < 0.05 FWE corrected was applied. AG, acupuncture groups; DLPFC, dorsolateral prefrontal cortex; HC, healthy controls; Inf, inferior; L, left side; MPFC, medial prefrontal cortex; MwoA, migraine without aura; Mid, middle; R, right side; rACC, rostral anterior cingulate cortex; VLPFC, ventrolateral prefrontal cortex.
Discussion
In this study, we found that MwoA patients showed reduced outside-network rs-fc with the bilateral precuneus for rFPN during the interictal period compared with healthy controls. The outside-network rs-fc with precuneus and intra-network rs-fc within MPFC/rACC for rFPN were positively associated with headache intensity in MwoA patients at baseline. Interestingly, acupuncture (both real and sham), could significantly reduce outside-network rs-fc with the precuneus for rFPN. Greater headache intensity relief was associated with greater reduced outside-network rs-fc with the right precuneus for rFPN. Seed-based functional connectivity analysis (using the right precuneus as the seed) showed that longitudinal acupuncture treatment significantly enhanced precuneus rs-fc with MPFC/rACC, ventral striatum37, and DLPFC/VLPFC38,39.
Our result is partly consistent with previous studies in which investigators found timpaired rFPN rs-fc in MwoA patients20,21. Xue and colleagues20 found that migraineurs (n=23) showed increased rFPN rs-fc in the middle frontal gryus and anterior insula and in another study, Russo and colleagues21 found that MwoA patients (n=14) had reduced rFPN rs-fc with the middle frontal gyrus and dorsal anterior cingulate cortex compared to healthy controls. The different rFPN rs-fc changes in migraineurs between our study and previous studies may not necessarily be contradictory, as we believe the differences reflect the complexity of the neural physiopathology of migraine40.
Previous studies have suggested38,39 that the key regions of rFPN including VLPFC, DLPFC and the parietal gyrus are involved in the cognitive control of pain, and that all these regions have direct connections with brain regions involved in affective (i.e., ACC, MPFC, amygdala) and sensory (i.e., SI, S2/insula) pain process components. We find that MwoA patients showed reduced outside-network rs-fc with the precuneus for rFPN, which is associated with reduced headache intensity. This result is consistent with previous studies showing that the precuneus is closely connected with the rFPN both anatomically and functionally41,42. The precuneus is a key node in the default mode network (DMN)36, a brain network associated with self-referential processing43,44 and mind-wandering45 whereas the rFPN plays an important role in attention, memory process and cognitive control 16. We thus speculate that the reduced rs-fc between the rFPN and the precuneus may represent the brain’s self-compensatory adaptation/coping responses to continued attacks of migraine46,47. Specifically, paying attention to pain48 results in more suffering while distraction49 from pain results in a less painful experience. The body may automatically apply a distraction strategy as a natural response to avoid suffering.
Interestingly, we found that longitudinal acupuncture treatment could further reduce outside-network rs-fc with the right precuneus for rFPN, and that reduced right precuneus-rFPN rs-fc was associated with migraine headache intensity reduction. Previous studies suggested that expectation, attention and reappraisal are crucial components of the non-specific effect of treatments38,39,50. And studies have also shown that the non-specific effect plays an important role in acupuncture’s treatment of chronic pain51,52,53. Taken together, our results suggest that acupuncture may relieve headache intensity by enhancing the self-compensatory adaptation/coping process. This finding is consistent with a previous brain imaging cognitive behavioral therapy on fibromyalgia showing that rather than reducing pain response in patients with fibromyalgia, cognitive behavioral therapy increases access to executive regions for reappraisal of pain54.
Seed-based functional connectivity analysis showed that after longitudinal acupuncture treatments, the right precuneus rs-fc with the MPFC/rACC significantly increased. MPFC/rACC have wide functional connections55 and involvement in many functions; several studies have suggested that the MPFC/rACC is functionally connected with PAG56,57, a key region in the descending pain modulatory regions. We thus speculate that the increased precuneus rs-fc and MPFC/rACC imply an enhancement between the self-referral system and pain modulation process.
We also found increased precuneus rs-fc with cognitive control brain regions (i.e., VLPFC and DLPFC) and reward regions (i.e., ventral striatum/nucleus accumbens). A previous study58 showed that pain relief could produce negative reinforcement through activation of the mesocorticolimbic reward-valuation circuitry. A recent human fMRI-PET study59 found that increased endogenous opioid releases were at nucleus accumbens during pressure pain. Taken together, our results suggest that the cognitive control network, reward system, and descending pain modulatory network may all be involved in the modulation process of acupuncture treatment.
There are several limitations to this study. 1) The sample size in each acupuncture treatment group is small, which prevents us from testing clinical outcome differences between different acupuncture treatment groups. In addition, the dropout rate is relatively high; however, we would like to emphasize that the reasons for dropout do not seem to be associated with treatment response. Also, the aim of this study is to explore the neural physiopathology of migraine so using the treatment as a mediator is intended to investigate how an effective treatment can modulate the rFPN rs-fc rather than test the efficacy of acupuncture itself. 2) Although the patients were migraine-free for at least 72 hours at the time of the MRI scan, they could have been in different stages with regards to the upcoming migraine attack60. 3) We do not have a second fMRI scan for the matched healthy controls. Thus, we can not completely rule out the result observed in drift effects over time or habituation to the scanning environment.
Conclusion
Migraine is associated with abnormal rFPN rs-fc during the interictal period. The reduced rFPN rs-fc with the DMN is associated with lower headache intensity, suggesting an adapting/coping cognitive mechanism in migraine patients. An effective treatment, such as acupuncture, may achieve symptom relief by strengthening the cognitive adapting/coping mechanism.
Table 3.
Comparisons of the therapeutic effects between different groups.
| Outcome measures | VA1, n=12 | VA2, n=14 | VA3, n=15 | SA, n=13 | P value * | WT, n=18 | AG, n=54 | P value ** |
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Headache intensity | ||||||||
| Mean (95%CI) | ||||||||
|
| ||||||||
| End of treatment | 3.25 | 3.57 | 2.87 | 4.19 | 0.101 | 5.53 | 3.45 | 0.000 |
| (2.39; 4.11) | (2.83; 4.31) | (2.01; 3.72) | (3.34; 5.04) | (4.69; 6.36) | (3.06; 3.85) | |||
|
| ||||||||
| End - baseline | −2.08 | −1.75 | −2.93 | −1.27 | 0.139 | −0.06 | −2.04 | 0.000 |
| (−3.31; −0.86) | (−2.42; −1.08) | (−4.01; −1.86) | (−2.73; −0.19) | (−0.75; 0.64) | (−2.57; −1.50) | |||
|
| ||||||||
| Headache frequency | ||||||||
| Mean (95%CI) | ||||||||
|
| ||||||||
| End of treatment | 3.92 | 5.93 | 4.20 | 6.15 | 0.132 | 8.17 | 5.06 | 0.016 |
| (2.37; 5.46) | (4.38; 7.47) | (2.42; 5.98) | (4.03; 8.27) | (5.81; 10.52) | (4.21; 5.90) | |||
|
| ||||||||
| End - baseline | −1.83 | −1.57 | −1.53 | 0.15 | 0.250 | 3.67 | −1.20 | 0.000 |
| (−3.21; −0.46) | (−2.87; −0.28) | (−2.69; −0.37) | (−2.32; 2.63) | (1.63; 5.70) | (−1.96; −0.44) | |||
|
| ||||||||
| SAS score | ||||||||
| Mean (95%CI) | ||||||||
|
| ||||||||
| End of treatment | 38.13 | 41.45 | 37.98 | 37.37 | 0.626 | 41.39 | 38.76 | 0.257 |
| (31.15; 45.10) | (37.12; 45.78) | (32.61; 43.36) | (33.09; 41.64) | (37.83; 44.94) | (36.36; 41.17) | |||
|
| ||||||||
| End - baseline | −6.50 | −3.41 | −9.03 | −9.85 | −5.71 | −7.21 | 0.591 | |
| (−13.16; 0.17) | (−7.79; 0.97) | (−14.78; −3.28) | (−17.78; −1.92) | 0.379 | (−10.26; −1.16) | (−10.08; −4.33) | ||
|
| ||||||||
| SDS score | ||||||||
| Mean (95%CI) | ||||||||
|
| ||||||||
| End of treatment | 40.63 | 42.68 | 39.15 | 37.56 | 0.638 | 41.18 | 40.01 | 0.675 |
| (32.17; 49.08) | (37.07; 48.28) | (33.41; 44.89) | (32.06; 43.06) | (36.57; 45.80) | (37.14; 42.88) | |||
|
| ||||||||
| End - baseline | −1.50 | −6.30 | −5.65 | −7.50 | 0.469 | −5.69 | −5.34 | 0.902 |
| (−6.44; 3.44) | (−12.26; −0.35) | (−10.38; −0.92) | (−14.96; −0.05) | (−11.81; 0.43) | (−5.34; −8.03) | |||
AG, acupuncture groups; HC, healthy controls; VA, verum acupuncture; SA, sham acupuncture; SAS, self-rating anxiety scale; SDS, self-rating depression scale; WT, waiting list;
one-way ANOVA was applied for the comparisons among VA1, VA2, VA3, SA and WT groups;
two-sample t test was applied for the comparisons between MwoA and HC.
Table 5.
Results from seed-based functional connectivity analysis. The altered right precuneus resting state functional connectivity in MwoA as compared with healthy controls, and pre- and post-treatment resting state functional connectivity differences across patients. DLPFC, dorsolateral prefrontal cortex;Inf, inferior; L, left side; MPFC, medial prefrontal cortex; MwoA, migraine without aura; Mid, middle; R, right side; rACC, rostral anterior cingulate cortex; rFPN, right frontoparietal network; Sup, superior; VLPFC, ventrolateral prefrontal cortex.
| The right precuneus resting state functional connectivity Difference between MwoA patients and healthy controls | ||||||
|---|---|---|---|---|---|---|
| Contrast | Voxels | Brain Region | MNI (x, y, z) | Z | ||
| HC>MwoA | 322 | L Precuneus | 42 | −63 | 39 | 4.68 |
| L Supramarginal G/Inf Temperal G | 51 | −42 | 36 | 3.77 | ||
|
| ||||||
| MwoA>HC | No brain region above the threshold | |||||
|
| ||||||
| Resting state functional connectivity changes before and after acupuncture treatment | ||||||
| Contrast | Voxels | Brain Region | MNI (x, y, z) | Z | ||
|
| ||||||
| Post>Pre | 1693 | L MPFC/rACC | −6 | 66 | 3 | 4.62 |
| L VLPFC | −3 | 54 | −24 | 4.57 | ||
| L Ventral stratuim | −12 | 18 | −9 | 3.55 | ||
| L DLPFC | −33 | −63 | 0 | 4.1 | ||
| R MPFC/rACC | 9 | 69 | 6 | 4.2 | ||
| R Ventral stratuim | 15 | 15 | −12 | 4.16 | ||
| R DLPFC | 18 | 69 | −3 | 3.96 | ||
| R Sup Temporal G | 36 | 6 | −33 | 3.87 | ||
|
| ||||||
| 207 | L Cerebellum | −42 | −63 | −48 | 4.32 | |
|
| ||||||
| 294 | L Mid/Inf occipital G | −27 | −99 | −9 | 4.3 | |
|
| ||||||
| 305 | R Cerebellum | 51 | −69 | −39 | 4.36 | |
|
| ||||||
| 347 | R Mid/Inf occipital G | 21 | −102 | 12 | 4.51 | |
|
| ||||||
| Pre>Post | No brain region above the threshold | |||||
Clinical Implications.
Migraineurs might be associated with abnormal rFPN rs-fc. An effective treatment, such as acupuncture, may relieve symptoms by strengthening the cognitive adaption/coping process. Elucidation of the adaption/coping mechanism may open a new window for migraine management.
Acknowledgments
This study was supported by grants from the State Key Program for Basic Research of China (2012CB518501), the National Natural Science Foundation of China (No.81273154 and No.81473602), the Program for New Century Talents in the University of Ministry of Education of China (2013) and the Youth Foundation of Sichuan Province (No.2012JQ0052). J. K. is supported by R01AT006364 (NIH/NCCAM) and P01AT006663 (NIH/NCCAM).
The authors would like to thank Wei Qin, Jinbo Sun, Jixin Liu, Minghao Dong, Qizhu Wu and Xiaoqi Huang from Xidian University and the West China Hospital of Sichuan University for their assistance in this study.
Footnotes
Disclosure
The authors report no disclosures relevant to the manuscript.
Author contributions
F. L. and F. Z. are the corresponding authors. Z. L. and L. L. contributed equally to this article. Study protocol and design: F. L., F. Z., Y. L. and Q. G.; acquisition of data: M. L., L. L., T. G., F. W., Y. G., M. D., and J. Y.; analysis and interpretation of data: Z. L., N. M., J. H., F. Z., and J. K.; drafting of the manuscript: Z. L., L. L., S. S., N. M., and J. K. All authors reviewed the manuscript.
References
- 1.Stovner LJ, Hagen K. Prevalence, burden, and cost of headache disorders. Curr Opin Neurol. 2006;19:281–285. doi: 10.1097/01.wco.0000227039.16071.92. [DOI] [PubMed] [Google Scholar]
- 2.Leonardi M, Steiner TJ, Scher AT, et al. The global burden of migraine: measuring disability in headache disorders with WHO’s Classification of Functioning, Disability and Health (ICF) J Headache Pain. 2005;6:429–440. doi: 10.1007/s10194-005-0252-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Guitera V, Munoz P, Castillo J, et al. Quality of life in chronic daily headache: a study in a general population. Neurology. 2002;58:1062–1065. doi: 10.1212/wnl.58.7.1062. [DOI] [PubMed] [Google Scholar]
- 4.Diener H-C, Dodick DW, Goadsby PJ, et al. Chronic migraine—classification, characteristics and treatment. Nature Reviews Neurology. 2012;8:162–171. doi: 10.1038/nrneurol.2012.13. [DOI] [PubMed] [Google Scholar]
- 5.Linde K, Allais G, Brinkhaus B, et al. Acupuncture for migraine prophylaxis. Cochrane Database Syst Rev. 2009:CD001218. doi: 10.1002/14651858.CD001218.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Li Y, Zheng H, Witt CM, et al. Acupuncture for migraine prophylaxis: a randomized controlled trial. CMAJ. 2012;184:401–410. doi: 10.1503/cmaj.110551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Han JS. Acupuncture analgesia: areas of consensus and controversy. Pain. 2011;152:S41–8. doi: 10.1016/j.pain.2010.10.012. [DOI] [PubMed] [Google Scholar]
- 8.Hadjikhani N, Ward N, Boshyan J, et al. The missing link: enhanced functional connectivity between amygdala and visceroceptive cortex in migraine. Cephalalgia. 2013;33:1264–8. doi: 10.1177/0333102413490344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schwedt TJ, Larson-Prior L, Coalson RS, et al. Allodynia and descending pain modulation in migraine: a resting state functional connectivity analysis. Pain Med. 2014;15:154–165. doi: 10.1111/pme.12267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vecchia D, Pietrobon D. Migraine: a disorder of brain excitatory-inhibitory balance? Trends Neurosci. 2012;35:507–520. doi: 10.1016/j.tins.2012.04.007. [DOI] [PubMed] [Google Scholar]
- 11.Maleki N, Becerra L, Brawn J, et al. Common hippocampal structural and functional changes in migraine. Brain Struct Funct. 2013;218:903–912. doi: 10.1007/s00429-012-0437-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Liu P, Qin W, Zhang Y, et al. Combining spatial and temporal information to explore function-guide action of acupuncture using fMRI. J Magn Reson Imaging. 2009;30:41–46. doi: 10.1002/jmri.21805. [DOI] [PubMed] [Google Scholar]
- 13.Noseda R, Burstein R. Migraine pathophysiology: Anatomy of the trigeminovascular pathway and associated neurological symptoms, cortical spreading depression, sensitization, and modulation of pain. Pain. 2013 doi: 10.1016/j.pain.2013.07.021. [DOI] [PubMed] [Google Scholar]
- 14.Schwedt TJ, Chiang C-C, Chong CD, et al. Functional MRI of migraine. Lancet Neurol. 2015;14:81–91. doi: 10.1016/S1474-4422(14)70193-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Barkhof F, Haller S, Rombouts SARB. Resting-state functional MR imaging: a new window to the brain. Radiology. 2014;272:29–49. doi: 10.1148/radiol.14132388. [DOI] [PubMed] [Google Scholar]
- 16.Corbetta M, Shulman GL. Control of goal-directed and stimulus-driven attention in the brain. Nat Rev Neurosci. 2002;3:201–215. doi: 10.1038/nrn755. [DOI] [PubMed] [Google Scholar]
- 17.Biswal BB, Mennes M, Zuo X-N, et al. Toward discovery science of human brain function. Proc Natl Acad Sci U S A. 2010;107:4734–4739. doi: 10.1073/pnas.0911855107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Moriarty O, Finn DP. Cognition and pain. Curr Opin Support Palliat Care. 2014;8:130–6. doi: 10.1097/SPC.0000000000000054. [DOI] [PubMed] [Google Scholar]
- 19.Moriarty O, McGuire BE, Finn DP. The effect of pain on cognitive function: A review of clinical and preclinical research. Progress in Neurobiology. 2011;93:385–404. doi: 10.1016/j.pneurobio.2011.01.002. [DOI] [PubMed] [Google Scholar]
- 20.Xue T, Yuan K, Zhao L, et al. Intrinsic Brain Network Abnormalities in Migraines without Aura Revealed in Resting-State fMRI. PLoS One. 2012:7. doi: 10.1371/journal.pone.0052927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Russo A, Tessitore A, Giordano A, et al. Executive resting-state network connectivity in migraine without aura. Cephalalgia. 2012;32:1041–1048. doi: 10.1177/0333102412457089. [DOI] [PubMed] [Google Scholar]
- 22.Headache Classification Subcommittee of the International Headache S. The International Classification of Headache Disorders: 2nd edition. Cephalalgia. 2004;24(Suppl 1):9–160. doi: 10.1111/j.1468-2982.2003.00824.x. [DOI] [PubMed] [Google Scholar]
- 23.Li Y, Zheng H, Witt CM, et al. Acupuncture for migraine prophylaxis: a randomized controlled trial. CMAJ. 2012;184:401–410. doi: 10.1503/cmaj.110551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kong J, Gollub R, Huang T, et al. Acupuncture de qi, from qualitative history to quantitative measurement. J Altern Complement Med. 2007;13:1059–1070. doi: 10.1089/acm.2007.0524. [DOI] [PubMed] [Google Scholar]
- 25.Headache Classification Subcommittee of the International Headache S. The International Classification of Headache Disorders: 2nd edition. Cephalalgia. 2004;24(Suppl 1):9–160. doi: 10.1111/j.1468-2982.2003.00824.x. [DOI] [PubMed] [Google Scholar]
- 26.Seidel S, Hartl T, Weber M, et al. Quality of sleep, fatigue and daytime sleepiness in migraine - A controlled study. Cephalalgia. 2009;29:662–669. doi: 10.1111/j.1468-2982.2008.01784.x. [DOI] [PubMed] [Google Scholar]
- 27.Usai S, Grazzi L, D’Amico D, et al. Psychological variables in chronic migraine with medication overuse before and after inpatient withdrawal: Results at 1-year follow-up. Neurol Sci. 2009:30. doi: 10.1007/s10072-009-0066-2. [DOI] [PubMed] [Google Scholar]
- 28.Zuo X-N, Xu T, Jiang L, et al. Toward reliable characterization of functional homogeneity in the human brain: preprocessing, scan duration, imaging resolution and computational space. Neuroimage. 2013;65:374–86. doi: 10.1016/j.neuroimage.2012.10.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zuo X, Xing X. Neuroscience and Biobehavioral Reviews Test-retest reliabilities of resting-state FMRI measurements in human brain functional connectomics: A systems neuroscience perspective. Neurosci Biobehav Rev. 2014;45:100–118. doi: 10.1016/j.neubiorev.2014.05.009. [DOI] [PubMed] [Google Scholar]
- 30.Jenkinson M, Smith S. A global optimisation method for robust affine registration of brain images. Med Image Anal. 2001;5:143–156. doi: 10.1016/s1361-8415(01)00036-6. [DOI] [PubMed] [Google Scholar]
- 31.Jenkinson M, Bannister P, Brady M, et al. Improved optimization for the robust and accurate linear registration and motion correction of brain images. Neuroimage. 2002;17:825–841. doi: 10.1016/s1053-8119(02)91132-8. [DOI] [PubMed] [Google Scholar]
- 32.Beckmann CF, Smith SM. Probabilistic Independent Component Analysis for Functional Magnetic Resonance Imaging. IEEE Trans Med Imaging. 2004;23:137–152. doi: 10.1109/TMI.2003.822821. [DOI] [PubMed] [Google Scholar]
- 33.Filippini N, MacIntosh BJ, Hough MG, et al. Distinct patterns of brain activity in young carriers of the APOE-epsilon4 allele. Proc Natl Acad Sci U S A. 2009;106:7209–7214. doi: 10.1073/pnas.0811879106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Vickers AJ, Cronin AM, Maschino AC, et al. Acupuncture for chronic pain: individual patient data meta-analysis. Arch Intern Med. 2012;172:1444–1453. doi: 10.1001/archinternmed.2012.3654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Vickers AJ, Linde K. Acupuncture for chronic pain. JAMA. 2014;311:955–956. doi: 10.1001/jama.2013.285478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Smith SM, Fox PT, Miller KL, et al. Correspondence of the brain’s functional architecture during activation and rest. Proc Natl Acad Sci U S A. 2009;106:13040–13045. doi: 10.1073/pnas.0905267106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Leknes S, Tracey I. A common neurobiology for pain and pleasure. Nat Rev Neurosci. 2008;9:314–320. doi: 10.1038/nrn2333. [DOI] [PubMed] [Google Scholar]
- 38.Bushnell MC, Ceko M, Low LA. Cognitive and emotional control of pain and its disruption in chronic pain. Nat Rev Neurosci. 2013;14:502–11. doi: 10.1038/nrn3516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wiech K, Ploner M, Tracey I. Neurocognitive aspects of pain perception. Trends in Cognitive Sciences. 2008;12:306–313. doi: 10.1016/j.tics.2008.05.005. [DOI] [PubMed] [Google Scholar]
- 40.Pietrobon D, Moskowitz MA. Pathophysiology of migraine. Annu Rev Physiol. 2013;75:365–91. doi: 10.1146/annurev-physiol-030212-183717. [DOI] [PubMed] [Google Scholar]
- 41.Utevsky AV, Smith DV, Huettel Sa. Precuneus is a functional core of the default-mode network. J Neurosci. 2014;34:932–40. doi: 10.1523/JNEUROSCI.4227-13.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Margulies DS, Vincent JL, Kelly C, et al. Precuneus shares intrinsic functional architecture in humans and monkeys. Proc Natl Acad Sci U S A. 2009;106:20069–74. doi: 10.1073/pnas.0905314106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Raichle ME, Snyder AZ. A default mode of brain function: A brief history of an evolving idea. Neuroimage. 2007;37:1083–1090. doi: 10.1016/j.neuroimage.2007.02.041. [DOI] [PubMed] [Google Scholar]
- 44.Buckner RL, Andrews-Hanna JR, Schacter DL. The brain’s default network: Anatomy, function, and relevance to disease. Annals of the New York Academy of Sciences. 2008;1124:1–38. doi: 10.1196/annals.1440.011. [DOI] [PubMed] [Google Scholar]
- 45.Mason MF, Norton MI, Van Horn JD, et al. Wandering minds: the default network and stimulus-independent thought. Science. 2007;315:393–5. doi: 10.1126/science.1131295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Mansour AR, Farmer MA, Baliki MN, et al. Chronic pain: the role of learning and brain plasticity. Restor Neurol Neurosci. 2014;32:129–39. doi: 10.3233/RNN-139003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Borsook D, Maleki N, Becerra L, et al. Perspective Understanding Migraine through the Lens of Maladaptive Stress Responses: A Model Disease of Allostatic Load. Neuron. 2012;73:219–234. doi: 10.1016/j.neuron.2012.01.001. [DOI] [PubMed] [Google Scholar]
- 48.Quevedo AS, Coghill RC. Attentional modulation of spatial integration of pain: evidence for dynamic spatial tuning. J Neurosci. 2007;27:11635–11640. doi: 10.1523/JNEUROSCI.3356-07.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Villemure C, Bushnell MC. Cognitive modulation of pain: How do attention and emotion influence pain processing? Pain. 2002;95:195–199. doi: 10.1016/S0304-3959(02)00007-6. [DOI] [PubMed] [Google Scholar]
- 50.Freeman S, Yu R, Egorova N, et al. Distinct neural representations of placebo and nocebo effect. Neuroimage. 2015;112:197–207. doi: 10.1016/j.neuroimage.2015.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Han JS. Acupuncture analgesia: areas of consensus and controversy. Pain. 2011;152:S41–8. doi: 10.1016/j.pain.2010.10.012. [DOI] [PubMed] [Google Scholar]
- 52.Kong J, Kaptchuk TJ, Polich G, et al. Expectancy and treatment interactions: A dissociation between acupuncture analgesia and expectancy evoked placebo analgesia. Neuroimage. 2009;45:940–949. doi: 10.1016/j.neuroimage.2008.12.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kong J, Kaptchuk TJ, Polich G, et al. An fMRI study on the interaction and dissociation between expectation of pain relief and acupuncture treatment. Neuroimage. 2009;47:1066–1076. doi: 10.1016/j.neuroimage.2009.05.087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Jensen KB, Kosek E, Wicksell R, et al. Cognitive Behavioral Therapy increases pain-evoked activation of the prefrontal cortex in patients with fibromyalgia. Pain. 2012;153:1495–503. doi: 10.1016/j.pain.2012.04.010. [DOI] [PubMed] [Google Scholar]
- 55.Margulies DS, Kelly AMC, Uddin LQ, et al. Mapping the functional connectivity of anterior cingulate cortex. Neuroimage. 2007;37:579–588. doi: 10.1016/j.neuroimage.2007.05.019. [DOI] [PubMed] [Google Scholar]
- 56.Kong J, Tu PC, Zyloney C, et al. Intrinsic functional connectivity of the periaqueductal gray, a resting fMRI study. Behav Brain Res. 2010;211:215–219. doi: 10.1016/j.bbr.2010.03.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Yu R, Gollub R, Spaetha V, Napadowa A, Wasana J, Kong R. Disrupted functional connectivity of the periaqueductal gray in chronic low back pain. NeuroImage Clin. 2014;6:100–108. doi: 10.1016/j.nicl.2014.08.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Navratilova E, Xie JY, Okun A, et al. Pain relief produces negative reinforcement through activation of mesolimbic reward-valuation circuitry. Proc Natl Acad Sci U S A. 2012;109:20709–20713. doi: 10.1073/pnas.1214605109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Wey HY, Catana C, Hooker JM, et al. Simultaneous fMRI-PET of the opioidergic pain system in human brain. Neuroimage. 2014;102P2:275–282. doi: 10.1016/j.neuroimage.2014.07.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Stankewitz A, Aderjan D, Eippert F, et al. Trigeminal nociceptive transmission in migraineurs predicts migraine attacks. J Neurosci. 2011;31:1937–1943. doi: 10.1523/JNEUROSCI.4496-10.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]


