Abstract
Pediatric brain tumor survivors are at risk for significant difficulties related to social competence. Little research has examined factors that contribute to survivor social problems.
Purpose
The current study is grounded in a model of social competence for youth with brain disorder and used qualitative and quantitative methods to obtain caregiver perspectives on survivor social competence and identify pertinent risk and resistance factors.
Methods
The study occurred in two phases, including focus groups with 36 caregivers of 24 survivors and confirmatory interviews with 12 caregivers of 12 survivors.
Results
Qualitative content analyses resulted in three themes that were illustrative of the model of social competence. Themes included 1) the impact of survivor sequelae on social function; 2) the role of family in evaluating and promoting survivor social development; and 3) the match between the survivor’s social context and developmental needs. Quantitative data supported the associations between survivor social skills, survivor executive function and family functioning.
Conclusions
Overall, findings underscore the influence of risk and resistance factors across different systems on survivor social competence and suggest directions for future research and intervention efforts.
Keywords: pediatric brain tumor, qualitative, social competence
Pediatric brain tumor survivors (PBTS) have the poorest health-related quality of life (HRQL) [1] among childhood cancer survivors and are at risk for social difficulties [2]. PBTS have lower rates of peer acceptance and increased social isolation [2], and achieve adult milestones (e.g., living independently) at lower rates compared to controls [3,4]. While neurodevelopmental late effects, including neurocognitive [5] and physical deficits [3,4], likely contribute to poor psychosocial functioning [2], little research has examined factors related to PBTS social functioning. Given the significance of social development [6], additional research exploring PBTS social competence is needed.
Social competence refers to successfully attaining goals in social interactions while maintaining positive relationships [7,8]. It is comprised of personal characteristics (i.e. social skills), social interactions (i.e. prosocial, aggressive or withdrawn behaviors), and social adjustment (i.e. perception of relationship quality and social/developmental goal attainment) [8,9]. Social competence is a developmental construct dependent upon time, context, and the self [9]. Prior research on PBTS social competence suggests deficits in social adjustment [2]. Few studies have examined risk/resilience factors for survivor social adjustment. In general, lower IQ [10], attention and executive function problems [11], poor facial expression recognition abilities [12], and lower socio-economic status [13] have been associated with poorer parent-rated social adjustment.
Given the lack of research on survivor social adjustment and the complex challenges of PBTS and families, studies are warranted that employ varying methodologies and a guiding framework. Qualitative research, in particular, offers opportunities to provide in-depth understanding of multiple aspects of families’ experiences with survivor social competence that can guide future research and clinical intervention [14]. Furthermore, qualitative research that employs a guiding theoretical framework strengthens the conceptualization and methods of such procedures and the various factors that should be explored [14].
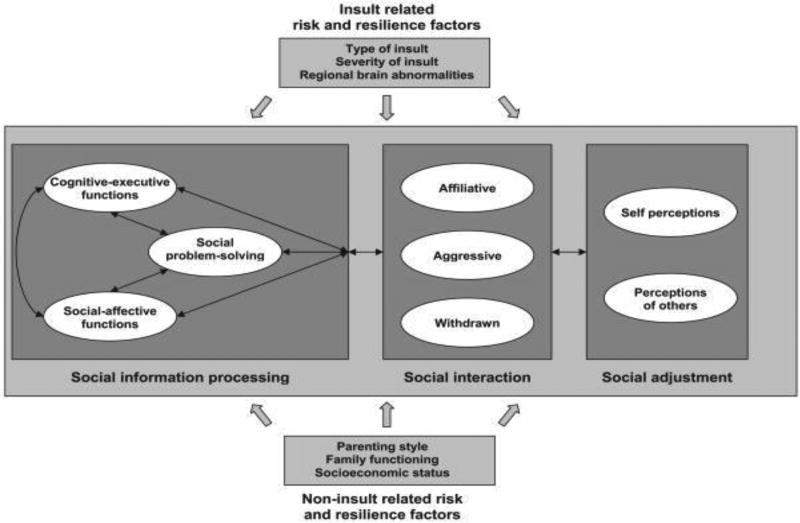
A model of social competence for childhood brain disorder (Figure 1) [8] provides a framework for enhancing our understanding of PBTS social functioning [15]. The model is grounded in developmental psychology and social cognitive neuroscience and emphasizes the role of neurocognitive function and social cognition abilities [8, 16]. These abilities influence interactions with peers and subsequently social adjustment. The model also specifies risk and resilience factors that may moderate the impact of CNS insults on three domains of social competence [8, 16, 17]. These factors encompass insult-related and proximal environmental (e.g., family functioning, parenting style) and distal environmental non-insult-related variables (e.g., socioeconomic status) [10, 18].
Fig. 1.
A model of social competence in children with brain disorder [8]
The model of social competence [8] informs the current study by providing comprehensive factors to examine, thereby reducing bias. The primary aim of this study was to use qualitative methods to obtain caregivers’ perspectives on survivor social competence and important risk/resilience factors. Such data may increase our understanding of survivor social competence and relevant influences, inform future longitudinal investigations, and facilitate intervention development [19]. A secondary aim was to use quantitative data to supplement the qualitative data and further describe the sample.
Methods
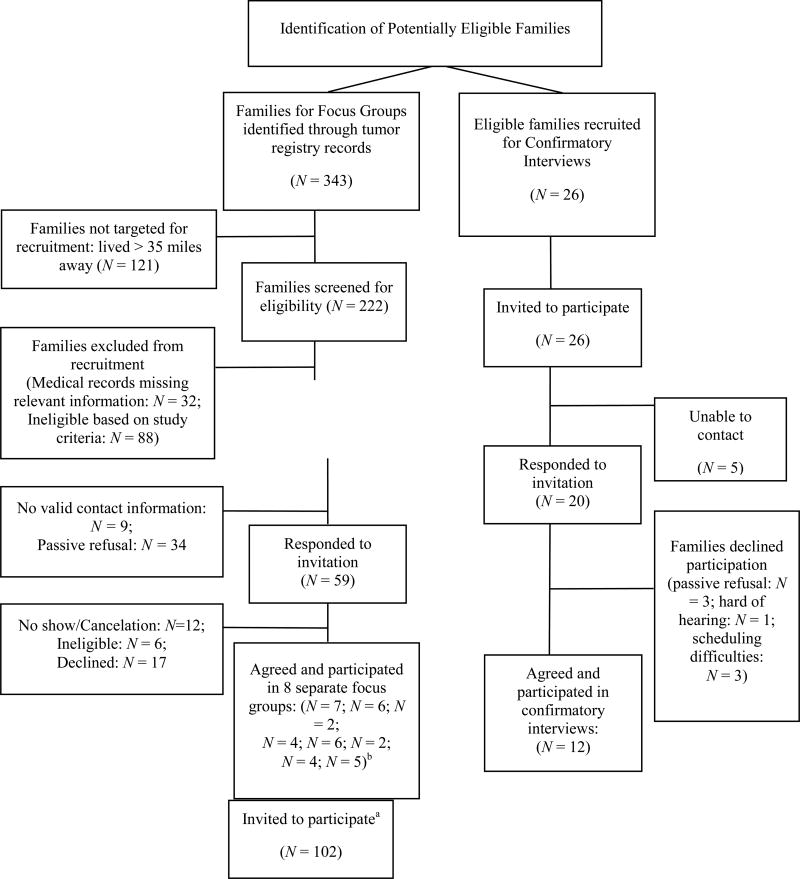
This study involved two phases with caregivers of PBTS ages 8–17 years. The first phase included focus groups and content analysis of qualitative data to identify themes. Questionnaire data also were collected to explore themes quantitatively. The second phase involved individual confirmatory interviews with caregivers to substantiate the themes identified in the focus groups [20]. Such an approach enhances the rigor of the methodology and the validity of the findings [20]. For both phases, purposeful, maximum variation-based samples were recruited to obtain data from varying perspectives [21]. Caregiver eligibility criteria included 1) being the parent/guardian of a PBTS meeting eligibility criteria; 2) living with the survivor at least 50% of the time; and 3) former/current involvement in their survivor’s oncology-related care. Survivors were at least five years from diagnosis and two years removed from tumor-directed treatment. Survivors with neurofibromatosis (n = 54) or a history of cognitive or developmental delays prior to brain tumor diagnosis noted in their medical record (n = 8) and those from non-English speaking families were excluded. Figure 2 provides a recruitment overview. Focus groups occurred at the cancer center while interviews were conducted via phone. An institutional review board approved all study procedures. Participants did not differ from non-participants on any demographic variables. Three participants from the focus groups also participated in a confirmatory interview.
Fig. 2.
Study Recruitment Summary
aUp to two caregivers per survivor were invited to participate
bN’s represent number of caregivers rather than number of survivors as in rest of figure
Focus Group Procedures
Up to two caregivers per survivor were invited to participate in focus groups. Caregivers were contacted via letter and then by phone. Of the 17 families that actively declined to participate, typical reasons included distance to the hospital and feeling too busy. Facilitators obtained informed consent and guided discussion using scripts (Appendix 1). Participants were asked to discuss a) survivor social functioning (e.g., “How do they get along with others their own age?”), b) factors contributing to social functioning (e.g., “What factors work for/against your survivor in social situations?”), and c) their attempts to promote survivor adjustment (e.g., “What kinds of things have you tried to promote better social relationships?”). Focus groups lasted approximately 1.5 hours and were audiotaped and transcribed. Focus groups were moderated by a licensed psychologist (MH) or nurse (JD), both with experience in conducting focus groups and pediatric neuro-oncology. Participants completed a demographics questionnaire and measures described below. Caregivers were compensated for participating.
Measures
Family Functioning
The 12-item General Functioning Scale from the McMaster Family Assessment Device (FAD GFS) measured general family functioning [22]. Higher scores (range 1–4) indicate greater dysfunction with scores above 2.0 representing poor family functioning. Internal consistency was .91.
Survivor Social Adjustment
Caregivers rated survivor social adjustment using the PedsQL 4.0 [23]. The PedsQL 4.0 measures HRQL across physical, emotional, social and school domains over the past month. Social HRQL scores were used in analyses with higher scores representing better functioning. Internal consistency was .77 for social HRQL.
Survivor Executive Functioning
The Global Executive Composite (GEC) from the Behavior Rating Inventory of Execute Function (BRIEF) assessed executive function [24], with higher scores suggesting greater dysfunction. Internal consistency was .98 for GEC scores.
Survivor Social Skills
The Social Skills Improvement System (SSIS) evaluated social skills and problem behaviors [25]. Higher social skills scores indicate better developed skills, while higher problem behaviors scores indicate more difficulties. The internal consistencies were .94 and .97 for the social skills and problem behaviors scales, respectively.
Confirmatory Interviews
Interviews with caregivers of PBTS were conducted to confirm the themes identified from focus groups. Participants read a fictional case summary (Appendix 2) of a PBTS that highlighted the identified themes and then responded to standardized questions (Appendix 3). Caregivers completed a demographics questionnaire and were compensated for participating.
Data analyses
Qualitative data
Qualitative data from focus groups and interviews were analyzed the same way using ATLAS.ti© software. Analysis followed an established protocol using content analytic methods, including deductive and inductive approaches. Qualitatively-oriented content analyses evaluated the data, initially directed by an a priori list of codes [26]. Analysis proceeded from specific codes to broader categories to larger themes.
Coding teams reviewed and coded transcripts using inductively-derived codes. Primary coders coded each transcript followed by secondary coders, who reviewed the coding and suggested edits. Coding teams discussed discrepancies until reaching a consensus. An audit trail was kept to enhance rigor [27]. A working group reviewed coding categories and their related content to identify broader themes. Focus groups and interviews were conducted until it was determined that saturation had been achieved. Given that the results from the individual interviews largely confirmed the findings from the focus groups, the qualitative findings are presented together.
Quantitative data
Descriptive statistics summarized demographic characteristics, tumor-related variables, family functioning, and survivor outcomes. Pearson bivariate correlations examined associations between variables. In the 12 families where two caregivers provided data for a survivor, one caregiver’s data was included in analyses to avoid issues related to non-independence [28] and was typically the father’s data in order to increase their representativeness in the sample.
Results
Sample Characteristics
Thirty-six caregivers (13 fathers; Mage = 48.53; 91.7% Caucasian) participated in the focus groups representing 24 survivors (13 male; Mage = 14.47; Mage at diagnosis = 6.29). Twelve caregivers participated in the confirmatory interviews (2 male; Mage = 51.25; 83.3% Caucasian) representing 12 survivors (7 male; Mage = 13.17; Mage at diagnosis = 4.89). Caregivers varied in terms of education and household income. See Table 1 for more information on demographic characteristics.
Table 1.
Sample Characteristics
| Variables | Focus Groups (n = 36) | Interviews (n = 12) | |
|---|---|---|---|
|
| |||
| n (%) or M ± SD | n (%) or M ± SD | ||
| Caregiver Sex | |||
| Male | 13 (36.1) | 2 (16.7) | |
| Female | 23 (63.9) | 10 (83.3) | |
| Caregiver Age (years) | 48.53 ± 6.76 | 51.25 ± 16.81 | |
| Caregiver Ethnicity | |||
| White | 33 (91.7) | 10 (83.3) | |
| African-American | 2 (5.6) | 2 (14.3) | |
| Asian | 1 (2.8) | 0 (0.0) | |
| Caregiver Education | |||
| High school degree or less | 10 (27.8) | 2 (16.7) | |
| Some college/vocational school | 11 (30.5) | 2 (16.7) | |
| Graduate of 4 year college or higher | 15 (41.7) | 8 (66.6) | |
| Household/Family Income | |||
| Less than $50,000 | 3 (8.4) | 2 (16.7) | |
| $50,000 – $74,000 | 12 (33.3) | 5 (41.7) | |
| $75,000 – $99,000 | 2 (5.6) | 3 (25) | |
| Over $100,000 | 16 (48.4) | 2 (16.7) | |
| Survivor Sex | |||
| Male | 13 (54.2) | 7 (58.3) | |
| Female | 11 (45.8) | 5 (41.7) | |
| Survivor Age (years) | 14.47 ± 2.29 | 13.17 ± 3.10 | |
| Survivor Age at Diagnosis (years) | 6.29 ± 3.29 | 4.89 ± 2.95 | |
| Survivor Diagnosis | |||
| Astrocytoma | 9 (37.5) | 3 (25) | |
| Medulloblastoma | 4 (16.7) | 4 (33.3) | |
| Craniopharyngioma | 3 (12.5) | 0 (0.0) | |
| Ependymoma | 2 (8.3) | 2 (16.7) | |
| Other | 6 (25) | 3 (25) | |
| Treatment | |||
| Surgical resection | 23 (95.8) | 12 (100) | |
| Chemotherapy | 9 (37.5) | 6 (50) | |
| Radiation therapy | 10 (41.7) | 7 (58.3) | |
Qualitative Results
Three themes were identified that are consistent with the social competence model and broader social ecological theory [15]. Themes include individual survivor factors and issues relevant to other systems affecting the survivor, including the family and broader social context. Themes are discussed below and presented in Table 2 with example quotations and implications for research and clinical care.
Table 2.
Qualitative Themes
| Themes | Example Quotations: Focus Groups |
Example Quotations: Interviews | Research/Clinical Implications |
|---|---|---|---|
|
| |||
Impact of medical, physical and psychological sequelae on survivors’ social functioning
|
“And then he got into junior high and he seemed perfectly normal. They were having parties and they were having good times… Then he started having seizures. His entire life changed. He has never been the same since then. Never.” (17 year-old survivor) | “The one younger boy who’s about three years younger, he’ll say, well, can survivor come over? And my husband and I do feel like that’s kind of weird. Like not weird that he gets along with him, ‘cause I think he… he’s a nice kid and everything, but it’s, um… unusual for a fifteen-year-old to want to hang out with a twelve-year-old.” (15 year-old survivor) |
|
| “So now you’re a teenager. You got no hair on the left side of your head. You can’t drive ‘cause you can’t see. So he is very introverted. It’s been a real tough three years for him. Real tough.” (17 year-old survivor) | “She’s just speaking as if she, you know, has no microphone and a crowd of two hundred thousand.” (11 year-old survivor) | ||
| “I had the same thing with survivor with sleepovers. Eight and a half pills a day…nine needles a day. Who wants to take her for a sleepover? Oh, that’s a challenge.” (11 year-old survivor) | “Yeah, reading body language… he totally (chuckling) is not able to like… he doesn’t get sarcasm, um, anymore, you know, like uh, body language.” (17 year-old survivor) | ||
|
| |||
Role of family in evaluating and supporting survivor social development
|
“It’s like if I don’t push him to get stuff done socially, then it’s not going to get done. So and I just kind of pick and choose the ones that I want to escalate to that level.” (17 year-old survivor) | “And so I think any parent who has a kid with a disability walks that fine line of… how much should I push them to, you know, accomplish or go beyond what they’re able to do, you know, how much should I, you know, let them go and just back off.” (17 year-old survivor) |
|
| “And this social thing, when you’re in hospital for the physical part of it, the resection and the chemo… you know, like you can put it in their hands, but like with this, it’s in my hands and I don’t know what to do.” (17 year-old survivor) | “His father and I are like the total opposites… like I tend to be more, okay, you can do it, go ahead and go, and he is… he totally is like the shelter person. No, don’t let him walk out of the house. He can’t leave. He’s going to be here forever. You know, he’s going to get hurt. He’s like the total opposite.” (17 year-old survivor) | ||
| “It’s really hard to know what typical seventeen year old behavior… is and what is caused by the brain tumor.” (17 year-old survivor) | “All the other kids are interacting immediately off of what the next kid is saying and she wouldn’t be. So…if I happen to be in the setting, I would kind of almost like interpret for her… because I just feel like if she doesn’t have that, then she’s really missing a big chunk of what’s going on.” (16 year-old survivor) | ||
|
| |||
Importance of match between survivor social context and developmental needs
|
“And to further complicate that in our situation he’s… in our neighborhood there aren’t any kids his age. Plus all his friends are at school, and they all live like an hour away. So getting out to them on a regular basis, … it’s difficult.” (13 year-old survivor) | “Because we’re in the projects … not saying it’s not safe, ‘cause I… she don’t be out here.” (13 year-old survivor) |
|
| “… there’s kids from say like first to like seventh grade like in the group of kids…and they all kind of like congregate together and play together. You know what I mean? They’ll be running, playing tag and stuff like that.” (12 year-old survivor) | |||
| “…with his music teachers, he has much more connections or camaraderie. Like I think if he could stay at his guitar teacher’s house and talk to him about music and life … he would do that, versus doing anything with his peers.” (13 year-old survivor) | “And the school is apparently used to socialization and academic skills being on the same level. And they don’t know what to do with a child who socializes at their age level but who was academically several years behind their age level.” (11 year-old survivor) | ||
Theme 1: Impact of medical, physical and psychological sequelae on survivors’ social functioning
Caregivers described issues related to the effects of tumor and treatments on social functioning. Physical limitations and demands related to sequelae were noted to impact participation in normative activities (e.g., sports, sleepovers), hindering social engagement. Caregivers also highlighted how survivors’ and others’ reactions to medical sequelae impact social behavior, noting issues related to self-esteem or inclusion by others in activities. When discussing interactions with peers, caregivers described discomfort with same-age peers, noting that survivors often prefer to socialize with older or younger individuals. They attributed this to mismatched developmental levels with peers; one parent stated that his survivor “…thinks she’s 36 but she’s 11 and I think that sometimes she sets herself up socially for a fall in that regard” (11 year-old survivor). Additionally, some caregivers described challenges related to survivor interpretation of peer behavior (e.g., social cues, nonverbal communication).
Theme 2: Role of family in evaluating and supporting survivor social development
Caregivers expressed difficulties with evaluating whether or not survivor social behavior was developmentally appropriate. This evaluation process contributed to variability across and within families in terms of parental involvement in survivor social engagement. Some caregivers reported a significant role in promoting survivor involvement in social activities, while others were not as involved. Caregivers described different approaches within families, noting conflict between partners. One father stated, “…sometimes my wife and I … we’ll butt heads because of … different solutions to the problem” (16 year-old survivor). Caregivers also noted variability related to how much the family serves as their survivor’s main social outlet.
Theme 3: Importance of the match between survivor social context and developmental needs
A final theme related to how well the broader social environment provides appropriate opportunities for survivors to engage socially and develop an identity. Survivors living in areas offering more social opportunities (e.g., neighborhoods populated with children) appeared to have higher quality friendships and interactions with peers. Caregivers also reported better outcomes related to social engagement and identity when survivors participate in activities that suit their physical or developmental abilities. One mother noted that her son’s participation in band, despite his physical limitations, “…serves as a unifying force for his friendships” (14 year-old survivor). Some caregivers, however, indicated challenges related to how well schools or communities include their survivors and address their social needs.
Quantitative Results
Table 3 presents descriptive and correlational data of measures given following focus groups. Overall, caregivers reported survivor social skills and problem behaviors and family functioning in the average range. Parent-reported executive function abilities also were in the average range with only 12.5% of survivors in the range for clinical difficulties. However, caregiver-reported levels of survivor social HRQL were low compared to healthy norms, t = − 2.06, p = .05 [29]. Correlations revealed that better family functioning and executive function were significantly associated with better social skills. Additionally, executive function difficulties and problem behaviors were associated with poor social HRQL.
Table 3.
Means, Standard Deviations and Correlations Among Quantitative Variables
| Variables | Mean (SD) | 2 | 3 | 4 | 5 | 6 | 7 |
|---|---|---|---|---|---|---|---|
| 1. Survivor Social Skills (SSIS) | 98.54 (14.71) | .44* | −.49* | −.41* | −.56** | −.28 | −.18 |
| 2. Survivor Social Quality of Life (PedsQL) | 75.42 (19.72) | - | −.70** | −.38 | −.73** | −.16 | −.31 |
| 3. Survivor Problem Behaviors (SSIS) | 100.75 (18.88) | - | - | .63** | .88** | .09 | .50* |
| 4. Family Functioning (FAD) | 1.64 (0.62) | - | - | - | .42* | −.04 | .28 |
| 5. Survivor Executive Functioning (BRIEF) | 54.42 (12.96) | - | - | - | - | .34 | .41* |
| 6. Survivor Age | 14.46 (2.23) | - | - | - | - | - | .13 |
| 7. Time Since Diagnosis (Years) | 8.80 (2.93) | - | - | - | - | - | - |
p ≤ .05;
p ≤ .01
Conclusions
This study employed multiple methodologies to obtain caregiver perspectives on the factors important to PBTS social functioning. Qualitative and quantitative data support the relevance of variables highlighted in an integrative model of social competence [8]. Individual interviews with caregivers confirmed the findings and themes identified from the focus groups, enhancing the rigor and validity of this study. Caregivers endorsed the importance of medical and neurodevelopmental sequelae, family interpretation and management of survivor social functioning, and broader contextual circumstances. This study provides information not currently seen in the literature, particularly related to the role of parents in promoting social engagement, and offers directions for research and implications for intervention, including assessment of survivor social cognition, family-based interventions, and development of programs that support survivor inclusion in developmentally-appropriate activities.
Consistent with prior literature [15], caregivers highlighted the direct and indirect influences of insult-related factors on survivor SIP and social interactions. Caregivers discussed how insult-related factors affect survivors’ ability to engage in social activities, as well as how neurodevelopmental late effects impact survivor performance in social situations. Difficulties attending to conversations and understanding non-verbal communication (e.g., body language, sarcasm) were noted. Secondary quantitative data underscored these issues, suggesting associations between poorer executive function and worse social skills and social HRQL, supporting an earlier study with PBTS [11]. Research in pediatric traumatic brain injury (TBI) highlight social cognition processes in social adjustment, including pragmatic language [30], social problem-solving [31] and facial expression recognition [32]. However, outside of a study suggesting facial expression recognition deficits in PBTS [12], little research has examined social cognition processes in PBTS.
In accordance with the model, caregivers emphasized family systems factors affecting survivor social functioning. While family factors have been shown to moderate youth social outcomes in TBI [16], few studies have examined associations between family processes and PBTS social competence. Caregivers noted issues related to parental interpretation of behavior and parenting style that affect how they support survivor social functioning. This suggests that interventions that educate parents on normative social development and offer strategies for promoting social engagement (e.g., problem-solving skills therapy) throughout development might positively affect PBTS social adjustment. Quantitative data supported the qualitative findings indicating that broader family functioning is positively associated with survivor social skills.
Interestingly, caregivers endorsed the significance of contextual factors beyond the family in PBTS social competence. The presence of positive environmental factors (e.g., neighborhoods with same-age children) was identified as important in promoting survivor social competence and potentially offsetting insult-related risk factors. Caregivers noted that survivors who found a social niche through a neighborhood or activity were more active socially and able to establish a social identity. While the model of social competence acknowledges socio-economic status [8] and broader social ecological theory [18] underscores the impact of systems beyond the family on child development, the influential nature of these systems has not been thoroughly studied in relation to PBTS neurodevelopmental outcomes. The findings in this study emphasize the importance of the match between environmental resources and survivors’ developmental needs. Future research should examine the extent to which broader contextual factors moderate PBTS’ social adjustment and explore adding such factors to the model of social competence.
The current study offers several directions for research and clinical intervention. At the survivor level, additional studies are needed that examine the contributions of SIP factors, particularly social cognition, on social interactions and social adjustment. Additionally, in-depth investigation of the caregiver factors related to PBTS social competence is warranted, including the role of caregiver attributions of survivor behavior and caregiver involvement. Such research on social cognition and caregiver roles could identify important intervention targets. Furthermore, interventions incorporating technology could facilitate social connectedness for survivors who have limited options in their immediate environment.
This study has limitations that should be considered. First, data was collected solely from caregivers and does not reflect survivor or peer perspectives. Collecting qualitative information from survivors would provide an interesting comparison. Additionally, the quantitative measures are only intended for caregivers and do not allow for survivor input. Second, while there is diversity in terms of caregiver sex, there is less diversity in terms of caregiver ethnicity and socio-economic background, limiting exploration of cultural or economic factors. Finally, the overall participation rate was relatively low. However, participants did not differ from non-participants on demographic variables.
In summary, this study provides innovative data on caregiver perspectives of PBTS social competence. The findings demonstrate the importance of studying survivor social competence from a strong theoretical framework and suggest key directions for future research and clinical intervention for this at-risk population.
Supplementary Material
Acknowledgments
The National Cancer Institute funded this research (1K07CA178100). The authors thank all study participants and Julie Baran, Lauren Lipshutz, Linda Maldonado, Kelly Mannion, Mark McCurdy, and Elise Turner for their roles in data analyses.
Footnotes
There are no conflicts of interest to disclose.
References
- 1.Zeltzer L, Recklitis CJ, Buchbinder D, Zebrack B, Casillas JN, Tsao JCI, Lu Q, Krull K. Psychological status in childhood cancer survivors: A report from the Childhood Cancer Survivor Study. J Clin Oncol. 2009;27:2396–2404. doi: 10.1200/JCO.2008.21.1433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Schulte F, Barrera M. Social competence in childhood brain tumor survivors: A comprehensive review. Support Care Cancer. 2010;18:1499–1513. doi: 10.1007/s00520-010-0963-1. [DOI] [PubMed] [Google Scholar]
- 3.Ness KK, Morris EB, Nolan VG, Howell CR, Gilchrist LS, Stovall M, Cox CL, Klosky JL, Gajjar A, Neglia JP. Physical performance limitations among adult survivors of childhood brain tumors. Cancer. 2010;116:3034–3044. doi: 10.1002/cncr.25051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zebrack B, Gurney JG, Oeffinger KC, Whitton JA, Packer RJ, Mertens A, Turk N, Castleberry R, Dreyer Z, Robison LL, Zeltzer LK. Psychological outcomes in long-term survivors of childhood brain cancer: A report from the Childhood Cancer Survivor Study. J Clin Oncol. 2004;22:999–1006. doi: 10.1200/JCO.2004.06.148. [DOI] [PubMed] [Google Scholar]
- 5.Robinson KE, Kuttesch JF, Champion JE, Andreotti CF, Hipp DW, Bettis A, Barnwell A, Compas BE. A quatitative meta-analysis of neurocognitive sequelae in survivors of pediatric brain tumors. Pediatr Blood Cancer. 2010;55:525–531. doi: 10.1002/pbc.22568. [DOI] [PubMed] [Google Scholar]
- 6.Parker JG, Asher SR. Peer relations and later personal adjustment: Are low-accepted children at risk? Psychol Bull. 1987;102:357–389. doi: 10.1037//0033-2909.102.3.357. [DOI] [PubMed] [Google Scholar]
- 7.Parker JG, Rubin KH, Erath SA, Wojslawowicz JC, Buskirk AA. Peer relationships and developmental psychopathology. In: Cicchetti D, Cohen D, editors. Developmental psychopathology: Risk, disorder, and adaptation. Wiley; New York: 2006. pp. 419–493. [Google Scholar]
- 8.Yeates KO, Bigler ED, Dennis M, Gerhardt CA, Rubin KH, Stancin T, Taylor HG, Vannatta K. Social outcomes in childhood brain disorder: A heuristic integration of social neuroscience and developmental psychology. Psychol Bull. 2007;133:535–556. doi: 10.1037/0033-2909.133.3.535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rubin KH, Rose-Krasnor L. Interpersonal problem-solving and social competence in children. In: Van Hassett VB, Hersen M, editors. Handbook of social development. Plenum; New York: 1992. pp. 283–323. [Google Scholar]
- 10.Moyer KH, Willard VW, Gross AM, Netson KL, Ashford JM, Kahalley LS, Wu S, Xiong X, Conklin HM. The impact of attention on social functioning in survivors of pediatric acute lymphoblastic leukemia and brain tumors. Pediatr Blood Cancer. 2012;59:1290–1295. doi: 10.1002/pbc.24256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wolfe KR, Walsh KS, Reynolds NC, Mitchell F, Reddy AT, Paltin I, Madan-Swain A. Executive functions and social skills in survivors of pediatric brain tumor. Child Neuropsychol. 2012;19:370–384. doi: 10.1080/09297049.2012.669470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bonner MJ, Hardy KK, Willard VW, Anthony KK, Hood M, Gururangan S. Social functioning and facial expression recognition in survivors of pediatric brain tumors. J Pediatr Psychol. 2008;33:1142–1152. doi: 10.1093/jpepsy/jsn035. [DOI] [PubMed] [Google Scholar]
- 13.Carlson-Green B, Morris RD, Krawiecki NS. Family and illness predictors of outcome in pediatric brain tumors. J Pediatr Psychol. 1995;20:769–784. doi: 10.1093/jpepsy/20.6.769. [DOI] [PubMed] [Google Scholar]
- 14.Wu YP, Thompson D, Aroian KJ, McQuaid EL, Deatrick JA. Commentary: Writing and Evaluating Qualitative Research Reports. J Pediatr Psychol. 2016;41(5):493–505. doi: 10.1093/jpepsy/jsw032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hocking MC, McCurdy M, Turner E, Kazak AE, Noll RB, Phillips P, Barakat LP. Social competence in pediatric brain tumor survivors: Application of a model from social neuroscience and developmental psychology. J Pediatr Blood Cancer. 2015;62:375–384. doi: 10.1002/pbc.25300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yeates KO, Swift E, Taylor HG, Wade SL, Drotar D, Stancin T, Minich N. Short- and long-term social outcomes following pediatric traumatic brain injury. J Int Neuropsychol Soc. 2004;10:412–426. doi: 10.1017/S1355617704103093. [DOI] [PubMed] [Google Scholar]
- 17.Ganesalingam K, Yeates KO, Taylor HG, Walz NC, Stancin T, Wade SL. Executive functions and social competence in young children 6 months following traumatic brain injury. Neuropsychology. 2011;25:466–476. doi: 10.1037/a0022768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bronfrenbrenner U. The ecology of human development. Harvard University Press; Cambridge: 1979. [Google Scholar]
- 19.Crick NR, Dodge KA. A review and reformulation of social information-processing mechanisms in children's social adjustment. Psychol Bull. 1994;115:74–101. [Google Scholar]
- 20.Guba EG. Criteria for assessing the trustworthiness of naturalistic inquiries. Educ Comm Technol. 1981;29:75–91. [Google Scholar]
- 21.Patton MQ. Qualitative research and evaluation methods. 3. Thousand Oaks, CA: Sage; 2002. [Google Scholar]
- 22.Epstein NB, Baldwin LM, Bishop DS. The McMaster Family Assessment Device. J. Marital Fam. Ther. 1983;9:171–180. [Google Scholar]
- 23.Varni JW, Seid M, Kurtin PS. The PedsQL 4.0: Reliability and validity of the Pediatric Quality of Life Inventory 4.0 version. Medical Care. 2001;39:800–812. doi: 10.1097/00005650-200108000-00006. [DOI] [PubMed] [Google Scholar]
- 24.Gioia GA, Isquith PK, Guy SC, Kenworthy L. Behavior Rating Inventory of Executive Function: BRIEF. Psychological Assessment Resources; Odessa: 2000. [Google Scholar]
- 25.Gresham FM, Elliott SN. Social Skills Improvement System Rating Scales manual. NCS Pearson.Patton; Minneapolis: 2008. [Google Scholar]
- 26.Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277–1288. doi: 10.1177/1049732305276687. [DOI] [PubMed] [Google Scholar]
- 27.Sandelowski M. The problem of rigor in qualitative research. Adv Nurs Sci. 1986;8:27–37. doi: 10.1097/00012272-198604000-00005. [DOI] [PubMed] [Google Scholar]
- 28.Kenny DA, Kashy DA, Cook WL. Dyadic data analysis. Cambridge Univeristy Press; New York: 2006. [Google Scholar]
- 29.Varni JW, Limbers C, Burwinkle TS. Literature Reviews: Health-related quality of life measurement in pediatric oncology: Hearing the voices of the children. J Pediatr Pscyhol. 2007;32:1151–1163. doi: 10.1093/jpepsy/jsm008. [DOI] [PubMed] [Google Scholar]
- 30.Dennis M, Barnes MA, Wilkinson M, Humphreys RP. How children with head injury represent real and deceptive emotion in short narratives. Brain Lang. 1998;61:450–483. doi: 10.1006/brln.1997.1886. [DOI] [PubMed] [Google Scholar]
- 31.Janusz JA, Kirkwood MW, Yeates KO, Taylor HG. Social problem-solving skills in children with traumatic brain injury: Long-term outcomes and prediction of social competence. Child Neuropsychol. 2002;8:179–194. doi: 10.1076/chin.8.3.179.13499. [DOI] [PubMed] [Google Scholar]
- 32.Dennis M, Simic N, Agostino A, Taylor HG, Bigler ED, Rubin K, Vannatta K, Gerhardt CA, Stancin T, Yeates KO. Irony and empathy in children with traumatic brain injury. J Int Neuropsychol Soc. 2013;19:338–348. doi: 10.1017/S1355617712001440. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.