Abstract
Childhood maltreatment is associated with elevated risk for depression across the human lifespan. Identifying the pathways through which childhood maltreatment relates to depressive symptoms may elucidate intervention targets that have the potential to reduce the lifelong negative health sequelae of maltreatment exposure. In this cross-sectional study, 271 women with early-stage breast cancer were assessed after their diagnosis but before the start of adjuvant treatment (chemotherapy, radiation, endocrine therapy). Participants completed measures of childhood maltreatment exposure, psychological resources (optimism, mastery, self-esteem, mindfulness), and depressive symptoms. Using multiple mediation analyses, we examined which psychological resources uniquely mediated the relationship between childhood maltreatment and depressive symptoms. Exposure to maltreatment during childhood was robustly associated with lower psychological resources and elevated depressive symptoms. Further, lower optimism and mindfulness mediated the association between childhood maltreatment and elevated depressive symptoms. These results support existing theory that childhood maltreatment is associated with lower psychological resources, which partially explains elevated depressive symptoms in a sample of women facing breast cancer diagnosis and treatment. These findings warrant replication in populations facing other major life events and highlight the need for additional studies examining childhood maltreatment as a moderator of treatment outcomes.
Keywords: Childhood maltreatment, psychological resources, depressive symptoms, breast cancer, optimism, mindfulness, risk factor
Childhood maltreatment is behavior toward a person under the age of 18 years that results in actual or potential harm to the child’s health, survival, development or dignity and is perpetrated by a person of responsibility, trust, or power in that child’s life (“WHO | Child maltreatment,” 2016). Childhood maltreatment includes abuse and/or neglect during childhood that can be physical, sexual, or emotional in nature (Bernstein & Fink, 1998). Childhood maltreatment exposure is associated with persistent symptoms of depression throughout the lifespan (Chapman et al., 2004; Kessler et al., 2010; Nanni, Uher, & Danese, 2012), and is among the most robust associations in clinical psychology and psychiatry. For example, a meta-analysis of 16 studies reflecting data from more than 23,000 participants demonstrated that maltreatment exposure increased the risk of developing depression in adulthood, and was associated with persistent or recurrent illness, and lack of response to treatment (Nanni et al., 2012). In fact, it is estimated that childhood adversity accounts for 30% of all psychiatric morbidity (Kessler et al., 2010). Childhood maltreatment may increase risk for depression by interfering with the development of a robust and functional store of psychological resources during childhood (Repetti et al., 2002; Taylor et al., 2004; Taylor & Stanton, 2007), which help individuals effectively cope with adult life stress. Indeed, the vast majority of depressive episodes occur in the wake of a major life stressor (Hammen, Henry, & Daley, 2000; Hammen, 2005). Thus, lower psychological resources may have the largest implications during this vulnerable time. The purpose of this study was to examine psychological resources as a mechanism through which childhood maltreatment is associated with depressive symptoms in women recently diagnosed with breast cancer.
Psychological resources are skills, beliefs, and individual personality factors that influence how people manage stressful events (Donaldson, Csikszentmihalyi, & Nakamura, 2011; Taylor & Stanton, 2007). Healthy environments are safe environments that allow children to emotionally and socially develop in ways that will help them pay attention to, learn what to expect from, and respond to their environment. Living in a family characterized by low nurturance, abuse, or a high degree of unpredictability has long been theorized to predict lower psychological resources (Repetti et al., 2002). In particular, unsafe environments can foster negative expectations about future events, bias attention toward negative or threatening aspects of the environment, and impede the development of a wide range of socioemotional abilities. For example, adults exposed to childhood maltreatment have lower reports of dispositional optimism (Broekhof et al., 2015; Korkeila et al., 2004; Murthi & Espelage, 2005), and demonstrate biased attention to potentially threatening aspects of the environment (McLaughlin, Sheridan, & Lambert, 2014; Pollak & Sinha, 2002). Yet, empirical tests of the link between childhood maltreatment and specific psychological resources remain rare. In this study, we examined the associations between childhood maltreatment and optimism, mastery, self-esteem, and mindfulness in a sample of women following their recent diagnosis with breast cancer.
Optimism, mastery, self-esteem, and mindfulness have all emerged as important psychological resources that promote health and well-being (Brown, Ryan, & Creswell, 2007; Taylor & Seeman, 1999), including in the wake of stressful life events such cancer diagnosis and treatment (Taylor, 1983; Taylor & Armor, 1996; Taylor & Stanton, 2007). Optimism is the extent to which an individual holds a generalized, favorable expectancy for the future (Carver, Scheier, & Segerstrom, 2010). Mastery reflects the extent to which an individual feels they have control over events in their lives (Pearlin & Schooler, 1978). Self-esteem is an individual’s global positive or negative attitude toward the self as a totality (Rosenberg, 1965; Rosenberg, Schooler, Schoenbach, & Rosenberg, 1995). Mindfulness is an individual’s degree of awareness of and attention to external and internal stimuli (Brown, Ryan, & Creswell, 2007). Each of these resources likely play a role in an individual’s adaptation to a breast cancer diagnosis and motivation to actively participate in treatment and recovery.
Optimism, self-esteem, mastery, and mindfulness are all psychological resources that have been linked to better health and specifically fewer depressive symptoms. Higher reported optimism has been repeatedly linked to positive health outcomes (Carver et al., 2010; Scheier & Carver, 1987), including lower depressive symptoms in medical populations (Milaniak et al., 2016). Mastery is protective against negative health outcomes in older adults (Pudrovska, Schieman, Pearlin, & Nguyen, 2005), including depressive symptoms (King, Wardecker, & Edelstein, 2015). Low self-esteem has often been prospectively linked to depression and other health outcomes (Abela & Payne, 2003; Abela & Skitch, 2007; McCaulay, Mintz, & Glenn, 1988). Finally, interventions targeting mindfulness can be effective in reducing symptoms of depression and anxiety (Hofmann, Sawyer, Witt, & Oh, 2010).
Past studies have also posited psychological resources as mediators in the relationship between childhood adversity and depression (Schetter & Dolbier, 2011; Scott Heller, Larrieu, D’Imperio, & Boris, 1999), yet only a few studies have provided empirical support for this hypothesis. For example, adults exposed to childhood maltreatment have lower reports of dispositional optimism (Broekhof et al., 2015), and higher reported optimism in adults exposed to childhood maltreatment is a predictor of psychological adjustment (Himelein & McElrath, 1996; Scott Heller et al., 1999). Further, high reported mastery attenuates the association between childhood sexual abuse and depressive symptoms (King et al., 2015). In a large sample of homeless women, self-esteem mediated the association between childhood abuse and depressive symptoms (Stein, Leslie, & Nyamathi, 2002). Further, mindfulness-based interventions are effective in reducing symptoms of depression and anxiety (Hofmann et al., 2010), including among adult survivors of childhood abuse (Kimbrough, Magyari, Langenberg, Chesney, & Berman, 2010). These studies offer initial evidence that optimism, mastery, self-esteem, and mindfulness may all explain variability in depressive symptoms among individuals exposed to maltreatment in childhood. Yet, empirical support for their role remains rare and no study to date has examined these potential mediators simultaneously which would isolate important intervention targets during a period of high risk for depressive symptoms.
Optimism, mastery, self-esteem, and mindfulness may play an important role in resilience to symptoms of depression in the context of cancer. One in eight women will be diagnosed with breast cancer (American Cancer Society, 2016). Depressive symptoms remain elevated during the year after breast cancer diagnosis and can interfere with effective treatment, reduce quality of life, and impair recovery after treatment completion (Antoni et al., 2006; Giese-Davis et al., 2011; Stanton et al., 2005, 2015; Stanton & Bower, 2015). Further, childhood adversity has been linked to important outcomes in women with breast cancer, including depression (McFarland et al., 2016; Witek Janusek, Tell, Albuquerque, & Mathews, 2013), but also fatigue (Bower, Crosswell, & Slavich, 2014), inflammation (Crosswell, Bower, & Ganz, 2014), and cancer-related distress (Fagundes, Lindgren, Shapiro, & Kiecolt-Glaser, 2012; Goldsmith et al., 2010).
Examining the role of psychological resources in the relationship between childhood maltreatment and depressive symptoms in women recently diagnosed with breast cancer may be an important step toward identifying psychosocial intervention targets. Yet, no previous studies have identified specific psychological resources that may confer risk for depression in women with a history of child maltreatment. Further, few studies have examined the role of psychological resources in risk for depression in a high risk sample, such as women recently diagnosed with breast cancer. In this study we examined whether psychological resources (optimism, mastery, self-esteem, and mindfulness) mediate the association between childhood maltreatment and depressive symptoms in a sample of women recently diagnosed with breast cancer. We hypothesized that childhood maltreatment would be associated with elevated symptoms of depression, and that psychological resources would account for variability in this association.
Methods
Participants
Participants were 271 women with breast cancer enrolled in a parent study examining predictors of cancer-related fatigue. Women were eligible for participation in the study if they met the following criteria: 1) diagnosed with early-stage, resectable breast cancer (Stage 0, I, II, IIIA); 2) had not started adjuvant or neoadjuvant therapy with chemotherapy, radiation, trastuzumab, and/or endocrine therapy; 3) able to speak, read, and understand English. The University of California Los Angeles Institutional Review Board approved the study procedures, and written informed consent was obtained from all participants.
Procedures
Participants were recruited from oncology clinics in the Los Angeles metropolitan area. Upon informed consent and study enrollment, participants received a link via email to demographic, medical, and psychosocial questionnaires on www.Qualtrics.com. Participants could also complete paper copies of the questionnaires if they preferred this method of administration. Women completed the psychosocial questionnaires after surgical resection of their breast tumor, but before adjuvant therapy (chemotherapy, radiation, endocrine therapy, trastuzumab), if prescribed. For those who received neoadjuvant chemotherapy prior to surgery, the questionnaires were completed prior to onset of neoadjuvant chemotherapy.
Measures
Childhood maltreatment
The Childhood Trauma Questionnaire-Short Form (CTQ) (Bernstein et al., 2003) is a 28-item, self-report question naire which assesses exposure to abuse and neglect during childhood. Each item begins with “When I was growing up…” and proceeds to identify experiences in the childhood rearing environment. Examples of items include: “I was punished with a belt/board/cord/other hard object,” “People in my family said hurtful or insulting things to me,” and “My parents were too drunk or high to take care of the family.” For each item, participants indicated the frequency of each of these experiences according to a six-point Likert-type scale where response options ranged from 0 (“never true”) to 5 (“very often true”), and higher scores on the CTQ indicate more severe and frequent maltreatment experiences. We created two mutually exclusive groups using the cut points established in the Walker scoring procedure (Walker et al., 1999): no maltreatment exposure and maltreatment exposed. Participants with scores for emotional abuse ≥ 10, emotional neglect ≥ 15, physical abuse ≥ 8, physical neglect ≥ 8, or sexual abuse ≥ 8 were included in the maltreated group. Sensitivity and specificity of these thresholds when compared to clinical interviews were ≥ .85 for all 5 subscales (Bernstein & Fink, 1998). Internal reliability for each CTQ subscale was as follows: emotional neglect α = .92, emotional abuse α = .86, sexual abuse α = .94, physical abuse α = .83, physical neglect α = .65.
Optimism
The Life Orientation Test (LOT-R) (Scheier & Carver, 1985) assesses generalized positive outcome expectancies using 6 self-report items. For each item, participants indicated their level of agreement with a given statement according to a five-point Likert-type scale where response options ranged from “I agree a lot” to “I disagree a lot”. Example items include, “In uncertain times, I usually expect the best” and “I’m always optimistic about my future.” Higher scores indicate greater dispositional optimism. Substantial research supports the reliability and validity of the LOT-R instrument (Scheier, Carver, & Bridges, 1994), and the internal consistency of the LOT-R in this sample was high, α = .85.
Mastery
The personal mastery scale is a 7-item scale that measures the extent to which an individual feels control over life outcomes (Pearlin & Schooler, 1978). For each item, participants indicated their level of agreement with a given statement according to a four-point Likert-type scale where response options ranged from “Strongly Agree” to “Strongly Disagree.” Example items include, “I have little control over the things that happen to me” and “I often feel helpless in dealing with the problems of life.” Higher scores indicate higher mastery. This scale is widely used in health research with cancer patients (e.g., Buffart et al., 2014; Robb, Lee, Jacobsen, Dobbin, & Extermann, 2013) and demonstrated high internal reliability within this sample, α = .88.
Self-esteem
Participants completed the original 10-item Rosenberg Self-esteem Scale (RSES) (Rosenberg, 1965). The RSES was developed to reflect an individual’s global self-esteem (Rosenberg et al., 1995). For each item, participants indicated their level of agreement with a given statement according to a four-point Likert-type scale where response options ranged from “Strongly Agree” to “Strongly Disagree.” Example items include, “I feel I do not have much to be proud of” and “I wish I could have more respect for myself.” Higher scores on the RSES indicate higher global self-esteem. This scale is widely used in research on women with breast cancer (e.g., Awick, Phillips, Lloyd, & McAuley, 2016; Schroevers, Ranchor, & Sanderman, 2006), and demonstrated high internal reliability within this sample, α = .89.
Mindfulness
Dispositional mindfulness was measured using the Mindful Attention and Awareness Scale (MAAS) (Brown & Ryan, 2003). This 15-item scale measures the frequency of mindful states in day-to-day life, using both general and situation-specific statements. For each item, participants indicated how frequently they experience the events described in each of the provided statements according to a six-point Likert-type scale where response options ranged from “Almost Always” to “Almost Never.” Example items include, “I could be experiencing some emotion and not be conscious of it until some time later” and “I break or spill things because of carelessness, not paying attention, or thinking of something else.” Higher scores indicate greater mindfulness. This scale has been validated for use in cancer patients and survivors (Carlson & Brown, 2005). The MAAS demonstrated high internal reliability within this sample, α = .91.
Depressive symptoms and history
Depressive symptoms in the past week were assessed via the Center for Epidemiologic Studies Depression Scale (CES-D; Radloff, 1977). The CES-D is a 20-question, self-report instrument with excellent reliability and validity (Radloff, 1977). Example items on the CES-D include, “I was bothered by things that usually don’t bother me” and “I felt that I could not shake off the blues even with help from my family or friends.” Participants indicated how often they have felt this way with 4 response options ranging from “Rarely or none of the time” to “Most or all of the time.” Scores on the CES-D can range from 0–60, and a score of 16 or higher suggests clinically significant symptoms of depression. This measure also demonstrated good internal reliability in the current sample, α = .87. The CES-D was identified as useful in measuring psychosocial functioning in cancer patients (Pinquart & Duberstein, 2010), and has demonstrated good sensitivity and specificity with major depressive episodes determined via semi-structured clinical interview (Lyness et al., 1997; Mulrow et al., 1995). History of Major Depressive Disorder (MDD) was assessed by trained research staff using the Structured Clinical Interview for DSM (First & Gibbon, 2004) and diagnostic decisions were supervised by a licensed clinician.
Demographics and clinical characteristics
Age, ethnicity, income, education, marital status, disease stage, and surgery type were provided via self-report questionnaires.
Data Analysis
All continuous variables were examined for skew and kurtosis and found to be normally distributed. Specifically, the range of skewness for all continuous variables was −1.16 to 1.35 and the range of kurtosis was 0.06 to 1.76. Demographic and clinical characteristics that have previously been associated with childhood maltreatment or depression were included in multivariate models as covariates. These included age, ethnicity, history of MDD, income, education, marital status, disease stage, and surgery type (see for example Stanton et al., 2015; Wingo et al., 2010).
To test hypothesized associations and mediating processes between childhood maltreatment, psychological resources, and depressive symptoms, we fit a multiple mediator model with resampling strategies for assessing and comparing indirect effects (Hayes, 2013; Preacher & Hayes, 2008). To do this, we employed the PROCESS macro for SPSS developed by Preacher & Hayes (2008). All analyses generated 95% bias-corrected and accelerated bootstrap confidence intervals for the indirect effects using 10,000 bootstrap samples. This analytic strategy can be used for comparing the relative magnitude of multiple, simultaneous indirect effects. In this model, the IV (childhood maltreatment) affects the DV (depressive symptoms) through multiple mediators (optimism, mastery, self-esteem, mindfulness) which are entered simultaneously. Within the multiple mediator model, the indirect effect for each mediator is its unique effect on the outcome, controlling for the effects of the other mediator (Preacher & Hayes, 2008). This approach uses ordinary least squares regression to establish the associations between the independent variable (IV; childhood maltreatment), the dependent variable (DV; depressive symptoms), and the mediator (psychological resources). These associations can be characterized by five regression coefficients: a) the total effect (c path) of the IV on the DV, independent of the effect of the mediator; b) the direct effect (c′ path) of the IV on the DV, including the effect of the mediator; c) the effect of the IV on the mediator (a path); d) the effect of the mediator on the DV while accounting for the IV (b path); and e), the mediated, or indirect effect, the cross-product of a and b (ab path). If the bootstrap confidence intervals for ab do not contain zero, the mediated effect is considered significant (Hayes, 2013). Such an analysis is ideal for juxtaposing several pathways by which the IV can affect the DV, and provides a more rigorous test compared to conducting separate analyses for each mediator.
Results
Participants in this study were approximately 56 years old, predominantly non-Hispanic white, college-educated, and had a household income over $100,000. The majority of women had received breast-conserving surgery (i.e., lumpectomy) and 21.8% had a history of MDD. Table 1 includes detailed demographic, social, and clinical information on this sample including maltreatment history, psychological resources, depressive symptoms, and history of depression. We found that 39.5% of our sample were maltreatment exposed. Women exposed to any childhood maltreatment reported lower educational attainment, χ2 = 10.77, p = .005, were less likely to be married, χ2 = 9.88, p = .002, reported lower annual income, χ2 = 8.76, p = .013, and were more likely to have a history of MDD, χ2 = 12.42, p < .001. There were no statistically significant differences between women with and without a history of childhood maltreatment in ethnicity, χ2 = 0.54, p = .46, disease stage, χ2 = 6.29, p = .098, or surgery type, χ2 = 0.01, p = .943. Not surprisingly, psychological resources were significantly correlated with one another. See Table 2 for means and standard deviations for continuous variables, and bivariate correlations between them.
Table 1.
Demographic, clinical, and psychosocial characteristics of the study sample.
| M (SD) | % | |
|---|---|---|
| Age | 56.23 (11.49) | |
| Married | 64.6 | |
| Ethnicity/Race | ||
| Non-Hispanic white | 71.6 | |
| Asian | 11.1 | |
| Black | 4.4 | |
| Hispanic/Latina | 3.7 | |
| Other | 9.2 | |
| Income | ||
| < $60,000 | 25.1 | |
| $60,000 – $100,000 | 19.9 | |
| > $100,000 | 55.1 | |
| Education | ||
| High school | 28.8 | |
| College degree | 39.9 | |
| Post-graduate degree | 31.4 | |
| Surgery Type | ||
| Lumpectomy | 60.1 | |
| Mastectomy | 39.9 | |
| Childhood Maltreatment (CTQ) | ||
| CTQ Total Score | 36.04 (13.26) | |
| No Maltreatment | 60.5 | |
| Maltreatment | 39.5 | |
| Psychological resources | ||
| Optimism | 19.01 (4.90) | |
| Mastery | 22.21 (4.45) | |
| Self-Esteem | 34.33 (4.99) | |
| Mindfulness | 4.47 (0.83) | |
| Depression | ||
| Depressive symptoms (CESD) | 12.69 (10.35) | |
| Current MDD | 5.9 | |
| History of MDD | 21.8 | |
Table 2.
Descriptive statistics and bivariate correlations between all continuous variables.
| M (SD) | 1. | 2. | 3. | 4. | 5. | 6. | 7. | |
|---|---|---|---|---|---|---|---|---|
| 1. Age | 56.23 (11.5) | 1.0 | ||||||
| 2. CTQ Total | 36.04 (13.26) | −.02 | 1.0 | |||||
| 3. Optimism | 19.01 (4.9) | .12* | −.24** | 1.0 | ||||
| 4. Mastery | 22.21 (4.5) | −.17** | −.20** | .43** | 1.0 | |||
| 5. Self-Esteem | 34.33 (5.0) | .10+ | −.28** | .58** | .58** | 1.0 | ||
| 6. Mindfulness | 4.47 (0.8) | .19** | −.34** | .28** | .23** | .40** | 1.0 | |
| 8. Depressive symptoms | 12.69 (10.35) | −.19** | .31** | −.44** | −.31** | −.47** | −.43** | 1.0 |
p< .01
p<.05
p < .10
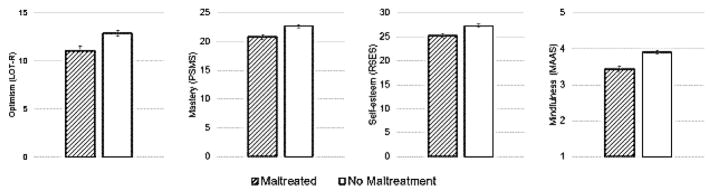
The total effect of childhood maltreatment on depressive symptoms was significant, such that childhood maltreatment was associated with more depressive symptoms, c path B = 5.04, SE = 1.26, 95%CI [2.76, 7.70], p < .001. Childhood maltreatment was associated with lower optimism, B = −1.80, SE = .64, 95%CI [−3.06, −0.54], lower mastery, B = −1.88, SE = .60, 95%CI [−3.05, −0.70], lower self-esteem, B = −2.07, SE = .65, 95%CI [−3.35, −0.79], and lower mindfulness, B = −0.47, SE = .11, 95%CI [−0.69, −0.25]. See Figure 1 for a comparison of estimated psychological resources for women with and without childhood maltreatment exposure.
Figure 1.
Adjusted mean differences in psychological resources in women with breast cancer by childhood maltreatment exposure.
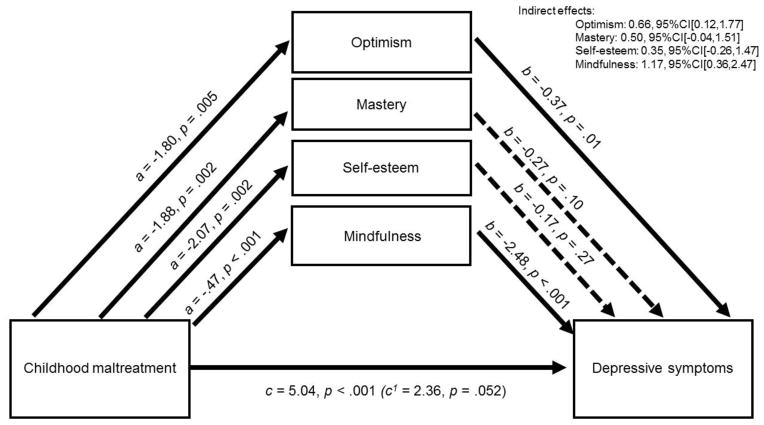
Lower optimism, B = −0.37, SE = .14, 95%CI [−0.64, −0.09], and lower mindfulness were associated with more depressive symptoms, B = −2.48, SE = .73, 95%CI [−3.91, −1.05]. There was a significant indirect effect of childhood maltreatment on depressive symptoms through optimism, ab) B = 0.66, SE = .39, 95%CI [0.12, 1.77], and mindfulness, ab) B = 1.17, SE = .52, 95%CI [0.36, 2.47]. Results of the multiple mediation analysis suggest that when accounting for these significant indirect effects the association between childhood maltreatment and depressive symptoms, or the direct path, was no longer significant, c′ path B = 2.36, SE = 1.20, 95%CI [−0.02, 4.73], p = .052. See Figure 2 for estimates of total, direct, and indirect paths from childhood maltreatment to depressive symptoms using multiple mediation.
Figure 2.
Optimism and mindfulness mediate the association between childhood maltreatment and depressive symptoms in women with breast cancer.
Note: All analyses account for age, surgery type, ethnic minority status, education, income, marital status, and history of MDD.
Discussion
Childhood maltreatment exposure in this sample was 39.5%, comparable with other published studies in non-cancer populations (Bradley et al., 2008; Dong et al., 2004; Scher, Forde, McQuaid, & Stein, 2004), and was associated with elevated depressive symptoms, consistent with previous research (Chapman et al., 2004; Walker et al., 1999). We examined optimism, mastery, self-esteem, and mindfulness as potential psychological resources that mediate the association between childhood maltreatment and depressive symptoms. Although childhood maltreatment was associated with lower psychological resources overall, results of multiple mediation analyses indicated that optimism and mindfulness specifically mediated the association between childhood maltreatment and depressive symptoms in the immediate aftermath of breast cancer diagnosis, whereas mastery and self-esteem did not. These findings provide empirical support for the hypothesis that childhood maltreatment may impede development of psychological resources, which explain variability in depressive symptoms among women facing diagnosis and treatment for breast cancer.
Our results provide insight into the specific psychological pathways through which adversity may lead to depression during a stressful life experience. Studies have repeatedly shown that childhood maltreatment is associated with elevated risk for depression across the lifespan (Kessler et al., 2010; Nanni et al., 2012). This may be because harsh family environments that are characterized by conflict and aggression are associated with disrupted psychosocial functioning (Repetti et al., 2002). Optimism involves holding positive expectations for the future. Yet, children living in abusive environments can develop learned helplessness, or maladaptive passivity in the context of stress. Children in these environments may learn over time that actively coping with or responding to the environment is futile, thus undermining the development of optimism in the face of future adversity or uncontrollable events (Peterson & Seligman, 1983). Learned helplessness can be adaptive in the moment for maltreated youth, but if used habitually can be deleterious (Briere & Jordan, 2009), and predispose the individual to depression.
Childhood environments may also interfere with the development of mindfulness as a psychological resource, though research examining the psychosocial predictors of mindfulness in pediatric populations is still limited (Greenberg & Harris, 2012). Adult women exposed to childhood maltreatment are more likely to cope with stress by trying to control their immediate emotional states (Hager & Runtz, 2012; Repetti et al., 2002). This can often take the form of distraction and emotional distancing that are adaptive in the moment (Briere & Jordan, 2009), but may simultaneously prevent the cultivation of mindfulness to the present moment and external surroundings as a skill for coping with stress. Indeed, mindfulness-training in children appears to strengthen top-down self-regulation which in turn dampens the physiological processes associated with anxiety and stress (Zelazo & Lyons, 2012). Thus, depleted optimism and mindfulness may explain why women exposed to maltreatment experience elevated symptoms of depression in the wake of major life events, such as breast cancer diagnosis. More longitudinal studies are needed, however, to understand how mindfulness and optimism develop in different types of social environments during childhood.
Indeed, mindfulness and optimism may be particularly important psychological resources in the context of cancer diagnosis and treatment. Several intervention studies targeting mindfulness have been effective in mitigating depressive symptoms in women with breast cancer (Bower et al., 2015; Hilton et al., 2017; Zainal, Booth, & Huppert, 2013), and may also improve other important outcomes, such as pain (Hilton et al., 2017). Mindfulness may be beneficial to women with breast cancer specifically because mindfulness often involves awareness and acceptance of internal sensations that may help patients with the physical symptoms that accompany their treatments. This may have important implications for survivorship because mindfulness interventions improve depressive symptoms for up to 2.5 years (Earley et al., 2014; Kimbrough et al., 2010), and even prevent relapse (Williams et al., 2014) in women with a childhood maltreatment history. There is also evidence that cognitive-behavioral stress management decreases depression in women with breast cancer by increasing generalized optimism (Antoni et al., 2001). Optimism may also have additional benefits in breast cancer populations because optimism has been linked to health behaviors, such as exercise, that promote better adjustment to cancer (Harper et al., 2007). Taken together, interventions that increase optimism and mindfulness may be effective for mitigating depressive symptoms in women with breast cancer, and may disproportionately benefit those patients with a history of childhood maltreatment. However, it is important to note that no study to our knowledge has explicitly tested childhood maltreatment history as a moderator of treatment effectiveness in a breast cancer sample. This is an important next step in understanding how to implement personalized behavioral medicine given that trauma history has been observed as a moderator of treatment effectiveness in non-cancer trials (Nanni et al., 2012).
These results should be interpreted in the context of several strengths and limitations. First, these data are cross-sectional and therefore no causal conclusions can be drawn. However, there is practical and theoretical support for structuring our model as we did. Specifically, childhood maltreatment, although retrospectively reported, temporally precedes stabilization of any psychological resources measured, and depressive symptoms via the CES-D are designed to be transitory based upon progression and remittance of depressive illness. Further, all of the psychological resources measured in this study are dispositional in nature (Brown & Ryan, 2003; Taylor & Stanton, 2007), thus justifying their position as a mediator, rather than the DV. We acknowledge that psychological resources likely fluctuate as a function of depressive status, and longitudinal investigations examining the transactional dynamics between psychological resources and depressive episodes would be informative in this regard. We also used a dichotomous variable to reflect childhood maltreatment status. Exposure to different types of adversity tend to co-occur in maltreated samples (Edwards, Holden, Felitti, & Anda, 2003). Thus, we took a conservative approach by using a categorical variable for maltreatment exposure that has been previously associated with health and health care costs (Walker et al., 1999), and may be more easily used in clinical practice. It should be noted that the pattern of mediation results do not change when using a continuous total score for childhood maltreatment. Also, within our sample, all of the CTQ subscales were significantly correlated with one another, with the strongest association between emotional abuse and emotional neglect, r = .74, p < .001, and the weakest between physical abuse and sexual abuse, r = .25, p < .001. All of the CTQ subscales were significantly correlated with depressive symptoms, ranging from physical abuse, r = .17, p = .006, to emotional neglect, r = .28, p = .001. Finally, this study reflects data from a predominantly Caucasian, well-educated, and fairly high income sample of women with breast cancer. Efforts to understand how these results generalize to samples varying in social and demographic characteristics as well as in those facing other major life stressors are warranted.
Depressive symptoms have been repeatedly linked to poorer cancer recovery and risk for recurrence (Pinquart & Duberstein, 2010; Satin, Linden, & Phillips, 2009). One strength of the present study design is the assessment of depressive symptoms and underlying psychological resources in the immediate aftermath of breast cancer diagnosis. Between 22–38% of major depressive episodes can be prevented with existing evidence-based therapies (Muñoz, Beardslee, & Leykin, 2012) and interventions that mitigate depressive symptoms in breast cancer patients may significantly improve patient trajectories and treatment outcomes (Antoni et al., 2001; Giese-Davis et al., 2011; Pinquart & Duberstein, 2010). This study extends our understanding by suggesting that women who have a history of maltreatment may disproportionately benefit from interventions targeting optimism and mindfulness. This is important because, in non-cancer populations, intervention studies targeting some psychological resources have proven to be ineffective, such as those targeting self-esteem (Baumeister, Campbell, Krueger, & Vohs, 2003), and individuals with a trauma history may benefit from different types of treatment than those without (Lewis et al., 2010; Nanni et al., 2012; Weisz, McCarty, & Valeri, 2006). Childhood maltreatment may predispose individuals to cancer (Holman et al., 2016), and is associated with earlier all-cause mortality (Chen, Turiano, Mroczek, & Miller, 2016). Identifying key psychological pathways from childhood maltreatment to psychopathology that are responsive to interventions is essential to mitigating the lifelong health disparities associated with childhood maltreatment exposure.
Acknowledgments
This work was supported by the National Cancer Institute (R01 CA160427) awarded to Julienne E. Bower. Preparation of this manuscript was made possible by the National Institute of Mental Health (T32MH015750 and K08MH112773) awarded to Dr. Kate Ryan Kuhlman. We would also like to thank our participants for their willingness to participate in this study during such a challenging time in their lives.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Abela JRZ, Payne AV. A test of the integration of the hopelessness and self-esteem theories of depression in schoolchildren. Cognitive Therapy and Research. 2003;27(5):519–535. https://doi.org/10.1023/A:1026303020478. [Google Scholar]
- Abela JRZ, Skitch SA. Dysfunctional attitudes, self-esteem, and hassles: Cognitive vulnerability to depression in children of affectively ill parents. Behaviour Research and Therapy. 2007;45(6):1127–1140. doi: 10.1016/j.brat.2006.09.011. https://doi.org/10.1016/j.brat.2006.09.011. [DOI] [PubMed] [Google Scholar]
- Antoni MH, Lechner SC, Kazi A, Wimberly SR, Sifre T, Urcuyo KR, … Carver CS. How stress management improves quality of life after treatment for breast cancer. Journal of Consulting and Clinical Psychology. 2006;74(6):1143. doi: 10.1037/0022-006X.74.6.1152. https://doi.org/10.1037/0022-006X.74.6.1143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Antoni MH, Lehman JM, Kilbourn KM, Boyers AE, Culver JL, … Alferi SM. Cognitive-behavioral stress management intervention decreases the prevalence of depression and enhances benefit finding among women under treatment for early-stage breast cancer. Health Psychology. 2001;20(1):20. doi: 10.1037//0278-6133.20.1.20. https://doi.org/10.1037//0278-6133.20.1.20. [DOI] [PubMed] [Google Scholar]
- Awick EA, Phillips SM, Lloyd GR, McAuley E. Physical activity, self-efficacy and self-esteem in breast cancer survivors: A panel model. Psycho-Oncology. 2016 doi: 10.1002/pon.4180. https://doi.org/10.1002/pon.4156. [DOI] [PMC free article] [PubMed]
- Baumeister RF, Campbell JD, Krueger JI, Vohs KD. Does high self-esteem cause better performance, interpersonal success, happiness, or healthier lifestyles? Psychological Science in the Public Interest: A Journal of the American Psychological Society. 2003;4(1):1–44. doi: 10.1111/1529-1006.01431. https://doi.org/10.1111/1529-1006.01431. [DOI] [PubMed] [Google Scholar]
- Bernstein DP, Fink LA. CTQ: Childhood Trauma Questionnaire: A retrospective self-report. San Antonio, TX: Psychological Corp; 1998. [Google Scholar]
- Bernstein DP, Stein JA, Newcomb MD, Walker E, Pogge D, Ahluvalia T, … Zule W. Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abuse & Neglect. 2003;27(2):169–190. doi: 10.1016/s0145-2134(02)00541-0. https://doi.org/10.1016/S0145-2134(02)00541-0. [DOI] [PubMed] [Google Scholar]
- Bower JE, Crosswell AD, Slavich GM. Childhood adversity and cumulative life stress risk factors for cancer-related fatigue. Clinical Psychological Science. 2014;2(1):108–115. doi: 10.1177/2167702613496243. https://doi.org/10.1177/2167702613496243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bower JE, Crosswell AD, Stanton AL, Crespi CM, Winston D, Arevalo J, … Ganz PA. Mindfulness meditation for younger breast cancer survivors: A randomized controlled trial. Cancer. 2015;121(8):1231. doi: 10.1002/cncr.29194. https://doi.org/10.1002/cncr.29194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bradley RG, Binder EB, Epstein MP, Tang Y, Nair HP, Liu W, … Ressler KJ. Influence of child abuse on adult depression: Moderation by the corticotropin-releasing hormone receptor gene. Archives of General Psychiatry. 2008;65(2):190. doi: 10.1001/archgenpsychiatry.2007.26. https://doi.org/10.1001/archgenpsychiatry.2007.26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breast cancer facts and figures, 2015–2016. American Cancer Society; 2016. [Google Scholar]
- Briere J, Jordan CE. Childhood maltreatment, intervening variables, and adult psychological difficulties in women: An overview. Trauma, Violence, & Abuse. 2009;10(4):375–388. doi: 10.1177/1524838009339757. https://doi.org/10.1177/1524838009339757. [DOI] [PubMed] [Google Scholar]
- Broekhof R, Rius-Ottenheim N, Spinhoven P, van der Mast RC, Penninx BWJH, Zitman FG, Giltay EJ. Long-lasting effects of affective disorders and childhood trauma on dispositional optimism. Journal of Affective Disorders. 2015;175:351–358. doi: 10.1016/j.jad.2015.01.022. https://doi.org/10.1016/j.jad.2015.01.022. [DOI] [PubMed] [Google Scholar]
- Brown KW, Ryan RM. The benefits of being present: Mindfulness and its role in psychological well-being. Journal of Personality and Social Psychology. 2003;84(4):822. doi: 10.1037/0022-3514.84.4.822. https://doi.org/10.1037/0022-3514.84.4.822. [DOI] [PubMed] [Google Scholar]
- Brown KW, Ryan RM, Creswell JD. Mindfulness: Theoretical foundations and evidence for its salutary effects. Psychological Inquiry. 2007;18(4):211–237. https://doi.org/10.1080/10478400701598298. [Google Scholar]
- Buffart LM, Ros WJG, Chinapaw MJM, Brug J, Knol DL, Korstjens I, … May AM. Mediators of physical exercise for improvement in cancer survivors’ quality of life. Psycho-Oncology. 2014;23(3):330–338. doi: 10.1002/pon.3428. https://doi.org/10.1002/pon.3428. [DOI] [PubMed] [Google Scholar]
- Carlson LE, Brown KW. Validation of the Mindful Attention Awareness Scale in a cancer population. Journal of Psychosomatic Research. 2005;58(1):29. doi: 10.1016/j.jpsychores.2004.04.366. https://doi.org/10.1016/j.jpsychores.2004.04.366. [DOI] [PubMed] [Google Scholar]
- Carver CS, Scheier MF, Segerstrom SC. Optimism. Clinical Psychology Review. 2010;30(7):879–889. doi: 10.1016/j.cpr.2010.01.006. https://doi.org/10.1016/j.cpr.2010.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chapman DP, Whitfield CL, Felitti VJ, Dube SR, Edwards VJ, Anda RF. Adverse childhood experiences and the risk of depressive disorders in adulthood. Journal of Affective Disorders. 2004;82(2):217–225. doi: 10.1016/j.jad.2003.12.013. https://doi.org/10.1016/j.jad.2003.12.013. [DOI] [PubMed] [Google Scholar]
- Chen E, Turiano NA, Mroczek DK, Miller GE. Association of reports of childhood abuse and all-cause mortality rates in women. JAMA Psychiatry. 2016;73(9):920–927. doi: 10.1001/jamapsychiatry.2016.1786. https://doi.org/10.1001/jamapsychiatry.2016.1786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crosswell AD, Bower JE, Ganz PA. Childhood adversity and inflammation in breast cancer survivors. Psychosomatic Medicine. 2014;76(3):208–214. doi: 10.1097/PSY.0000000000000041. https://doi.org/10.1097/PSY.0000000000000041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donaldson SI, Csikszentmihalyi M, Nakamura J. Applied Positive Psychology: Improving Everyday Life, Health, Schools, Work, and Society. Routledge; 2011. [Google Scholar]
- Dong M, Anda RF, Felitti VJ, Dube SR, Williamson DF, Thompson TJ, … Giles WH. The interrelatedness of multiple forms of childhood abuse, neglect, and household dysfunction. Child Abuse & Neglect. 2004;28(7):771. doi: 10.1016/j.chiabu.2004.01.008. https://doi.org/10.1016/j.chiabu.2004.01.008. [DOI] [PubMed] [Google Scholar]
- Earley MD, Chesney MA, Frye J, Greene PA, Berman B, Kimbrough E. Mindfulness intervention or child abuse survivors: A 2.5-year follow-up. Journal of Clinical Psychology. 2014;70(10):933–941. doi: 10.1002/jclp.22102. https://doi.org/10.1002/jclp.22102. [DOI] [PubMed] [Google Scholar]
- Edwards VJ, Holden GW, Felitti VJ, Anda RF. Relationship between multiple forms of childhood maltreatment and adult mental health in community respondents: Results from the Adverse Childhood Experiences Study. American Journal of Psychiatry. 2003;160(8):1453–1460. doi: 10.1176/appi.ajp.160.8.1453. https://doi.org/10.1176/appi.ajp.160.8.1453. [DOI] [PubMed] [Google Scholar]
- Fagundes CP, Lindgren ME, Shapiro CL, Kiecolt-Glaser JK. Child maltreatment and breast cancer survivors: Social support makes a difference for quality of life, fatigue and cancer stress. European Journal of Cancer (Oxford, England: 1990) 2012;48(5):728–736. doi: 10.1016/j.ejca.2011.06.022. https://doi.org/10.1016/j.ejca.2011.06.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- First MB, Gibbon M. The Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-I) and the Structured Clinical Interview for DSM-IV Axis II Disorders (SCID-II) 2004. [Google Scholar]
- Giese-Davis J, Collie K, Rancourt KMS, Neri E, Kraemer HC, Spiegel D. Decrease in depression symptoms is associated with longer survival in patients with metastatic breast cancer: A secondary analysis. Journal of Clinical Oncology. 2011;29(4):413–420. doi: 10.1200/JCO.2010.28.4455. https://doi.org/10.1200/JCO.2010.28.4455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldsmith RE, Jandorf L, Valdimarsdottir H, Amend KL, Stoudt BG, Rini C, … Bovbjerg DH. Traumatic stress symptoms and breast cancer: The role of childhood abuse. Child Abuse & Neglect. 2010;34(6):465–470. doi: 10.1016/j.chiabu.2009.10.007. https://doi.org/10.1016/j.chiabu.2009.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenberg MT, Harris AR. Nurturing mindfulness in children and youth: Current state of research. Child Development Perspectives. 2012;6(2):161–166. https://doi.org/10.1111/j.1750-8606.2011.00215.x. [Google Scholar]
- Hager AD, Runtz MG. Physical and psychological maltreatment in childhood and later health problems in women: An exploratory investigation of the roles of perceived stress and coping strategies. Child Abuse & Neglect. 2012;36(5):393–403. doi: 10.1016/j.chiabu.2012.02.002. https://doi.org/10.1016/j.chiabu.2012.02.002. [DOI] [PubMed] [Google Scholar]
- Hammen C. Stress and depression. Annual Review of Clinical Psychology. 2005;1:293–319. doi: 10.1146/annurev.clinpsy.1.102803.143938. [DOI] [PubMed] [Google Scholar]
- Hammen CL, Henry R, Daley SE. Depression and sensitization to stressors among young women as a function of childhood adversity. Journal of Consulting and Clinical Psychology. 2000;68(5):782–787. https://doi.org/10.1037//0022-006X.68.5.782. [PubMed] [Google Scholar]
- Harper FW, Schmidt JE, Beacham AO, Salsman JM, Averill AJ, Graves KD, Andrykowski MA. The role of social cognitive processing theory and optimism in positive psychosocial and physical behavior change after cancer diagnosis and treatment. Psycho-Oncology. 2007;16(1):79–91. doi: 10.1002/pon.1068. https://doi.org/10.1002/pon.1068. [DOI] [PubMed] [Google Scholar]
- Hayes AF. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach. Guilford Press; 2013. [Google Scholar]
- Hilton L, Hempel S, Ewing BA, Apaydin E, Xenakis L, Newberry S, … Maglione MA. Mindfulness meditation for chronic pain: Systematic review and meta-analysis. Annals of Behavioral Medicine. 2017;51(2):199–213. doi: 10.1007/s12160-016-9844-2. https://doi.org/10.1007/s12160-016-9844-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Himelein MJ, McElrath JAV. Resilient child sexual abuse survivors: Cognitive coping and illusion. Child Abuse & Neglect. 1996;20(8):747–758. doi: 10.1016/0145-2134(96)00062-2. https://doi.org/10.1016/0145-2134(96)00062-2. [DOI] [PubMed] [Google Scholar]
- Hofmann SG, Sawyer AT, Witt AA, Oh D. The effect of mindfulness-based therapy on anxiety and depression: A meta-analytic review. Journal of Consulting and Clinical Psychology. 2010;78(2):169. doi: 10.1037/a0018555. https://doi.org/10.1037/a0018555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holman DM, Ports KA, Buchanan ND, Hawkins NA, Merrick MT, Metzler M, Trivers KF. The association between Adverse Childhood Experiences and risk of cancer in adulthood: A systematic review of the literature. Pediatrics. 2016;138(Suppl 1):S81–S91. doi: 10.1542/peds.2015-4268L. https://doi.org/10.1542/peds.2015-4268L. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, McLaughlin KA, Green JG, Gruber MJ, Sampson NA, Zaslavsky AM, … Williams DR. Childhood adversities and adult psychopathology in the WHO World Mental Health Surveys. The British Journal of Psychiatry. 2010;197(5):378–385. doi: 10.1192/bjp.bp.110.080499. https://doi.org/10.1192/bjp.bp.110.080499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimbrough E, Magyari T, Langenberg P, Chesney M, Berman B. Mindfulness intervention for child abuse survivors. Journal of Clinical Psychology. 2010;66(1):17. doi: 10.1002/jclp.20624. https://doi.org/10.1002/jclp.20624. [DOI] [PubMed] [Google Scholar]
- King A, Wardecker BM, Edelstein RS. Personal Mastery Buffers the Effects of Childhood Sexual Abuse on Women’s Health and Family Functioning. Journal of Family Violence. 2015;30(7):887–897. https://doi.org/10.1007/s10896-015-9728-4. [Google Scholar]
- Korkeila K, Kivelä SL, Suominen S, Vahtera J, Kivimäki M, Sundell J, … Koskenvuo M. Childhood adversities, parent-child relationships and dispositional optimism in adulthood. Social Psychiatry and Psychiatric Epidemiology. 2004;39(4):286–292. doi: 10.1007/s00127-004-0740-x. https://doi.org/10.1007/s00127-004-0740-x. [DOI] [PubMed] [Google Scholar]
- Lewis CC, Simons AD, Nguyen LJ, Murakami JL, Reid MW, Silva SG, March JS. Impact of childhood trauma on treatment outcome in the treatment for adolescents with depression study (TADS) Journal of the American Academy of Child & Adolescent Psychiatry. 2010;49(2):132–140. doi: 10.1097/00004583-201002000-00007. https://doi.org/10.1016/j.jaac.2009.10.007. [DOI] [PubMed] [Google Scholar]
- Lyness JM, Noel T, Cox C, King DA, Conwell Y, Caine ED. Screening for depression in elderly primary care patients: A comparison of the Center for Epidemiologic Studies—Depression scale and the Geriatric Depression Scale. Archives of Internal Medicine. 1997;157(4):449–454. https://doi.org/10.1001/archinte.1997.00440250107012. [PubMed] [Google Scholar]
- McCaulay M, Mintz L, Glenn AA. Body image, self-esteem, and depression-proneness: Closing the gender gap. Sex Roles. 1988;18(7–8):381–391. https://doi.org/10.1007/BF00288390. [Google Scholar]
- McFarland DC, Andreotti C, Harris K, Mandeli J, Tiersten A, Holland J. Early childhood adversity and its associations with anxiety, depression, and distress in women with breast cancer. Psychosomatics. 2016;57(2):174–184. doi: 10.1016/j.psym.2015.11.008. https://doi.org/10.1016/j.psym.2015.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin KA, Sheridan MA, Lambert HK. Childhood adversity and neural development: Deprivation and threat as distinct dimensions of early experience. Neuroscience and Biobehavioral Reviews. 2014;47:578. doi: 10.1016/j.neubiorev.2014.10.012. https://doi.org/10.1016/j.neubiorev.2014.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milaniak I, Wilczek-Rużyczka E, Wierzbicki K, Sadowski J, Kapelak B, Przybyłowski P. Role of personal resources in depression and stress in heart transplant recipients. Transplantation Proceedings. 2016;48(5):1761–1766. doi: 10.1016/j.transproceed.2016.01.080. https://doi.org/10.1016/j.transproceed.2016.01.080. [DOI] [PubMed] [Google Scholar]
- Mulrow CD, Williams JW, Gerety MB, Ramirez G, Montiel OM, Kerber C. Case-finding instruments for depression in primary care settings. Annals of Internal Medicine. 1995;122(12):913–921. doi: 10.7326/0003-4819-122-12-199506150-00004. https://doi.org/10.7326/0003-4819-122-12-199506150-00004. [DOI] [PubMed] [Google Scholar]
- Muñoz RF, Beardslee WR, Leykin Y. Major depression can be prevented. American Psychologist. 2012;67(4):285–295. doi: 10.1037/a0027666. https://doi.org/10.1037/a0027666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murthi M, Espelage DL. Childhood sexual abuse, social support, and psychological outcomes: A loss framework. Child Abuse & Neglect. 2005;29(11):1215–1231. doi: 10.1016/j.chiabu.2005.03.008. https://doi.org/10.1016/j.chiabu.2005.03.008. [DOI] [PubMed] [Google Scholar]
- Nanni V, Uher R, Danese A. Childhood maltreatment predicts unfavorable course of illness and treatment outcome in depression: A meta-analysis. American Journal of Psychiatry. 2012;169(2):141–151. doi: 10.1176/appi.ajp.2011.11020335. https://doi.org/10.1176/appi.ajp.2011.11020335. [DOI] [PubMed] [Google Scholar]
- Pearlin LI, Schooler C. The structure of coping. Journal of Health and Social Behavior. 1978;19(1):2–21. [PubMed] [Google Scholar]
- Peterson C, Seligman MEP. Learned helplessness and victimization. Journal of Social Issues. 1983;39(2):103–116. https://doi.org/10.1111/j.1540-4560.1983.tb00143.x. [Google Scholar]
- Pinquart M, Duberstein PR. Depression and cancer mortality: A meta-analysis. Psychological Medicine. 2010;40(11):1797–1810. doi: 10.1017/S0033291709992285. https://doi.org/10.1017/S0033291709992285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pollak SD, Sinha P. Effects of early experience on children’s recognition of facial displays of emotion. Developmental Psychology. 2002;38(5):784–791. doi: 10.1037//0012-1649.38.5.784. https://doi.org/10.1037/0012-1649.38.5.784. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods. 2008;40(3):879. doi: 10.3758/brm.40.3.879. https://doi.org/10.3758/BRM.40.3.879. [DOI] [PubMed] [Google Scholar]
- Pudrovska T, Schieman S, Pearlin LI, Nguyen K. The sense of mastery as a mediator and moderator in the association between economic hardship and health in late life. Journal of Aging and Health. 2005;17(5):634–660. doi: 10.1177/0898264305279874. https://doi.org/10.1177/0898264305279874. [DOI] [PubMed] [Google Scholar]
- Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1(3):385–401. https://doi.org/10.1177/014662167700100306. [Google Scholar]
- Repetti RL, Taylor SE, Seeman TE. Risky families: Family social environments and the mental and physical health of offspring. Psychological Bulletin. 2002;128(2):330–366. https://doi.org/10.1037/0033-2909.128.2.330. [PubMed] [Google Scholar]
- Robb C, Lee A, Jacobsen P, Dobbin KK, Extermann M. Health and personal resources in older patients with cancer undergoing chemotherapy. Journal of Geriatric Oncology. 2013;4(2):166–173. doi: 10.1016/j.jgo.2012.12.002. https://doi.org/10.1016/j.jgo.2012.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenberg M. Society and the adolescent self-image. Middletown, CT, England: Wesleyan University Press Society; 1965. Retrieved from http://psycnet.apa.org/journals/ort/36/3/560.pdf%26productCode=pa. [Google Scholar]
- Rosenberg M, Schooler C, Schoenbach C, Rosenberg F. Global self-esteem and specific self-esteem: Different concepts, different outcomes. American Sociological Review. 1995;60(1):141–156. https://doi.org/10.2307/2096350. [Google Scholar]
- Satin JR, Linden W, Phillips MJ. Depression as a predictor of disease progression and mortality in cancer patients: A meta-analysis. Cancer. 2009;115(22):5349–5361. doi: 10.1002/cncr.24561. https://doi.org/10.1002/cncr.24561. [DOI] [PubMed] [Google Scholar]
- Scheier MF, Carver CS. Optimism, coping, and health: Assessment and implications of generalized outcome expectancies. Health Psychology. 1985;4(3):219–247. doi: 10.1037//0278-6133.4.3.219. https://doi.org/10.1037/0278-6133.4.3.219. [DOI] [PubMed] [Google Scholar]
- Scheier MF, Carver CS. Dispositional optimism and physical well-being: the influence of generalized outcome expectancies on health. Journal of Personality. 1987;55(2):169. doi: 10.1111/j.1467-6494.1987.tb00434.x. https://doi.org/10.1111/j.1467-6494.1987.tb00434.x. [DOI] [PubMed] [Google Scholar]
- Scheier MF, Carver CS, Bridges MW. Distinguishing optimism from neuroticism (and trait anxiety, self-mastery, and self-esteem): A reevaluation of the Life Orientation Test. Journal of Personality and Social Psychology. 1994;67(6):1063. doi: 10.1037//0022-3514.67.6.1063. [DOI] [PubMed] [Google Scholar]
- Scher CD, Forde DR, McQuaid JR, Stein MB. Prevalence and demographic correlates of childhood maltreatment in an adult community sample. Child Abuse & Neglect. 2004;28(2):167–180. doi: 10.1016/j.chiabu.2003.09.012. https://doi.org/10.1016/j.chiabu.2003.09.012. [DOI] [PubMed] [Google Scholar]
- Schetter CD, Dolbier C. Resilience in the context of chronic stress and health in adults. Social and Personality Psychology Compass. 2011;5(9):634. doi: 10.1111/j.1751-9004.2011.00379.x. https://doi.org/10.1111/j.1751-9004.2011.00379.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schroevers M, Ranchor AV, Sanderman R. Adjustment to cancer in the 8 years following diagnosis: A longitudinal study comparing cancer survivors with healthy individuals. Social Science & Medicine. 2006;63(3):598–610. doi: 10.1016/j.socscimed.2006.02.008. https://doi.org/10.1016/j.socscimed.2006.02.008. [DOI] [PubMed] [Google Scholar]
- Scott Heller S, Larrieu JA, D’Imperio R, Boris NW. Research on resilience to child maltreatment: empirical considerations. Child Abuse & Neglect. 1999;23(4):321–338. doi: 10.1016/s0145-2134(99)00007-1. https://doi.org/10.1016/S0145-2134(99)00007-1. [DOI] [PubMed] [Google Scholar]
- Stanton AL, Bower JE. Psychological adjustment in breast cancer survivors. Advances in Experimental Medicine and Biology. 2015;862:231. doi: 10.1007/978-3-319-16366-6_15. https://doi.org/10.1007/978-3-319-16366-6_15. [DOI] [PubMed] [Google Scholar]
- Stanton AL, Ganz PA, Rowland JH, Meyerowitz BE, Krupnick JL, Sears SR. Promoting adjustment after treatment for cancer. Cancer. 2005;104(S11):2608–2613. doi: 10.1002/cncr.21246. https://doi.org/10.1002/cncr.21246. [DOI] [PubMed] [Google Scholar]
- Stanton AL, Wiley JF, Krull JL, Crespi CM, Hammen C, Allen JJB, … Weihs KL. Depressive episodes, symptoms, and trajectories in women recently diagnosed with breast cancer. Breast Cancer Research and Treatment. 2015;154(1):105–115. doi: 10.1007/s10549-015-3563-4. https://doi.org/10.1007/s10549-015-3563-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein JA, Leslie MB, Nyamathi A. Relative contributions of parent substance use and childhood maltreatment to chronic homelessness, depression, and substance abuse problems among homeless women: Mediating roles of self-esteem and abuse in adulthood. Child Abuse & Neglect. 2002;26(10):1011–1027. doi: 10.1016/s0145-2134(02)00382-4. https://doi.org/10.1016/S0145-2134(02)00382-4. [DOI] [PubMed] [Google Scholar]
- Taylor SE. Adjustment to threatening events: A theory of cognitive adaptation. American Psychologist. 1983;38(11):1161. [Google Scholar]
- Taylor SE, Armor DA. Positive illusions and coping with adversity. Journal of Personality. 1996;64(4):873–898. doi: 10.1111/j.1467-6494.1996.tb00947.x. https://doi.org/10.1111/j.1467-6494.1996.tb00947.x. [DOI] [PubMed] [Google Scholar]
- Taylor SE, Lerner JS, Sage RM, Lehman BJ, Seeman TE. Early environment, emotions, responses to stress, and health. Journal of Personality. 2004;72(6):1365. doi: 10.1111/j.1467-6494.2004.00300.x. https://doi.org/10.1111/j.1467-6494.2004.00300.x. [DOI] [PubMed] [Google Scholar]
- Taylor SE, Seeman TE. Psychosocial resources and the SES-health relationship. Annals of the New York Academy of Sciences. 1999;896:210–225. doi: 10.1111/j.1749-6632.1999.tb08117.x. [DOI] [PubMed] [Google Scholar]
- Taylor SE, Stanton AL. Coping resources, coping processes, and mental health. Annual Review of Clinical Psychology. 2007;3:377. doi: 10.1146/annurev.clinpsy.3.022806.091520. https://doi.org/10.1146/annurev.clinpsy.3.022806.091520. [DOI] [PubMed] [Google Scholar]
- Walker EA, Unutzer J, Rutter C, Gelfand A, Saunders K, VonKorff M, … Katon W. Costs of health care use by women HMO members with a history of childhood abuse and neglect. Archives of General Psychiatry. 1999;56(7):609. doi: 10.1001/archpsyc.56.7.609. https://doi.org/10.1001/archpsyc.56.7.609. [DOI] [PubMed] [Google Scholar]
- Weisz JR, McCarty CA, Valeri SM. Effects of psychotherapy for depression in children and adolescents: A meta-analysis. Psychological Bulletin. 2006;132(1):132–149. doi: 10.1037/0033-2909.132.1.132. https://doi.org/10.1037/0033-2909.132.1.132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO. Child maltreatment. 2016 Retrieved August 16, 2017, from http://www.who.int/mediacentre/factsheets/fs150/en/
- Williams JMG, Crane C, Barnhofer T, Brennan K, Duggan DS, … Fennell MJ, et al. Mindfulness-based cognitive therapy for preventing relapse in recurrent depression: A randomized dismantling trial. Journal of Consulting and Clinical Psychology. 2014;82(2):275. doi: 10.1037/a0035036. https://doi.org/10.1037/a0035036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wingo AP, Wrenn G, Pelletier T, Gutman AR, Bradley B, Ressler KJ. Moderating effects of resilience on depression in individuals with a history of childhood abuse or trauma exposure. Journal of Affective Disorders. 2010;126(3):411–414. doi: 10.1016/j.jad.2010.04.009. https://doi.org/10.1016/j.jad.2010.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witek Janusek L, Tell D, Albuquerque K, Mathews HL. Childhood adversity increases vulnerability for behavioral symptoms and immune dysregulation in women with breast cancer. Brain, Behavior, and Immunity. 2013;30:S149–S162. doi: 10.1016/j.bbi.2012.05.014. https://doi.org/10.1016/j.bbi.2012.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zainal NZ, Booth S, Huppert FA. The efficacy of mindfulness-based stress reduction on mental health of breast cancer patients: A meta-analysis. Psycho-Oncology. 2013;22(7):1457. doi: 10.1002/pon.3171. https://doi.org/10.1002/pon.3171. [DOI] [PubMed] [Google Scholar]
- Zelazo PD, Lyons KE. The potential benefits of mindfulness training in early childhood: A developmental social cognitive neuroscience perspective. Child Development Perspectives. 2012;6(2):154–160. https://doi.org/10.1111/j.1750-8606.2012.00241.x. [Google Scholar]