Abstract
Objective
Gay, bisexual, and other men who have sex with men (MSM) might be particularly likely to migrate to experience freedoms unavailable in their home countries. Structural stigma (e.g., laws and policies promoting the unequal treatment of oppressed populations) in MSM migrants’ sending and receiving countries represent potential barriers to HIV prevention among this intersectional population. This present study represents the first investigation of structural determinants of HIV risk in a large, geographically-diverse sample of MSM migrants.
Design
The 2010 European MSM Internet Survey (EMIS) (n=23,371 migrants) was administered across 38 European countries.
Methods
Structural stigma was assessed using (1) national laws and policies promoting unequal treatment of MSM across 181 countries worldwide and (2) national attitudes against immigrants in the 38 receiving countries. We also assessed linguistic status, time since migrating, and five HIV-prevention outcomes.
Results
Structural stigma toward sexual minorities (in sending and receiving countries) and toward immigrants (in receiving countries) was associated with a lack of HIV-prevention knowledge, service coverage, and precautionary behaviors among MSM migrants. Linguistic status and time since migrating moderated some associations between structural stigma and lack of HIV prevention.
Conclusions
Structural stigma toward MSM and immigrants represents a modifiable structural determinant of the global HIV epidemic.
Keywords: HIV, gay and bisexual, stigma, discrimination, migration
Stigma undermines global HIV-prevention efforts for gay, bisexual, and other men who have sex with men (MSM).1 While stigma occurs on many levels, including the individual and interpersonal, stigma that occurs through discriminatory laws, institutional policies, and cultural norms, otherwise known as structural stigma, has been recently implicated as a risk factor underlying the global HIV epidemic among MSM. This research has shown, for example, that MSM living in more (vs. less) structurally stigmatizing locales experience critical gaps in HIV-prevention service coverage, knowledge, and behavior.2
In geographically mobile populations, exposure to structural stigma varies over the life course. Globally, more people have moved recently than at any point in history.3 Evidence suggests that MSM may be particularly likely to move, whether by choice or duress, to seek social and sexual freedom unavailable in homonegative contexts.4 While scant epidemiologic evidence exists regarding the HIV-prevention needs of MSM migrants, emerging evidence suggests that stigma in MSM migrants’ home contexts, also known as sending contexts, might put them at risk of HIV infection upon arrival.5 However, existing research on stigma and MSM migrants’ HIV-prevention needs is limited by small samples of migrant MSM, lack of variation in structural forms of stigma in both sending and receiving contexts, and reliance on self-reported stigma exposure.6,7
Importantly, as an intersectional population, MSM migrants are potentially affected by two forms of structural stigma in their receiving countries – stigma directed toward sexual minorities and stigma directed toward immigrants. Yet previous research has only examined these influences in isolation, showing that anti-gay structural stigma adversely affects the health of sexual minorities,8 while anti-immigrant stigma adversely affects the health of immigrants.9 It is therefore unknown whether MSM migrants are simultaneously affected by both forms of structural stigma in their receiving countries.
To advance this literature on structural stigma, migration, and sexual health in MSM, we tested six hypotheses predicting lack of HIV-prevention (i.e., HIV-prevention service coverage, HIV-transmission knowledge, and precautionary behaviors, such as condom use):
First, given that stigma can impede equitable access of at-risk populations to health-promoting resources,10 anti-gay and anti-immigrant structural stigma in MSM’s receiving countries will each be associated with lower odds of HIV prevention.
Second, operating as intersectional influences on MSM migrants’ health,11 anti-gay and anti-immigrant structural stigma in MSM’s receiving countries will interact such that migrants living in anti-gay and anti-immigrant receiving countries will experience the lowest odds of adequate HIV prevention.
Third, higher, compared to lower, levels of anti-gay structural stigma in MSM’s sending countries will be associated with lower odds of HIV prevention, consistent with life-course-persistent effects of early exposure to adverse environments on later health-risk behavior.12,13
Fourth, anti-gay structural stigma in sending and receiving countries will interact such that MSM migrants from gay-supportive, compared to anti-gay, countries will experience lower odds of incorrect HIV-prevention knowledge and precautionary behaviors even in anti-gay receiving countries, consistent with the possibility that knowledge and behavioral patterns are transferable across contexts once instilled;14 this protective effect will not extend to HIV-prevention service coverage, which is context dependent.
Fifth, anti-immigrant structural stigma in MSM migrants’ receiving countries will interact with migrants’ language status to predict their HIV risk, such that HIV risk will be greatest for linguistic minority migrants who live in anti-immigrant countries given their potentially greater exposure to acculturative stress.15
Sixth, consistent with a “healthy migrant” effect,16 recently-arrived migrants will be more likely to report HIV prevention than those who arrived more distantly. Further, duration of residence in receiving countries will interact with those countries’ anti-gay and anti-immigrant structural stigma to predict migrants’ HIV risk. Specifically, the longer that MSM migrants have lived in countries with high anti-gay and anti-immigrant structural stigma, the more likely that their HIV-prevention outcomes will be compromised, consistent with life-course accumulating effects observed for long-term exposure to other forms of social disadvantage.12,17
Answering these questions requires a unique data structure, including a large number of MSM migrants, wide variation in structural stigma in respondents’ sending and receiving contexts, and linkage to measures of structural stigma related to sexual orientation and immigration. Until recently, a data structure did not exist that met these criteria. The European MSM Internet Survey (EMIS) represents the largest-known dataset of MSM, over 23,000 of whom report migrating from 181 countries to the 38 countries of Europe included in EMIS. EMIS respondents therefore have moved from both countries with high and low anti-gay structural stigma to countries with high- and low- anti-gay and anti-immigrant structural stigma. Further, EMIS responses can be linked with a recently created objective index of anti-gay structural stigma in all world countries,18 thereby bypassing previous studies’ reliance on MSM’s self-reported exposure to structural stigma.5 This dataset therefore provides an unprecedented opportunity to examine our research questions.
Method
Participants
The EMIS was administered in 25 languages between June and August 2010 across 38 European countries. The EMIS represented a joint effort of five Associated Partners; dozens of European-wide government health institutes, academic programs, and NGOs; and two major online media partners. Participants were recruited online from over 235 local, national, and international sexual minority websites through instant messages or banner advertising and offline through posters, cards, and face-to-face communication. Eligibility criteria included: male identification, European residence, at or above the age of homosexual consent in the country of residence, and sexual attraction to and/or sexual experiences with men. Eligible respondents had to indicate understanding the study’s purpose and provide consent. Survey completion required an average of 21 minutes; no material remuneration was offered. Items were generated through consultation with NGOs, pilot testing with MSM with feedback from 21 countries for comprehension, and cognitive interviewing to ensure accurate interpretation.19,20
The survey received 184,469 submissions. Three cases were lost to data corruption. Cases were removed for respondents not specifying a current country or indicating residing outside of the study catchment area (n=2,427); being from a country that did not reach 100 qualifying cases (n=291); indicating being women, having no same-sex attraction or experience, or providing no age or being outside the 13–89-year age range (n=544); or submitting more than one inconsistent response (n=6,995). These exclusions produced a dataset containing 174,209 respondents.19 Given our interest in MSM migrants, we restricted all analyses to the 13.4% of respondents (n=23,371) who indicated currently living in a country other than their birth country.
Measures
Explanatory variables
Respondents indicated the country in which they were born (sending country) and the country in which they currently lived (receiving country). We characterized sending and receiving countries’ anti-gay structural stigma as each country’s national legislation toward sexual minorities derived from the International Lesbian, Gay, Bisexual, Trans, and Intersex Association’s (ILGA) Rainbow Map.18 This 9-item scale reflects the criminalization, protection, and recognition of same-sex individuals as follows: 9 (country prescribes the death penalty for same-sex sexual acts), 8 (country imprisons sexual minorities for same-sex sexual acts from 14 years to life), 7 (country imprisons sexual minorities for same-sex sexual acts for up to 14 years), 6 (country contains laws against the promotion of homosexuality, but no criminalization of same-sex sexual acts), 5 (country contains criminalizing laws without a specific penalty), 4 (country does not contain any criminalizing laws, but also does not recognize same –sex marriage), 3 (country contains a clearly inferior substitute to marriage), 2 (country recognizes same-sex domestic partnerships), 1 (country recognizes same-sex marriage). While structural stigma is typically defined as “societal-level conditions, cultural norms, and institutional policies that constrain the opportunities, resources, and well-being of the stigmatized,”21 data regarding cultural norms toward sexual minorities were unavailable for the 181 countries, thereby limiting our operationalization of structural stigma to the national legislation contained in the ILGA index. The strong correlation (r = 0.85) between this index and attitudes toward sexual minorities in the 2008 European Values Survey (EVS), a survey of social attitudes that randomly sampled approximately 1,500 residents per European country, supports the validity of our index.
We derived receiving countries’ anti-immigrant structural stigma from the 2008 wave of the EVS. We calculated each country’s average response for five immigrant-related questions on the EVS concerning immigrants and crime, jobs, financial strain, national threat, and cultural erosion (α =0.88). Our indices of receiving countries’ anti-gay and anti-immigrant structural stigma were weakly correlated (r=0.30, p=0.07), as were sending and receiving countries’ anti-gay stigma (r=0.18, p<0.001), indicating a lack of multicollinearity.
Respondents indicated the number of years that they had been living in their current country (range = 1–71). Linguistic minority status was assessed according to whether respondents opted to complete the survey in a language other than one of the official languages of their current country (yes/no).
Outcome variables
We assessed five HIV-prevention outcomes (i.e., HIV-prevention service coverage, HIV-transmission knowledge, and precautionary behaviors, including condom use) largely based on recommendations of the United Nations’ General Assembly Special Session (UNGASS) on HIV/AIDS (Joint United Nations Programme on HIV/AIDS, 2009) and the European Centre for Disease Control (ECDC, 2009):20 (1) EMIS-modified UNGASS indicator #9: Participants were classified as being inadequately reached by HIV-prevention services if, in the last 12 months, they were not confident they could access HIV testing (if not diagnosed HIV-positive) or reported not having visited a provider for HIV monitoring (if diagnosed HIV-positive), reported condomless anal sex due to lack of condom access, or reported not seeing or hearing MSM-specific information about HIV or STIs; (2) EMIS-modified UNGASS indicator #14: To assess HIV knowledge, respondents were presented with five true statements about HIV and for each were asked whether they already knew this. Although this approach likely underestimates ignorance, it avoids providing falsehoods while serving an educational purpose. Lack of HIV-risk knowledge was classified as not knowing all of the five items; (3) UNGASS indicator #8: Having received an HIV test in the previous 12 months was measured by asking tested-negative respondents when they had last received a negative HIV test result, and tested-positive respondents if they were first diagnosed within the last 12 months; (4) Participants who reported having had anal sex with a non-steady male partner within the previous 12 months were asked about frequency of condom use (not at all or seldom versus sometimes, mostly, or always); and (5) Participants were asked, “The last time you tested for HIV, did you talk about the sex you have with men?” to assess comfort and perceptions of safety in discussing same-sex sexual behaviors as part of testing (yes/no). The EMIS was conducted before European approval of HIV pre-exposure prophylaxis.
Covariates
Individual-level covariates included self-reported age, relationship status, employment status, educational attainment, settlement size (i.e., size of one’s city, town, or village), and HIV status. To control for the possibility that general structural inequality rather than inequality specific to sexual minorities or immigrants was responsible for associations between structural stigma and HIV-related outcomes, we controlled for each sending and receiving countries’ Gini coefficient, an index of income inequality. To control for the possibility that European-wide norms or attitudes toward sexual minorities or HIV prevention might be responsible for associations between sending country structural stigma and HIV-related outcomes, we also controlled for whether respondents migrated from Europe versus another continent.
Analytic Strategy
For each outcome, we specified a two-level cross-classified model to reflect the fact that respondents belonged to two hierarchical contexts (i.e., sending and receiving countries) that were not nested within each other. All outcomes were treated as dichotomous and estimated using a Bernoulli distribution. Respondents (i) simultaneously belonged to receiving countries (j) and sending countries (k). Thus, in the following equations, outcome is the log of the odds of an outcome’s occurrence for respondent i cross-classified in receiving country j and sending country k. The subscripts (jk) represent each sending and receiving country combination. is the overall model intercept. The model allows the intercept to vary independently across receiving and sending countries. At level 2, this intercept is modeled as a product of the level 2 intercept plus separate group-level error variances for receiving and sending countries. For simplicity, the below equations present a model containing only one covariate at level 1, two level 2 predictors, and no cross-hierarchy or cross-level effects:
- Level 1
- Level 2
Fixed effects were estimated for each explanatory variable by means of full information maximum likelihood using SPSS version 24. Individual-level factors (e.g., demographics) were modeled at Level 1; receiving country (e.g., anti-gay and anti-immigrant structural stigma) and sending country factors (e.g., anti-gay structural stigma) were modeled at Level 2. We estimated cross-hierarchy (e.g., anti-gay structural stigma in sending * receiving countries) and cross-level (e.g., structural stigma * linguistic status) effects as relevant for each hypothesis.
Sample size for each model depended on the amount of missing data for that model and the relevance of each outcome to each respondent (e.g., according to past-12-month intercourse, HIV testing history). Missing data for explanatory variables and covariates ranged from 0 (0.0%) for age to 565 (2.4%) for settlement size. Missing data for outcomes ranged from 39 (0.2%) for HIV service reach and HIV transmission knowledge to 281 (1.9%) for past-12-month condom use with non-steady partners. Gini coefficients were unavailable for 10 small sending countries, thereby removing an additional 163 participants. We used complete case analysis.
We created six models. In the first model, we simultaneously estimated main effects for the five explanatory variables predicting the five HIV-prevention outcomes controlling for covariates at each level. Subsequent models separately estimated each of our hypothesized interactions, controlling for all explanatory variables and covariates at each level.
Results
Table 1 shows descriptive statistics of the full sample. MSM migrants were born in 181 global countries. The majority (56.5%) of respondents were born in Europe; 13.8% were born in Asia; and 10.8% were born in South America. The most frequently represented sending countries were Germany (8.9%), Brazil (5.1%), and the United States (5.0%). The most frequently represented receiving countries were the United Kingdom (20.4%), Germany (18.9%), and Spain (12.3%).
Table 1.
Characteristics of Study Respondents in the European MSM Internet Survey (N = 23,371)a
| Demographic Characteristics | n | % |
|---|---|---|
| Relationship status | ||
| Single | 10,830 | 46.3 |
| Steady relationship | 12,494 | 53.5 |
| Employment status | ||
| Employed/student/retired/sick leave | 21,922 | 93.8 |
| Unemployed | 1,449 | 6.2 |
| Education (ISCED levels b) | ||
| Low (ISCED 1,2) | 1,299 | 5.6 |
| Mid (ISCED 3,4) | 6,511 | 27.9 |
| High (ISCED 5,6) | 15,400 | 65.9 |
| Settlement Size | ||
| ≥ 1 million | 10,304 | 44.1 |
| 500,000–999,999 | 3,593 | 15.4 |
| 100,000–499,999 | 4,416 | 18.9 |
| 10,000–99,999 | 2,868 | 12.3 |
| <10,000 | 1,623 | 6.9 |
| HIV diagnosis | ||
| Diagnosed positive | 2,324 | 9.9 |
| Last test negative or untested | 20,910 | 89.5 |
| WHO Region of sending countryc | ||
| Africa (excl. Algeria) | 974 | 4.2 |
| Americas: Canada, USA | 1,411 | 6.0 |
| Americas: Latin America & Caribbean | 3,806 | 16.3 |
| Eastern Mediterranean (incl. Algeria) | 597 | 2.6 |
| Europe | 15,129 | 64.7 |
| South-East Asia | 412 | 1.8 |
| Western Pacific: Australia and NZ | 425 | 1.8 |
| Western Pacific: all other countries | 617 | 2.6 |
| Linguistic Status | ||
| Majority | 14,636 | 62.6 |
| Minority | 8,657 | 37.0 |
|
|
||
| Mean | SD | |
|
|
||
| Age | 34.55 | 10.59 |
| Median = 33 | ||
| Length of receiving country residence | 12.77 | 11.56 |
| Median = 9 | ||
Percentages may not equal 100 due to missing data.
ISCED: 1997 International Standardized Classification of Educational Degrees.
World Health Organization
Hypothesis 1: Anti-gay and anti-immigrant structural stigma in receiving countries will be associated with MSM migrants’ HIV risk
Consistent with the hypothesis, anti-gay structural stigma in receiving countries was associated with higher odds of inadequate HIV-prevention coverage, lack of condom use with non-steady partners in the past 12 months, and lack of disclosure of sexuality during HIV testing (Table 2, Model 1). Anti-immigrant structural stigma in receiving countries was associated with higher odds of lack of past-12-month condom use. However, anti-immigrant stigma was associated with lower odds of inadequate HIV-prevention coverage and lack of disclosure of sexuality during HIV testing. We find that the direction, magnitude, and significance of effects for each structural stigma variable remain the same when examined independently and when controlling for the other structural stigma variable.
Table 2.
Odds of HIV-Prevention Service Coverage, Knowledge, and Behavior by Anti-gay and Anti-Immigrant Structural Stigma in Sending and Receiving Countries among MSM Migrants in Europea, b
| Inadequate HIV service coverage
|
Lack of HIV transmission knowledge
|
No HIV test result (12 mo.)
|
Condoms never/seldom (non-steady 12-mo. partners)
|
No disclosure of sexuality when testing
|
||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
n = 22,270
|
n = 22,263
|
n = 20,651
|
n = 14,284
|
n = 17,687
|
||||||
| aOR | 95% CI | aOR | 95% CI | aOR | 95% CI | aOR | 95% CI | aOR | 95% CI | |
| Model 1 | ||||||||||
|
| ||||||||||
| Anti-gay stigma (receiving country) | 1.19*** | 1.14, 1.24 | 1.02 | .98, 1.06 | 1.02 | .98, 1.06 | 1.19*** | 1.10, 1.28 | 1.42*** | 1.35, 1.49 |
| Anti-immigrant stigma (receiving country) | .84*** | .78, .90 | .99 | .93, 1.05 | 1.06 | .99, 1.12 | 1.26*** | 1.12, 1.43 | .72*** | .67, .78 |
| Anti-gay stigma (sending country) | 1.06*** | 1.03, 1.08 | 1.06*** | 1.04, 1.08 | 1.01 | .99, 1.03 | 1.01 | .97, 1.05 | 1.06** | 1.03, 1.08 |
| Linguistic minority | 1.11* | 1.02, 1.20 | 1.12** | 1.04, 1.20 | 1.19*** | 1.11, 1.28 | .98 | .84, 1.15 | 1.23*** | 1.13, 1.35 |
| Duration of residence (receiving country) | 1.00 | 1.00, 1.01 | 1.004* | 1.001,1.007 | 1.01*** | 1.01, 1.02 | 1.01 | 1.00, 1.01 | 1.00 | 1.00, 1.01 |
|
| ||||||||||
| Model 2c | ||||||||||
|
| ||||||||||
| Anti-immigrant stigma (receiving country) * Anti-gay stigma (receiving country) | 1.06 | .99, 1.13 | 1.03 | .97, 1.10 | .92** | .87, .98 | .92 | .80, 1.05 | 1.18*** | 1.09, 1.28 |
|
| ||||||||||
| Model 3c | ||||||||||
|
| ||||||||||
| Anti-gay stigma (receiving country) * Anti-gay stigma (sending country) | 1.00 | .99, 1.02 | 1.00 | .98, 1.02 | .99 | .97, 1.01 | 1.04** | 1.01, 1.08 | 1.03* | 1.004, 1.05 |
|
| ||||||||||
| Model 4c | ||||||||||
|
| ||||||||||
| Anti-immigrant stigma (receiving country) * Linguistic minority | 1.31*** | 1.17,1.48 | .94 | .85, 1.04 | .90 | .81, 1.00 | .70*** | .56, .87 | 1.45*** | 1.29, 1.64 |
|
| ||||||||||
| Model 5c | ||||||||||
|
| ||||||||||
| Duration of residence * Anti-gay stigma (receiving country) | 1.00 | 1.00, 1.00 | 1.002 | 1.00, 1.01 | 1.003* | 1.001, 1.01 | 1.00 | .99, 1.00 | 1.004 | 1.00, 1.01 |
|
| ||||||||||
| Model 6c | ||||||||||
|
| ||||||||||
| Duration of residence * Anti-immigrant stigma (receiving country) | 1.00 | 1.00, 1.01 | 1.01* | 1.001, 1.01 | 1.005* | 1.001, 1.01 | 1.01 | 1.00, 1.01 | 1.00 | .99, 1.00 |
p ≤ .05,
p ≤ .01,
p ≤ .001;
All models adjusted for age, relationship status, employment status, education, settlement size, HIV status, Gini index of sending and receiving country.
All continuous predictors were grand-mean centered; binary predictors were scored 0/1.
Models 2–6 also adjusted for all Model 1 predictors.
Hypothesis 2: Anti-immigrant structural stigma in receiving countries will exacerbate the association between anti-gay structural stigma and HIV outcomes in those countries
The hypothesis was supported for lack of sexuality disclosure during HIV testing (Table 2, Model 2; Figure 1). The association between anti-gay structural stigma in receiving countries and odds of lack of sexuality disclosure during testing was significantly stronger for MSM migrants who lived in anti-immigrant receiving countries compared to those who lived in immigrant-supportive countries. However, only in immigrant-supportive receiving countries was anti-gay stigma associated with reduced odds of HIV testing (Figure 1).
Figure 1.
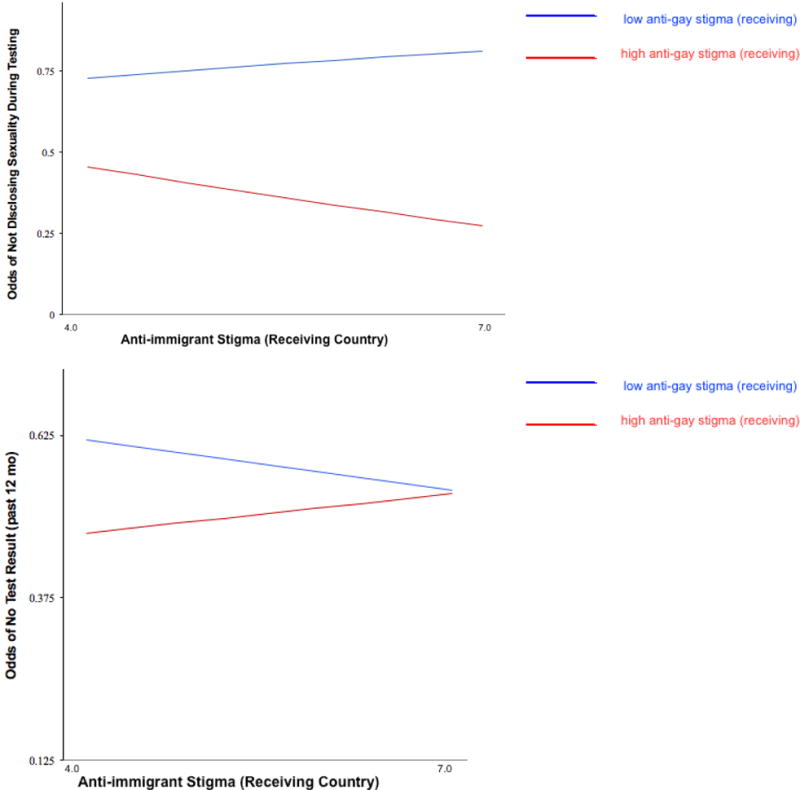
Interaction between anti-gay stigma and anti-immigrant stigma in MSM migrants’ receiving countries predicts lack of sexuality disclosure during HIV testing and lack of HIV testing (past 12 months).
Note. Low and high levels of receiving country structural stigma are displayed at the 25% and 75% percentile, respectively, of the structural stigma distribution.
Hypothesis 3: Anti-gay stigma in sending countries will be associated with MSM migrants’ higher odds of lacking HIV-prevention service coverage, knowledge, and behavior
Anti-gay stigma in MSM migrants’ sending countries was associated with greater odds of inadequate HIV-prevention coverage, lack of HIV transmission knowledge, and lack of disclosure of sexuality during HIV testing, supporting the hypothesis (Table 2, Model 1).
Hypothesis 4: MSM migrants from low-structural stigma sending countries will report HIV-prevention knowledge and behaviors regardless of anti-gay structural stigma in their receiving countries; this benefit will not extend to HIV-prevention service coverage
his hypothesis was supported for lack of condom use and lack of sexuality disclosure during testing (Table 2, Model 3). Specifically, we found a weaker association between receiving countries’ anti-gay structural stigma and these outcomes for MSM migrants from gay-supportive, compared to anti-gay, sending countries (Figure 2). This protective association did not extend to HIV-prevention coverage and HIV testing.
Figure 2.
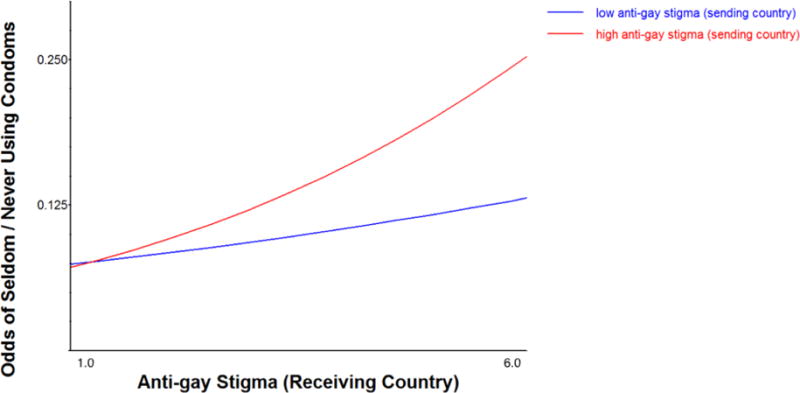
Weaker association between receiving countries’ anti-gay stigma and lack of condom use (past 12 months) for MSM migrants from gay-supportive, compared to anti-gay, sending countries.
Note. Low and high levels of sending country structural stigma are displayed at the 25% and 75% percentile, respectively, of the structural stigma distribution.
Hypothesis 5: Associations between anti-immigrant structural stigma and HIV risk will be stronger for linguistic minority (vs. majority) MSM migrants
This hypothesis was supported for inadequate HIV-prevention coverage and lack of sexuality disclosure during HIV testing (Table 2, Model 4). Namely, speaking a minority language in one’s receiving country strengthened odds of these HIV-risk outcomes (Figure 3). The slope of the association between anti-immigrant structural stigma and inadequate HIV-prevention coverage for linguistic minorities was not significant (b=−0.03 [SE=0.05], p=0.55); in contrast, for linguistic majorities, the slope was negative and significant (b=−0.30, [SE=0.04], p<0.01). For lack of sexuality disclosure during testing, the slope was significant and negative for both linguistic minorities and majorities, although weaker for linguistic minorities, b=−0.12 [SE=0.04], p<0.01, versus b=−0.48, [SE=0.05], p<0.01, respectively. Contrary to hypotheses, linguistic minorities were protected against lack of condom usage in high (vs. low) anti-immigrant receiving countries (Figure 3). For lack of condom usage, the slope for linguistic minorities was not significant (b=0.04 [SE=0.07], p=0.59) whereas the slope for linguistic majorities was significant (b=0.40, [SE=0.08], p<0.01).
Figure 3.
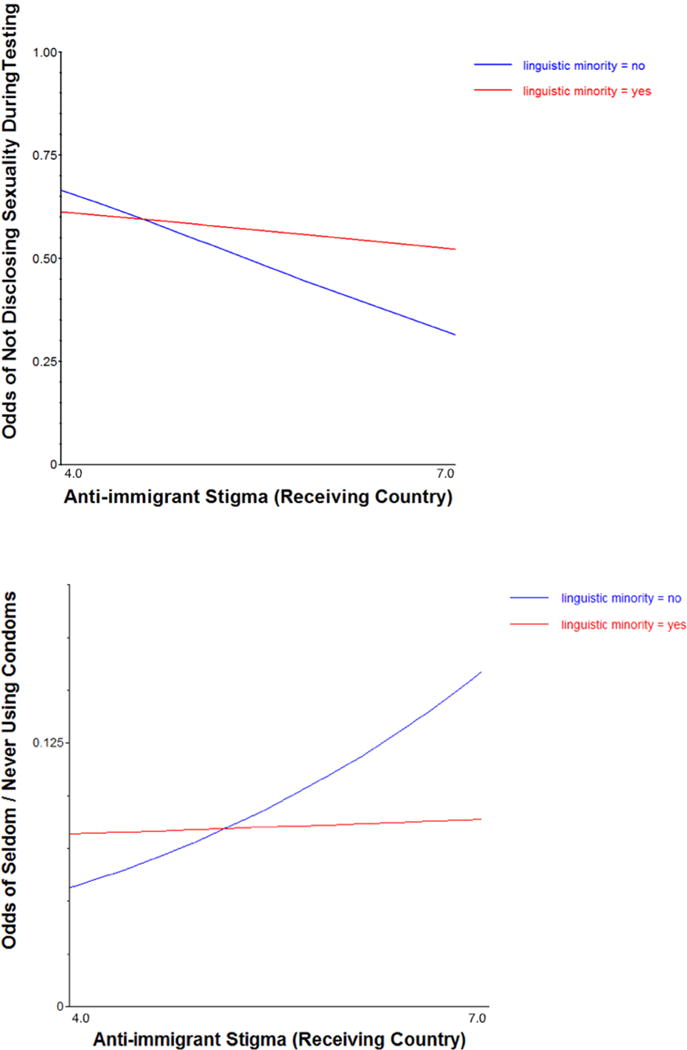
Association between anti-immigrant structural stigma and odds of not disclosing sexuality during testing and lack of condom usage as moderated by linguistic status.
Hypothesis 6: Length of residence in receiving countries with higher levels of anti-gay and anti-immigrant structural stigma will be associated with greater odds of lacking HIV-prevention service coverage, knowledge, and behavior
Length of receiving country residence was positively associated with both lack of HIV-transmission knowledge, especially in receiving countries with high anti-immigrant structural stigma (Table 2, Models 1 and 5), and lack of recent HIV testing, especially in receiving countries with high anti-immigrant and anti-gay structural stigma (Table 2, Models 1, 5, and 6; Figure 4).
Figure 4.
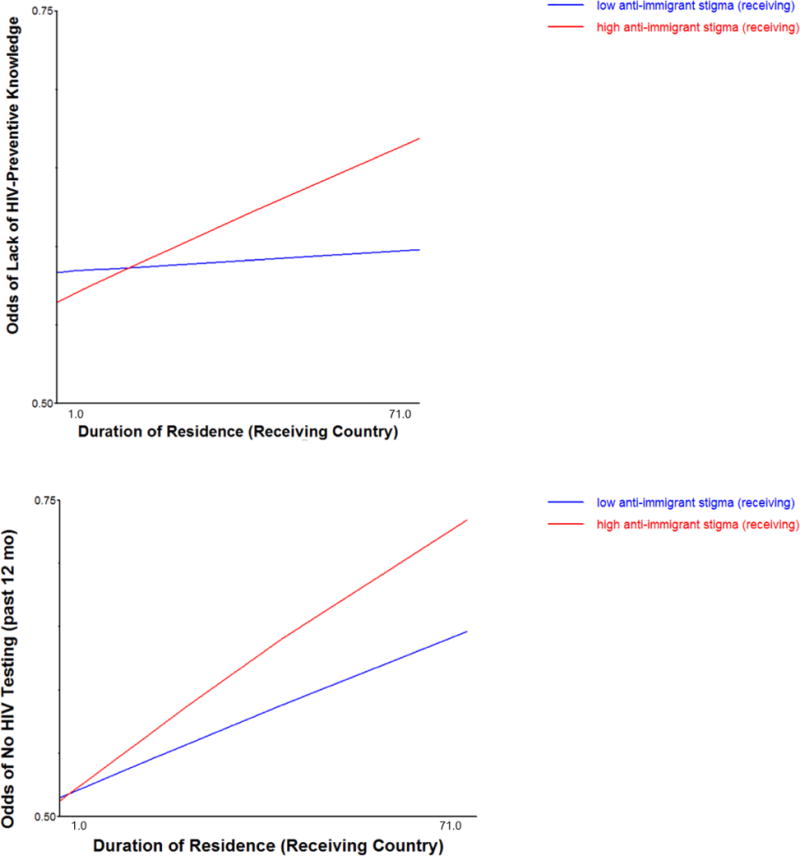
Length of receiving country residence is positively associated with lack of HIV-transmission knowledge and recent HIV testing, especially in receiving countries with high anti-immigrant stigma.
Note. Low and high levels of receiving country structural stigma are displayed at the 25% and 75% percentile, respectively, of the structural stigma distribution.
Discussion
This study examines structural correlates of HIV prevention in a large sample of MSM migrants. Results largely support our hypotheses that structural stigma toward sexual minorities and immigrants would be associated with MSM migrants’ lack of HIV-prevention service coverage, HIV-transmission knowledge, and precautionary behaviors. This study is also the first to our knowledge to find that anti-gay structural stigma in migrants’ sending countries might continue to impact MSM migrants’ HIV prevention upon arrival in a new country. While anti-immigrant structural stigma was unexpectedly associated with greater HIV-prevention service coverage and testing-related sexuality disclosure, this protective association was largely limited to migrants who spoke the language of their receiving country, perhaps suggesting that these migrants were viewed as citizens and therefore less exposed to immigration-related stigma. Newly-arrived MSM migrants displayed greater HIV-prevention knowledge and behaviors than those who had lived in the country longer, especially in anti-gay and anti-immigrant receiving countries.
These results help build a structural theory of MSM migrant health risk informed by research on life-course determinants of health,12 migrant acculturation,15 intersectionality,11 and structural stigma.21 In an increasingly mobile global population, life-course exposure to structural stigma is not a static phenomenon. Extending life-course research on early adverse structural exposures and ill health,12 this study demonstrates that prior exposure to structural stigma might continue to adversely influence health in new national contexts. We also find evidence suggesting that the greater length of exposure to structurally stigmatizing receiving environments might undermine MSM migrants’ HIV-prevention knowledge and precautionary behaviors, paralleling previous findings on the impact of length of exposure to new national contexts on other health-risk outcomes among other migrant populations.22 These intriguing findings require replication using longitudinal designs. Our findings are also the first, to our knowledge, to reflect the fact that distinct forms of structural stigma might simultaneously impact intersectional populations, in this case, individuals who are both sexual minorities and immigrants. In so doing, we extend intersectionality research by measuring and statistically modeling structural sources of inequality that affect individuals with intersectional identities (rather than examining interactions between demographic characteristics associated with these groups, as characterizes most prior work).11
Results largely suggest that exposure to structural stigma might interfere with HIV prevention, especially when exposures are longer in duration and more directly experienced, as measured by linguistic minority status. However, a few significant associations involving linguistic status and anti-immigrant structural stigma contradicted hypotheses, with implications for understanding the relevance of MSM migrants’ acculturation for HIV prevention. For instance, our finding that linguistic minority migrants, compared to linguistic majority migrants, were more likely to use condoms in anti-immigrant contexts contradicts previous research showing only adverse health correlates of structural stigma.8 Perhaps MSM migrants in anti-immigrant contexts also perceive less familiarity between themselves and their new local MSM peers, thereby driving protective behaviors.23 Similarly, perhaps the sex partners of linguistic minority migrants in anti-immigrant countries are more insistent on condom usage, as a function of anti-immigrant beliefs that associate migrants with risk. The unexpected protective role of anti-immigrant structural stigma against lack of HIV prevention coverage and sexuality disclosure during testing was largely limited to linguistic majorities, suggesting that prevention knowledge acquisition and comfort with healthcare providers might only extend to those who are most fluent in their receiving country’s language, perhaps an indicator of acculturation.24
While this study has several notable strengths (e.g., diverse sample of MSM migrants from 181 countries, objective measures of structural stigma), study results should be considered against several limitations. First, the EMIS did not assess important features of migration, including reasons for migrating, degree of connection with one’s sending country, religiosity, and the process of adaptation, all of which are important to a comprehensive understanding of migrant health.3,25,26 Further, the mechanisms linking structural stigma to MSM’s HIV risks remain largely unknown, although emerging research suggests MSM living in more homonegative countries report more sexual orientation concealment, which predicts some HIV-related risks.2 Future research might explore additional mechanisms linking early and current structural stigma to HIV-prevention outcomes, including learned behavioral responses to stress, lack of access to HIV-prevention knowledge during sensitive developmental stages, and perceptions of stigma in healthcare and other more proximal institutions.12
Second, due to data availability, we were limited to an index of current legislation affecting sexual minorities (coded in 2016) as our main sending-country predictor, which in some instances may not have precisely reflected previous levels of structural stigma in that country. However, this decision is supported by evidence that other forms of structural stigma remain relatively stable over time and that countries’ relative positions on our index are unlikely to have shifted substantially.27 Third, we used a measure of anti-immigrant attitudes to capture structural variation in anti-immigrant stigma across receiving countries, whereas we used legislation to represent anti-gay structural stigma, because population-based studies of attitudes toward sexual minorities do not exist for all countries. However, the fact that anti-gay legislation in Europe is strongly correlated with anti-gay attitudes in those countries2 strengthens the validity of our measurement approach. Fourth, because we only examined national forms of structural stigma, future research should consider the role of local laws that might reinforce or protect against structural stigma at the country level. Finally, while half (50%) of the examined associations were significant, when using a more conservative correction for multiple analyses (i.e., p < .001), this proportion is reduced to 30%. Yet, given that structural stigma operates at the population level with wide reach, even weak associations can be argued to be important for population health.
The results of this study suggest that structural forms of stigma toward sexual minorities and immigrants may be important risk factors for adverse HIV outcomes among MSM migrants. While HIV-prevention behavioral interventions have demonstrated modest efficacy,28 findings of the present study also call for developing and evaluating interventions that address structural drivers of the HIV epidemic in order to maximize equitable intervention coverage and efficacy.29 MSM migrants in unwelcoming societies might be particularly vulnerable to structural disadvantage given that they may not possess the political, social, or economic status necessary to access health-promoting resources and affect societal change.30 However, by modifying the structural contexts surrounding MSM migrants through legislation (e.g., enacting laws that recognize the equality of sexual minorities; enacting legal protections against discrimination based on sexual orientation or immigrant status), countries may ensure more equitable access to health-promotion interventions among MSM migrants. Given that these structural changes can be protracted, these findings suggest that in the meantime, recent migration, especially to and from stigmatizing countries, represents an important window of opportunity during which local public health authorities can deliver HIV prevention resources to curb the spread of the HIV epidemic in the increasingly mobile global population.
Acknowledgments
We begin by thanking all of the men who took part in EMIS 2010. We also thank the more than 235 websites who placed the EMIS banner, and particularly to those who sent individual messages to their users: PlanetRomeo, Manhunt, Qruiser, Qguys, and Gaydar. We also thank all NGOs who promoted the survey. This research was made possible by The EMIS Network. EMIS Associated Partners: DE: GTZ, Robert Koch Institute; ES: Centre de Estudis Epidemiològics sobre les ITS i SIDA de Catalunya (CEEISCat); IT: Regional Centre for Health Promotion Veneto; NL: University College Maastricht; UK: Sigma Research, London School of Hygiene & Tropical Medicine. EMIS Collaborating Partners: AT: Aids-Hilfe Wien; BE: Institute of Tropical Medicine, Facultés Universitaires Saint-Louis, Ex Aequo, Sensoa, Arc-en-ciel Wallonie; BG: National Centre of Infectious and Parasitic Diseases, Queer Bulgaria Foundation; BY: Vstrecha; CH: Institut universitaire de medicine sociale et préventive, Aids-Hilfe Schweiz; CY: Research Unit in Behaviour & Social Issues; CZ: Charles University (Institute of Sexology), Ceska spolecnost AIDS pomoc; DE: Berlin Social Science Research Center (WZB), Deutsche AIDS-Hilfe; Federal Centre for Health Education (BZgA); DK: Statens Serum Institut, Department of Epidemiology, STOP AIDS; ES: National Centre of Epidemiology, STOP SIDA, Ministry of Health, Social Policy and Equality; EE: National Institute for Health Development; FI: University of Tampere (Nursing Science), HIV-saatio/Aids-tukikeskus; FR: Institut de veille sanitaire (InVS), AIDeS, Act Up Paris, Sida Info Service, Le Kiosque, The Warning; GR: Positive Voice; HR: University of Zagreb (Humanities and Social Sciences); HU: Hungarian Civil Liberties Union (TASZ), Háttér; IE: Gay Men’s Health Service, Health Services Executive; IT: University of Bologna, Arcigay, Instituto Superiore di Sanità; LT: Center for Communicable Diseases and AIDS; LV: The Infectiology Center of Latvia; Mozaika; MD: GenderDoc-M; MK: Equality for Gays and Lesbians (EGAL); NL: schorer; NO: Norwegian Knowledge Centre for the Health Services, Norwegian Institute of Public Health; PL: National AIDS Centre, Lambda Warszawa; PT: GAT Portugal, University of Porto (Medical School), Institute of Hygiene and Tropical Medicine; RO: PSI Romania RS: Safe Pulse of Youth; RU: PSI Russia, LaSky; SE: Malmö University, Riksforbundet for homosexuellas, bisexuellas och transpersoners rattigheter (RFSL); SI: National Institute of Public Health, Legebitra, ŠKUC-Magnus, DIH; SK: OZ Odyseus; TR: Turkish Public Health Association, KAOS-GL, Istanbul LGBTT, Siyah Pembe Ucgen Izmir; UA: Gay Alliance, Nash Mir, LiGA Nikolaev; UK: City University, London, CHAPS (Terrence Higgins Trust); EU: ILGA-Europe, Aids Action Europe, European AIDS Treatment Group, PlanetRomeo, Manhunt & Manhunt Cares. EMIS Advisory Partners: Executive Agency for Health and Consumers (EAHC), European Centre for Disease Prevention and Control (ECDC), WHO-Europe.
Funding
EMIS was funded by grants from the Executive Agency for Health and Consumers (EU Health Programme 2008–2013); Centre d’Estudis Epidemiológics sobre les ITS HIV/SIDA de Catalunya (CEEISCat); Terrence Higgins Trust for the CHAPS partnership; Regione de Veneto; Robert Koch Institute; Maastricht University; German Ministry of Health; Finnish Ministry of Health; Norwegian Institute of Public Health; Swedish Board of Health and Welfare; and, for Dr. Hatzenbuehler’s contribution, the National Institute on Drug Abuse (K01DA032558).
Footnotes
Conflicts of interest
The authors declare that they have no conflicts of interests.
Authors’ contributions
The survey was designed and executed by AJS, UM, and PW in association with The EMIS Network (see Acknowledgements). AJS coordinated the study, PW coordinated the survey promotion, UM initiated the study. Data were prepared and coded by AJS. JP and MH designed the analysis. JP conducted the statistical analyses. The manuscript was drafted by JP and MH and co-authored by all other authors. All authors approved the final manuscript.
References
- 1.Beyrer C, Baral SD, van Griensven F, et al. Global epidemiology of HIV infection in men who have sex with men. Lancet. 2012;380(9839):367–377. doi: 10.1016/S0140-6736(12)60821-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pachankis JE, Hatzenbuehler ML, Hickson F, et al. Hidden from health: structural stigma, sexual orientation concealment, and HIV across 38 countries in the European MSM Internet Survey. Aids. 2015;29(10):1239–1246. doi: 10.1097/QAD.0000000000000724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization. Health of migrants: The way forward - Report of a global consultation, Madrid, Spain. Geneva: World Health Organization; Mar 3–5, 2010. 2010. [Google Scholar]
- 4.Bruce D, Harper GW, Adolescent Medicine Trials Network for HIVAI Operating without a safety net: gay male adolescents and emerging adults’ experiences of marginalization and migration, and implications for theory of syndemic production of health disparities. Health Educ Behav. 2011;38(4):367–378. doi: 10.1177/1090198110375911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pachankis JE, Eldahan AI, Golub SA. New to New York: Ecological and Psychological Predictors of Health Among Recently Arrived Young Adult Gay and Bisexual Urban Migrants. Ann Behav Med. 2016;50(5):692–703. doi: 10.1007/s12160-016-9794-8. [DOI] [PubMed] [Google Scholar]
- 6.Lewis NM, Wilson K. HIV risk behaviours among immigrant and ethnic minority gay and bisexual men in North American and Europe: A systematic review. Soc Sci Med. 2017;179:115–128. doi: 10.1016/j.socscimed.2017.02.033. [DOI] [PubMed] [Google Scholar]
- 7.Blondell SJ, Kitter B, Griffin MP, Durham J. Barriers and Facilitators to HIV Testing in Migrants in High-Income Countries: A Systematic Review. Aids Behav. 2015;19(11):2012–2024. doi: 10.1007/s10461-015-1095-x. [DOI] [PubMed] [Google Scholar]
- 8.Hatzenbuehler ML, McLaughlin KA, Keyes KM, Hasin DS. The Impact of Institutional Discrimination on Psychiatric Disorders in Lesbian, Gay, and Bisexual Populations: A Prospective Study. Am J Public Health. 2010;100(3):452–459. doi: 10.2105/AJPH.2009.168815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Salas LM, Ayon C, Gurrola M. Estamos Traumados: The Effect of Anti-Immigrant Sentiment and Policies on the Mental Health of Mexican Immigrant Families. J Community Psychol. 2013;41(8):1005–1020. [Google Scholar]
- 10.Bränström R, Hatzenbuehler ML, Pachankis JE, Link BG. Sexual Orientation Disparities in Preventable Disease: A Fundamental Cause Perspective. Am J Public Health. 2016;106(6):1109–1115. doi: 10.2105/AJPH.2016.303051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bauer GR. Incorporating intersectionality theory into population health research methodology: Challenges and the potential to advance health equity. Soc Sci Med. 2014;110:10–17. doi: 10.1016/j.socscimed.2014.03.022. [DOI] [PubMed] [Google Scholar]
- 12.Pollitt RA, Rose KM, Kaufman JS. Evaluating the evidence for models of life course socioeconomic factors and cardiovascular outcomes: a systematic review. Bmc Public Health. 2005;5 doi: 10.1186/1471-2458-5-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Miller GE, Chen E, Fok AK, et al. Low early-life social class leaves a biological residue manifested by decreased glucocorticoid and increased proinflammatory signaling. P Natl Acad Sci USA. 2009;106(34):14716–14721. doi: 10.1073/pnas.0902971106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bouton ME. Context and behavioral processes in extinction. Learning & Memory. 2004;11(5):485–494. doi: 10.1101/lm.78804. [DOI] [PubMed] [Google Scholar]
- 15.Viruell-Fuentes EA, Miranda PY, Abdulrahim S. More than culture: Structural racism, intersectionality theory, and immigrant health. Soc Sci Med. 2012;75(12):2099–2106. doi: 10.1016/j.socscimed.2011.12.037. [DOI] [PubMed] [Google Scholar]
- 16.Abraido-Lanza AF, Dohrenwend BP, Ng-Mak DS, Turner JB. The Latino mortality paradox: a test of the “salmon bias” and healthy migrant hypotheses. Am J Public Health. 1999;89(10):1543–1548. doi: 10.2105/ajph.89.10.1543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gee GC, Walsemann KM, Brondolo E. A Life Course Perspective on How Racism May Be Related to Health Inequities. Am J Public Health. 2012;102(5):967–974. doi: 10.2105/AJPH.2012.300666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.International Lesbian G, Bisexual, Trans, and Intersex Association. Sexual Orientation Laws in the World. 2016 http://ilga.org/downloads/03_ILGA_WorldMap_ENGLISH_Overview_May2016.pdf Accessed February 3, 2017.
- 19.Weatherburn P, Schmidt AJ, Hickson F, et al. The European Men-Who-Have-Sex-With-Men Internet Survey (EMIS): Design and Methods. Sex Res Soc Policy. 2013;10(4):243–257. [Google Scholar]
- 20.The EMIS Network. EMIS 2010: the European men-who-have-sex-with-men internet survey Findings from 38 countries. Stockholm: European Centre for Disease Prevention and Control; 2013. http://www.emis-project.eu/ [Google Scholar]
- 21.Hatzenbuehler ML, Link BG. Introduction to the special issue on structural stigma and health. Soc Sci Med. 2014;103:1–6. doi: 10.1016/j.socscimed.2013.12.017. [DOI] [PubMed] [Google Scholar]
- 22.Urquia ML, O’Campo PJ, Heaman MI. Revisiting the immigrant paradox in reproductive health: The roles of duration of residence and ethnicity. Soc Sci Med. 2012;74(10):1610–1621. doi: 10.1016/j.socscimed.2012.02.013. [DOI] [PubMed] [Google Scholar]
- 23.Newcomb ME, Mustanski B. Racial Differences in Same-Race Partnering and the Effects of Sexual Partnership Characteristics on HIV Risk in MSM: A Prospective Sexual Diary Study. Jaids-J Acq Imm Def. 2013;62(3):329–333. doi: 10.1097/QAI.0b013e31827e5f8c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Berry JW. Immigration, acculturation, and adaptation. Appl Psychol-Int Rev. 1997;46(1):5–34. [Google Scholar]
- 25.Acevedo-Garcia D, Sanchez-Vaznaugh EV, Viruell-Fuentes EA, Almeida J. Integrating social epidemiology into immigrant health research: A cross-national framework. Soc Sci Med. 2012;75(12):2060–2068. doi: 10.1016/j.socscimed.2012.04.040. [DOI] [PubMed] [Google Scholar]
- 26.Ruiz Y, Guilamo-Ramos V, McCarthy K, Munoz-Laboy MA, Lopez MDR. Exploring Migratory Dynamics on HIV Transmission: The Case of Mexicans in New York City and Puebla, Mexico. Am J Public Health. 2014;104(6):1036–1044. doi: 10.2105/AJPH.2013.301770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.McKetta S, Hatzenbuehler M, Pratt C, et al. Does Social Selection Explain the Association between State-Level Racial Animus and Racial Disparities in Self-Rated Health in the United States? New York, NY: Columbia University; 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Higa DH, Crepaz N, Marshall KJ, et al. A Systematic Review to Identify Challenges of Demonstrating Efficacy of HIV Behavioral Interventions for Gay, Bisexual, and Other Men Who Have Sex with Men (MSM) Aids Behav. 2013;17(4):1231–1244. doi: 10.1007/s10461-013-0418-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Amon JJ. The political epidemiology of HIV. J Int Aids Soc. 2014;17 doi: 10.7448/IAS.17.1.19327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hernando V, Alvarez-del Arco D, Alejos B, et al. HIV Infection in Migrant Populations in the European Union and European Economic Area in 2007–2012: An Epidemic on the Move. Jaids-J Acq Imm Def. 2015;70(2):204–211. doi: 10.1097/QAI.0000000000000717. [DOI] [PubMed] [Google Scholar]


