Abstract
Aspects of social support during combat deployment, such as ‘unit cohesion,’ have been shown to affect later posttraumatic stress disorder (PTSD) development among veterans. We utilized a longitudinal database to assess how relationship quality with fellow soldiers in World War II (WWII) might be linked with postwar PTSD symptoms. Data were available on 101 men who experienced combat exposure in WWII documented through postwar assessment. Upon study entry (1939 to 1942), data were collected on participants' early childhood relationships quality and their emotional adjustment during college. Data on WWII experiences were collected in 1946. Relationship quality with fellow soldiers in WWII was examined as a moderator of the link between combat exposure and postwar PTSD symptoms. Prewar emotional adjustment was examined as a mediator between quality of childhood relationships and subsequent relationship quality with fellow soldiers during war. Better quality relationships with fellow soldiers attenuated (i.e., moderated) the link between combat exposure severity and PTSD symptom count, explaining a significant percent of the variance, R2 = .19, p < .001. There was also a significant indirect mediation effect of childhood relationship quality on relationships with soldiers through prewar emotional adjustment, ab = 0.02, 95% BCa CI [0.01, 0.05]. Results suggest that better peer relationship quality during deployment may reduce the likelihood of subsequent PTSD symptom development, and that the quality of early relationships may set the stage for better relationships during stressful contexts such as war. These findings have implications for PTSD risk factor screening prior to deployment, and underscore the importance of interpersonal support among soldiers during deployment.
What protects those exposed to extreme stress from debilitating psychological sequelae such as posttraumatic stress disorder (PTSD)? This question takes on particular urgency in the United States, as our most recent war veterans continue to return from the decade-long campaigns in Iraq and Afghanistan that have marked the longest sustained combat operations in U.S. history. There has been significant interest in predeployment vulnerabilities as well as protective factors during deployment that may affect PTSD development (Wright, Kelsall, Sim, Clarke, & Creamer, 2013). To date, studies have focused primarily on more recent conflicts in the Persian Gulf, Iraq, and Afghanistan (Magruder & Yeager, 2009), showing that unit cohesion buffers soldiers from the effects of combat exposure on the risk of developing PTSD (Wright et al., 2013).
This study extended this most recent line of research to World War II (WWII) veterans using a rare longitudinal database. We examined whether a related but more specific aspect of unit cohesion – the quality of relationships with fellow soldiers – predicted the likelihood of developing PTSD. We also examine predeployment factors that might predict better peer relationships during war. To our knowledge, this is one of the few studies to report on the quality of peer relationships during wartime and subsequent PTSD development in WWII combat veterans, in addition to examining the precursors of how better quality relationships might have developed.
Research on combat trauma has examined specific types of social support during war that may play a role in preventing PTSD. A common focus in prior research has been ‘unit cohesion’ (Shay, 2010). Unit cohesion is defined as assistance and encouragement during deployment from fellow unit members, leaders of the unit, and the military in general (King, King, Vogt, Knight, & Samper, 2006). Two meta-analyses have demonstrated that higher levels of unit cohesion are associated with lower risk of developing PTSD among soldiers exposed to combat (Oliver, Harman, Hoover, Hayes, & Pandhi, 1999; Wright et al., 2013). In addition, studies specific to WWII veterans have suggested that better social relationships (both during and after the war) moderate negative effects of combat (Elder & Clipp, 1988, 1989). Similarly, in nonmilitary adult populations, meta-analyses have shown that higher perceived social support in both the peritraumatic and posttraumatic contexts has protective effects on PTSD development (Brewin, Andrews, & Valentine, 2000; Ozer, Best, Lipsey, & Weiss, 2003). In addition, poor social support is thought to be an important factor in combat-exposed veterans who abuse substances (Benda, 2006), and greater social connectedness has been shown to be a protective factor against suicide in veterans (Smith et al., 2016).
The importance of interpersonal factors both during and after trauma exposure has prompted investigators to inquire about predeployment factors as possible predictors of who might go on to develop PTSD after combat. Studies have shown that early childhood adversity (Boscarino, Hoffman, Pitcavage, & Urosevich, 2015; Zheng et al., 2016) and lower levels of family cohesion (Vogt & Tanner, 2007) are associated with later PTSD development in veterans. In a retrospective study of WWII veterans two decades after the end of WWII, those who recalled more cohesive childhood family environments also recalled their combat units as more cohesive and reported more social support (Kang, Aldwin, Choun, & Spiro, 2016), which in turn led to fewer PTSD symptoms. The findings of this study support the hypothesis that positive early environments typically lead to better attachment and emotional stability, which in turn leads to the ability to form friendships and gain social support in adulthood, especially during times of stress. In addition, recent efforts have assessed the degree of predeployment emotional stability and overall adjustment of soldiers as potential PTSD risk factors. Studies have shown that negative emotionality (Karstoft, Statnikov, Andersen, Madsen, & Galatzer-Levy, 2015) and types of temperament (e.g., Type D, distressed personality; Mommersteeg et al., 2011) just prior to deployment are predictive of PTSD symptoms following combat. Taken together, these findings emphasize the importance of examining soldiers' childhood environments and their emotional adjustment prior to deployment.
The present study used a rare longitudinal database that spanned adolescence to late life, including data on WWII military service, to examine risk and protective factors around combat exposure. We hypothesized that better relationship quality with fellow soldiers would be linked with fewer PTSD symptoms reported immediately after WWII. In addition, we hypothesized that better relationships in childhood as well as stable emotional adjustment in college (prior to deployment) would predict better relationships with wartime peers and fewer postwar PTSD symptoms.
Method
Participants and Procedure
Between 1939 and 1942, a university health service recruited 268 male college sophomores (aged 18 to 19 years) for an intensive multidisciplinary study (Heath, 1945; Vaillant, 2000). These students were selected because college entrance examinations revealed no significant mental or physical health problems, and their deans perceived them as likely to become successful adults. All were white. 50.2% were on scholarships or needed to work during college to meet expenses, and 64.3% eventually obtained graduate degrees. In post-college adult life, most worked as physicians, lawyers, university professors, or business executives. The students' parents were interviewed, and extensive family, social, and medical histories were obtained. On entering the study, the men were assessed by internists, psychiatrists, psychologists, and anthropologists. Participants completed questionnaires every two years thereafter, and they were reinterviewed by study staff at approximately ages 25, 30, and 50 years. Of the original study group of 268 men, 12 dropped out of the study during college and 8 were killed in WWII. There were 224 men who served in the military and survived WWII; combat data was available for 202 of these men (89 with no combat, 113 with combat). The subset of 101 participants in the current study was selected based on the availability of data from early childhood, college rating of prewar emotional adjustment, rating of relationship with fellow soldiers, and documented exposure to combat in WWII as reported during postwar interview and questionnaire assessments. There were 12 participants with combat exposure who were excluded from analyses due to incomplete data; independent samples t tests showed that the differences between these 12 participants and this study's sample were not statistically significant for the following measures: combat exposure, number of PTSD symptoms, early relationships quality, and prewar college adjustment. Of the 12 excluded, only one of these men filled out the ‘relationship with fellows’ section of the postwar questionnaire, so this could not be adequately compared. In addition, t tests also determined that the 101 individuals we ultimately included in our sample did not differ significantly from the other 89 participants without combat exposure in terms of IQ, social class, quality of early childhood relationships, prewar adjustment to college, and relationship quality with fellow soldiers during WWII. Data for the specific branch of military service during WWII were available for 72 of the 101 participants in our sample: 39.6% were Navy, 21.8% were Army, 6.9% were Air Force, 2.0% were Marines, and 1.0% were Coast Guard, with 28.7% (29 participants) unknown. Data in the current study were collected at 3 specific time points: (1) childhood relationship quality upon study entry when participants were ages 18 to 19 years of age (1939 to 1942); (2) college adjustment during college prior to the war; and (3) wartime experiences within a year after return home from deployment in WWII (January to October, 1946). All procedures involved with the study were reviewed and approved by the Partners Human Research Committee.
Measures
Quality of early childhood relationships
Upon study entry (1939 to 1942), two independent raters assessed the quality of each participant's relationship with parents and siblings during childhood and adolescence, after reviewing the following data: psychiatrist's and family worker's notes on the participant's reports of his home life; family worker's interviews with parents; and a developmental history obtained from parents by the family worker. Ratings of sibling relationship quality were made on a 3-point scale (0 = severe rivalry or conflict in the absence of closeness with at least one sibling, 1 = absence of closeness with at least one sibling and absence of severe sibling rivalry or conflict, and 2 = close relationship with at least one sibling). Participants who were close to at least one sibling were rated as such even if relations with other siblings were characterized as conflictual or not close. Previous research has shown that a close relationship with at least one sibling can be protective for adult outcomes such as depression and mood-altering drug use, even when controlling for hereditary factors (Waldinger, Vaillant, & Orav, 2007). The two coders' ratings were added, and summed scores were raised by 1, resulting in a scale of 1 to 5. All participants in this sample had at least one sibling. Parent relationship quality ratings were made on a 3-point scale (0 = distant, hostile, or smothering, 1 = average, and 2 = nurturing, encouraged positive autonomy, fostered self-esteem). The two coders' ratings were added, and each summed score was raised by 1, resulting in a scale of 1 to 5. Interrater reliability for these childhood measures was good (r = .71; Vaillant, 1974).
Predictive validity for these variables has been supported in several prior studies (Lee, Vaillant, Torrey, & Elder, 1995; Waldinger et al., 2007), including a study by McLaughlin et al. (2010), in which childhood environment predicted an elevated risk for developing mood and anxiety disorders in adulthood. Because the focus in the present study is on relationship quality, an overall composite for the quality of early childhood relationships was made by summing the 3 available relationship measures for the men's mother, father, and siblings from 3 (worst score) to 15 (best score).
Prewar Emotional Adjustment
During their college careers, the men were assessed by psychiatrists through in-person interviews and self-report on their level of emotional stability (Heath, 1945). At that time, study staff created a 3-item scale of emotional adjustment in college that rated the likelihood the participant would encounter emotional difficulties in the future based on their personality assessment: 1 = likely to encounter difficulties, 2 = may encounter intermediate difficulty, 3 = very unlikely to encounter difficulties. In prior studies this rating was found to predict successful psychosocial adjustment at age 65 (G. E. Vaillant & Vaillant, 1990) and better mental health between ages 50 to 65 years (G. Vaillant, Templeton, Ardelt, & Meyer, 2008).
Combat Exposure Scale
In 1946, a comprehensive questionnaire asking about participants' war experiences was sent to all 224 surviving men who had served in the military; 217 (97.1%) completed the questionnaire. In the same year, most of these men were interviewed in-person by the study staff about their wartime experiences (Monks, 1957). Both the questionnaire and the interview focused on the effects of the war, the men's exposure to combat, and their descriptions of thoughts and bodily symptoms in the face of danger. Combat exposure was measured through two aspects that together form the Combat Exposure Scale: (1) an interview focused on the presence of specific combat experiences, and (2) a self-report of participants' perception and quantity of the danger level to which they were exposed. The first aspect was based on the men's responses to combat-related questions, with the following six experiences coded as 1 (present) or 0 (absent) for six possible points: being under enemy fire, firing at the enemy, killing anyone, seeing allies killed or wounded, seeing the enemy killed or wounded, and being wounded. The second aspect was based on the sustained danger scale (Monks, 1957), a self-report scale created by study staff prior to 1946. The highest level on this scale represented severe danger at the height of action with the enemy (e.g., “being shelled heavily”, “vessel hit”, and “heavy combat with enemy”), the moderate level represented experience in clearly dangerous contexts (“sporadic action with enemy”, “bomb disposal”, and sporadic shelling”), and the lowest category represented complete absence of combat-related danger. Four points were possible from this danger scale depending on how many days the participant spent in either the severe or moderate danger levels (0 = no days; 1 = 1 to 21 days; 2 = 22 days or more) and the highest level of danger they experienced (0 = no danger, 1 = moderate danger, 2 = severe danger). The combination of these two aspects resulted in the Combat Exposure Scale (Lee et al., 1995), a 10-point scale which assesses exposure to specific combat experiences and the extent to which a person was exposed to sustained danger. For instance, in order to score 6 out of the maximum 10 points, a participant might have been exposed to four wartime experiences (4 points), and spent 15 days (1 point) at the moderate danger level (1 point).
All variables that created the Combat Exposure Scale were significantly intercorrelated at p < .001, except that being wounded was not significantly correlated with high level of perceived danger. In the current study, Cronbach's alpha for this scale was .74. The Combat Exposure Scale is unique in that it combines both self-report and interview methods, and its two aspects share similarity to two subscales of the widely used Deployment Risk and Resilience Inventory research tool (Subscale D: combat experiences, Subscale G: perceived threat; Vogt et al., 2013). The Combat Exposure Scale has been supported in prior studies as a predictor of PTSD symptoms and early mortality following WWII (Lee et al., 1995), as well as a predictor of later life well-being in WWII veterans (Ardelt, Landes, & Vaillant, 2010). In the present study all individuals had combat exposure (range: 1 to 10 points), and 55.4% of the sample had higher levels of exposure (≥ 6 points).
Relationship quality with fellow soldiers
To assess how well each participant got along with the unit members with whom they were in most contact and on whom they might rely for support during the stressful context of war, the 1946 postwar assessment included a self-report scale to assess the participant's quality of relationships with fellow soldiers of similar rank (Monks, 1957). In particular, study staff were interested in a social relationship measure that focused on peer interaction, rather than asking about relationships within the military hierarchy (i.e., this measure did not focus on superiors). This was a 7-item self-report scale: 7 = got on superbly with everyone in outfit [the respondent's company of 80 to 120 men]; 6 = excellent relationships with everyone in own group [platoon of 15 to 30 men], no friction with anyone in outfit; 5 = good relationships with own group, maybe minimum friction with particularly difficult person; 4 = got on well with most fellows in own group, some friction elsewhere; 3 = though a definite part of the group, slight difficulty with own group, as well as elsewhere; 2 = moderate amount of difficulty with most of group; 1 = got on well with no one, accepted almost no one as friend, rejected by nearly all.
Number of postwar PTSD Symptoms (DSM-III-R; 3rd ed., rev.; DSM-III-R; American Psychiatric Association [APA], 1987)
A psychiatrist unaware of all other data reviewed two sources of information: (a) interview transcripts from postwar interviews done from January to August of 1946 and, (b) a questionnaire sent to participants in September of 1946 regarding war experiences. From this information 16 symptoms – subsequently included in the DSM-III-R definition of PTSD – were rated as present or absent: distressing recollections of the traumatic event, dreams about the trauma, acts as if traumatic event were recurring, distress at symbol of trauma, avoids thought/feelings of trauma, avoids activities/situations of trauma, cannot recall important aspects of traumatic event, diminished interest in significant activities, estrangement from others, restricted range of affect, sense of a foreshortened future, sleep difficulties, angry outbursts, difficulty concentrating, hypervigilance, and exaggerated startle response. In a previous study using this sample (Lee et al., 1995), Combat Exposure Scale scores were significantly linked with more PTSD symptoms. Analyses are based on the DSM-III-R definition of PTSD, as diagnostic information was rated by study staff before DSM-IV (4th ed.; DSM-IV; American Psychiatric Association, 1994) and DSM-V (5th ed.; DSM-5; American Psychiatric Association, 2013) PTSD criteria had been developed. However, the criteria used are consistent with modern criteria regarding PTSD symptoms, and diagnoses were made by trained psychiatrists on the basis of multiple data sources. The DSM-III-R includes symptom descriptions that align with the four DSM-V symptom criterion categories: B (intrusion), C (avoidance), D (negative alterations in cognitions and mood), and E (alterations in arousal and reactivity). The DSM-III-R includes all DSM-V symptoms in Criteria B and C, and all but one in Criterion E (i.e., ‘self-destructive or reckless behavior’). Criterion D represents the largest difference, with DSM-III-R covering 4 of the 7 DSM-V symptoms listed in this category.
Data Analysis
Distributions for variables were first examined for normality. In our combat-exposed sample, 25.7% had one or more symptoms of PTSD (from DSM-III-R criteria) with two participants meeting full criteria for PTSD, resulting in a positive skew due to the high number of participants with no symptoms. Therefore, a square-root transformation was conducted for this variable prior to analyses. Pearson correlations (2-tailed) were first examined among variables of interest. Based on these correlations, we conducted two hierarchical linear regression analyses: (1) a moderation model (predictors mean-centered) to test whether combat exposure interacts with relationship quality with fellow soldiers to predict number of postwar PTSD symptoms, and (2) a mediation model utilizing bias-corrected bootstrapping methods to test whether prewar emotional adjustment mediated a link between early childhood relationships and relationship quality with fellow soldiers in WWII. Analyses were conducted using IBM SPSS version 23 via the PROCESS macro for SPSS v2.13.2 macro by Andrew F. Hayes (Hayes, 2013). To probe the interaction model we utilized the Johnson-Neyman technique (Bauer & Curran, 2005; Johnson & Neyman, 1936) from the PROCESS macro to inform where in the distribution of the proposed moderator (i.e., relationship quality with fellow soldiers) combat exposure may have had an effect on number of PTSD symptoms (Figure 1). This technique has advantages over the selection of various values of the moderator to estimate the conditional effect, as it derives appropriate values of the moderator to be tested that better reflect a ‘region of significance’ of the effect of X on Y (Hayes, 2013). In addition, an output option utilizing simple slopes from the PROCESS macro for visualizing the conditional effect of combat exposure on memory at three values of the moderator (low, mean, and high) was utilized to construct a graphical representation for the moderation model (Figure 2). To assess the strength of any indirect effect in our mediation analysis, we utilized the ‘kappa-squared’ index from the PROCESS output. This index is defined as the ratio of the indirect effect relative to its maximum possible value in the data, it is bounded between 0 and 1 with a value closer to 1 representing a bigger indirect effect (Preacher & Kelley, 2011).
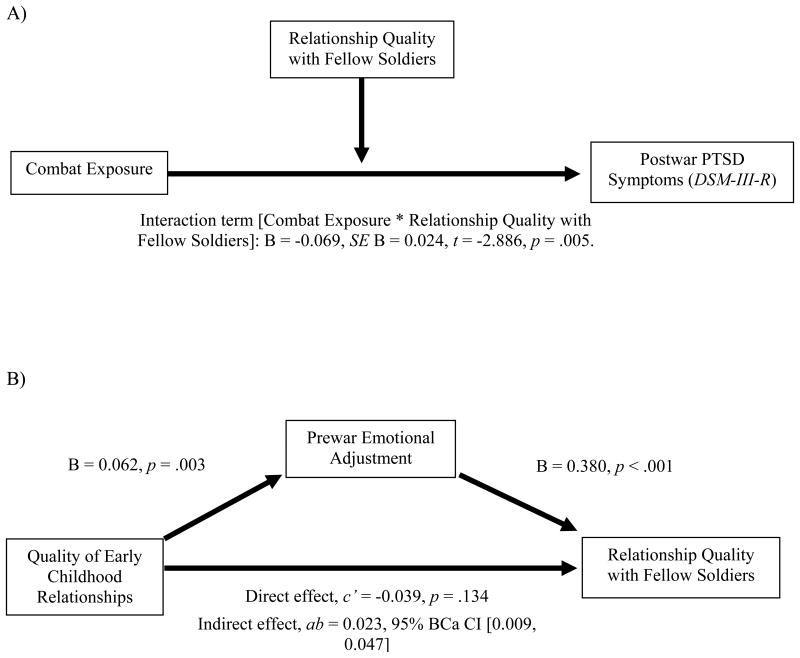
Figure 1.
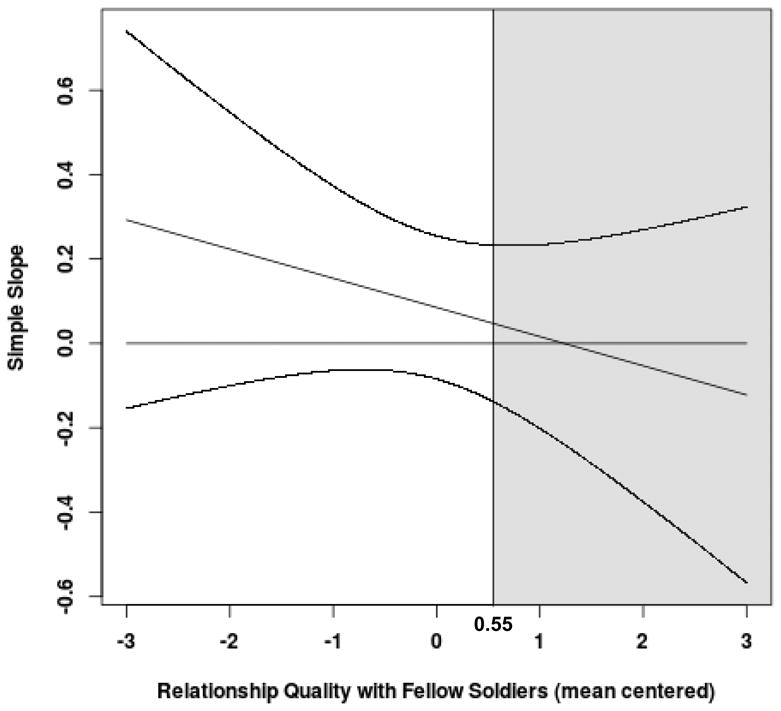
Region of significance (nonshaded area) and confidence bands for the conditional effect of combat exposure level on number of DSM-III-R PTSD (APA, 1987) symptoms at values of the moderator (relationship quality with fellow soldiers).
Figure 2.
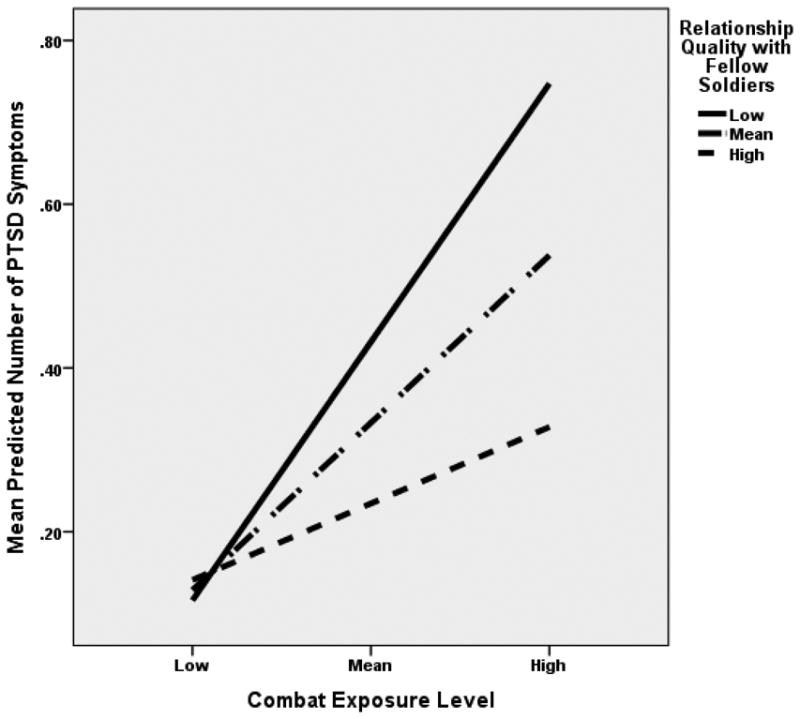
Levels of relationship quality with fellow soldiers as a moderator between combat exposure level and mean number of DSM-III-R (APA, 1987) posttraumatic stress disorder (PTSD) symptoms.
Results
Means, standard deviations, and correlations among variables of interest are presented in Table 1. We found statistically significant negative associations between relationship quality with fellows and number of postwar PTSD symptoms. In addition, prewar emotional adjustment was positively linked with early childhood relationships and relationships with peers, and prewar emotional adjustment was negatively linked with number of PTSD symptoms. As expected, statistically significant links were found between number of PTSD symptoms and combat exposure.
Table 1. Means, Standard Deviations, and Pearson Correlations.
| Prewar variables | Warzone variables | Postwar variable | |||
|---|---|---|---|---|---|
| Quality of Early Childhood Relationships | Prewar Emotional Adjustment | Combat Exposure Scale | Relationship Quality with Fellow Soldiers | Number of PTSD Symptoms (DSM-III-R) | |
| Prewar Emotional Adjustment | 0.26** | — | |||
| Combat Exposure Scale | 0.10 | -0.13 | — | ||
| Relationship Quality with Fellow Soldiers | -0.07 | 0.35** | -0.16 | — | |
| Number of DSM-III-R PTSD Symptoms | 0.09 | -0.22* | 0.30** | -0.24* | — |
| Mean | 8.92 | 2.25 | 5.68 | 5.25 | 0.53 |
| SD | 2.88 | 0.68 | 2.40 | 0.67 | 1.20 |
| Potential Score Range | 3 – 15 | 1 – 3 | 1 – 10 | 1 – 7 | 0 – 16 |
Note: N = 101. All p values are two-tailed. PTSD = posttraumatic stress symptoms.
p < .05.
p < .01.
Relationship quality with fellow soldiers was examined as a potential moderator of the link between combat exposure level and number of PTSD symptoms (Figure 3). The overall model showed a main effect that explained 18.8% of the variance (p < .001) in number of postwar PTSD symptoms (Table 2). The regression coefficient for the product of relationship with fellow soldiers and combat exposure was statistically different from zero (B = -0.069, p = .005), meaning that the effect of combat exposure on PTSD symptoms depended on the level relationship quality with fellow soldiers. The Johnson-Neyman technique revealed that for values of relationship quality with fellows (mean-centered) less than M = 0.55 (equivalent to a raw score of 5.8 on the self-report scale), the conditional effect of combat on number of PTSD symptoms was increasingly positive and remained statistically different from zero (see Figure 1). For values of relationship quality with fellow soldiers greater than or equal to 0.55 (mean-centered), the conditional effect was not statistically significant. Therefore, the positive relationship between combat exposure and number of postwar PTSD symptoms was exacerbated in those with poor relationship quality with fellow soldiers, and in those with higher quality relations with fellow soldiers, the association between combat and PTSD symptoms was not affected (Figure 2). Prewar emotional adjustment was also examined as a moderator of the link between combat and number of PTSD symptoms, but the interaction term was not significant, suggesting the specific role of relationship factors during, rather than prior to, wartime.
Figure 3.
Regression models: (A) relationships with fellow soldiers moderates the association between combat exposure and number of DSM-III-R posttraumatic stress disorder (PTSD) symptoms (R2 = .19, p < .001); (B) prewar emotional adjustment mediates the association between quality of early childhood relationships and relationships with fellow soldiers (R2 = .15, p < .001).
Table 2. Relationship Quality with Fellow Soldiers (Moderator), Predicting Number of Postwar DSM-III-R Posttraumatic Stress Disorder (PTSD) symptoms.
| Model | B | SE B | t | p |
|---|---|---|---|---|
| Constant | 0.333 | 0.059 | 5.642 | < .001 |
| Relationship Quality with Fellow Soldiers | -0.147 | 0.067 | -2.207 | .030 |
| Combat Exposure | 0.085 | 0.020 | 4.300 | < .001 |
| Relationship Quality with Fellow Soldiers * Combat Exposure | -0.069 | 0.024 | -2.886 | .005 |
Note. Model summary: R2 = .188, mean square error (MSE) = .348, F(3, 97) = 9.476, p < .001.
We next tested a model that examined whether prewar emotional adjustment mediated the link between the quality of early childhood relationships and relationship quality with fellow soldiers (Figure 3). There was a significant indirect effect of the quality of early childhood relationships on relationships with fellow soldiers through prewar emotional adjustment, ab = 0.023, 95% BCa CI [0.009, 0.047]. This represented a relatively small effect, κ2 = .11, 95% BCa CI [.04, .20], and the overall mediation model (mean squared error = 0.39, F = 7.69, df = 98) accounted for 14.6% (p < .001) of the variance in the quality of relationships with fellow soldiers. In separate models, we also investigated whether or not early relationships quality or prewar emotional adjustment moderated the relationship between combat exposure and number of postwar PTSD symptoms. However, the interaction terms were non-significant: early relationships quality (p = .731 for interaction term), prewar emotional adjustment (p = .313 for interaction term).
Discussion
As soldiers continue to return from long battle campaigns, it is imperative that we gain a clearer understanding of those factors that foster and those that protect against PTSD. In a unique cohort of male WWII veterans, our results are consistent with the hypothesis that better quality relationships with fellow soldiers may play a protective role against postwar PTSD symptoms, particularly at higher levels of combat exposure. Given this finding, we examined possible precursors of better wartime relationships and found that better childhood relationships led to higher quality peer relationships by fostering healthy prewar emotional adjustment in young adulthood. Although unit cohesion has been studied extensively as a possible protective factor in other wars, this study represents a rare opportunity to examine the role of peer relationships in a WWII cohort.
One of the unique aspects of the current study is that research staff inquired about PTSD symptoms long before the diagnostic category was established. It has been difficult to determine the general prevalence of PTSD among WWII veterans (Langer, 2011), and ours is one of the very few studies to have conducted post-WWII assessments that aligned with the later definition of PTSD (DSM-III-R). However, our sample's rates of postwar PTSD (2.0%) and any postwar PTSD symptom (25.7%) are lower compared with more recent studies. For example, a study of U.S. Army soldiers in the Iraq War by Milliken et al. investigated PTSD prevalence at a median of 6 months after return from deployment utilizing the 4-item Primary Care PTSD Screen (PC-PTSD; positive screen if ‘yes’ to any 3 items) and 3 questions on combat experiences (Milliken, Auchterlonie, & Hoge, 2007). They found that 29% of active duty personnel and 38.6% of reserve personnel answered ‘yes’ to at least one of the 4-items on the PC-PTSD, with 9.1% of active duty and 14.3% of reserves having a positive screen for PTSD. These differences compared with our data may be due to more accurate contemporary screening tools, and/or that Milliken et al. exclusively studied the Army branch of service. Some studies have shown that those who served in the Army have a higher risk for a positive PTSD screen compared with other branches of military service (OR = 2.67; Dursa, Reinhard, Barth, & Schneiderman, 2014), and our sample had many fewer Army participants (less than half of the total sample, at most). Furthermore, the PC-PTSD brief self-report screen utilized by Milliken et al. has been shown to have a high sensitivity (.91) and therefore may potentially overestimate PTSD prevalence rates (Bliese et al., 2008).
The majority of previous studies assessing unit cohesion have used the unit support subscale of the Deployment Risk and Resilience Inventory or similar self-report measures (Dickstein et al., 2010; Du Preez, Sundin, Wessely, & Fear, 2012; Iversen et al., 2008; Jones et al., 2012). These measures typically combine two different constructs: (a) the individual's experience with colleagues (e.g., ‘I felt valued by my fellow unit members’), and (b) the individual's experience with unit leaders (e.g., ‘My service was appreciated by the leaders in my unit’). In contrast to most previous studies that used a definition of unit cohesion that encompasses relationships with unit leaders and out-of-unit personnel (King et al., 2006), the current study is unique in its specific focus on peer relationships during combat.
Our findings are consistent with the hypothesis that early childhood relationships may lay the groundwork for better young adult peer relations during stressful situations such as combat exposure, which may in turn prevent PTSD symptoms. These findings are also consistent with prior studies showing that better early relationships predicted less likelihood of developing PTSD after exposure to trauma. For example, Kang et al. (2016) found that soldiers from WWII and the Korean war who retrospectively recalled cohesive childhood environments were more likely to recall more cohesiveness in their military unit, and developed fewer PTSD symptoms than those who had conflictual childhood environments and less supportive wartime experience. Furthermore, prior research on attachment shows that healthy early relationships and nurturance increase the potential for better relationships under stressful contexts as adults (Bowlby, 1988). By contrast, those who are insecurely attached perceive less social support during stress and subsequently develop more PTSD symptoms than those who are securely attached (Besser & Neria, 2012; Besser, Neria, & Haynes, 2009).
How might better peer relationships during wartime protect combat-exposed soldiers from developing PTSD symptoms? Existing literature demonstrates support for the notion that “lifelong friendships” and strengthened social ties are positive outcomes of war service that could lessen the negative effects of combat exposure on PTSD symptom development (Spiro III, Schnurr, & Aldwin, 1997). It is hypothesized that painful memories of war and stress symptoms in later life are likely to weaken through exposure to a supportive community of servicemates and/or spouses (Elder & Clipp, 1988). Work by Elder & Clipp (1988) shows that veterans exposed to heavy combat are more likely to have enduring social ties with military fellows than veterans who were exposed to less combat. This may be due to the fact that experiencing hardship and learning to navigate the loss of comrades instills in military men a heightened appreciation of life and friendship (Settersten, 2006). Men who maintained these relationships over time scored lower on trauma memory scales compared with men who did not have a supportive community of servicemates (Elder & Clipp, 1988, 1989). These studies suggest that stronger relationships during combat may be more likely to be maintained, or serve as a marker for other supportive relationships that may attenuate development of PTSD symptoms (Ingraham & Manning, 1986).
Strengths of this investigation include its naturalistic longitudinal design, use of multiple methods (self-reports, interviews, multiple assessors), and postwar measures done within 10 months after return from combat. The study also has limitations that are important to acknowledge. A potential disadvantage of our measure of relationship quality with fellow soldiers is that it was created by the original study staff and, in contrast to the Deployment Risk and Resilience Inventory, has not been tested in multiple populations. Furthermore, over half of our participants reported very positive relationships with peers and on average manifested good emotional adjustment on entering the war – qualities that might or might not be generalizable to other groups of soldiers. Because this sample was comprised of predominantly middle-class and upper-middle-class Caucasian males from an elite university who served in WWII, all from two-parent families with siblings, we must be cautious about generalizing our findings to female soldiers, and to those from other ethnic groups, social classes, and historical birth cohorts. However, even in this privileged cohort with good prewar emotional adjustment, the ability to form close friendships, and fewer PTSD symptoms, we found that peer relationships were still protective. Finally, our main finding that relationship quality with fellows moderates the link between combat exposure level and PTSD symptoms is based on data that are cross-sectional rather than prospective, as these data were collected concurrently during the 1946 postwar timeframe.
To our knowledge, the current study is the first to investigate the quality of wartime peer relationships and subsequent PTSD development in WWII combat veterans, as well as the first to examine antecedents of peer relations in wartime in this population. In addition to examining these links in more diverse groups of individuals exposed to combat, it will be important in future studies to focus on the ways that a sense of belonging to a peer group during potentially traumatic experiences may contribute to the development of resiliency. Examining the neurophysiology of social support during times of stress and its potential role as a buffer against negative sequelae may be a logical next step. Based on the current work and existing literature, it is reasonable to suggest that relationships in both the pre-war and deployment contexts should be taken into account as potential markers for PTSD risk. Potential clinical implications may involve screening and interventions based on theories of belonging (Baumeister & Leary, 1995). Specifically in military personnel, measures of low belonging are associated with increased depression both pre- and postdeployment (Bryan & Heron, 2015), and higher thwarted belongingness measures (i.e., the feeling that one does not belong) are positively associated with PTSD symptoms (Pennings, Finn, Houtsma, Green, & Anestis, 2016). Furthermore, examples of interventions to increase social belonging in vulnerable groups undergoing stressful transitions (e.g., African American students about to start college) show benefit even 3 years post intervention (Walton & Cohen, 2011). This study joins a host of others suggesting that social connections can support resilience in the face of stress.
Acknowledgments
This study was supported by grants from the National Institute on Aging (R01 AG045230). Dr. Nevarez, Ms. Yee, and Dr. Waldinger report no conflicts of interest.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 3rd ed., rev. Washington, DC: Author; 1987. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. Washington, DC: Author; 1994. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. Washington, DC: Author; 2013. [Google Scholar]
- Ardelt M, Landes SD, Vaillant GE. The Long-Term Effects of World War II Combat Exposure on Later Life Well-Being Moderated by Generativity. Research in Human Development. 2010;7:202–220. https://doi.org/10.1080/15427609.2010.504505. [Google Scholar]
- Bauer DJ, Curran PJ. Probing Interactions in Fixed and Multilevel Regression: Inferential and Graphical Techniques. Multivariate Behavioral Research. 2005;40:373–400. doi: 10.1207/s15327906mbr4003_5. https://doi.org/10.1207/s15327906mbr4003_5. [DOI] [PubMed] [Google Scholar]
- Baumeister RF, Leary MR. The need to belong: desire for interpersonal attachments as a fundamental human motivation. Psychological Bulletin. 1995;117:497–529. https://doi.org/10.1037/0033-2909.117.3.497. [PubMed] [Google Scholar]
- Benda BB. Survival Analyses of Social Support and Trauma Among Homeless Male and Female Veterans Who Abuse Substances. American Journal of Orthopsychiatry. 2006;76:70–79. doi: 10.1037/0002-9432.76.1.70. https://doi.org/10.1037/0002-9432.76.1.70. [DOI] [PubMed] [Google Scholar]
- Besser A, Neria Y. When home isn't a safe haven: Insecure attachment orientations, perceived social support, and PTSD symptoms among Israeli evacuees under missile threat. Psychological Trauma: Theory, Research, Practice, and Policy. 2012;4:34–46. https://doi.org/10.1037/a0017835. [Google Scholar]
- Besser A, Neria Y, Haynes M. Adult attachment, perceived stress, and PTSD among civilians exposed to ongoing terrorist attacks in Southern Israel. Personality and Individual Differences. 2009;47(8):851–857. https://doi.org/10.1016/j.paid.2009.07.003. [Google Scholar]
- Bliese PD, Wright KM, Adler AB, Cabrera O, Castro CA, Hoge CW. Validating the primary care posttraumatic stress disorder screen and the posttraumatic stress disorder checklist with soldiers returning from combat. Journal of Consulting and Clinical Psychology. 2008;76:272–281. doi: 10.1037/0022-006X.76.2.272. https://doi.org/10.1037/0022-006X.76.2.272. [DOI] [PubMed] [Google Scholar]
- Boscarino JA, Hoffman SN, Pitcavage JM, Urosevich TG. Mental Health Disorders and Treatment Seeking Among Veterans in Non-VA Facilities: Results and Implications from the Veterans' Health Study. Military Behavioral Health. 2015;3:244–254. doi: 10.1080/21635781.2015.1077179. https://doi.org/10.1080/21635781.2015.1077179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowlby J. A Secure Base: Clinical Applications of Attachment Theory. Psychology Press; 1988. [Google Scholar]
- Brewin CR, Andrews B, Valentine JD. Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults. Journal of Consulting and Clinical Psychology. 2000;68:748–766. doi: 10.1037//0022-006x.68.5.748. https://doi.org/10.1037//0022-006x.68.5.748. [DOI] [PubMed] [Google Scholar]
- Bryan CJ, Heron EA. Belonging protects against postdeployment depression in military personnel. Depression and Anxiety. 2015;32:349–355. doi: 10.1002/da.22372. https://doi.org/10.1002/da.22372. [DOI] [PubMed] [Google Scholar]
- Dickstein BD, McLean CP, Mintz J, Conoscenti LM, Steenkamp MM, Benson TA, Litz BT. Unit cohesion and PTSD symptom severity in Air Force medical personnel. Military Medicine. 2010;175:482–486. doi: 10.7205/milmed-d-09-00178. https://doi.org/10.7205/milmed-d-09-00178. [DOI] [PubMed] [Google Scholar]
- Du Preez J, Sundin J, Wessely S, Fear NT. Unit cohesion and mental health in the UK armed forces. Occupational Medicine (Oxford, England) 2012;62:47–53. doi: 10.1093/occmed/kqr151. https://doi.org/10.1093/occmed/kqr151. [DOI] [PubMed] [Google Scholar]
- Dursa EK, Reinhard MJ, Barth SK, Schneiderman AI. Prevalence of a positive screen for PTSD among OEF/OIF and OEF/OIF-era veterans in a large population-based cohort. Journal of Traumatic Stress. 2014;27:542–549. doi: 10.1002/jts.21956. https://doi.org/10.1002/jts.21956. [DOI] [PubMed] [Google Scholar]
- Elder GH, Clipp EC. Wartime losses and social bonding: influences across 40 years in men's lives. Psychiatry. 1988;51:177–198. doi: 10.1080/00332747.1988.11024391. https://doi.org/10.1080/00332747.1988.11024391. [DOI] [PubMed] [Google Scholar]
- Elder GH, Clipp EC. Combat experience and emotional health: impairment and resilience in later life. Journal of Personality. 1989;57:311–341. doi: 10.1111/j.1467-6494.1989.tb00485.x. https://doi.org/10.1111/j.1467-6494.1989.tb00485.x. [DOI] [PubMed] [Google Scholar]
- Hayes AF. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach. Guilford Press; 2013. https://doi.org/10.1111/jedm.12050. [Google Scholar]
- Heath CW. What people are; a study of normal young men. Cambridge, Mass: Harvard University Press; 1945. [Google Scholar]
- Ingraham L, Manning F. Military Psychiatry: A Comparative Perspective. New York: Greenwood; 1986. American military psychiatry; pp. 22–65. [Google Scholar]
- Iversen AC, Fear NT, Ehlers A, Hacker Hughes J, Hull L, Earnshaw M, Hotopf M. Risk factors for post-traumatic stress disorder among UK Armed Forces personnel. Psychological Medicine. 2008;38:511–522. doi: 10.1017/S0033291708002778. https://doi.org/10.1017/S0033291708002778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson PO, Neyman J. Tests of certain linear hypotheses and their application to some educational problems. Statistical Research Memoirs. 1936;1:57–93. [Google Scholar]
- Jones N, Seddon R, Fear NT, McAllister P, Wessely S, Greenberg N. Leadership, cohesion, morale, and the mental health of UK Armed Forces in Afghanistan. Psychiatry. 2012;75:49–59. doi: 10.1521/psyc.2012.75.1.49. https://doi.org/10.1521/psyc.2012.75.1.49. [DOI] [PubMed] [Google Scholar]
- Kang S, Aldwin CM, Choun S, Spiro A. A Life-span Perspective on Combat Exposure and PTSD Symptoms in Later Life: Findings From the VA Normative Aging Study. The Gerontologist. 2016;56:22–32. doi: 10.1093/geront/gnv120. https://doi.org/10.1093/geront/gnv120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karstoft KI, Statnikov A, Andersen SB, Madsen T, Galatzer-Levy IR. Early identification of posttraumatic stress following military deployment: Application of machine learning methods to a prospective study of Danish soldiers. Journal of Affective Disorders. 2015;184:170–175. doi: 10.1016/j.jad.2015.05.057. https://doi.org/10.1016/j.jad.2015.05.057. [DOI] [PubMed] [Google Scholar]
- King LA, King DW, Vogt DS, Knight J, Samper RE. Deployment Risk and Resilience Inventory: A Collection of Measures for Studying Deployment-Related Experiences of Military Personnel and Veterans. Military Psychology. 2006;18:89–120. https://doi.org/10.1207/s15327876mp1802_1. [Google Scholar]
- Langer R. Combat Trauma, Memory, and the World War II Veteran. War, Literature & the Arts. 2011;23(1):50. [Google Scholar]
- Lee KA, Vaillant GE, Torrey WC, Elder GH. A 50-year prospective study of the psychological sequelae of World War II combat. The American Journal of Psychiatry. 1995;152:516–522. doi: 10.1176/ajp.152.4.516. https://doi.org/10.1176/ajp.152.4.516. [DOI] [PubMed] [Google Scholar]
- Magruder KM, Yeager DE. The Prevalence of PTSD Across War Eras and the Effect of Deployment on PTSD: a Systematic Review and Meta-Analysis. Psychiatric Annals. 2009;39:778–788. https://doi.org/10.3928/00485713-20090728-04. [Google Scholar]
- McLaughlin KA, Kubzansky LD, Dunn EC, Waldinger R, Vaillant G, Koenen KC. Childhood social environment, emotional reactivity to stress, and mood and anxiety disorders across the life course. Depression and Anxiety. 2010;27:1087–1094. doi: 10.1002/da.20762. https://doi.org/10.1002/da.20762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milliken CS, Auchterlonie JL, Hoge CW. Longitudinal assessment of mental health problems among active and reserve component soldiers returning from the Iraq war. JAMA. 2007;298:2141–2148. doi: 10.1001/jama.298.18.2141. https://doi.org/10.1001/jama.298.18.2141. [DOI] [PubMed] [Google Scholar]
- Mommersteeg PMC, Denollet J, Kavelaars A, Geuze E, Vermetten E, Heijnen CJ. Type D personality, temperament, and mental health in military personnel awaiting deployment. International Journal of Behavioral Medicine. 2011;18:131–138. doi: 10.1007/s12529-010-9096-7. https://doi.org/10.1007/s12529-010-9096-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monks JP. College men at war. Boston: American Academy of Arts and Sciences; 1957. [Google Scholar]
- Oliver LW, Harman J, Hoover E, Hayes SM, Pandhi NA. A quantitative integration of the military cohesion literature. Military Psychology. 1999;11:57–83. https://doi.org/10.1207/s15327876mp1101_4. [Google Scholar]
- Ozer EJ, Best SR, Lipsey TL, Weiss DS. Predictors of posttraumatic stress disorder and symptoms in adults: a meta-analysis. Psychological Bulletin. 2003;129:52–73. doi: 10.1037/0033-2909.129.1.52. https://doi.org/10.1037//0033-2909.129.1.52. [DOI] [PubMed] [Google Scholar]
- Pennings SM, Finn J, Houtsma C, Green BA, Anestis MD. Posttraumatic Stress Disorder Symptom Clusters and the Interpersonal Theory of Suicide in a Large Military Sample. Suicide & Life-Threatening Behavior. 2016 doi: 10.1111/sltb.12317. https://doi.org/10.1111/sltb.12317. [DOI] [PubMed]
- Preacher KJ, Kelley K. Effect size measures for mediation models: Quantitative strategies for communicating indirect effects. Psychological Methods. 2011;16:93–115. doi: 10.1037/a0022658. https://doi.org/10.1037/a0022658. [DOI] [PubMed] [Google Scholar]
- Settersten RA. When Nations Call: How Wartime Military Service Matters for the Life Course and Aging. Research on Aging. 2006;28:12–36. https://doi.org/10.1177/0164027505281577. [Google Scholar]
- Shay J. Achilles in Vietnam: Combat Trauma and the Undoing of Character. Scribner; 1994. [Google Scholar]
- Smith NB, Mota N, Tsai J, Monteith L, Harpaz-Rotem I, Southwick SM, Pietrzak RH. Nature and determinants of suicidal ideation among U.S. veterans: Results from the national health and resilience in veterans study. Journal of Affective Disorders. 2016;197:66–73. doi: 10.1016/j.jad.2016.02.069. https://doi.org/10.1016/j.jad.2016.02.069. [DOI] [PubMed] [Google Scholar]
- Spiro A, III, Schnurr PP, Aldwin CM. A life-span perspective on the effects of military service. Journal of Geriatric Psychiatry. 1997;30:91–128. [Google Scholar]
- Vaillant GE. Adaptive mental mechanisms. Their role in a positive psychology. The American Psychologist. 2000;55:89–98. doi: 10.1037//0003-066x.55.1.89. https://doi.org/10.1037//0003-066x.55.1.89. [DOI] [PubMed] [Google Scholar]
- Vaillant GE, Vaillant CO. Natural history of male psychological health, XII: a 45-year study of predictors of successful aging at age 65. The American Journal of Psychiatry. 1990;147:31–37. doi: 10.1176/ajp.147.1.31. https://doi.org/10.1176/ajp.147.1.31. [DOI] [PubMed] [Google Scholar]
- Vaillant G, Templeton J, Ardelt M, Meyer SE. The Natural History of Male Mental Health: Health and Religious Involvement. Social Science & Medicine (1982) 2008;66:221–231. doi: 10.1016/j.socscimed.2007.09.011. https://doi.org/10.1016/j.socscimed.2007.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vaillant GE. Natural history of male psychological health: Ii. some antecedents of healthy adult adjustment. Archives of General Psychiatry. 1974;31:15–22. doi: 10.1001/archpsyc.1974.01760130005001. https://doi.org/10.1001/archpsyc.1974.01760130005001. [DOI] [PubMed] [Google Scholar]
- Vogt DS, Tanner LR. Risk and resilience factors for posttraumatic stress symptomatology in Gulf War I veterans. Journal of Traumatic Stress. 2007;20:27–38. doi: 10.1002/jts.20187. https://doi.org/10.1002/jts.20187. [DOI] [PubMed] [Google Scholar]
- Vogt D, Smith BN, King LA, King DW, Knight J, Vasterling JJ. Deployment risk and resilience inventory-2 (DRRI-2): an updated tool for assessing psychosocial risk and resilience factors among service members and veterans. Journal of Traumatic Stress. 2013;26:710–717. doi: 10.1002/jts.21868. https://doi.org/10.1002/jts.21868. [DOI] [PubMed] [Google Scholar]
- Waldinger RJ, Vaillant GE, Orav EJ. Childhood sibling relationships as a predictor of major depression in adulthood: a 30-year prospective study. The American Journal of Psychiatry. 2007;164:949–954. doi: 10.1176/ajp.2007.164.6.949. https://doi.org/10.1176/ajp.2007.164.6.949. [DOI] [PubMed] [Google Scholar]
- Walton GM, Cohen GL. A brief social-belonging intervention improves academic and health outcomes of minority students. Science (New York, NY) 2011;331:1447–1451. doi: 10.1126/science.1198364. https://doi.org/10.1126/science.1198364. [DOI] [PubMed] [Google Scholar]
- Wright BK, Kelsall HL, Sim MR, Clarke DM, Creamer MC. Support mechanisms and vulnerabilities in relation to PTSD in veterans of the Gulf War, Iraq War, and Afghanistan deployments: a systematic review. Journal of Traumatic Stress. 2013;26:310–318. doi: 10.1002/jts.21809. https://doi.org/10.1002/jts.21809. [DOI] [PubMed] [Google Scholar]
- Zheng WY, Kanesarajah J, Waller M, McGuire AC, Treloar SA, Dobson AJ. Childhood adversity and traumatic exposures during deployment as predictors of mental health in Australian military veterans. Australian and New Zealand Journal of Public Health. 2016;40:10–15. doi: 10.1111/1753-6405.12499. https://doi.org/10.1111/1753-6405.12499. [DOI] [PubMed] [Google Scholar]