Abstract
Objective
To explore whether a text message-based relapse prevention intervention (PIER1) is acceptable to treatment-seeking adults with opioid use disorder (OUD) after Emergency Department (ED) discharge using mixed methods design.
Methods
Adults seeking care in an urban ED for OUD (N=20; M age=22; 55% female; 75% white race) completed a baseline survey, and were invited to enroll in PIER1, which was delivered in 7-day blocks, with the option to re-enroll at the end of each block, up to four blocks. PIER1 included a morning “push” message focused on positive thinking, adaptive coping feedback tailored to twice daily assessments of craving severity and contextual correlates of craving, and end-of-day feedback on daily opioid use and goal commitment. Participants were asked to complete a follow-up phone interview after the first 7 days of PIER1. Transcripts were thematically coded.
Results
17/20 participants enrolled in PIER1. In the first 7 days, response rates to text message assessments averaged 30%. 10/17 participants re-enrolled after 7-days. Main themes from follow-up interviews (n=9) included ease of use, social connection, and self-empowerment. Participants desired more personalized support and the ability to communicate through text messaging with a human about their struggles. Event-level data suggests that higher craving severity increased risk of opioid lapses.
Conclusion
In this mixed-methods intervention development study, we found conflicting evidence supporting an automated text message intervention providing relapse prevention support for treatment-seeking individuals with OUD discharged from the ED. Qualitative feedback suggests that PIER1 could be useful and acceptability enhanced through personalized human support.
Keywords: opioid use disorder, behavioral, intervention
INTRODUCTION
The Emergency Department (ED) is an important contact point for individuals with opioid use disorder (OUD) (Weiss et al., 2016). Although the current standard of care in the ED for individuals with OUD is referral to detoxification and addiction treatment, seamless and immediate linkage to services remains sub-optimal, largely due to limited treatment capacity (Jones et al., 2015). The time between ED discharge and initiation of treatment is a vulnerable period (Gossop et al., 2002). Early in recovery, many individuals struggle with symptoms related to opioid withdrawal and have limited ability to cope with triggers for opioid use (Daughters et al., 2005), precipitating drug lapses and loss of motivation for abstinence (Redko et al., 2006).
Interventions that reduce early relapse among motivated individuals with OUD prior to detoxification and treatment initiation are needed (Larimer et al., 1992), Mobile technology (a.k.a. mHealth) behavioral interventions may be able to assist in this process by providing support in real-world contexts, at times and in situations when it may be most needed (“just-in-time”) (Nahum-Shani et al., 2016). They can also potentially offer greater privacy, convenience, and reach than in-person interventions (Litvin et al., 2012). Systematic reviews of computerized interventions for substance use disorders have shown to be effective as adjuncts to in-person treatment (Moore et al., 2011) but little is known about the efficacy of stand-alone mHealth programs for OUD (Guarino et al., 2016; Gustafson et a., 2016).
One mobile communication modality that could be used to efficiently deliver behavioral interventions for OUD is text messaging (Smith, 2011). It has advantages over other mobile platforms in being proactive, simple to interact with, and inexpensive (Suffoletto, 2016). These features may be particularly relevant for individuals with OUD, who may not have the patience or desire to navigate through pages of support materials, and for the short-term support that is needed for individuals with impaired executive function associated with substance use (Arias et al., 2016). We designed an interactive, automated text message intervention focused on providing individuals with support over the vulnerable period between ED discharge and treatment entry called PIER1 (Preventing and Interrupting Early Relapse).
PIER1 was based largely on theories that have been found to be useful in predicting and promoting behavior change for addiction (Webb et al., 2010) and incorporates techniques found to be effective in prior digital interventions (Heckler et al., 2016): assisting self-monitoring (Control Theory: Carver & Scheier, 1982), teaching adaptive coping skills (Self-Regulation Theory: Muraven & Baumeister, 2000), prompting goal commitment (Goal Setting Theory: Locke & Latham, 1990); and providing feedback on performance (Social Cognitive Theory: Bandura, 1977).
These techniques were operationalized through the following intervention components: (1) a morning reflection message; (2) two ecological momentary assessment (EMA) batteries delivered randomly during two day-time blocks that assessed severity of craving, and the relation of withdrawal symptoms, mood and anxiety, and environmental triggers to craving; (3) tailored feedback to help individuals cope with these triggers; (4) feedback specific to end-of-day report of illicit opioid use; (5) a goal commitment prompt and support for daily abstinence; and (6) user-triggered “just-in-time” craving support.
Automated responses were drawn from “libraries” of text messages initially written by a physician with experience in developing text message interventions (BS), reviewed by an addiction specialist (AD), and refined by three different adults who had a history of OUD. Message content was informed by cognitive behavioral therapy (Kiluk, 2010) and motivational interviewing (Miller & Rollnick, 2013) and selected according to an algorithm based on the participant’s response. PIER1 was delivered in 7-day blocks, with the option to re-enroll at the end of each 7-week block, up to four blocks.
Following recommendations for developing effective digital interventions (Collins et al., 2005; van Gement-Pijnen et al., 2011), we examined both quantitative outcomes and qualitative feedback from participants. For quantitative outcomes, we measured text message assessment response rates over the first 7 days, voluntary PIER1 re-enrollment rates for each subsequent 7-day block, and patient perceptions of PIER1 features. We chose to focus on response rates over the first 7 days as this was the outer limit to the amount of time we expected it to take in our region for an individual to initiate detoxification and/or treatment. We hypothesized that participants would respond to at least half of the assessments over the first 7 days, that most (at least 50%) participants would re-enroll after the first 7 days. We also thematically coded qualitative feedback to further examine acceptability. We explored event-level data and qualitative feedback to inform behavioral targets and techniques. Findings from this preliminary study could help guide further development of text-message interventions to prevent early relapse after ED discharge for adults with OUD.
2. METHODS
2.1. Procedures
2.1.a. Recruitment and enrollment in the ED
From July 17 to August 20, 2016 a convenience sample of patients (aged 18 to 60) who presented to an urban ED requesting detoxification for opioids and with a positive urine drug screen for opiates were identified through medical record review. If a patient agreed to be approached, research staff discussed the study procedures and obtained verbal consent for the anonymous collection of screening data. Eligible participants who had their own cellular phone with text messaging and had a Rapid Opioid Dependence Scale (RODS; Wickersham et al., 2015) score >3 (maximum score= 7) were invited to participate. Patients who provided written informed consent for study participation completed a baseline questionnaire. Participants were given a $15 debit card for completing the baseline survey. All procedures were approved by the university’s institutional review board. Enrolled patients received standard care in the ED, which included a handout providing names, locations, and telephone numbers of local detoxification and treatment services. No patients were offered medication assisted treatment, but all were offered mediations to help mitigate withdrawal symptoms, including clonidine and loperamide.
2.1.b. PIER1 (see Appendix for PIER1 flow chart)
Prior to ED discharge, participants were instructed on how to opt-in to initiate PIER1 by texting in a keyword. Upon enrolling, the participant received a series of welcome text messages, including instructions to text the keyword “crave” for immediate support, and to text “quit” to stop the program at any time. When possible, we checked the participant’s phone to ensure the welcome messages were received. Beginning on the day following enrollment, participants received morning reflection messages aimed at increasing positive cognitions about success in recovery (Krentzman, 2013), e.g., “Begin by visualizing yourself as a non-user. Think about what that person would look like, act and do. You may only have to change a little to accomplish this!”
Twice a day, during a randomly selected time between 9am and 1pm and 3pm and 6pm, participants received the query: “How strong is your urge to use opioids right now, on a scale from 0 (not at all) to 100 (completely)?” (Wasan et al. 2012). Based on their reported craving severity score, participants received a graded feedback message, i.e. “You report a high amount of craving right now” (if score >60). Participants then received the query: “Are physical withdrawal symptoms contributing to this sensation?” If they affirmed withdrawal symptoms, they received a message focused on assisting symptom management (Ziedonis et al., 2009). Participants then received the query: “Is your mood or anxiety level affecting any urge to use opioids?” If they reported contribution of mood or anxiety to craving, they received a message focused on stress management (Hendershot, Witkiewitz, George, & Marlatt, 2011). As the final query in the module, participants received: “Is your immediate environment (including people) contributing to this craving?” If they affirmed a contextual cue, they received a message focused on context management (Garland & Howard, 2014), e.g., “It is a good sign that you noticed a risky situation. Try to separate yourself.”
Each evening at 8pm, participants received the query: “Have you used any opioids in the past 24 hours?” If a participant responded that they had not used, they received a positive feedback message. If the participant reported opioid use, they received a message attempting to mitigate “abstinence violation” effects (Birke et al., 1990). Participants then received the query: “Would you be willing to commit to a goal to stay sober for the next 24 hours?” If the participant endorsed willingness to commit to staying sober, they received a positive reinforcement message. If goal commitment was not endorsed, participants received a message “rolling with resistance”. Goal commitment was included as a key feature because it has been shown to increase behavior change (Locke & Latham, 2003) and reduce substance use specifically (Kelly et al., 2016).
At the end of a 7-day PIER1 intervention block, participants received summary messages. For example, participants received a message tallying the total number of days with opioid use reported and another message framing their progress as positive (if they reported less than daily use) or concerning (if they reported opioid use every day). After the summaries, participants were provided the option to opt-in to continue: “Please text us ‘go’ if you want to continue with us for 1 more week.”
For all PIER1 queries, if a participant did not respond within 1 hour, they received a re-prompt. If a participant did not respond within 1 hour of the re-prompt, the response window closed. Any text sent by participants outside the 2 hour window prompted the reply message, “We are unable to respond to you right now. If you have a medical emergency, please dial 911 or contact your doctor.” As part of the informed consent process, participants were instructed to set up a password on their phones, turn off lock screen text notifications, and delete any texts that they did not want someone else to see.
2.1.c. Phone follow-up
All participants, regardless of duration of PIER1 enrollment, were asked to complete a follow-up phone call around 7 days after ED enrollment. At least 3 attempts were made to reach participants. Each phone call lasted between 10 and 15 minutes. We used a structured interview guide that used open-ended questions to assess perceived usability and benefit, which included, for example: “Were there any particular features of the texting program that you found especially helpful or useful?” and “Were there any particular features of the texting program that you did not find helpful or useful?” Participants received a $20 debit card for completing the follow-up interview.
2.2. Measures
2.2.a Baseline Assessments
We collected the RODS score as a measure of OUD during screening. The RODS was chosen because it is a brief tool that is feasible to complete in the limited time available in the ED. Participants reported their age, sex, race, ethnicity, education, and occupation. We measured frequency of substance use over the past 3 months using the NIDA Modified Alcohol, Smoking and Substance Involvement Screening Test (ASSIST) (Humeniuk et al., 2008). Cigarette use was recoded as: less than daily=0 and at least daily use=1. Other substances used were recoded into dichotomous variables (none=0; any=1). We used the Stages of Change Readiness and Treatment Eagerness Scale (SOCRATES-8D; Miller & Tonigan, 1996) to assess readiness to change opioid use. Responses were scored and summed to yield three scale scores: Recognition (7 items), Ambivalence (4 items), and Taking Steps (8 items). We also obtained self-reports of prior treatment for OUD.
2.2.b. Text Message Assessments
To understand craving severity, we created a variable “maximum craving” based on the highest reported craving severity in a given day. To understand presence of correlates of craving, opioid use and commitment to a sober goal, all other query replies were coded as No=0; Yes=1. All queries that did not receive a response within the time-window were coded as missing.
2.2.c. Perceptions of PIER1
We measured perceptions of PIER1 through qualitative feedback provided in exit phone interviews. We first transcribed all interviews verbatim. A preliminary codebook was created based on close readings of the transcripts, incorporating explicit domains from interview guides (deductive themes) as well as recurrent unanticipated themes that were emergent across transcripts (inductive themes). Coded text was reviewed through an iterative process, resulting in refined themes. We did not systematically examine interrater reliability of coding.
2.3. Data Analyses
We first examined baseline sample characteristics, using descriptive statistics to visually examine differences by length of PIER1 enrollment. We then calculated text-message query response rates and descriptive statistics of responses in the first 7 days. We plotted each participant’s reports of maximum craving and opioid use over time to understand both missing response patterns and relationships between craving severity and subsequent opioid lapses. To gain insights into perceptions of the PIER1 program and features, we examined themes in exit interviews. We chose participant quotes that represented both the majority sentiments within each theme as well as any quote that offered a contrasting opinion within that theme.
3.0 RESULTS
3.1. PIER1 Participants
20 participants completed baseline assessment in the ED (55% female, 75% white race, mean age= 22.0, SD=1.8). Baseline descriptive statistics are reported in Table 1. Most participants (90%) had undergone some OUD treatment in the past, and most (80%) had undergone treatment more than once. There was a higher rate of heroin use (90%) than prescription opioid use (70%). Co-substance use (based on the ASSIST reports) was common. Participants ranked low on recognition, ambivalence, and taking steps (based on SOCRATES-8 scores).
Table 1.
Sample descriptive statistics
| Characteristics | ED Enrolled (n=20) | PIER1, 7-days (n=7) | PIER1, 14-days (n=5) | PIER1, 21-days (n=3) | PIER1, 28-days (n=2) |
|---|---|---|---|---|---|
| Age, mean (SD) | 22 (1.8) | 32.7 (11) | 38.4 (8.0) | 49.3 (8.1) | 31 (11.3) |
| Age, range | 21–56 | 22–56 | 29–49 | 40–55 | 23–39 |
| Female, n (%) | 11 (55%) | 5 (71.4%) | 4 (80%) | 0 | 1 (50%) |
| Race, n(%) | |||||
| White/Caucasian | 15 (75%) | 6 (85.7%) | 3 (60%) | 2 (66.7%) | 2 (100%) |
| African American | 2 (10%) | 0 | 1 (20%) | 0 | 0 |
| Other | 3 (15%) | 1 (14.4%) | 1 (20%) | 1 (33.3%) | 0 |
| Hispanic ethnicity, n (%) | 0 | ||||
| Education | |||||
| Did not complete high school | 2 (10%) | 1 (14.3%) | 0 | 0 | 1 (50%) |
| High school graduate or GED | 9 (45%) | 4 (57.1%) | 1 (20%) | 1 (33%) | 0 |
| Some college | 6 (30%) | 2 (28.6%) | 1 (20%) | 2 (66.7%) | 1 (50%) |
| Post-graduate degree | 2 (10%) | 0 | 2 (40%) | 0 | 0 |
| Vocational | 3 (15%) | 0 | 1 (20%) | 0 | 0 |
| Occupation | |||||
| Stay-at-home parent | 2 (10%) | 1 (14.3) | 1 (20%) | 0 | 0 |
| Labor | 8 (40%) | 2 (28.6%) | 2 (40%) | 2 (66.7%) | 0 |
| None | 10 (50%) | 4 (57.1%) | 2 (40%) | 1 (33.3%) | 2 (100%) |
| Past treatment for substance use | |||||
| Never, n(%) | 2 (10%) | 1 (16.7%) | 0 | 0 | 1 (50%) |
| Median (IQR) | 3 (1–4) | 2 (1–4) | 5 (2–6) | 3 (2–3) | 4 (0–8) |
| Opioid Use Dependence (RODS score=7) | 12 (60%) | 4 (57.1%) | 4 (80%) | 1 (33.3%) | 1 (50%) |
| Opioid use | |||||
| Prescriptions | 14 (70%) | 4 (57.1%) | 4 (80%) | 3 (100%) | 2 (100%) |
| Heroin | 18 (90%) | 7 (100%) | 5 (100%) | 1 (33.3%) | 2 (100%) |
| Other drug use, n (%) | |||||
| At least daily tobacco | 14 (70%) | 5 (71.4) | 5 (100%) | 1 (33.3%) | 2 (100%) |
| Any cannabis | 10 (50%) | 5 (73.4%) | 1 (20%) | 1 (33.3%) | 1 (50%) |
| Any cocaine | 11 (55%) | 5 (73.4%) | 3 (60%) | 1 (33.3%) | 1 (50%) |
| Any stimulants | 7 (35%) | 3 (42.0%) | 2 (40%) | 0 | 1 (50%) |
| Any sedatives | 13 (65%) | 5 (73.4%) | 1 (20%) | 2 (66.7%) | 1 (50%) |
| Stage of Change, Median (IQR) scores | |||||
| Recognition | 27 (24–28) | 28 (21–28) | 25 (24–28) | 27 (23–28) | 26.5 (26–27) |
| Ambivalence | 12 (10–13) | 12 (10–15) | 11 (8–12) | 13 (11–14) | 11 (7–15) |
| Taking Steps | 26 (21–18) | 24 (20–27) | 26 (24–28) | 26 (13–29) | 22 (16–28) |
3.2. PIER1 Engagement
Among the 20 participants enrolled, 17 texted-in to initiate PIER1 for 7 days. 10/17 participants opted-in after the first 7-day intervention block, 5/10 opted-in after the second 7-day block, and 2/5 opted-in after the third 7-day block. Table 1 shows characteristics of the entire cohort as well as by length of PIER1 enrollment. Those who opted-in to PIER1 for 7-days only had lower perceived importance of substance use treatment at baseline than those who opted-in for longer periods. There were no clear differences in opioid use severity (RODS score) or stage of change (SOCRATES-8D scores) by duration of voluntary engagement.
3.3. Event-level Data
3.3.a. Response Rates
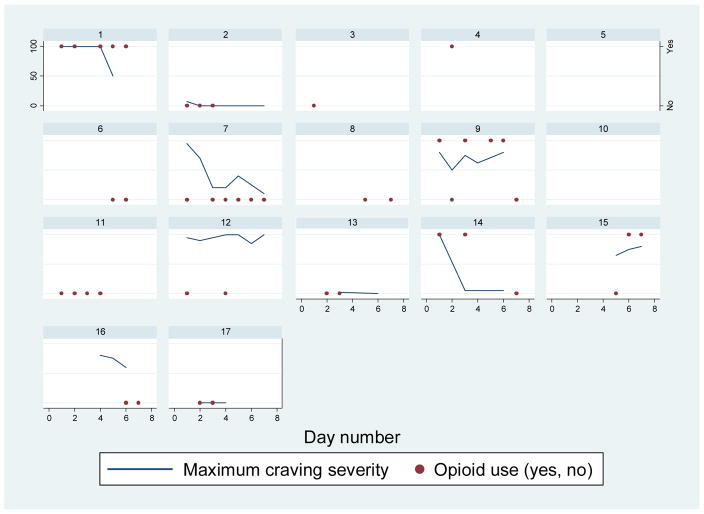
Over the first 7 days, 32/119 (26.9%) morning craving queries were replied to: 2 participants replied to a maximum of 5/7 days and 5 participants did not reply at all. 32/119 (26.9%) afternoon craving queries were replied to: 2 participants replied to a maximum of 6/7 days and 3 participants did not reply at all. 45/119 (37%) end-of-day opioid use queries were replied to: 2 participants responded to a maximum of 6/7 days and 2 participants did not reply at all. Each participant’s response patterns of maximum craving severity and opioid use across time are depicted in Figure 1.
Figure 1.
Reports of Max Craving Severity and Opioid Use over Time
Lines represent the highest value of AM and PM craving severity reported each day, labeled on left Y-axis. Circles represent opioid use reported on a given day, labeled on right Y-axis.
3.3.b. Craving severity
Over the first 7 days, out of the 48 occasions where at least one AM or PM craving severity report was made, maximum craving scores clustered at 0 (18.8% of reports) and 100 (22.9% of reports), with a median score of 68. When craving was reported, withdrawal symptoms were reported as contributing 65% of the time, anxiety contributing 73% of the time and the environment contributing to craving 21% of the time. The pairwise correlations between AM and PM craving reports were high (r=0.75).
3.3.c. Opioid Use
Over the first 7 days, opioid use was reported 14 times. At least one opioid use lapse was reported by 5/17 participants one participant reporting a maximum of 5 days of opioid use. On the 11 occasions where any craving severity and end-of day opioid use were reported, the median maximum craving score was 80 (IQR 75–100), whereas on the 16 occasions when no opioid use were reported, the median max craving score was 30 (IQR 5–80; rank sum test (p<0.0001). The relationships between daily max craving and opioid use by different durations of PIER1 engagement can be seen in Figure 1.
3.3.d. Goal Commitment
In the first 7 days, participants reported willingness to commit to a goal to stay sober 30 times and did not agree to commit 4 times. 16 out of 17 participants agreed to commit to a goal at least once, with one participant agreeing all 5 days they responded. Of the 14 times when participants reported yes to goal commitment and replied to the opioid use query the following day, the goal was met 4 times. Of the 22 times when participants reported either no to goal commitment or did not respond to the goal query, they reported opioid use the next day 7 times.
3.4. Qualitative Feedback
3.4.a. Overall themes
We were able to reach 10 participants (M age=34.8; 60% female; 10% black race) for follow-up phone calls, but lost one interview due to technical error, leaving 9 interviews for analysis. The interviewed group did not differ from those not interviewed on demographics, substance use severity, stage of change, or by intervention engagement. Those who completed interviews had a range of intervention engagement, with 2 participants not responding at all to the queries, 1 responding to only a few queries and 2 responding to almost every query. The main themes that emerged from the exit interviews were that PIER1 was easy to use, helped individuals feel connected, and empowered them to control their opioid use. In regards to the ease of use, one participant stated: “you can just text a couple words and you don’t have to put people in your business or like get really stressed out to the point where it’s a conversation.” The feeling of connection with someone was almost universal, and seemed to be especially important among this group because social ties were typically frayed or non-existent. According to one participant: “It’s nice when it says ‘we’ll check on you later’ and then they really do. Because that’s something that friends will say but they never really do.” Other participants commented that it was too difficult to talk to family because of stigma or the emotional drain inherent in such a conversation. Participants felt empowered by PIER1 to monitor and enact specific thoughts about being sober. One commented: ““…little things help keep the positivity going, and it makes you feel like you’re accomplishing something.”
3.4.b. Specific intervention features
Regarding specific features, participants universally liked the morning reflections. One participant detailed why the positive morning message was important: “It’s easy for me to wake up and be in the wrong place, and that was a good way to realign where I want to be.” The response to the craving queries was mixed. Many commented that they were useful as a measure of how they were doing. A couple of participants stated that the queries actually may have triggered cravings. Regarding the various queries about correlates of craving (e.g., withdrawal, mood, environment), participants generally felt they were useful. One participant said: “I guess people might tend to not really consider that, so breaking it down to little specifics helps lead you to a certain conclusion.” Participants felt comfortable reporting opioid use through text messaging. One commented that they liked PIER1’s feedback to help reframe a lapse: “You’re already hard on yourself. I did like that it encourages you to keep going.”
3.4.c. Suggestions for Intervention Improvement
Participants offered several suggestions for improvement. Several participants commented that the messages should be more personalized. One suggested: “The responses were kind of limited, maybe there is a way you could incorporate the subject being able to type a message.” Moreover, several participants stated that they wanted to be able to express their feelings about their cravings in a more personal way, outside of the “Yes/No” responses, and went on to suggest incorporating the ability for individuals to communicate with live people through texts about their struggles to increase motivation and feelings of social connection. One participant had a useful idea of tailoring the responses to craving based on past reports. For example, instead of reporting “high” craving, if it was less than their prior craving, then PIER1 could provide feedback on this improvement. Several participants commented that missing responses were due to the fact that they entered treatment facilities where cell phones were not allowed. They suggested providing an easy way to stop the program when these situations happen and to easily re-start it when they get their phones back.
4. Discussion
4.1. Main Findings
In this mixed-methods intervention development study, we found conflicting evidence in support of a theory-based relapse-prevention text message intervention for treatment-seeking individuals with OUD. On one hand, most participants (85%) texted in to initiate the program, among whom more than half (59%) re-enrolled voluntarily after 7 days. These findings were consistent with our a priori hypotheses and are considered markers for acceptability, especially given that participants were not monetarily incentivized to either enroll in PIER1 or respond to our text queries. On the other hand, overall response rates to the queries were low (30%), suggesting that participants did not have the ability or interest in interacting with the program in the context of their daily lives. For example, a couple of participants told us that they were in treatment programs that disallowed private mobile phone use. Despite variable and sub-optimal EMA completion, qualitative feedback suggests that most participants found benefit in using the program when they need it. The heterogeneity of intervention use supports tailoring to patient-specific preferences that are adaptable, rather than imposing uniform “doses” of message content and frequency.
Event-level data from text message responses suggests that higher craving severity is associated with increases risk of opioid lapses. In a recent review of text message interventions for drug dependence by Tofighi et al., 8 out of 11 studies incorporated some form of daily craving assessment. Our findings provide further evidence for designing features that use craving reports to either decrease the sensation of craving or provide skills to manage craving Also, all participants agreed to commit to daily abstinence goals at least once over the first week, suggesting that assisting abstinence through goal-commitment is acceptable to treatment-seeking individuals with OUD. Low rates of goal success (~28%) indicate the difficulties in this population in maintaining abstinence after ED discharge and highlight the importance of design refinements that support goal striving.
Main themes from qualitative feedback suggest that the intervention was accepted due to its ease of use, its ability to make vulnerable individuals with frayed and unreliable social networks feel connected to someone who is reliable and non-judgmental, and its ability to bring about confidence in managing contextual triggers. There was a concern among a couple of individuals that the assessments of craving could have led to lapses. In a recent study, Roth et al. (2017) found that 15/38 injection drug users who were exposed to a simulated mobile computerized EMA program reported that repetitive questioning about mood or drug use could potentially cause psychological (i.e., anxiety) or behavioral (i.e., drug use relapse) risks to individuals with OUD. However, all participants in their study indicated that completing the EMAs could also be beneficial as a potential catalyst for thinking reflectively about drug use.
Participants also provided useful suggestions for improvement, including the option to converse in more detail with a human through text messaging. Data from related fields (White WL et al., 2012) as well as for methamphetamine users (Reback et al., 2012) suggests that this could be accomplished with trained peer recovery support coaches who track text message responses and provide more detailed feedback and support. Early evidence suggests that trained peers providing telephone counseling could be useful for individuals with OUD (Winhusen T et al., 2016). Despite the lack of measures to safeguard patient privacy inherent in digital transmission of drug-related data, no participant mentioned this as a concern in follow-up interviews. Designs could minimize the potential for others to see sensitive data by codifying queries, like the craving query highlighted by Tofighi et al. (2017): “How are the skies in the past 24 hours? Respond SKIES clear, cloudy, rainy, snowy, or other.”
To our knowledge, this is the first report of a theory-based text-message program aimed at helping individuals early in recovery from OUD. Text messaging has been pilot tested as part of aftercare for substance use treatment. For example, Gonzales et al. (2014) found that participants in a texting aftercare pilot program reported significantly less substance use problem severity and were more likely to participate in extracurricular recovery behaviors compared to the standard aftercare group. Recently, Tofighi et al. (2016) asked 97 adults with OUD who were enrolled in buprenorphine treatment to complete a survey to understand preferences for a text message intervention. Most participants were interested in information pertaining to buprenorphine treatment and messages to help them reduce the risk of relapse. Also, the highest proportion of participants wanted the intervention delivered during the early phase of recovery. Importantly, PIER1 was designed to fill this critical service gap.
4.2. Limitations
This was a pilot study with a small number of participants. Participants were sampled from an urban ED, were mostly heroin users, and therefore may not represent adults with OUD broadly. All outcome data were self-report and subject to possible bias. We did not use randomization procedures given the primary aim of determining acceptability, and therefore are unable to comment on whether PIER1 reduces opioid use. We did not systematically record other treatments that participants were receiving during their exposure to PIER1 (i.e. methadone), and therefore cannot comment on whether these treatments were associated with PIER1 usage or reporting. We found low and variable completion of EMA, limiting interpretation of event-level associations. Finally, although there was a range of PIER1 program engagement among those who completed phone follow-up, roughly half of those enrolled went missing, potentially biasing qualitative findings.
4.3 Conclusions
In this early-phase intervention development study, we found conflicting evidence supporting an automated text message intervention providing relapse prevention support for treatment-seeking individuals with OUD discharged from the ED. Individuals liked the types of support provided, but did not respond to the daily text queries as much as expected, limiting potential effectiveness. Future digital communication interventions should tailor both content and schedule to individual needs, reduce the burden of daily assessments, allow more qualitative expression of experiences and challenges, and integrate human support to enhance engagement.
Supplementary Material
Acknowledgments
Funding: Emergency Medicine Foundation (EMF), in partnership with the National Institute of Drug Abuse (NIDA)
We would like to thank Jennifer Matesa and Lori Rogal for their feedback on intervention materials and Greg Schmutz for his tireless programming work. We would also like to thank Joshua Sojda for his help in developing the intervention. Joshua died of an opioid overdose. This work is in honor of his fight.
Works Cited
- Arias F, Arnsten JH, Cunningham CO, Coulehan K, Batchelder A, Brisbane M, Segal K, Rivera-Mindt M. Neurocognitive, psychiatric, and substance use characteristics in opioid dependent adults. Addict Behav. 2016 Sep;60:137–43. doi: 10.1016/j.addbeh.2016.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bandura A. Self-Efficacy: The Exercise of Control. New York: W.H. Freeman;; 1997. [Google Scholar]
- Birke SA, Edelmann RJ, Davis PE. An analysis of the abstinence violation effect in a sample of illicit drug users. Br J Addict. 1990;85(10):1299–307. doi: 10.1111/j.1360-0443.1990.tb01606.x. [DOI] [PubMed] [Google Scholar]
- Carver CS, Scheier MF. Control theory: a useful conceptual framework for personality, social, clinical and health psychology. Psychol Bull. 1982;92:111–35. [PubMed] [Google Scholar]
- Collins LM, Murphy SA, Nair VN, Strecher VJ. A strategy for optimizing and evaluating behavioral interventions. Ann Behav Med. 2005 Aug;30(1):65–73. doi: 10.1207/s15324796abm3001_8. [DOI] [PubMed] [Google Scholar]
- D’Onofrio G, O’Connor PG, Pantalon MV, et al. Emergency Department-Initiated Buprenorphine/Naloxone Treatment for Opioid Dependence: A Randomized Clinical Trial. JAMA. 2015;313(16):1636–1644. doi: 10.1001/jama.2015.3474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daughters SB, Lejuez CW, Bornovalova MA, et al. Distress tolerance as a predictor of early treatment dropout in a residential substance abuse treatment facility. J Abnorm Psychol. 2005;114:729–734. doi: 10.1037/0021-843X.114.4.729. [DOI] [PubMed] [Google Scholar]
- Epstein DH, Marrone GF, Heishman SJ, et al. Tobacco, cocaine, and heroin: Craving and use during daily life. Addictive Behaviors. 2010;35(4):318–324. doi: 10.1016/j.addbeh.2009.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garland EL, Howard MO. Opioid attentional bias and cue-elicited craving predict future risk of prescription opioid misuse among chronic pain patients. Drug and Alcohol Dependence. 2014;144:283–287. doi: 10.1016/j.drugalcdep.2014.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzales R, Ang A, Murphy DA, et al. Substance use recovery outcomes among a cohort of youth participating in a mobile-based texting aftercare pilot program. Journal of Substance Abuse Treatment. 2014;47(1):20–26. doi: 10.1016/j.jsat.2014.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gossop M, Stewart D, Browne N, et al. Factors associated with abstinence, lapse or relapse to heroin use after residential treatment: protective effect of coping responses. Addiction. 2002 Oct;97(10):1259–67. doi: 10.1046/j.1360-0443.2002.00227.x. [DOI] [PubMed] [Google Scholar]
- Hendershot CS, Witkiewitz K, George WH, et al. Relapse prevention for addictive behaviors. Substance Abuse Treatment, Prevention, and Policy. 2011;6(1):17. doi: 10.1186/1747-597X-6-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Humeniuk R, Ali R, Babor TF, Farrell M, et al. Validation of the Alcohol, Smoking and Substance Involvement Screening Test (ASSIST) Addiction. 2008;103(6):1039–1047. doi: 10.1111/j.1360-0443.2007.02114.x. [DOI] [PubMed] [Google Scholar]
- Kelly PJ, Leung J, Deane FP, et al. Predicting client attendance at further treatment following drug and alcohol detoxification: Theory of Planned Behaviour and Implementation Intentions. Drug Alcohol Rev. 2016;35(6):678–685. doi: 10.1111/dar.12332. [DOI] [PubMed] [Google Scholar]
- Kiluk BD, Nich C, Babuscio T, et al. Quality versus quantity: acquisition of coping skills following computerized cognitive-behavioral therapy for substance use disorders. Addiction. 2010;105(12):2120–2127. doi: 10.1111/j.1360-0443.2010.03076.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krentzman AR. Review of the application of positive psychology to substance use, addiction, and recovery research. Psychol Addict Behav. 2013;27(1):151–65. doi: 10.1037/a0029897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larimer ME, Palmer RS, Marlatt GA. Relapse prevention: An overview of Marlatt’s cognitive-behavioral model. Alcohol Research & Health: The Journal of the National Institute on Alcohol Abuse and Alcoholism. 1992;23(2):151–160. [PMC free article] [PubMed] [Google Scholar]
- Litvin EB, Abrantes AM, Brown RA. Computer and mobile technology-based interventions for substance use disorders: an organizing framework. Addict Behav. 2013 Mar;38(3):1747–56. doi: 10.1016/j.addbeh.2012.09.003. [DOI] [PubMed] [Google Scholar]
- Locke EA, Latham GP. Building a practically useful theory of goal setting and task motivation. A 35-year odyssey. Am Psychol. 2002 Sep;57(9):705–17. doi: 10.1037//0003-066x.57.9.705. [DOI] [PubMed] [Google Scholar]
- Miller WR, Rollnick S. Motivational Interviewing: Helping People Change. 3. New York, NY: The Guilford Press; 2013. [Google Scholar]
- Miller WR, Tonigan JS. Assessing drinkers’ motivation for change: The Stages of Change Readiness and Treatment Eagerness Scale (SOCRATES) Psychology of Addictive Behaviors. 1996;10(2):81–89. [Google Scholar]
- Nahum-Shani I, Smith SN, Spring BJ, et al. Just-in-Time Adaptive Interventions (JITAIs) in Mobile Health: Key Components and Design Principles for Ongoing Health Behavior Support. Ann Behav Med. 2016 Sep 23; doi: 10.1007/s12160-016-9830-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muraven M, Baumeister RF. Self-regulation and depletion of limited resources: does self-control resemble a muscle? Psychol Bull. 2000;126:247–59. doi: 10.1037/0033-2909.126.2.247. [DOI] [PubMed] [Google Scholar]
- Reback CJ, Grant DL, Fletcher JB, Branson CM, Shoptaw S, Bowers JR, Charania M, Mansergh G. Text messaging reduces HIV risk behaviors among methamphetamine-using men who have sex with men. AIDS Behav. 2012 Oct;16(7):1993–2002. doi: 10.1007/s10461-012-0200-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reback CJ, Fletcher JB, Shoptaw S, Mansergh G. Exposure to Theory-Driven Text Messages is Associated with HIV Risk Reduction Among Methamphetamine-Using Men Who have Sex with Men. AIDS Behav. 2015 Jun;19(Suppl 2):130–41. doi: 10.1007/s10461-014-0985-7. [DOI] [PubMed] [Google Scholar]
- Redko C, Rapp RC, Carlson RG. Waiting Time as a Barrier to Treatment Entry: Perceptions of Substance Users. J Drug Issues. 2006 Sep;36(4):831–852. doi: 10.1177/002204260603600404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roth AM, Rossi J, Goldshear JL, et al. Potential Risks of Ecological Momentary Assessment Among Persons Who Inject Drugs. Subst Use Misuse. 2017 Jun 7;52(7):840–847. doi: 10.1080/10826084.2016.1264969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith A. Americans and Text messaging. Pew Research Center; Washington, D.C: 2011. [Accessed November 1, 2016]. http://pewinternet.org/Reports/2011/Cell-Phone-Texting-2011.aspx. [Google Scholar]
- Suffoletto B. Text Message Behavioral Interventions: From Here to Where? Curr Opin Psychol. 2016;9:16–21. doi: 10.1016/j.copsyc.2015.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tofighi B, Grossman E, Sherman S, et al. Mobile Phone Messaging During Unobserved “Home” Induction to Buprenorphine. J Addict Med. 2016;10(5):309–13. doi: 10.1097/ADM.0000000000000198. [DOI] [PubMed] [Google Scholar]
- Tofighi B, Nicholson JM, McNeely J, Muench F, Lee JD. Mobile phone messaging for illicit drug and alcohol dependence: A systematic review of the literature. Drug Alcohol Rev. 2017 Jul;36(4):477–491. doi: 10.1111/dar.12535. [DOI] [PubMed] [Google Scholar]
- Wasan AD, Ross EL, Michna E, et al. Craving of Prescription Opioids in Patients with Chronic Pain: A Longitudinal Outcomes Trial. The Journal of Pain. 2012;13(2):146–154. doi: 10.1016/j.jpain.2011.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Gemert-Pijnen JE, Nijland N, van Limburg M, Ossebaard HC, Kelders SM, Eysenbach G, Seydel ER. A holistic framework to improve the uptake and impact of eHealth technologies. J Med Internet Res. 2011 Dec 5;13(4):e111. doi: 10.2196/jmir.1672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Webb TL, Sniehotta FF, Michie S. Using theories of behaviour change to inform interventions for addictive behaviours. Addiction. 2010 Nov;105(11):1879–92. doi: 10.1111/j.1360-0443.2010.03028.x. [DOI] [PubMed] [Google Scholar]
- Weiss AJ, Barrett ML, Heslin KC, et al. Healthcare Cost and Utilization Project (HCUP) Statistical Briefs [Internet] Rockville (MD): Agency for Healthcare Research and Quality (US); 2006 Feb–2016 Dec. Trends in Emergency Department Visits Involving Mental and Substance Use Disorders, 2006–2013: Statistical Brief #216. [Google Scholar]
- White WL, Kelly JF, Roth JD. New addiction recovery support institutions: mobilizing support beyond professional addiction treatment and recovery mutual aid. J Groups Addict Recover. 2012;7:297–317. [Google Scholar]
- Wickersham JA, Azar MM, Cannon CM, et al. Validation of a Brief Measure of Opioid Dependence: The Rapid Opioid Dependence Screen (RODS) Journal of Correctional Health Care. 2015;21(1):12–26. doi: 10.1177/1078345814557513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winhusen T, Theobald J, Lewis D, et al. Development and initial testing of a tailored telephone intervention delivered by peers to prevent recurring opioid-overdoses (TTIP-PRO) Health Educ Res. 2016 Apr;31(2):146–60. doi: 10.1093/her/cyw010. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.