Highlights
-
•
The cell biology of Candida albicans is adapted both for life as a commensal and as a pathogen.
-
•
C. albicans can either downregulate or upregulate virulence properties in the human host.
-
•
This fungus modulates the activity of phagocytes to enable its own survival.
-
•
Candida is metabolically flexible enabling it to survive in multiple niches in the host.
Abstract
Candida albicans is a commensal coloniser of most people and a pathogen of the immunocompromised or patients in which barriers that prevent dissemination have been disrupted. Both the commensal and pathogenic states involve regulation and adaptation to the host microenvironment. The pathogenic potential can be downregulated to sustain commensalism or upregulated to damage host tissue and avoid and subvert immune surveillance. In either case it seems as though the cell biology of this fungus has evolved to enable the establishment of different types of relationships with the human host. Here we summarise latest advances in the analysis of mechanisms that enable C. albicans to occupy different body sites whilst avoiding being eliminated by the sentinel activities of the human immune system.
Current Opinion in Microbiology 2016, 34:111–118
This review comes from a themed issue on Parasitic and fungal diseases
Edited by Gero Steinberg
For a complete overview see the Issue and the Editorial
Available online 28th September 2016
http://dx.doi.org/10.1016/j.mib.2016.08.006
1369-5274/© 2016 The Authors. Published by Elsevier Ltd. This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/).
Introduction
Candida albicans is the commonest serious fungal pathogen of humans, variously reported as causing between 250 000 and 400 000 deaths per annum worldwide as well as extensive morbidity of around 100 million episodes of recurrent vaginitis [1•, 2]. This fungus is a classical opportunistic pathogen residing harmlessly as a commensal in approximately 50% of individuals [1•], kept in check by our immune system and a protective bacterial microbiome of the gut and other mucosal surfaces [2, 3, 4]. In this review we survey latest advances in the cell biology of C. albicans that underpins its ecology as an organism exploring the interface between commensalism and pathogenesis.
Life as a successful saprophyte
C. albicans is a largely asexual fungus, but never-the-less it is morphologically and physiologically a highly variable and adaptable fungus. It is pleomorphic — being able to grow either as a budding yeast, or as a pseudomycelium of elongated and conjoined yeast cells or as true hyphae formed of generate parallel-sided tip-growing filaments [5]. It also exhibits a non-sexual form of variation called phenotypic switching that can generate stable cell and colony variants with distinct properties [6]. C. albicans can thrive in different host niches (gut, vagina, oral mucosa, skin) without causing disease. This observation suggests it is adapted for commensalism. GI tract colonization seems to involve predominantly carriage of the yeast form of the fungus, and low level systemic dissemination in the gut can occur even in yeast-locked mutants [7]. However, a mouse model of stable gastrointestinal candidiasis demonstrated that passage of C. albicans through the mammalian gut leads to the transition to a modified yeast cell, ‘GUT phenotype’ (gastrointestinally induced transition), that expresses a specialised transcriptome in the digestive tract to promote assimilation of common nutrients in the bowel. These GUT cells are morphologically altered and suppress the propensity for tissue invasion and the expression of certain virulence traits [8••]. Therefore, the commensal state does not solely depend on host immune status and is also supported by organism-specific adaptations mediated by transcriptional changes in the host-associated commensal state [9].
Changes in the availability of nutrients in the gut due to dietary intake, can further impact the abundance of Candida [10], and changes in diet or gut fungal microbiota may lead to dysbiosis and inflammatory pathologies such as Crohn's disease [11, 12]. Although Candida colonisation may promote gut inflammation under certain circumstances, chitin, a component of the Candida cell wall, has anti-inflammatory properties and has the potential to ameliorate inflammatory bowel disease (IBD) if exposed in the gut [13]. Also host mutations in, for example, fungal immune recognition receptors such as dectin-1, the immune signalling molecule CARD9 and the inflammatory cytokine IL-22 result in susceptibility to colitis and other forms of IBD [14, 15]. In a mouse model, tryptophan metabolites from some specific members of the gut microbiome were shown to be able to suppress C. albicans colonisation by controlling secretion of IL-22 in stomach [16]. Probiotic supplements are also known to suppress the fungal mycobiome [17]. Therefore the commensal status of Candida is also related to the host microbiome as a whole and the immune status of the host.
Collectively, these observations suggest that gut commensalism of Candida is related to both intrinsic factors (fungal gene regulation, cell morphology, adaptation, fungal burden) and extrinsic factors (competitive microbiome, diet, host immune status). We know less about the factors affecting colonisation at other body sites although it is likely that a similar complex array of factors sustain the commensal state in these host niches.
Life as a successful pathogen
During the course of infection C. albicans colonizes various host niches, with differences, for example, in nutrient availability, pH, hypoxia and CO2 levels [18, 19]. One of the key features establishing C. albicans as a successful pathogen is its adaptability to successfully thrive in these different conditions [18]. Host microenvironments have heterogeneous carbon sources and, as it traverses through different host niches, C. albicans can adapt to use alternative carbon sources simultaneously, for its survival and virulence [18, 19, 20]. This adaptation has resulted from the absence of catabolite inactivation due to the rewiring of ubiquitination sites in metabolic enzymes [21•, 22]. The metabolic flexibility of Candida also contributes to the alterations in the cellular proteome and secretome [23], and its ability to undergo yeast to hyphal transition, white-opaque switching [24], biofilm formation, as well as its adhesion characteristics [23, 25], and the capacity for cell wall remodelling [19, 20, 23, 26]. Changes in cell wall polysaccharide composition [19, 20, 25], modifies the pathogen's sensitivity to environmental stress and antifungals [18, 20, 23, 25], but also affect its immunogenicity by altering the expression and presentation of critical pathogen-associated molecular patterns (PAMPs), thus making C. albicans a moving target for the recognition by the host immune system [19, 20, 21•, 25, 26, 27].
The human host withholds the availability of micronutrients, like Fe, Zn, Cu and Mn, from the pathogen in a process termed ‘nutritional immunity’ [28]. These micronutrients are essential for many vital cellular functions in the pathogen [28]. Countering this, C. albicans has evolved mechanisms to overcome host nutritional immunity by expressing micronutrient transporters (e.g. Rbt5/Als3 for Fe; Zrt1/Zrt2/soluble Pra1 for Zn) [28], or redundant enzymes that use alternative micronutrients as cofactors [29].
C. albicans expresses a number of proteases, phospholipases, lipases and esterases (reviewed in [30]), which function in the degradation of host connective tissues, cleavage of host immune defence proteins, and thus aid nutrition acquisition, invasion and evasion of the pathogen from host immune defence [30, 31]. These hydrolases belong to multigene families, and each family member has a different substrate specificity, pH optimum, and expression profile [30]. Of these the secreted aspartyl proteases (Saps) have been shown to have important multiple roles. Regulation of the expression of this 10-membered gene family is regulated principally by host carbon and nitrogen sources and by pH [32]. Sap2 inactivates Factor-H and the complement receptors CR3 and CR4 on macrophages, thus mediating the escape of C. albicans from recognition by the host's innate immune system [33]. In mice, Anti-Sap2 antibodies or the protease inhibitor pepstatin A can reduce Sap2-mediated vaginal inflammation caused by C. albicans [34]. Sap2 and Sap6 have also been shown to induce inflammatory cytokine production by the host through the type I IFN, and caspase-11 induction as well as NLRP3 inflammasome activation [35, 36]. Following their uptake by the host epithelial cells, hypha-specific Saps4-6 cause lysosomal permeabilization and triggering of caspase-1 dependent apoptosis [37].
Recently, an entirely novel secretory host cell lysing agent from C. albicans, called ‘candidalysin’, has been described. The lytic activity is encoded by one of eight Kexp-processed peptides from the ECE1 gene product. The Ece1-III62–93 peptide alone can induce damage to epithelial membranes and the activation of a danger response in host epithelial immunity [38••].
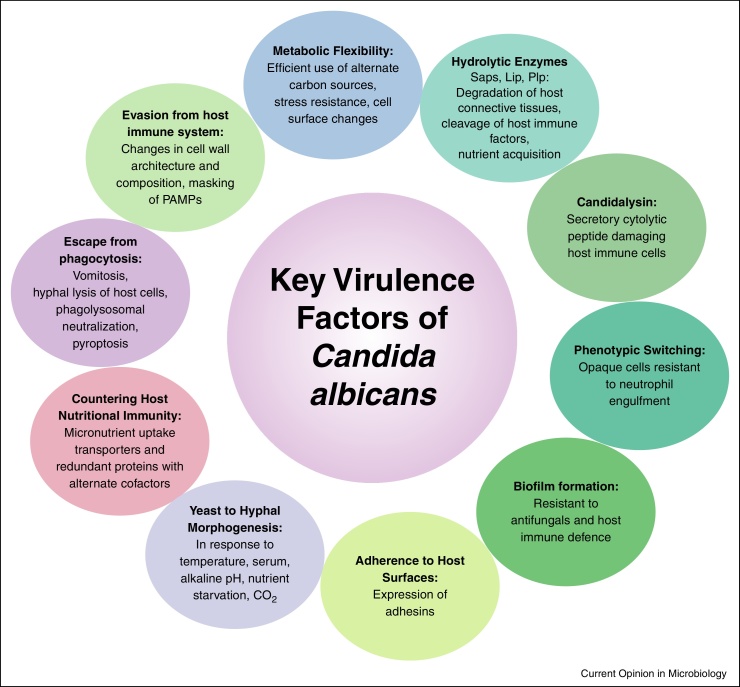
These evolutionary adaptive traits enable C. albicans to survive in various host niches, counter host immune defences and help C. albicans in establishing itself as a successful pathogen (Figure 1).
Figure 1.
Candida virulence factors. Virulence is a polygenic trait in C. albicans involving biochemical, physiological, genetic and morphogenetic characteristics.
Controlling interactions with human epithelia and endothelia
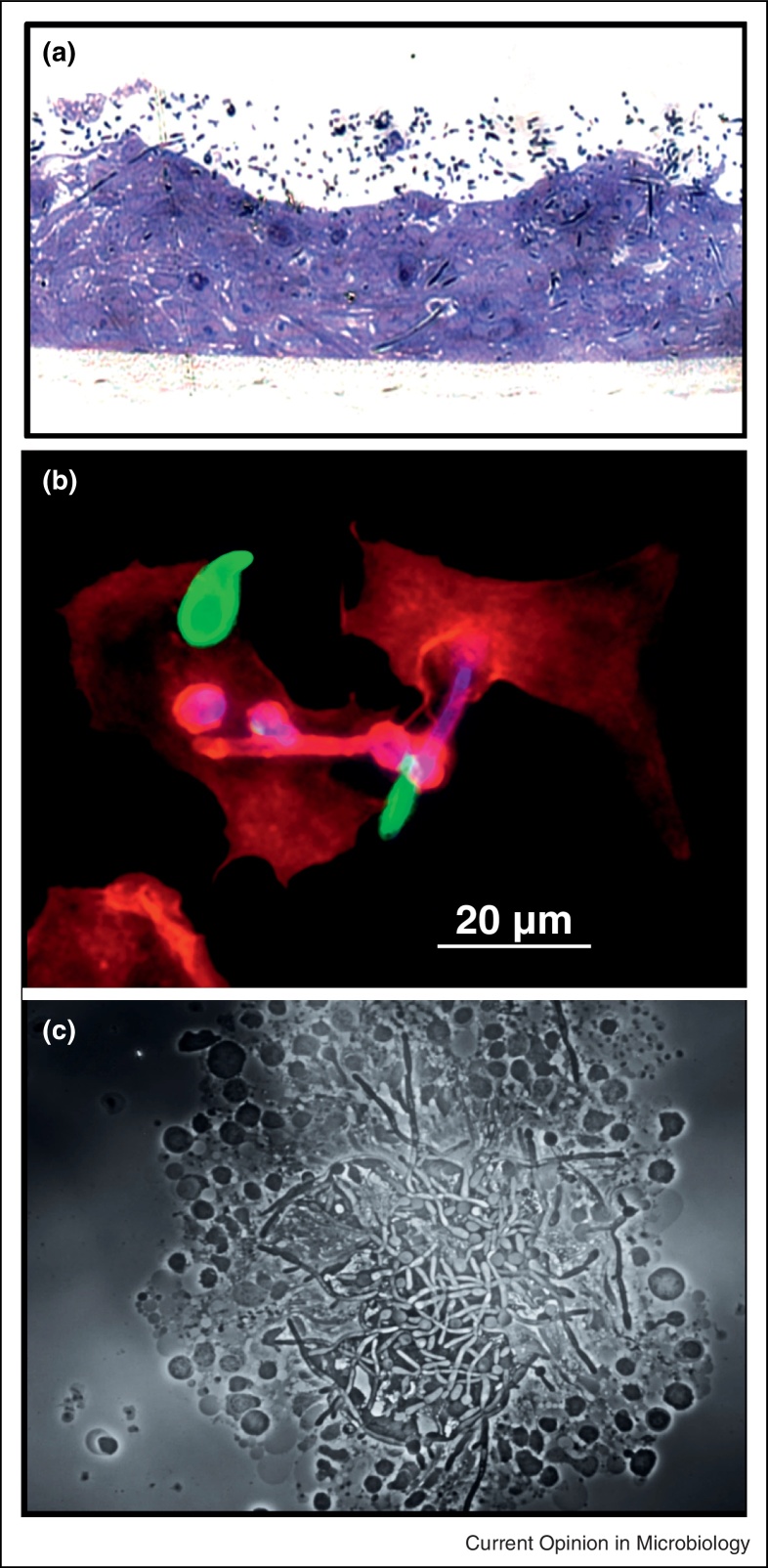
Two complementary mechanisms are involved in C. albicans host cell invasion through epithelial cells (EC) (Figure 3). Fungal-induced endocytosis contributes to the early stages of invasion, a process of host produced pseudopods surrounding the fungus to pull it into the host cell. By contrast, active penetration occurs at later time points when hyphae invade between or through ECs [39]. Although the mechanisms involved depend on invasion stage, fungal morphology and epithelial lineage, both are triggered by hypha-associated factors [40]. Notably, systemic dissemination, which is not dependent on morphological transition, occurs from the GI tract and trans-epithelial transport of the yeast form might be mediated by indirect mechanisms, such as by lumen sampling dendritic cells or M cell transcytosis [7].
Figure 3.
C. albicans interaction with host cells. [a] I invasion into oral epithelium with hyphae that have penetrated the host cells marked (*). [b] Phagocytosis by mouse peritoneal macrophages with extracellular parts of C. albicans stained with an anti-Candida Ab in green and counterstained with CFW in blue. The macrophages are stained red with phalloidin (F-actin) to visualize phagocytic uptake. [c] Human peripheral blood mononuclear cells aggregated around yeast cells and hyphae of C. albicans.
Both the oral and vaginal epithelial immune response differs to the presence of hyphae and yeast cells of C. albicans so that only large numbers of hyphae activate a host biphasic MKP1 and c-Fos dependent response leading to inflammatory cytokine formation [41]. This may allow the epithelium to control the pattern of immune activation so it is responsive mainly to fungal invasion rather than colonisation. Low level colonisation, may progress to the establishment of a mature surface biofilm, but as yet it is not clear how the establishment of a Candida biofilm may affect mucosal infection and immunity [42]. However, it would seem likely that mature biofilms would present challenges for the cellular immune system to clear such dense biomass mats.
Multiple stimuli including EC contact and body temperature trigger hyphal morphogenesis. C. albicans produces early virulence factors that are downstream of the process of invasion itself [43]. These include the expression of the GPI-linked cell surface proteins Hwp1 and the invasin Als3 or Ssa1, a member of HSP70 family [40]. Hwp1, under control of the transcription factor Bcr1 regulating biofilm formation, acts as a substrate for epithelial transglutaminases and is required for mucosal pathogenicity [39]. Als3 and Ssa1 mediate binding to host epithelial surface receptors which enable the fungus to attach to and invade host cells. Host ligands include E-cadherin on ECs, N-cadherin on endothelial cells and EGF receptor on oral ECs [40]. During induced endocytosis this interaction stimulates host cytoplasmic proteins to form clathrin-coated vesicles surrounding the fungus for an actin dependent internalization. E-cadherin interaction is however not necessary for endocytosis of C. albicans into enterocytes [44]. Recently it has been shown that C. albicans Als adhesins are also involved in adhesion to C. glabrata during oropharyngeal candidiasis (OPC) enabling C. glabrata to colonize and persist in the oral mucosa and cavity [45•].
During active penetration, C. albicans secretes hydrolytic enzymes (described in previous section) that affect epithelial cell–cell junctions and facilitate degradation of cell membrane components along with other ligands that facilitate fungal adhesion [39]. Cell surface localized superoxide dismutase detoxifies reactive oxygen species (ROS) produced when tissue is damaged and is also expressed on the surface of invading hyphae [46, 47].
Many other internal and cell wall-associated proteins also indirectly affect C. albicans adhesion and virulence, for example, proteins involved in protein trafficking and required for a functional vesicle transport system or proteins involved in hyphal formation, growth or cellular orientation. Others have a crucial role in cell wall assembly and integrity, or they modify other adhesins required for epithelial binding [39].
Interactions with phagocytes
Almost every component of the cell wall of Candida has been shown to have a role in the interactions between host and pathogen. Immune recognition of Candida is mediated by PAMP engagement with host pattern recognition receptors (PRRs). These recognition events are dominated by binding of fungal cell wall carbohydrates, although the cell wall proteins also contribute to shaping the immune response [3, 4]. Recently it has become clear that the innate immune response, which is of principle importance in conferring immunity, can be trained by prior exposure to Candida. As a consequence memory of prior innate immune interactions is epigenetically imprinted in the host and results in enhanced immune responses in subsequent encounters with the fungus. The paradigm of immunological memory was thought previously to be encoded entirely by the adaptive immune system but is clearly also a feature of innate immunity [48••, 49].
It is also increasingly evident that the immune response to Candida is influenced by yeast-hypha morphogenesis [50]. Hyphae specifically activate the NLRP3 inflammasome resulting in IL-1β secretion [51] and yeast and hyphae are differentially bound to, taken up and processed by phagocytes [3]. In addition, other morphological transitions, such as the switching from the white to the opaque form of this organism results in differential phagocytosis and the suppression of the production of phagocyte chemoattractants [52, 53].
Resisting phagocytes
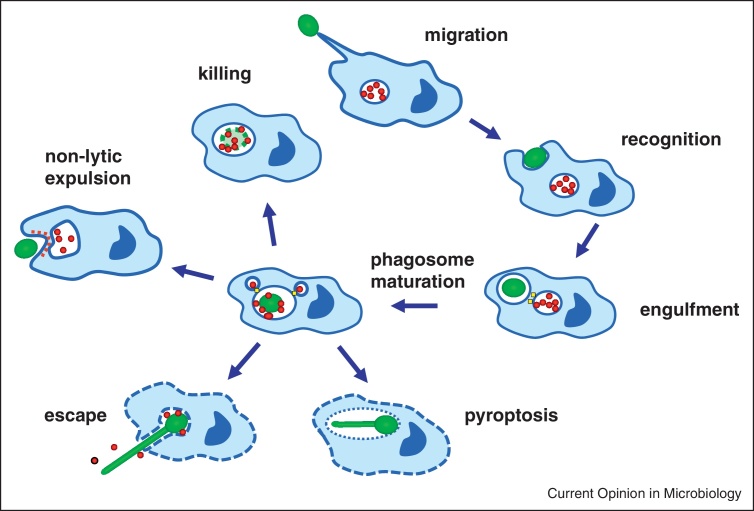
Following internalisation of the fungal target cell, maturation of the phagosome into phagolysosome is fundamental to fungal killing. The importance of phagolysosomes in promoting fungal killing is associated with the presence of cationic peptides, hydrolytic enzymes, ROS and reactive nitrogen species (RNS); which are generated in a vacuole with an acidic pH [3, 54]. Hence, in order to survive the harmful environment of the phagolysosome, C. albicans has developed strategies to allow its survival by the manipulation and escape from phagocytic cells (Figure 2, Figure 3) [54, 59].
Figure 2.
Interaction of C. albicans with macrophages showing the stages at which the fungus can deploy immune avoidance mechanisms. The macrophage uses chemotaxis to target the fungal cell, then fungus recognition and engulfment take place via interaction of fungal PAMPs and a series of immune cell PRRs that includes phagocytic receptors. The Candida cell is delivered to the phagosomal vesicle which undergoes fusion with lysosomes to create the mature acidic phagolysosome that can kill the fungal cargo using oxidative and nitrosative elements. However, C. albicans has the capacity to interfere with the phagolysomal maturation programme, increase its alkalinity, generate protective antioxidants and induce its own non-lytic expulsion. In addition, hypha formation and induced pyroptosis can cause the lysis of the phagocyte.
C. albicans promotes neutralization of the phagolysosome, in a process that requires the Stp2 transcription factor induction of the Ato5-mediated ammonia exporter [55, 56•]. The subsequent neutralization of the acidic environment of the phagolysosome allows C. albicans hyphal morphogenesis to occur hence facilitating its escape from macrophages [55, 56•]. In addition, the PKC-Mkc1-Rlm1 cell wall salvage pathway is also activated resulting in reinforcing chitin being made in the cell wall [57, 58].
When inside the phagosome Candida also induces a battery of protective enzymes and proteins including catalase, superoxide dismutase, thioredoxin, flavo-haemoglobin, glutathione recycling enzymes that degrade or scavenge RNS and ROS [47, 60]. Consequently, deletion of key regulators of oxidative and nitrosative stress response results in increased sensitivity to phagocyte killing [47, 60]. Multiple individual imposed toxic stresses have been shown to exert synergistic effects on the ability to kill Candida. These studies illustrate the importance of the Hog1 MAPK and the Cap1 transcription factor in the regulation of combinatorial stress responses [60, 61].
Candida cells share a property with Cryptococcus and other fungi to be able to induce their own non-lytic expulsion from macrophages (sometimes called vomocytosis), without any damage to the phagocyte [62]. By contrast, numerous studies have reported the ability of elongating hyphae to pierce the membrane of a macrophage resulting in their release [3]. However, there is no clear relation between yeast-hypha morphogenesis and macrophage lysis.
It is now clear that Candida hyphal cells can also induce pyroptosis in the host phagocyte — a form of programmed cell death that is dependent on caspase-1 activation of the NLRP3 inflammasome [63, 64, 65, 66]. However, although hyphae promote pyroptosis, pyroptosis is not always coincident with hypha formation. For example, a vps35 mutant formed hyphae normally but failed to induce macrophage lysis whilst, alg1 and alg11 mutants are hypha-deficient yet induced macrophage lysis via pyroptosis [67••].
Therefore the cell biology of Candida is well adapted to resist the killing potential of phagocytes thereby limiting the effectiveness of some elements of the adaptive immune system.
Conclusion
C. albicans has numerous cell biology attributes that enable it to exist commensally in the human body. These features presumably account for the fact that most healthy humans are colonised by this organism. However, its metabolic, morphogenetic and immunomodulatory properties means that it is also a pernicious and common pathogen in almost any setting in which immune vigour is compromised or the physical integrity of the host surface is disrupted. As a commensal organism Candida has likely acquired traits and properties that also enable it to flourish as a pathogen [68]. Commensal cells also have to avoid being eliminated by overcoming immune surveillance mechanisms that act to protect the mucosa. This organism can therefore ‘have its cake and eat it’ by withholding its full pathogenic potential under conditions of host immune fitness or aggressively invading the weakened host. In both situations this fungus shows remarkable flexibility and adaptability in its capacity for survival in the human body.
References and recommended reading
Papers of particular interest, published within the period of review, have been highlighted as:
• of special interest
•• of outstanding interest
Acknowledgements
The authors are supported by the Wellcome Trust via a Senior Investigator Award to NG, an ISST award and a Wellcome Trust Strategic Award in Medical Mycology and Fungal Immunology. The authors are also part of the MRC Centre for Medical Mycology at Aberdeen.
References
- 1•.Kullberg B.J., Arendrup M.C. Invasive Candidiasis. N Engl J Med. 2015;373:1445–1456. doi: 10.1056/NEJMra1315399. [DOI] [PubMed] [Google Scholar]; An excellent overview of the pathobiology and medical mycology of Candida invections.
- 2.Brown G.D., Denning D.W., Gow N.A.R., Levitz S.M., Netea M.G., White T.C. Hidden killers: human fungal infections. Sci Transl Med. 2012;4:165rv13. doi: 10.1126/scitranslmed.3004404. [DOI] [PubMed] [Google Scholar]
- 3.Erwig L.P., Gow N.A.R. Interactions of fungal pathogens with phagocytes. Nat Rev Microbiol. 2016;14:163–176. doi: 10.1038/nrmicro.2015.21. [DOI] [PubMed] [Google Scholar]
- 4.Sudbery P.E. Growth of Candida albicans hyphae. Nat Rev Immunol. 2011;9:737–748. doi: 10.1038/nrmicro2636. [DOI] [PubMed] [Google Scholar]
- 5.Soll D.R. The role of phenotypic switching in the basic biology and pathogenesis of Candida albicans. J Oral Microbiol. 2014;6:22993. doi: 10.3402/jom.v6.22993. http://dx.doi.org/10.3402/jom.v6.22993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Netea M.G., Joosten L.A.B., van der Meer J.W.M., Kullberg B.-J., van de Veerdonk F.L. Immune defence against Candida fungal infections. Nat Rev Immunol. 2015;15:630–642. doi: 10.1038/nri3897. [DOI] [PubMed] [Google Scholar]
- 7.Vautier S., Drummond R.A., Chen K., Murray G.I., Kadosh D., Brown A.J.P., Gow N.A.R., MacCallum D.M., Kolls J.K., Brown G.D. Candida albicans colonization and dissemination from the murine gastrointestinal tract: the influence of morphology and Th17 immunity. Cell Microbiol. 2015;17:445–450. doi: 10.1111/cmi.12388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8••.Pande K., Chen C., Noble S.M. Passage through the mammalian gut triggers a phenotypic switch that promotes Candida albicans commensalism. Nat Genet. 2013;45:1088–1091. doi: 10.1038/ng.2710. [DOI] [PMC free article] [PubMed] [Google Scholar]; In this paper the authors describe a new (GUT) phenotype for C. albicans which is adapted for growth in the commensal state in the intestine.
- 9.Neville B.A., d’Enfert C., Bougnoux M.-E. Candida albicans commensalism in the gastrointestinal tract. FEMS Yeast Res. 2015:15. doi: 10.1093/femsyr/fov081. [DOI] [PubMed] [Google Scholar]
- 10.Yamaguchi N., Sonoyama K., Kikuchi H., Nagura T., Aritsuka T., Kawabata J. Gastric colonization of Candida albicans differs in mice fed commercial and purified diets. J Nutr. 2005;135:109–115. doi: 10.1093/jn/135.1.109. [DOI] [PubMed] [Google Scholar]
- 11.Sokol H., Leducq V., Aschard H., Pham H.-P., Jegou S., Landman C., Cohen D., Liguori G., Bourrier A., Nion-Larmurier I. Fungal microbiota dysbiosis in IBD. Gut. 2016 doi: 10.1136/gutjnl-2015-310746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Li Q., Wang C., Tang C., He Q., Li N., Li J. Dysbiosis of gut fungal microbiota is associated with mucosal inflammation in Crohn's disease. J Clin Gastroenterol. 2014;48:513–523. doi: 10.1097/MCG.0000000000000035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wagener J., Malireddi R.K.S., Lenardon M.D., Köberle M., Vautier S., MacCallum D.M., Biedermann T., Schaller M., Netea M.G., Kanneganti T.-D. Fungal chitin dampens inflammation through IL-10 induction mediated by NOD2 and TLR9 activation. PLoS Pathog. 2014;10:e1004050. doi: 10.1371/journal.ppat.1004050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Iliev I.D., Funari V.A., Taylor K.D., Nguyen Q., Reyes C.N., Strom S.P., Brown J., Becker C.A., Fleshner P.R., Dubinsky M. Interactions between commensal fungi and the C-type lectin receptor Dectin-1 influence colitis. Science. 2012;336:1314–1317. doi: 10.1126/science.1221789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Underhill D.M., Iliev I.D. The mycobiota: interactions between commensal fungi and the host immune system. Nat Rev Immunol. 2014;14:405–416. doi: 10.1038/nri3684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zelante T., Iannitti R.G., Cunha C., De Luca A., Giovannini G., Pieraccini G., Zecchi R., D’Angelo C., Massi-Benedetti C., Fallarino F. Tryptophan catabolites from microbiota engage aryl hydrocarbon receptor and balance mucosal reactivity via interleukin-22. Immunity. 2013;39:372–385. doi: 10.1016/j.immuni.2013.08.003. [DOI] [PubMed] [Google Scholar]
- 17.Kumar S., Bansal A., Chakrabarti A., Singhi S. Evaluation of efficacy of probiotics in prevention of candida colonization in a PICU — a randomized controlled trial. Crit Care Med. 2013;41:565–572. doi: 10.1097/CCM.0b013e31826a409c. [DOI] [PubMed] [Google Scholar]
- 18.Brown A.J.P., Budge S., Kaloriti D., Tillmann A., Jacobsen M.D., Yin Z., Ene I.V., Bohovych I., Sandai D., Kastora S. Stress adaptation in a pathogenic fungus. J Exp Biol. 2014;217:144–155. doi: 10.1242/jeb.088930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hall R.A. Dressed to impress: impact of environmental adaptation on the Candida albicans cell wall. Mol Microbiol. 2015;97:7–17. doi: 10.1111/mmi.13020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Brown A.J.P., Brown G.D., Netea M.G., Gow N.A.R. Metabolism impacts upon Candida immunogenicity and pathogenicity at multiple levels. Trends Microbiol. 2014;22:614–622. doi: 10.1016/j.tim.2014.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21•.Childers D.S., Raziunaite I., Mol Avelar G., Mackie J., Budge S., Stead D., Gow N.A.R., Lenardon M.D., Ballou E.R., MacCallum D.M. The rewiring of ubiquitination targets in a pathogenic yeast promotes metabolic flexibility, host colonization and virulence. PLoS Pathog. 2016;12:e1005566. doi: 10.1371/journal.ppat.1005566. [DOI] [PMC free article] [PubMed] [Google Scholar]; In this paper the authors show that in C. albicans certain enzymes, that are subject to catabolite repression in Saccharomyces are expressed under a broader range of environmental conditions thus allowing the fungus to metabolise a wide range of nutrients at the same time.
- 22.Sandai D., Yin Z., Selway L., Stead D., Walker J., Leach M.D., Bohovych I., Ene I.V., Kastora S., Budge S. The evolutionary rewiring of ubiquitination targets has reprogrammed the regulation of carbon assimilation in the pathogenic yeast Candida albicans. mBio. 2012:3. doi: 10.1128/mBio.00495-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ene I.V., Heilmann C.J., Sorgo A.G., Walker L.A., de Koster C.G., Munro C.A., Klis F.M., Brown A.J.P. Carbon source-induced reprogramming of the cell wall proteome and secretome modulates the adherence and drug resistance of the fungal pathogen Candida albicans. Proteomics. 2012;12:3164–3179. doi: 10.1002/pmic.201200228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lan C.-Y., Newport G., Murillo L.A., Jones T., Scherer S., Davis R.W., Agabian N. Metabolic specialization associated with phenotypic switching in Candida albicans. Proc Natl Acad Sci U S A. 2002;99:14907–14912. doi: 10.1073/pnas.232566499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ene I.V., Adya A.K., Wehmeier S., Brand A.C., MacCallum D.M., Gow N.A.R., Brown A.J.P. Host carbon sources modulate cell wall architecture, drug resistance and virulence in a fungal pathogen. Cell Microbiol. 2012;14:1319–1335. doi: 10.1111/j.1462-5822.2012.01813.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lewis L.E., Bain J.M., Lowes C., Gillespie C., Rudkin F.M., Gow N.A.R., Erwig L.-P. Stage specific assessment of Candida albicans phagocytosis by macrophages identifies cell wall composition and morphogenesis as key determinants. PLoS Pathog. 2012;8:e1002578. doi: 10.1371/journal.ppat.1002578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hall R.A., Gow N.A.R. Mannosylation in Candida albicans: role in cell wall function and immune recognition. Mol Microbiol. 2013;90:1147–1161. doi: 10.1111/mmi.12426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Crawford A., Wilson D. Essential metals at the host–pathogen interface: nutritional immunity and micronutrient assimilation by human fungal pathogens. FEMS Yeast Res. 2015:15. doi: 10.1093/femsyr/fov071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Li C.X., Gleason J.E., Zhang S.X., Bruno V.M., Cormack B.P., Culotta V.C. Candida albicans adapts to host copper during infection by swapping metal cofactors for superoxide dismutase. Proc Natl Acad Sci U S A. 2015;112:E5336–E5342. doi: 10.1073/pnas.1513447112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Schaller M., Borelli C., Korting H.C., Hube B. Hydrolytic enzymes as virulence factors of Candida albicans. Mycoses. 2005;48:365–377. doi: 10.1111/j.1439-0507.2005.01165.x. [DOI] [PubMed] [Google Scholar]
- 31.Gropp K., Schild L., Schindler S., Hube B., Zipfel P.F., Skerka C. The yeast Candida albicans evades human complement attack by secretion of aspartic proteases. Mol Immunol. 2009;47:465–475. doi: 10.1016/j.molimm.2009.08.019. [DOI] [PubMed] [Google Scholar]
- 32.Hube B., Monod M., Schofield D.A., Brown A.J., Gow N.A. Expression of seven members of the gene family encoding secretory aspartyl proteinases in Candida albicans. Mol Microbiol. 1994;14:87–99. doi: 10.1111/j.1365-2958.1994.tb01269.x. [DOI] [PubMed] [Google Scholar]
- 33.Svoboda E., Schneider A.E., Sándor N., Lermann U., Staib P., Kremlitzka M., Bajtay Z., Barz D., Erdei A., Józsi M. Secreted aspartic protease 2 of Candida albicans inactivates factor H and the macrophage factor H-receptors CR3 (CD11b/CD18) and CR4 (CD11c/CD18) Immunol Lett. 2015;168:13–21. doi: 10.1016/j.imlet.2015.08.009. [DOI] [PubMed] [Google Scholar]
- 34.Pericolini E., Gabrielli E., Amacker M., Kasper L., Roselletti E., Luciano E., Sabbatini S., Kaeser M., Moser C., Hube B. Secretory aspartyl proteinases cause vaginitis and can mediate vaginitis caused by Candida albicans in mice. mBio. 2015;6:e00724. doi: 10.1128/mBio.00724-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pietrella D., Pandey N., Gabrielli E., Pericolini E., Perito S., Kasper L., Bistoni F., Cassone A., Hube B., Vecchiarelli A. Secreted aspartic proteases of Candida albicans activate the NLRP3 inflammasome. Eur J Immunol. 2013;43:679–692. doi: 10.1002/eji.201242691. [DOI] [PubMed] [Google Scholar]
- 36.Gabrielli E., Pericolini E., Luciano E., Sabbatini S., Roselletti E., Perito S., Kasper L., Hube B., Vecchiarelli A. Induction of caspase-11 by aspartyl proteinases of Candida albicans and implication in promoting inflammatory response. Infect Immun. 2015;83:1940–1948. doi: 10.1128/IAI.02895-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wu H., Downs D., Ghosh K., Ghosh A.K., Staib P., Monod M., Tang J. Candida albicans secreted aspartic proteases 4-6 induce apoptosis of epithelial cells by a novel Trojan horse mechanism. FASEB J Off Publ Fed Am Soc Exp Biol. 2013;27:2132–2144. doi: 10.1096/fj.12-214353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38••.Moyes D.L., Wilson D., Richardson J.P., Mogavero S., Tang S.X., Wernecke J., Höfs S., Gratacap R.L., Robbins J., Runglall M. Candidalysin is a fungal peptide toxin critical for mucosal infection. Nature. 2016;532:64–68. doi: 10.1038/nature17625. [DOI] [PMC free article] [PubMed] [Google Scholar]; The first report of a toxin produced by Candida species. This lysin is the product of proteolysis of the Ece1 protein and damages mucosal surfaces and activates epithelial immunity.
- 39.Naglik J.R., Moyes D.L., Wächtler B., Hube B. Candida albicans interactions with epithelial cells and mucosal immunity. Microbes Infect Inst Pasteur. 2011;13:963–976. doi: 10.1016/j.micinf.2011.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Yang W., Yan L., Wu C., Zhao X., Tang J. Fungal invasion of epithelial cells. Microbiol Res. 2014;169:803–810. doi: 10.1016/j.micres.2014.02.013. [DOI] [PubMed] [Google Scholar]
- 41.Moyes D.L., Runglall M., Murciano C., Shen C., Nayar D., Thavaraj S., Kohli A., Islam A., Mora-Montes H., Challacombe S.J., Naglik J.R. A biphasic innate immune MAPK response discriminates between the yeast and hyphal forms of Candida albicans in epithelial cells. Cell Host Microbe. 2010;8:225–235. doi: 10.1016/j.chom.2010.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Nobile C.J., Johnson A.J. Candida albicans biofilms and human disease. Annu Rev Microbiol. 2015;69:71–92. doi: 10.1146/annurev-micro-091014-104330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Jacobsen I.D., Wilson D., Wächtler B., Brunke S., Naglik J.R., Hube B. Candida albicans dimorphism as a therapeutic target. Expert Rev Anti Infect Ther. 2012;10:85–93. doi: 10.1586/eri.11.152. [DOI] [PubMed] [Google Scholar]
- 44.Goyer M., Loiselet A., Bon F., L’Ollivier C., Laue M., Holland G., Bonnin A., Dalle F. Intestinal cell tight junctions limit invasion of Candida albicans through active penetration and endocytosis in the early stages of the interaction of the fungus with the intestinal barrier. PloS One. 2016;11:e0149159. doi: 10.1371/journal.pone.0149159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45•.Tati S., Davidow P., McCall A., Hwang-Wong E., Rojas I.G., Cormack B., Edgerton M. Candida glabrata binding to Candida albicans hyphae enables its development in oropharyngeal Candidiasis. PLoS Pathog. 2016;12:e1005522. doi: 10.1371/journal.ppat.1005522. [DOI] [PMC free article] [PubMed] [Google Scholar]; Here it is shown for the first time that Candida hyphae act as a substrate to anchor a second Candida species to the oral mucosa.
- 46.Frohner I.E., Bourgeois C., Yatsyk K., Majer O., Kuchler K: Candida albicans cell surface superoxide dismutases degrade host-derived reactive oxygen species to escape innate immune surveillance. Mol Microbiol. 2009;71:240–252. doi: 10.1111/j.1365-2958.2008.06528.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Dantas A., da S., Day A., Ikeh M., Kos I., Achan B., Quinn J. Oxidative stress responses in the human fungal pathogen, Candida albicans. Biomolecules. 2015;5:142–165. doi: 10.3390/biom5010142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48••.Quintin J., Saeed S., Martens J.H.A., Giamarellos-Bourboulis E.J., Ifrim D.C., Logie C., Jacobs L., Jansen T., Kullberg B.-J., Wijmenga C. Candida albicans infection affords protection against reinfection via functional reprogramming of monocytes. Cell Host Microbe. 2012;12:223–232. doi: 10.1016/j.chom.2012.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]; A landmark paper showing that prior exposure of the immune system to Candida potentiates subsequent immune responses suggesting that the innate immune system has memory.
- 49.Saeed S., Quintin J., Kerstens H.H.D., Rao N.A., Aghajanirefah A., Matarese F., Cheng S.-C., Ratter J., Berentsen K., van der Ent M.A. Epigenetic programming of monocyte-to-macrophage differentiation and trained innate immunity. Science. 2014;345:1251086. doi: 10.1126/science.1251086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Gow N.A.R., van de Veerdonk F.L., Brown A.J.P., Netea M.G. Candida albicans morphogenesis and host defence: discriminating invasion from colonization. Nat Rev Microbiol. 2012;10:112–122. doi: 10.1038/nrmicro2711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Joly S., Ma N., Sadler J.J., Soll D.R., Cassel S.L., Sutterwala F.S. Cutting edge: Candida albicans hyphae formation triggers activation of the Nlrp3 inflammasome. J Immunol Baltim Md 1950. 2009;183:3578–3581. doi: 10.4049/jimmunol.0901323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Geiger J., Wessels D., Lockhart S.R., Soll D.R. Release of a potent polymorphonuclear leukocyte chemoattractant is regulated by white-opaque switching in Candida albicans. Infect Immun. 2004;72:667–677. doi: 10.1128/IAI.72.2.667-677.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Lohse M.B., Johnson A.D. Differential phagocytosis of white versus opaque Candida albicans by Drosophila and mouse phagocytes. PloS One. 2008;3:e1473. doi: 10.1371/journal.pone.0001473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Miramón P., Kasper L., Hube B. Thriving within the host: Candida spp. interactions with phagocytic cells. Med Microbiol Immunol (Berl) 2013;202:183–195. doi: 10.1007/s00430-013-0288-z. [DOI] [PubMed] [Google Scholar]
- 55.Vylkova S., Lorenz M.C. Modulation of phagosomal pH by Candida albicans promotes hyphal morphogenesis and requires Stp2p, a regulator of amino acid transport. PLoS Pathog. 2014;10:e1003995. doi: 10.1371/journal.ppat.1003995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56•.Danhof H.A., Lorenz M.C. The Candida albicans ATO gene family promotes neutralization of the macrophage phagolysosome. Infect Immun. 2015;83:4416–4426. doi: 10.1128/IAI.00984-15. [DOI] [PMC free article] [PubMed] [Google Scholar]; Here the mechanism is shown how Candida prevents the acidification of the phagolysosome thus enabling hypha formation to occur within a macrohage.
- 57.Munro C.A., Selvaggini S., de Bruijn I., Walker L., Lenardon M.D., Gerssen B., Milne S., Brown A.J.P., Gow N.A.R. The PKC, HOG and Ca2+ signalling pathways co-ordinately regulate chitin synthesis in Candida albicans. Mol Microbiol. 2007;63:1399–1413. doi: 10.1111/j.1365-2958.2007.05588.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Delgado-Silva Y., Vaz C., Carvalho-Pereira J., Carneiro C., Nogueira E., Correia A., Carreto L., Silva S., Faustino A., Pais C. Participation of Candida albicans transcription factor RLM1 in cell wall biogenesis and virulence. PloS One. 2014;9:e86270. doi: 10.1371/journal.pone.0086270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Miramón P., Dunker C., Windecker H., Bohovych I.M., Brown A.J.P., Kurzai O., Hube B. Cellular responses of Candida albicans to phagocytosis and the extracellular activities of neutrophils are critical to counteract carbohydrate starvation, oxidative and nitrosative stress. PloS One. 2012;7:e52850. doi: 10.1371/journal.pone.0052850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Kaloriti D., Jacobsen M., Yin Z., Patterson M., Tillmann A., Smith D.A., Cook E., You T., Grimm M.J., Bohovych I. Mechanisms underlying the exquisite sensitivity of Candida albicans to combinatorial cationic and oxidative stress that enhances the potent fungicidal activity of phagocytes. mBio. 2014;5 doi: 10.1128/mBio.01334-14. e01334-1314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Kos I., Patterson M.J., Znaidi S., Kaloriti D., da Silva Dantas A., Herrero-de-Dios C.M., d’Enfert C., Brown A.J.P., Quinn J. Mechanisms underlying the delayed activation of the Cap1 transcription factor in Candida albicans following combinatorial oxidative and cationic stress important for phagocytic potency. mBio. 2016:7. doi: 10.1128/mBio.00331-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Bain J.M., Lewis L.E., Okai B., Quinn J., Gow N.A.R., Erwig L.-P. Non-lytic expulsion/exocytosis of Candida albicans from macrophages. Fungal Genet Biol. 2012;49:677–678. doi: 10.1016/j.fgb.2012.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Joly S., Eisenbarth S.C., Olivier A.K., Williams A., Kaplan D.H., Cassel S.L., Flavell R.A., Sutterwala F.S. Cutting edge: Nlrp10 is essential for protective antifungal adaptive immunity against Candida albicans. J Immunol Baltim Md 1950. 2012;189:4713–4717. doi: 10.4049/jimmunol.1201715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Krysan D.J., Sutterwala F.S., Wellington M. Catching fire: Candida albicans, macrophages, and pyroptosis. PLoS Pathog. 2014;10:e1004139. doi: 10.1371/journal.ppat.1004139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Uwamahoro N., Verma-Gaur J., Shen H.-H., Qu Y., Lewis R., Lu J., Bambery K., Masters S.L., Vince J.E., Naderer T. The pathogen Candida albicans hijacks pyroptosis for escape from macrophages. mBio. 2014;5:e00003–e14. doi: 10.1128/mBio.00003-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Wellington M., Koselny K., Sutterwala F.S., Krysan D.J. Candida albicans triggers NLRP3-mediated pyroptosis in macrophages. Eukaryot. Cell. 2014;13:329–340. doi: 10.1128/EC.00336-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67••.O’Meara T.R., Veri A.O., Ketela T., Jiang B., Roemer T., Cowen L.E. Global analysis of fungal morphology exposes mechanisms of host cell escape. Nat Commun. 2015;6:6741. doi: 10.1038/ncomms7741. [DOI] [PMC free article] [PubMed] [Google Scholar]; In this analysis a screen of mutants is used to conclude that whist hyphae of C. albicans can activate pyroptosis, this is not an obligate association.
- 68.Gow N.A.R., Hube B. Importance of the Candida albicans cell wall during commensalism and infection. Curr Opin Microbiol. 2012;15:406–412. doi: 10.1016/j.mib.2012.04.005. [DOI] [PubMed] [Google Scholar]