Abstract
In addition to its contribution to child mortality, HIV/AIDS has a substantial impact on the psychosocial well-being of children across the globe and particularly in sub-Saharan Africa. We conducted a systematic review of the literature in order to identify studies that assess the effectiveness of interventions developed to improve the psychosocial well-being of children affected by HIV/AIDS, published between January 2008 and February 2016.
Studies that were eligible for the review included male and/or female children under the age of 18 years of age, who had lost a parent to HIV/AIDS, were living with a parent with HIV/AIDS, or were vulnerable because of other social and economic factors and living in communities of high HIV and AIDS prevalence, including child and caregiver reports. Studies were included if they documented any intervention to improve the psychosocial well-being of children including psychological therapy, psychosocial support and/or care, medical interventions and social interventions, with psychological and/or social factors as outcomes.
We identified 17 interventions to improve the psychosocial well-being of children affected by HIV/AIDS. Of these, 16 studies took place in eight different low and middle-income countries (LMIC), of which 6 were in southern and eastern Africa. One study took place in a high-income setting. Of the total, fifteen showed some significant benefits of the intervention, while two showed no difference to psychosocial outcomes as a result of the intervention. The content of interventions, dosage and length of follow up varied substantially between studies. There were few studies on children under seven years and several focused mostly on girls.
Efforts to improve evaluation of interventions to improve the psychosocial well-being of children affected by HIV/AIDS have resulted in a number of new studies which met the inclusion criteria for the review. Most studies are specially designed research projects and not evaluations of existing services. We call for increased partnerships between policy-makers, practitioners and researchers in order to design evaluation studies and can feed into the growing evidence base.
INTRODUCTION
HIV exerts a negative influence on child psychosocial outcomes, both directly through infection, and indirectly through increased risk at family and community (Stein et al. 2014). Children who are infected with HIV/AIDS face life-long risk of related illnesses, and are more likely to experience cognitive and motor development delays, stigma, trauma, and low mood (Vreeman et al 2015, Abubakar et al., 2008; Sherr et al., 2009). Children who have lost one or both parents to HIV are at increased risk of mental health problems (Mutumba et al 2016, Stein et al 2014, Sherr et al 2014), such as internalising disorders and post-traumatic stress (Cluver & Gardner, 2007), and are often living in alternative care situations. HIV exhausts family financial resources, through job loss or reduced productivity due to illness, the expenses associated with accessing health care, and the high cost of funerals (Thomas, 2006).
Recent years have seen an increase in the attention and resources dedicated to mitigating the impact of HIV/AIDS on children (Akwara et al. 2010) and there has also been a growing realisation of the importance of community-led initiatives to support families affected by the pandemic (Campbell and Cornish 2012). Across sub-Saharan Africa, there are a vast number of grassroots organisations and programmes activities providing care and support in a variety of different ways, a number of which are supported by international donors. For example in 2009, it was estimated that World Bank, Global Fund, and PEPFAR were providing in excess of 100 million USD funding to support programmes for vulnerable children in Uganda (JLICA 2009). Programme types are varied and include psychological interventions (e.g. support groups, psychological debriefing), support programmes (e.g. home visiting or play groups), and social programmes (e.g. cash transfer programmes, material assistance, skills building programmes) (King et al. 2009). However, there is relatively little evidence available on what types of community-based programmes can improve health and well-being outcomes for children affected by the pandemic. In fact, research suggests the opposite: that there is very little routine evaluation of community programmes, and that the information that is generated is not reaching the evidence base.
The paucity of evidence in this field is problematic. Considering the large burden of disease of HIV/AIDS in the sub-Saharan African region in particular, the moral case for investing in research into these interventions is indisputable. In order to develop evidence-based interventions, we need to design studies that ascertain the efficacy of interventions and define causal pathways more clearly. Reliable evidence is needed to support the efficient use of limited resources for training, supervision and management (Kim, Farmer, & Porter, 2013). It is also important to ascertain whether existing programmes are creating unintended negative effects for the children and their families, for example by singling out certain children for participation, leading to stigma or isolation of the child. Finally, without evidence of what works we also do not know if there are particular groups within the target population that are not responding to community-based programming, and are particularly vulnerable.
The objective of this review was to evaluate the overall effectiveness of interventions that aim to improve the psychosocial well-being of children affected by HIV and AIDS, conducted since the original King et al (2009) review which did not identify any adequately evaluated interventions. This includes both psychological and social interventions, as well as other interventions that might have a psychosocial impact (e.g. medical interventions). Psychosocial intervention is a broad term referring to interventions that improve the psychosocial well-being of children affected by HIV/AIDS which employ either a psychological, health, general or social approach, or a combination of the two, to improve well-being (Richter et al., 2006). Psychosocial interventions thus place an emphasis on social and psychological factors rather than exclusively focusing on biological factors. Psychosocial interventions make use a wide variety of delivery methods, which can impact on individual level processes, or improve outcomes at a family, group or community level. Improved psychosocial outcomes can be as a result of psychosocial or other types of interventions, and psychosocial interventions can generate more than psychosocial effects, and other types of interventions, such as biomedical interventions may also affect psychosocial outcomes.
METHODOLOGY
The methodology utilised standardised systematic review methodology, derived from the original review, with some minor modifications based on some of the constraints of the original systematic review (King et al., 2009).
Criteria for considering studies for this review
Types of studies
The review allowed for inclusion of all intervention studies that carried out as randomized controlled trials, crossover trials, cluster-randomised trials and factorial trials. Data from well-designed non-randomised intervention studies with comparison groups were also included. Studies from both high-income countries (HIC) and low and middle income countries (LMIC) were eligible for inclusion.
Types of participants
Participants included both male and female children under the age of 18 years of age, who had lost a parent to HIV/AIDS, were living with a parent with HIV and AIDS, or were vulnerable because of other social and economic factors and living in communities of high HIV and AIDS prevalence. Reports by caregivers on young children were also eligible for inclusion.
In the King (2009) first systematic review, studies were only included if they were of children who had lost a parent due to HIV and AIDS, or were living with a parent with HIV and AIDS or another chronic illness. Furthermore, King et al. (2009) set a criterion that studies were only included if 80% of the sample could be identified as orphaned or vulnerable as a result of HIV/AIDS. These criteria were considered and questioned as researchers. Researchers may not have been able to establish causes of death or current HIV status of parents and caregivers, or may not have reported the actual percentages. This definition may have excluded more studies of children living in poverty in HIV-endemic communities. Furthermore, the first review also excluded studies based on caregiver-report outcomes. This may have led to the exclusion of studies of younger children, who may be too young to respond to interviews. Validated parent and caregiver measures are a reliable source of information about the psychosocial development of children (e.g. Warnick et al., 2008) and so for the purpose of this updated review, studies using caregiver report on child outcomes were included.
Types of interventions
We included interventions that aim to improve the psychosocial well-being of children affected by HIV/AIDS. We repeated the inclusion criteria included in the first review (King et al., 2009). Thus interventions were generally clustered under four types set out below:
Psychological interventions, such as cognitive behavioural therapy, interpersonal psychotherapy, psychodynamic therapy, non-directive counselling, psychological debriefing and problem-solving therapy.
Psychosocial support and/or care, such as play groups, homework clubs and home-based care programmes.
Physical health interventions, including medical interventions, such as antiretroviral therapy and other pharmacological interventions
Social interventions, such as economic assistance (e.g. cash transfers, work and skills training programmes) and material assistance (e.g. provision of school materials, food baskets).
We included studies that compared outcomes between groups who received an intervention and those who received usual or no care, and/or those who received a different intervention.
Types of outcome measures
Studies that included any outcome measure/s based on psychological or social well-being were included. These included studies that used the following outcome measures:
Psychological measures to record any form of mental health status
Measures of social outcomes such as school attendance, quality of life, and/or
Adverse outcomes such as suicide or incarceration
Search methods for identification of studies
This updated review was set up to include relevant studies which were identified by searching for publications between January 2008 and February 2016.
Electronic searches
The methodology utilised standardised systematic review methodology and was derived from the original review, with some minor modifications from some of the constraints of the original systematic review (King et al., 2009). We utilised search strategies on electronic data bases. Using a combination of key terms derived exactly from the previous review, we conducted an updated systematic search using PubMed, Medline, Embase, The Cochrane Library, PsycINFO, LILACS, Social Science Citation Index, Science Citation Index, the International Bibliography of Social Sciences, Web of Science.
Searching other resources
Studies were also identified in the following ways:
Searching for studies and programmatic reports found on websites of relevant organisations involved in providing services for children affected by AIDS, such as governments, non-governmental organisations, international donors and multilateral agencies.
Direct contact with funding organisations within the Coalition for Children Affected by AIDS network.
Following references in papers in short-listed studies.
Hand searching through journals published in the specified time frame that had been identified as being likely to publish papers on this topic.
Data collection and analysis
Two reviewers independently examined the titles and abstracts of all the articles identified in the search using a short checklist of inclusion criteria. In cases of doubt, the full text article was obtained and subjected to adjudication by a senior researcher on the team. From this list, the full-text versions of studies that were deemed to be potentially relevant were obtained and two reviewers independently evaluated each paper using the inclusion flow chart shown in Figure 1.
Figure 1.
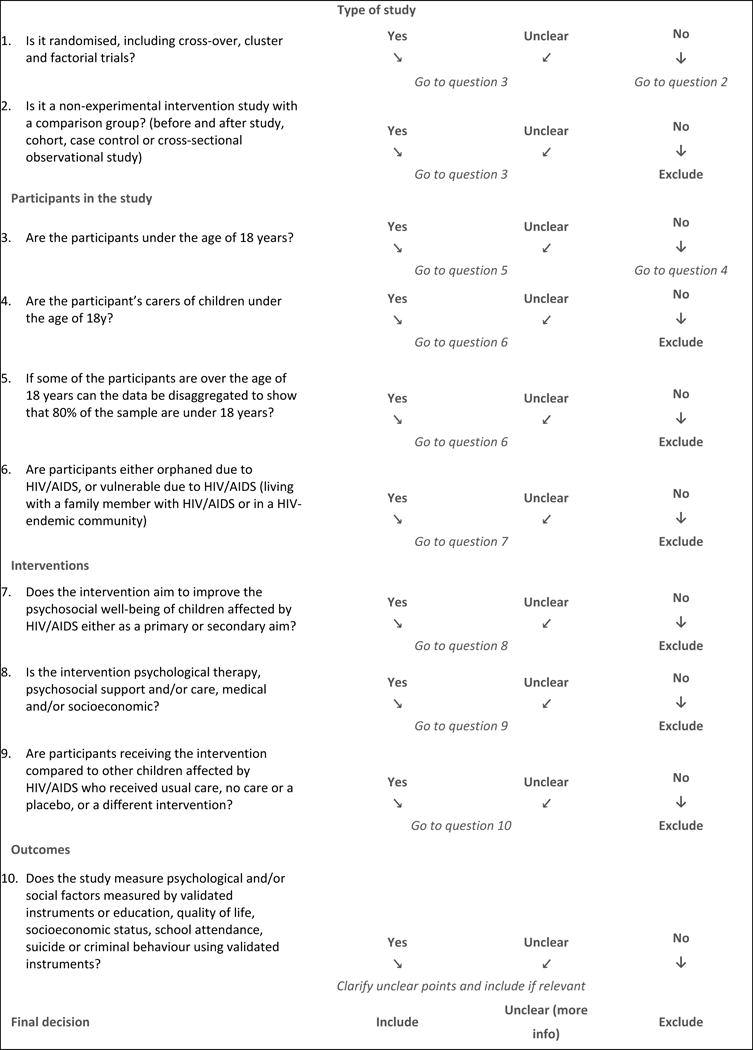
Study inclusion flow chart (adapted from King et al, 2009).
Data from each of the selected studies was entered into a specially designed database, constructed to extract study details including author, date of study, design, place of study, sample characteristics (age, gender, sample size sampling procedure, participation rate), setting (community-based, school-based, clinic-based, etc) nature of intervention, outcomes and significant findings.
RESULTS
Description of studies
The full search procedure is set out in Figure 2. We identified 17 studies that qualified for inclusion in this review. On inspection it was evident in two cases there was more than one published report of the same intervention study. In both cases we considered this as a single intervention. In one case, several papers had been written on an economic intervention which took place in Uganda, with two of these reporting on psychosocial outcomes specifically. In another case, two papers reported on outcomes from a school support intervention in Kenya, one from the first follow up point of the study and the other from a subsequent follow up.
Figure 2.
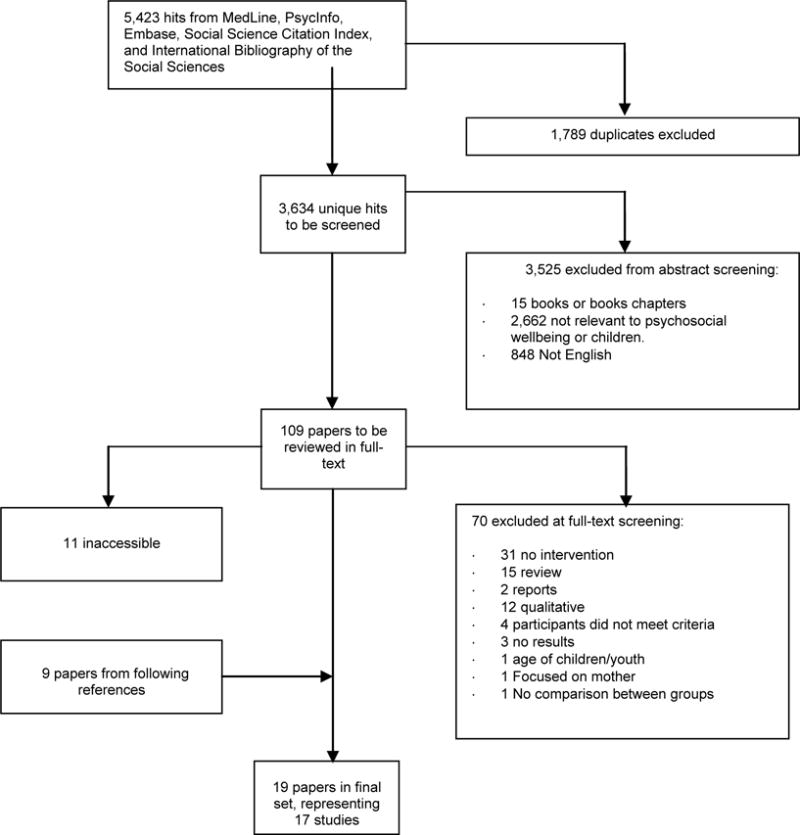
Systematic review results
Sixteen studies took place in eight low and middle income countries, and one study took place in a high income setting. All the studies except three were conducted in southern and eastern African countries. Eleven of the studies were randomized control trials. Twelve of the studies were developed specifically for research purposes and four reported on evaluations of existing and ongoing programmes.
A variety of interventions were included. Three studies reported on a psychological intervention, seven studies were of psychosocial support and/or care interventions, and six studies were of social interventions, there was one physical health intervention. Two of the interventions were focused on caregivers only, seven were child only, while seven focused on both the child and their caregiver or family (and one did not specify). The psychological and psychosocial interventions were all delivered in group-based settings. All of the social intervention studies focused on providing material support to individual children affected by HIV/AIDS, through cash transfers or school materials. The health intervention was delivered on a one-to-one basis to the child. The length of interventions varied, with some as short as 8 weeks, up to 10 months or in some cases unspecified. In addition, follow up varied from 10 weeks to 2 years.
The outcomes and outcome measures used within the studies differed considerably which prevented us from conducting a meta-analysis. Even when similar concepts were measured, different scales were utilized.
Sample selection
Sample selection varied, with some studies only including HIV-infected or AIDS orphaned children, and others including all children affected by HIV/AIDS. Eight of the studies were targeted specifically at children who were HIV positive or had HIV positive carers, whilst the others took place in communities with high HIV prevalence.
Sampling methods varied. Methods included both one-stage (individuals selected directly) and two-stage sampling (with schools or communities first selected, and then individuals selected within the cluster). At each stage, there were instances of random, systematic and convenience sampling being employed. Studies included children from the age of 2 years into early adulthood, but only one studies included children of 5 or younger. The number of studies per age is included in Figure 2. Most studies included children between the ages of 10 and 14 years, with few studies focusing on early and middle childhood, or the mid-late teen years.
Studies that did include young children did not provide an analysis of their results based on child age. Nine of the nineteen studies in this review focused more or less equally on both girls and boys. Two studies included only girls, while a further three had more than 60% of girls included in their sample. No studies focused only on boys, and two studies did not report child gender at all.
Effects of interventions
The interventions are clustered into four groups – psychological (n=3), psychosocial (n=7), social (n=6) and physical health (n=1). All three of the psychological interventions identified showed at least one positive result. Six out of seven of the psychosocial interventions, and five out of six of the social interventions also reported a positive impact, as did the physical health interventions.
Psychological interventions
All three of the psychological interventions engaged caregivers directly in their delivery. The only high-income country study was a psychological intervention targeting mothers with HIV and their children (Rotheram-Borus et al., 2012). Mothers and their children met concurrently in their own groups for some sessions, and attended joint groups at certain stages. The intervention took place twice a week over 8 weeks. For adolescents, the intervention had some positive impact in that intervention adolescents had lower frequency of use of alcohol and hard drug users, but findings were mixed in that frequency of marijuana was significantly higher in the intervention group and there were no group differences in the reduction of internalizing and externalizing behaviours over time. In Kenya, Thurman et al (2012) evaluated an ongoing support group programme for caregivers of orphans and vulnerable children. The intervention was delivered on a weekly basis in large caregiver groups. They found that support group members reported higher prosocial behavior and fewer behavioral difficulties for the children under their care and no negative psychosocial impact was reported. Eloff et al. (2014) conducted an individual randomized control trial to promote resilience of young children with HIV-positive mothers. The intervention was delivered over 24 weekly sessions, with over hald of the sessions held with caregivers and children separately and the rest held together. The focus of the sessions was to improve the well-being of the mother and child, family relationships, and to provide information about HIV/AIDS. The intervention group children showed a significant improvement in externalizing behaviors, communication and daily living skills, and no difference in internalising behviour and emotional intelligence between groups. On the other hand, children in the intervention group reported significantly higher levels of anxiety. Boys tended to gain greater benefit from the intervention than did girls.
Psychosocial interventions
Of the seven psychosocial interventions, two reported positive results, four reported mixed results, and one reported a null result. Five of the seven identified psychosocial interventions were all delivered in group-based support interventions targeted at peers.
Two family-centred psychosocial interventions were identified. Bell et al. (2008) used a family group-based intervention in South Africa, which included both caregiver and child, delivered each weekend over 10 sessions. The focus was on reducing youth HIV risk behaviors by the strengthening of family relationships, and targeting peer influences through enhancing social problem-solving and peer negotiation skills for youths. While there were differences noted between intervention and control group for AIDS transmission knowledge and stigmatizing attitudes, there was no difference between groups for psychosocial outcomes specifically. In China, Liang et al. (2014) delivered to family groups and at community level in China, was made up of six sessions with adult family members, followed by joint activities with children, and three community events, with a focus on improving family’s capacity to overcome the impact of living with HIV. Mixed results were reported, with no differences in psychological measures of self-esteem or problem behaviours between groups, but improved perceived parental care at 6 months in the intervention group compared to controls.
There were four interventions directed at children or adolescents specifically. Carlson et al (2012) report on another group-based intervention that was delivered weekly over 28 weeks, after school or on weekends, focused on increasing self- and collective efficacy through public education and community mobilization. The authors found a positive impact on different types of self-efficacy, but no difference in academic efficacy or peer resistance. Two school-based interventions were identified. Mueller et al (2009) report on using an art-based intervention to increase increasing self-esteem, self-efficacy and psychological well-being. The intervention was delivered during class over 6 months, meaning that the children received 50 or more sessions. Intervention children in this study also had significantly better self-efficacy than comparisons post-intervention, but similar levels of self-esteem, depression, and behavioural problems. In Uganda, Kumakech et al (2009) reported on a school-based group intervention delivered to groups of children only, in the form of exercise (e.g. a game or play) over a period of 10 weeks. The focus of the intervention was to reflect on the challenges of being an orphan, and to develop coping strategies to deal with these issues. Intervention children had significantly lower anxiety, depression and anger than controls, but similar levels of self esteem. Soccer was used as an intervention tool in the WhizzKids programme, which was delivered in eight sessions over 12 weeks to large groups (Balfour et al, 2013). It aimed to change attitudes towards HIV and to improve self-efficacy to make healthy choices, including the uptake of sexual health services. Intervention participants had a significantly lower likelihood of engaging in drug and alcohol use than the comparison group and lower reported HIV stigma.
Finally, in South Africa, Sherr et al. (2016) compared outcomes for children attending community-based programmes and those who were not, drawing data from two comparable studies. The community-based programmes were specifically for children affected by HIV/AIDS but had different modalities of service provision, including income, emotional, child development, medical provision or emergency support. The authors found that children in community-based programmes were less likely to experience domestic violence, suicidal ideation, depression, stigma, peer problems and conduct problems, and more likely to display prosocial behaviour. However, there was no difference in perceived parental praise or post-traumatic stress symptoms.
Social interventions
All six of the social interventions that were eligible for the review documented material assistance programmes. Three of the studies reported positive results, two studies had mixed results and one a null result (Table 2). Two of the six studies focused only on girls, while a further three enrolled approximately 60% girls in their samples. No studies focused only on boys.
Table 2.
Positive effects of interventions (interventions showing any positive effect included below)
| Psychological | Psychosocial | Social | Medical/physical |
|---|---|---|---|
|
| |||
|
|
|
|
An economic intervention tested on two different occasions in Uganda tested the impact of the Suubi Maka intervention. In the first study, the intervention group received usual care for orphaned children (counselling and education supplies) plus a comprehensive microfinance intervention consisting of matched savings accounts, financial management classes and an adult mentor for children, over 10–12 months (Ssewamala, Han and Neilands 2009, Ssewamala et al. 2012). Intervention group children had significantly better self-esteem and lower depression compared to controls at follow up. In the second study, the same intervention was delivered, in addition to ten workshops focused on starting family-based income generating activities. Children in the treatment group reported significantly lower levels of hopelessness than control children as well as significantly higher scores of self-concept (Ssewamala et al. 2016).
Similarly, a community-based conditional cash transfer intervention in Malawi to promote staying in school for girls resulted in significantly higher rates of school retention in the intervention group (Baird et al., 2010). Cash transfers were paid to households over 10 months, split between caregiver and child, conditional on school attendance record, and secondary school fees were paid to schools on behalf of families upon confirmation of enrolment. Being involved in the programme was associated with large increases in self-reported school enrolment, as well as declines in early marriage, teenage pregnancy, sexual activity, and risky sexual behavior. Two related interventions, in Zimbabwe and Kenya, tested the provision of material support for schooling, including fees and school supplies to provide comprehensive support for girls to stay in school and reduce HIV risk. In Zimbabwe, this was coupled with an assigned teacher from the girl’s school to monitor her attendance and assist with issues relating to absenteeism. In this study, girls were significantly less likely to drop out of school, engage in early marriage, while they were more likely to attend school, have higher educational aspirations and delay sexual debut. There were no differences in their perceptions in the caring of teachers and in gender equity attitudes compared to the comparison group. In Kenya, however, where teachers were replaced with visits from a female community visitor, there was no significant intervention effect 2 years post-intervention. Finally, a Zimbabwean study comparing three groups (receiving unconditional or conditional cash transfers and control group) found that receiving cash transfers was associated with significantly better schools attendance in the conditional cash transfer group, but insignificant in the unconditional group compared with controls (Robertson et al, 2013).
Physical health intervention
The only physical health intervention section looked at the impact of a massage intervention vs. play group attendance for HIV+ children. The authors found a positive impact of massage therapy on internalizing behaviour and self-help skills for children over 6y, but no impact on social development and no impact for younger children (Hernandez-Reif et al., 2008).
Measurement of outcomes
Outcome measures were diverse. Nine of the studies directly measured mental health problems, with a focus on depression, anxiety and behavioural problems, using validated tools. However, these studies used a variety of different instruments. The most commonly used measures were the Child Behaviour Checklist, used in three studies, and the Child Depression Inventory, used in three studies. Nine of the studies measured positive mental health outcomes, such as self-esteem, self-efficacy, positive behaviour and feelings of social connection. Widely different measurement tools were used for these outcomes. Only the Rosenberg Self-Esteem scale was used more than once. Finally, ten of the studies measured social outcomes, including substance use and school attendance indicators.
Studies that were not included
We found a number of studies that were relevant to the research question but that did not meet the criteria for the review. For example, a comprehensive study which took place at six different Partners in Health sites in Haiti showed that participation in a psychosocial support group for youth affected by HIV and their carers led to positive mental health and social functioning outcomes for both sets of participants (Smith Fawzi et al., 2012). No comparison between sites or with different forms of the intervention was reported, and thus this study did not meet design criteria for inclusion in our review. An evaluation of a sports project for Kenyan girls compared participants who were attending the same intervention at newly established vs. long running sites and found that girls at well-established project sites had better psychosocial outcomes, however there was limited information given about any differences in the delivery of the intervention at these sites (Woodcock, Cronin, & Forde, 2012). A study from the United States showed that accessing child development services was associated with significantly higher rates of children remaining in their family homes and not having contact with child protective services (Reich & Fuger, 2012). This study focused particularly on mothers who were substance users or HIV+, however, only 2 of the 17 sites in the study focused on HIV-affected families, and HIV prevalence rates were not reported.
Other studies of intervention for children affected by HIV/AIDS were identified that focused on outcomes that beyond the scope of this review, due to the specific focus on psychological or social outcomes. For example, we located two studies from the same home-based visiting programme in South Africa which showed that undernourished children who are recipients of a home-visiting programme are more likely to achieve healthy weights for their age than controls (le Roux et al., 2010, 2011). We also found that several studies focused purely on improving knowledge about HIV transmission and reducing risky sexual behaviour, which fell beyond the scope of our review and has been investigated separately (e.g. Medley et al. 2009). Finally, we also found studies that made use of psychological intervention, but which only reported child survival outcomes. Van Winghem et al (2008) describe an intervention in Kenya which employed a range of techniques, including the provision of psycho-social support with HAART services, to significantly improve child survival rates for children under 15 who were receiving anti-retroviral treatment. Similarly, Grimwood et al. (2012) report on a community-based adherence support programme that improved retention in care of children in antiretroviral therapy services. Children in the intervention group received visits from Patient Advocates, who worked in designated geographical areas to provide psychosocial support to children’s caregivers, monitored medication taking, and helped families to identify and address barriers to adherence in the home.
DISCUSSION
In contrast to the earlier review on this topic, we identified a growing set of interventions to improve the psychosocial well-being of children affected by HIV/AIDS, most of which took place in low and middle income countries. More specifically, the majority took place in eastern and southern Africa where the burden of HIV is greatest. This increase in the evaluation of interventions is promising, and shows that there has been a shift towards the prioritization of generating evidence in this area.
There are lessons to be learned from the identified studies. In the final set of identified studies, most studies showed at least one significant benefit of the intervention on psychosocial outcomes, with only two showing no difference between those receiving the intervention and a control or comparison group. While it is possible that this reflects a publication bias towards positive outcome reporting, most of the studies reported mixed results. Overall, psychological changes noted for children included the reduction in internalizing and externalizing behaviours, decrease in symptoms of depression, anger, and anxiety, and higher rates of prosocial behaviour, self-help abilities and communication. Positive social outcomes that were recorded included retention in school, better school attendance, and less early marriage. There was no clear pattern in terms of type of intervention, target recipient, length of intervention, length of follow up, or intensity of delivery, but each of the four different types of intervention (psychological, psychosocial, social, and physical health) showed at least one positive benefit on child psychosocial wellbeing. It is also interesting to note that interventions targeting the child only, caregiver only, caregiver and child together and entire family all showed some positive impact.
However, it is important to note that the identified studies differed greatly and there are already emerging gaps in the existing database. Firstly, sampling techniques used were diverse. Some studies employed random community-based sampling techniques or random sampling of schools, and others used convenience sampling selecting participants from registers of children or adults seeking treatment for HIV. These reflect the ‘real life’ contexts in which these studies took place, but may also mean that some study results have not accurately represent the study population (Suresh, Thomas and Suresh 2011). Inclusion criteria also varied, with eight of the studies targeted specifically at children who were HIV positive or had HIV positive carers. The remainder of the studies used a broader approach, and included all potentially vulnerable children within the study population. This is promising, as definitions of vulnerability shift from focusing purely on HIV child and carer diagnosis to looking at the broader social context which places children at risk in an era of HIV/AIDS (Sherr et al., 2008). Studies were also more likely to include girls and children aged 10–14 years. In particular, research on younger children was particularly scarce. Given the impact of HIV on early child development (ECD) outcomes, there is a need to prioritise the evaluation of these types of interventions targeted at children affected by HIV/AIDS (Chandan and Richter 2009). In terms of gender, recent research on children affected by HIV has shown that while girls often bear the brunt of additional caregiving, boys may be worse off in terms of exposure to violence and related externalizing behaviours (Hensels et al., 2016). Gender issues are rarely discussed in child HIV research, for example, UNAIDS does not provide a breakdown of child data by gender until early adolescence or adulthood (UNAIDS 2015). It is thus important that we continue to include both boys and girls in programming and research, and that we endeavor to find a balance between promoting equity for girls in these efforts, and ensuring that boys are included.
Secondly, studies showed wide variation in outcome measurement, meaning that for this review, it was difficult to compare outcomes across studies. This is partly due to the broad nature of psychosocial interventions and outcomes. Most studies focused on mental health problems, but some included positive measurement of mental well-being and other social factors. School retention was widely used as a social measure of well-being. The variety of measures used may relate to the broader problem of a lack of standardized outcome measurement tools for child-related research in low and middle income countries, and in sub-Saharan Africa in particular (Holding et al. 2004). Globally, there are no accepted indicators or frameworks to measure child development, partially due to concerns about training and administration of tools and cultural differences between different groups (Engle et al. 2007). A recommended set of measurements or a database of tools available for programmers and researchers to draw from would make evaluation studies more comparable.
Thirdly, study design also varied. For example, some studies had as much as two years follow up time, but in most cases follow ups were confined to immediate post-intervention assessments. This may have affected the reported results of the identified studies. For example, in Hallfors et al. (2012) the length of follow up was shown to be crucial in understanding the impact of the intervention. The material support intervention that the authors described showed a positive impact after one year, but the impact had disappeared by two years post-intervention. Similarly, the Thinking Healthy programme in Pakistan improved maternal and infant outcomes, but a longer term follow up when the children were aged 7 years showed no impact of the intervention (Maselko et al. 2015). Programmers and researchers should be encouraged to include longer-term follow ups in the designs of their studies. The Blueprints for Healthy Youth Development registry of evidence-based positive child and youth development programs (Mihalic and Elliott 2015) requires a follow up period of at least one year beyond the end of the intervention, which is likely to be feasible for psychosocial programmes for children affected by HIV who are often operating in short funding cycles.
Surprisingly, given the community contexts of the studies in this review, 11 out of the 19 studies included were randomized control trials. This is a positive finding, given that randomised controlled trials are the gold standard for intervention evaluation and provide the best evidence of a programme’s effectiveness (Campbell and Russo 1999). On the other hand, only four of the studies in the review were of existing, real-life programmes, meaning that the rest were developed specifically for research purposes only. This is likely due to the challenges of evaluating these types of community-based programmes, where study methodology often needs to fit into the reality of how programmes are delivered. As a result, it will be important to assess issues of context and implementation for these programmes before scale up of these interventions can be recommended. In addition, increased investment in promoting partnerships between programmers and researchers is required. There are good examples of collaboration where strong study designs can be integrated into existing programming without compromising intervention delivery. One example is the Philani Maternal, Child Health and Nutrition Project, a non-governmental organization that provides home visits through its Mentor Mother programme to pregnant women, new mothers and their infants. They have been engaged in a collaborative project with researchers over several years to assess the impact of their intervention, using a cluster randomized controlled trial (Rotheram-Borus et al. 2011, Rotheram-Borus et al. 2014).
This study has shown that there are effective and proven programmes to improve outcomes for children affected by HIV/AIDS. Funders and NGO partners should undertake to share these lessons learnt with their community-level partners and find ways to make these stories of success accessible to different stakeholders in these programmes. It is imperative that there are ongoing efforts to support community-based programmes in their work to improve the psychosocial well-being of their children. Funders and NGOs should continue to develop their research capacity, in partnership with researchers, to find innovative solutions to measuring their impact.
Conclusion
Efforts to improve evaluation of interventions to improve the psychosocial well-being of children affected by HIV/AIDS have resulted in a number of new studies which met the inclusion criteria for the review. However, studies are highly heterogenous, employing different methods of implementation and evaluation, meaning that it is difficult to compare them. Existing evaluation studies should be broadly disemmindated and programmers should take account of the existing evidence which shows that different types of interventions can have an impact on psychosocial outcomes, including material or financial support. Finally, we call for increased partnerships between policy-makers, practitioners and researchers in order to design evaluation studies that are comparable and can feed into the growing evidence base.
Figure 3.
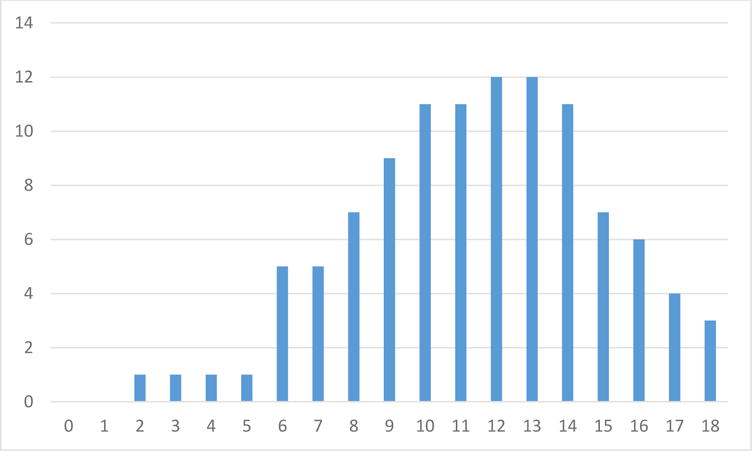
Number of studies per age year
Table 1.
| Year | Author | Country | Study Design | Sample | Intervention | Outcomes | Results |
|---|---|---|---|---|---|---|---|
| Psychological | |||||||
| 2012 | Rotheram-Borus et al., 2012 | USA | Randomized control trial | 339 mothers with HIV and 259 of their school-age children, children aged 6–20 years, mean age 15y. | Group, bi-weekly, mother and adolescent sessions, 8 weeks. | Internalising and externalising behaviours, school attendance, grades, problem behaviour | Mixed - alcohol and hard drug use reduced marijuana use increased in intervention group. No difference in internalising and externalising behaviours. |
| 2012 | Thurman, et al., 2012 | Kenya | Cross-sectional post-intervention design. | 766 caregivers and 1028 children aged 8 – 14 years. | Group, weekly, ongoing intervention for caregivers | Child psychosocial well-being: emotional and behavioural problems, prosocial behaviour | Higher prosocial behaviour and fewer behavioural problems. |
| 2014 | Eloff et al (2014) | South Africa | Randomised clinical trial. | HIV positive mothers and their children. 390 mother-child pairs. Children 6–10y. | Group, weekly, caregivers and children, 24 weeks in duration | Children’s behaviour (internalising and externalising problems), adaptive functioning, depressive symptoms, anxiety, emotional intelligence | Decreased externalising problems, improved communication and daily living skills, no difference for internalising behviour and emotional intelligence, negative outcome for anxiety. |
| Psychosocial | |||||||
| 2014 | Liang et al., 2014 | China | Cluster randomized design. Interviews were administered at baseline, 3 and 6 months. | 79 families in four village clusters. Participants: (1) with confirmation of an AIDS diagnosis or HIV-positive status; (2) having a seronegative family member living at home; and (3) having at least one child aged 6 to 18 years living with a PLH participant. Two age groups of children (6–12 and 13–18 years) were included in the study. | Family groups and community events. | Children’s self-esteem, perceived parental care, and problem behaviour | No difference in self-esteem or problem behaviour, increased in perception of parental care |
| 2008 | Bell et al., 2008 | South Africa | Randomized control trial | 281 intervention and 298 control children, aged 9 to 14y. Being reared by an adult caregiver age >18 years that fulfills parenting responsibilities, enrolled in school, and indicated agreement to participate in the study via caregiver consent and child assent. | Group, caregiver and child, weekly, 10 sessions. | Anxiety, AIDS transmission knowledge, stigma, Psychological autonomy, range of parenting skills | No differences between groups in child psychosocial outcomes |
| 2009 | Kumakech et al., 2009 | Uganda | Cluster randomised control trial | 326 AIDS ‘orphans’ (lost one or both parents to HIV/AIDS) aged 10–15y | Groups, children in school, 10 weeks. | self-concept, anxiety, anger, and depression | Lower anxiety, depression and anger. |
| 2011 | Mueller et al., 2011 | South Africa | Quasi-experimental, cross-sectional post-intervention | 177 intervention group and 120 control group children aged 8–18 years. | Groups, children in school, 50 or more sessions over 6 months. Focus on increasing self-esteem, self-efficacy and psychological well-being. | self-esteem, self-efficacy, child depression was, emotional–behavioural problems | No differences in depression, emotional and behavioural problems and self-esteem, but increase self-efficacy. |
| 2012 | Carlson et al., 2012 | Tanzania | Cluster randomised control trial | 726 children, aged 9–14y. | Group, adolescents, weekly, 28 weeks | Five aspects of self-efficacy | Improvements in deliberative self efficacy, communicative self efficacy and emotional control, no difference in academic efficacy or peer resistance. |
| 2016 | Sherr et al., 2016 | South Africa | Longitudinal study | 1848 children aged 9–13 years old from South Africa and Malawi who were either CBO attenders or had not received CBO support (control group) | Range of different community-based programmes for children affected by HIV/AIDS with different modalities of provision | Depressive symptoms, suicide ideation, post-traumatic symptoms, harsh discipline, perceived praise for child | Less suicidal ideation, depression, stigma, domestic violence, peer problems and conduct problems, and improved prosocial behaviour. No difference in perceived parental praise or post-traumatic stress symptoms. |
| 2013 | Balfour et al., 2013 | South Africa | Quasi experimental design | 629 participants, age range not reported | Group sport, children, eight sessions over 12 weeks. | HIV stigma, substance use. | Lower HIV stigma and drug use. |
| Social | |||||||
| 2011 | Hallfors et al., 2011 | Zimbabwe | Randomised control trial | 329 girls in Grade 6 in 25 schools (ages range 10–16 years) | Individual material support, child and family support, duration not specified | Child perceptions of caring adults, school dropout, educational aspiration, gender equity, attitudes towards sex, sexual debut, marital status, pregnancy | Reduced school drop out, early marriage and increased school attendance, educational aspiration, and delayed sexual debut. No differeence for perceptions of caring of teachers and gender equity. |
| 2012 | Cho et al, 2011 and Hallfors, et al., 2012 | Kenya | Randomized control trial. 2 year follow up. | 105 children, 11–14y | Ongoing programme delivered on an individual level to learners to provide material support for school supplies, as well as visits from a female community visitor, as a means to provide comprehensive support for girls to stay in school and reduce HIV risk. | School absence, perceptions of caring adults, school dropout, educational aspiration, future expectations, gender equity, attitudes towards sex | No differences between groups. |
| 2010 | Baird et al., 2010 | Malawi | Quasi-experimental, intervention and control group | 1225 adolescent girls, 13–22 years old (mean <18) | Cash transfers paid to households over 10 months, split between caregiver and child, conditional on school attendance record, and secondary school fees paid to schools upon confirmation of enrolment. | school attendance, early marriage | Increased school enrolment, reduced early marriage, pregnancy, sexual activitity, risky sexual behaviour. |
| 2009, 2010, 2012 | Ssewamala et al 2009; 2010; 2012 | Uganda | Randomised control trial | 2009: 267; 2010: 260, 2012: 286. Mean age 13.71. | Intervention group received usual care for orphaned childrne (counselling and education supplies) plus a comprehensive microfinance intervention consisting of matched savings accounts, financial management classes and an adult mentor for children. Duration between 10 and 12 months. | Depression, self-esteem | Reduced depression, higher self-esteem |
| 2013 | Robertson et al., 2013 | Zimbabwe | Cluster randomized control trial | 5172 children aged 6–12y in 4043 households | Comparison of conditional and unconditional cash transfers delivered at household level over 12 months. UC and CC groups received same cash amounts, but CC group had to comply with various conditions, including applying for a birth certificate, vaccinations, attending parenting classes and others. | School attendance for 6–12 year olds and other non-relevant outcomes | Increased school attendance |
| 2016 | Ssewamala et al., (2015) | Southern Uganda | Quasi-experimental design (schools randomised, not individuals) | 317 AIDS-orphaned adolescents | An further study of the Suubi Maka intervention focused on matched savings for promoting monetary savings for educational opportunities for children, financial management workshops and family level income generating projects, and providing mentors to children (one mentorship meeting per month for the 12-month intervention period), and an additional 10 workshops about starting family-based income generating activities. | Hopelessness and self concept | Lower levels of hopelessness, higher self-concept. |
| Physical health | |||||||
| 2008 | Hernandez-Reif et al., 2008 | Dominican Republic | Randomized control trial | 52 HIV infected children, data for 48 children reported, 2–8y. | Bi-weekly massage sessions or group play sessions, 12 weeks. | Internalizing and externalizing problems, self-help age, social age. | Children under 6y no differences between group but positive results for internalising and self help for children over 6y, negative for social development. |
Acknowledgments
To all those who contributed and supported developing this manuscript including: Steward Hird, Latoya Idele and Camilla Braine.
References
- Abubakar A, Van Baar A, Van de Vijver FJR, Holding P, Newton CRJC. Paediatric HIV and neurodevelopment in sub-Saharan Africa: a systematic review. Tropical Medicine & International Health: TM & IH. 2008;13(7):880–887. doi: 10.1111/j.1365-3156.2008.02079.x. [DOI] [PubMed] [Google Scholar]
- Akwara PA, Noubary B, Lim Ah Ken P, Johnson K, Yates R, Winfrey W, Luo C. Who is the vulnerable child? Using survey data to identify children at risk in the era of HIV and AIDS. AIDS Care. 2010;22(9):1066–1085. doi: 10.1080/09540121.2010.498878. [DOI] [PubMed] [Google Scholar]
- Baird S, Chirwa E, McIntosh C, Ozler B. The short-term impacts of a schooling conditional cash transfer program on the sexual behavior of young women. Health Economics. 2010;19(Suppl):55–68. doi: 10.1002/hec.1569. [DOI] [PubMed] [Google Scholar]
- Balfour L, Farrar T, McGilvray M, Wilson D, Tasca GA, Spaans JN, et al. HIV prevention in action on the football field: The Whizzkids United Program in South Africa. AIDS and Behavior. 2013;17(6):2045–2052. doi: 10.1007/s10461-013-0448-6. [DOI] [PubMed] [Google Scholar]
- Bass JK, Nakasujja N, Familiar-Lopez I, Sikorskii A, Murray SM, Opoka R, Augustinavicius J, Boivin MJ. Association of caregiver quality of care with neurocognitive outcomes in HIV-affected children aged 2–5 years in Uganda. AIDS Care. 2016 Mar;28(Suppl 1):76–83. doi: 10.1080/09540121.2016.1146215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bell CC, Bhana A, Petersen I, McKay MM, Gibbons R, Bannon W, Amatya A. Building Protective Factors to Offset Sexually Risky Behaviors among Black Youths. Journal of the National Medical Association. 2008;100(8):936–944. doi: 10.1016/s0027-9684(15)31408-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belsey MA, Sherr L. The definition of true orphan prevalence: Trends, contexts and implications for policies and programmes. Vulnerable Children and Youth Studies. 2011;6(3):185–200. doi: 10.1080/17450128.2011.587552. [DOI] [Google Scholar]
- Betancourt TS, Meyers-Ohki SE, Charrow A, Hansen N. Research Review: Mental health and resilience in HIV/AIDS-affected children: a review of the literature and recommendations for future research. Journal of Child Psychology and Psychiatry, and Allied Disciplines. 2012 doi: 10.1111/j.1469-7610.2012.02613.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown JL, Sales JM, DiClemente RJ. Combination HIV prevention interventions: the potential of integrated behavioral and biomedical approaches. Curr HIV/AIDS Rep. 2014 Dec;11(4):363–75. doi: 10.1007/s11904-014-0228-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bryant M, Beard J, Sabin L, Brooks MI, Scott N, Larson BA, Simon J. PEPFAR’s Support For Orphans And Vulnerable Children: Some Beneficial Effects, But Too Little Data, And Programs Spread Thin. Health Affairs. 2012;31(7):1508–1518. doi: 10.1377/hlthaff.2012.0230. [DOI] [PubMed] [Google Scholar]
- Campbell C, Cornish F. How can community health programmes build enabling environments for transformative communication? Experiences from India and South Africa. AIDS Behav. 2012;16:847–57. doi: 10.1007/s10461-011-9966-2. [DOI] [PubMed] [Google Scholar]
- Campbell DT, Russo JJ. Social experimentation. Thousand Oaks, CA: Sage; 1999. [Google Scholar]
- Carlson M, Brennan RT, Earls F. Enhancing adolescent self-efficacy and collective efficacy through public engagement around HIV/AIDS competence: a multilevel, cluster randomized-controlled trial. Social Science & Medicine (1982) 2012;75(6):1078–1087. doi: 10.1016/j.socscimed.2012.04.035. [DOI] [PubMed] [Google Scholar]
- Casale M, Crankshaw T. “They laugh when I sing”: perceived effects of caregiver social support on child wellbeing among South African caregivers of children. J Child Adolesc Ment Health. 2015;27(2):149–55. doi: 10.2989/17280583.2015.1067216. [DOI] [PubMed] [Google Scholar]
- Casale M. The importance of family and community support for the health of HIV-affected populations in Southern Africa: what do we know and where to from here? Br J Health Psychol. 2015 Feb;20(1):21–35. doi: 10.1111/bjhp.12127. [DOI] [PubMed] [Google Scholar]
- Chandan U, Richter L. Strengthening families through early intervention in high HIV prevalence countries. AIDS Care. 2009;21:76–82. doi: 10.1080/09540120902923097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chi P, Li X, Tam CC, Du H, Zhao G, Zhao J. Parenting Mediates the Impact of Caregivers’ Distress on Children’s Well-Being in Families Affected by HIV/AIDS. AIDS Behav. 2015 Nov;19(11):2130–9. doi: 10.1007/s10461-015-1104-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chibanda D, Cowan FM, Healy JL, Abas M, Lund C. Psychological interventions for Common Mental Disorders for People Living With HIV in Low- and Middle-Income Countries: systematic review. Trop Med Int Health. 2015 Jul;20(7):830–9. doi: 10.1111/tmi.12500. [DOI] [PubMed] [Google Scholar]
- Cluver L, Gardner F. The mental health of children orphaned by AIDS: a review of international and southern African research. Journal of Child & Adolescent Mental Health. 2007;19(1):1–17. doi: 10.2989/17280580709486631. [DOI] [PubMed] [Google Scholar]
- Cluver L, Operario D. Inter-generational Linkages of AIDS: Vulnerability of Orphaned Children for HIV Infection. IDS Bulletin. 2008;39(5):27–35. doi: 10.1111/j.1759-5436.2008.tb00492.x. [DOI] [Google Scholar]
- Cluver LD, Orkin FM, Boyes ME, Sherr L. Cash plus care: social protection cumulatively mitigates HIV-risk behaviour among adolescents in South Africa. AIDS. 2014 Jul;28(Suppl 3):S389–97. doi: 10.1097/QAD.0000000000000340. [DOI] [PubMed] [Google Scholar]
- Desmond C, Bruce F, Tomlinson M, Marlow MB, Aber JL, Ouifki R, Welte A. Modelling the long-term impacts on affected children of adult HIV: benefits, challenges and a possible approach. AIDS. 2014 Jul;28(Suppl 3):S269–75. doi: 10.1097/QAD.0000000000000329. [DOI] [PubMed] [Google Scholar]
- Eloff I, Finestone M, Makin JD, Boeving-Allen A, Visser M, Ebersohn L, et al. A randomized clinical trial on an intervention to promote resilience in young children of HIV-positive mothers in South Africa. AIDS 2014. 2014;28(Suppl 3):S347–S357. doi: 10.1097/QAD.0000000000000335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Engle PL, Fernald LC, Alderman H, Behrman J, O’Gara C, Yousafzai A, Iltus S. Strategies for reducing inequalities and improving developmental outcomes for young children in low-income and middle-income countries. The Lancet. 2011;378(9799):1339–1353. doi: 10.1016/S0140-6736(11)60889-1. [DOI] [PubMed] [Google Scholar]
- Grimwood A, Fatti G, Mothibi E, Malahlela M, Shea J, Eley B. Community adherence support improves programme retention in children on antiretroviral treatment: A multicentre cohort study in South Africa. Journal of the International AIDS Society. 2012;15:17381. doi: 10.7448/IAS.15.2.17381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo Y, Li X, Sherr L. The impact of HIV/AIDS on children’s educational outcome: A critical review of global literature. AIDS Care. 2012;24(8):993–1012. doi: 10.1080/09540121.2012.668170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hallfors D, Cho H, Rusakaniko S, Iritani B, Mapfumo J, Halpern C. Supporting adolescent orphan girls to stay in school as HIV risk prevention: evidence from a randomized controlled trial in Zimbabwe. American Journal of Public Health. 2011;101(6):1082–1088. doi: 10.2105/AJPH.2010.300042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hallfors DD, Cho H, Mbai I, Milimo B, Itindi J. Process and outcome evaluation of a community intervention for orphan adolescents in western Kenya. Journal of Community Health. 2012;37(5):1101–1109. doi: 10.1007/s10900-012-9548-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han CK, Ssewamala FM, Wang JSH. Family economic empowerment and mental health among AIDS-affected children living in AIDS-impacted communities: evidence from a randomised evaluation in southwestern Uganda. Journal of Epidemiology and Community Health. 2013;67(3):225–230. doi: 10.1136/jech-2012-201601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hernandez-Reif M, Shor-Posner G, Baez J, Soto S, Mendoza R, Castillo R, Zhang G. Dominican Children with HIV Not Receiving Antiretrovirals: Massage Therapy Influences their Behavior and Development. Evidence-Based Complementary and Alternative Medicine. 2008;5(3):345–354. doi: 10.1093/ecam/nem032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holding PA, Taylor HG, Kazungu SD, Mkala T, Gona J, Mwamuye B, Mbonani L, Stevenson J. Assessing cognitive outcomes in a rural African population: development of a neuropsychological battery in Kilifi District, Kenya. J Int Neuropsychol Soc. 2004;10:246–60. doi: 10.1017/S1355617704102166. [DOI] [PubMed] [Google Scholar]
- JLICA. Final Report of the Joint Learning Initiative on Children and HIV/AIDS 2009 [Google Scholar]
- Kaljee L, Zhang L, Langhaug L, Munjile K, Tembo S, Menon A, Stanton B, Xiaoming L, Malungo J. A randomised-control trial for the teachers’ diploma programme on psychosocial care, support and protection in Zambian government primary schools. Psychology, Health and Medicine. 2016:1–12. doi: 10.1080/13548506.2016.1153682. [DOI] [PubMed] [Google Scholar]
- King E, De Silva M, Stein A, Patel V. Interventions for improving the psychosocial well-being of children affected by HIV and AIDS In Cochrane Database of Systematic Reviews. John Wiley & Sons, Ltd; 2009. Retrieved from http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD006733.pub2/abstract. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumakech E, Cantor-Graae E, Maling S, Bajunirwe F. Peer-group support intervention improves the psychosocial well-being of AIDS orphans: Cluster randomized trial. Social Science & Medicine. 2009;68(6):1038–1043. doi: 10.1016/j.socscimed.2008.10.033. [DOI] [PubMed] [Google Scholar]
- Le Roux IM, le Roux K, Comulada WS, Greco EM, Desmond KA, Mbewu N, Rotheram-Borus MJ. Home visits by neighborhood Mentor Mothers provide timely recovery from childhood malnutrition in South Africa: results from a randomized controlled trial. Nutrition Journal. 2010;9:56. doi: 10.1186/1475-2891-9-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Le Roux IM, le Roux K, Mbeutu K, Comulada WS, Desmond KA, Rotheram-Borus MJ. A randomized controlled trial of home visits by neighborhood mentor mothers to improve children’s nutrition in South Africa. Vulnerable Children and Youth Studies. 2011;6(2):91–102. doi: 10.1080/17450128.2011.564224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li L, Liang LJ, Ji G, Wu J, Xiao Y. Effect of a family intervention on psychological outcomes of children affected by parental HIV. AIDS and Behavior. 2014;18:2051–2058. doi: 10.1007/s10461-014-0744-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Louw KA, Ipser J, Phillips N, Hoare J. Correlates of emotional and behavioural problems in children with perinatally acquired HIV in Cape Town, South Africa. AIDS Care. 2016 Feb;5:1–9. doi: 10.1080/09540121.2016.1140892. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- Maselko J, Sikander S, Bhalotra S, Bangash O, Ganga N, Mukherjee S, Egger H, Franz L, Bibi A, Liaqat R, Kanwal M, Abbasi T, Noor M, Ameen N, Rahman A. Effect of an early perinatal depression intervention on long-term child development outcomes: follow-up of the Thinking Healthy Programme randomised controlled trial. Lancet Psychiatry. 2015;2:609–17. doi: 10.1016/S2215-0366(15)00109-1. [DOI] [PubMed] [Google Scholar]
- Medley A, Kennedy C, O’Reilly K, Sweat M. Effectiveness of Peer Education Interventions for HIV Prevention in Developing Countries: A Systematic Review and Meta-Analysis. AIDS Education and Prevention. 2009;21(3):181–206. doi: 10.1521/aeap.2009.21.3.181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mihalic SF, Elliott DS. Evidence-based programs registry: blueprints for Healthy Youth Development. Eval Program Plann. 2015;48:124–31. doi: 10.1016/j.evalprogplan.2014.08.004. [DOI] [PubMed] [Google Scholar]
- Mueller J, Alie C, Jonas B, Brown E, Sherr L. A quasi-experimental evaluation of a community-based art therapy intervention exploring the psychosocial health of children affected by HIV in South Africa. Tropical Medicine & International Health: TM & IH. 2011;16(1):57–66. doi: 10.1111/j.1365-3156.2010.02682.x. [DOI] [PubMed] [Google Scholar]
- Mutumba M, Bauermeister JA, Elkington KS, Bucek A, Dolezal C, Leu CS, Mellins CA. A Prospective Longitudinal Study of Mental Health Symptoms Among Perinatally HIV-Infected and HIV-Exposed but Uninfected Urban Youths. J Adolesc Health. 2016 Apr;58(4):460–6. doi: 10.1016/j.jadohealth.2015.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reich WA, Fuger KL. Accessing child developmental services predicts in-home placement of substance- and HIV-affected children. Children and Youth Services Review. 2012;34(12):2474–2480. [Google Scholar]
- Richter L, Foster G, Sherr L. Where the heart is: meeting the psychosocial needs of young children in the context of HIV/AIDS. 2006:54. [Google Scholar]
- Richter LM, Sherr L, Adato M, Belsey M, Chandan U, Desmond C, Wakhweya A. Strengthening families to support children affected by HIV and AIDS. AIDS Care. 2009;21(sup1):3–12. doi: 10.1080/09540120902923121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robertson L, Mushati P, Eaton JW, Dumba L, Mavise G, Makoni J, Gregson S. Effects of unconditional and conditional cash transfers on child health and development in Zimbabwe: a cluster-randomised trial. The Lancet. 2013;381(9874):1283–1292. doi: 10.1016/S0140-6736(12)62168-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rotheram-Borus MJ, Rice E, Comulada WS, Best K, Elia C, Peters K, Valladares E. Intervention Outcomes Among HIV-Affected Families Over 18 Months. AIDS and Behavior. 2012;16(5):1265–1275. doi: 10.1007/s10461-011-0075-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rotheram-Borus MJ, le Roux IM, Tomlinson M, Mbewu N, Comulada WS, le Roux K, Stewart J, O’Connor MJ, Hartley M, Desmond K, Greco E, Worthman CM, Idemundia F, Swendeman D. Philani Plus (+): a Mentor Mother community health worker home visiting program to improve maternal and infants’ outcomes. Prev Sci. 2011;12:372–88. doi: 10.1007/s11121-011-0238-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rotheram-Borus MJ, Tomlinson M, le Roux IM, Harwood JM, Comulada S, O’Connor MJ, Weiss RE, Worthman CM. A cluster randomised controlled effectiveness trial evaluating perinatal home visiting among South African mothers/infants. PLoS One. 2014;9:e105934. doi: 10.1371/journal.pone.0105934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherr L, Cluver LD, Betancourt TS, Kellerman SE, Richter LM, Desmond C. Evidence of impact: health, psychological and social effects of adult HIV on children. AIDS. 2014 Jul;28(Suppl 3):S251–9. doi: 10.1097/QAD.0000000000000327. [DOI] [PubMed] [Google Scholar]
- Sherr L, Mueller J, Varrall R. A systematic review of cognitive development and child human immunodeficiency virus infection. Psychology, Health & Medicine. 2009;14(4):387–404. doi: 10.1080/13548500903012897. [DOI] [PubMed] [Google Scholar]
- Sherr L, Varrall R, Mueller J, Richter L, Wakhweya A, Adato M, Desmond C. A systematic review on the meaning of the concept “AIDS Orphan”: confusion over definitions and implications for care. AIDS Care. 2008;20(5):527–536. doi: 10.1080/09540120701867248. [DOI] [PubMed] [Google Scholar]
- Sherr L, Yakubovich AR, Skeen S, Cluver LD, Hensels IS, et al. How Effective Is Help on the Doorstep? A Longitudinal Evaluation of Community-Based Organisation Support. PLoS ONE. 2016;11(3):e0151305. doi: 10.1371/journal.pone.0151305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherr L, Zoll M. PEPFAR OVC evaluation: How good at doing good. Washington, DC: United States Agency for International Development; 2011. [Google Scholar]
- Sikkema KJ, Dennis AC, Watt MH, Choi KW, Yemeke TT, Joska JA. Improving mental health among people living with HIV: a review of intervention trials in low- and middle-income countries. Glob Ment Health (Camb) 2015 Jan;2:e19. doi: 10.1017/gmh.2015.17. pii. Epub 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith Fawzi MC, Eustache E, Oswald C, Louis E, Surkan PJ, Scanlan F, Mukherjee JS. Psychosocial support intervention for HIV-affected families in Haiti: implications for programs and policies for orphans and vulnerable children. Social Science & Medicine (1982) 2012;74(10):1494–1503. doi: 10.1016/j.socscimed.2012.01.022. [DOI] [PubMed] [Google Scholar]
- Ssewamala FM, Han CK, Neilands TB. Asset Ownership and Health and Mental Health Functioning Among AIDS-Orphaned Adolescents: Findings From a Randomized Clinical Trial in Rural Uganda. Social Science & Medicine (1982) 2009;69(2):191. doi: 10.1016/j.socscimed.2009.05.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ssewamala FM, Neilands TB, Waldfogel J, Ismayilova L. The impact of a comprehensive microfinance intervention on depression levels of AIDS-orphaned children in Uganda. The Journal of Adolescent Health: Official Publication of the Society for Adolescent Medicine. 2012;50(4):346–352. doi: 10.1016/j.jadohealth.2011.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ssewamala FM, Karimli L, Torsten N, Wang JS, Han CK, Ilic V, Nabunya P. Applying a family-level economic strengthening intervention to improve education and health-related outcomes of school-going AIDS-orphaned children: Lessons from a randomized experiment in Southern Uganda. Prevention Science. 2015;17(1):134–143. doi: 10.1007/s11121-015-0580-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein A, Desmond C, Garbarino J, Van IJzendoorn MH, Barbarin O, Black MM, Stein AD, Hillis SD, Kalichman SC, Mercy JA, Bakermans-Kranenburg MJ, Rapa E, Saul JR, Dobrova-Krol NA, Suresh K, Thomas SV, Suresh G. Design, data analysis and sampling techniques for clinical research. Ann Indian Acad Neurol. 2011:287–90. doi: 10.4103/0972-2327.91951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richter LM. Predicting long-term outcomes for children affected by HIV and AIDS: perspectives from the scientific study of children’s development. AIDS. 2014 Jul;28(Suppl 3):S261–8. doi: 10.1097/QAD.0000000000000328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas F. Stigma, fatigue and social breakdown: Exploring the impacts of HIV/AIDS on patient and carer well-being in the Caprivi Region, Namibia. Social Science & Medicine. 2006;63(12):3174–3187. doi: 10.1016/j.socscimed.2006.08.016. [DOI] [PubMed] [Google Scholar]
- Thurman TR, Jarabi B, Rice J. Caring for the caregiver: evaluation of support groups for guardians of orphans and vulnerable children in Kenya. AIDS Care. 2012;24(7):811–819. doi: 10.1080/09540121.2011.644229. [DOI] [PubMed] [Google Scholar]
- UNAIDS. Children and AIDS Fifth Stocktaking Report. Geneva: UNAIDS; 2010. [Google Scholar]
- Vreeman RC, Scanlon ML, McHenry MS, Nyandiko WM. The physical and psychological effects of HIV infection and its treatment on perinatally HIV-infected children. J Int AIDS Soc. 2015 Dec 2;18(Suppl 6):20258. doi: 10.7448/IAS.18.7.20258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walker SP, Wachs TD, Grantham-McGregor S, Black MM, Nelson CA, Huffman SL, Richter L. Inequality in early childhood: risk and protective factors for early child development. The Lancet. 2011;378(9799):1325–1338. doi: 10.1016/S0140-6736(11)60555-2. [DOI] [PubMed] [Google Scholar]
- Warnick EM, Bracken MB, Kasl S. Screening Efficiency of the Child Behavior Checklist and Strengths and Difficulties Questionnaire: A Systematic Review. Child and Adolescent Mental Health. 2008;13(3):140–147. doi: 10.1111/j.1475-3588.2007.00461.x. [DOI] [PubMed] [Google Scholar]
- Winghem JV, Telfer B, Reid T, Ouko J, Mutunga A, Jama Z, Vakil S. Implementation of a comprehensive program including psycho-social and treatment literacy activities to improve adherence to HIV care and treatment for a pediatric population in Kenya. BMC Pediatrics. 2008;8(1):52. doi: 10.1186/1471-2431-8-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woodcock A, Cronin Ó, Forde S. Quantitative evidence for the benefits of Moving the Goalposts, a Sport for Development project in rural Kenya. Evaluation and Program Planning. 2012;35(3):370–381. doi: 10.1016/j.evalprogplan.2012.01.001. [DOI] [PubMed] [Google Scholar]


