Abstract
Objective
To examine the association between baseline mindfulness and response from exercise interventions in knee osteoarthritis (OA).
Design
Cohort Study; Responder analysis of a clinical trial subset
Setting
Urban tertiary care academic hospital
Participants
86 participants with symptomatic, radiographic knee OA (mean age, 60 years; 74% female; 48% white)
Interventions
12 weeks (twice per week) of Tai Chi or Physical Therapy exercise
Main Outcome Measure(s)
Treatment response was defined using Osteoarthritis Research Society International criteria indicating meaningful improvements in the Western Ontario and McMaster Osteoarthritis Index (WOMAC) pain, function, or Patient Global Assessment scores. At baseline, participants completed the Five Facet Mindfulness Questionnaire (FFMQ; mean total score ±SD: 142±17) and were grouped into three categories of total mindfulness: higher, medium, or lower. Relative risk (RR) ratios were used to compare treatment response across groups.
Results
Participants with higher total mindfulness appeared to be 38% (95% CI: 1.05, 1.83) more likely to meet responder criteria than those with lower mindfulness. We found no significant difference between medium and lower mindfulness groups (RR=1.0; 95% CI: 0.69, 1.44). Among the 5 mindfulness facets, medium Acting-with–Awareness was 46% (95% CI: 1.09, 1.96) more likely to respond than lower Acting-with–Awareness, and higher Acting-with–Awareness was 34% more likely to respond, but this did not reach significance (95% CI: 0.97, 1.86).
Conclusions
In this study, higher mindfulness, primarily driven by its Acting-with-Awareness facet, was significantly associated with a greater likelihood of response to non-pharmacological exercise interventions in knee OA. This suggests that mindfulness-cultivating interventions may increase the likelihood of response from exercise.
Keywords: Osteoarthritis, Mindfulness, Tai Chi, Physical Therapy, Responder Analysis, Exercise Intervention
Knee osteoarthritis (OA) affects more than 20 million Americans and is a leading cause of physical disability and chronic pain1,2. Current clinical guidelines emphasize rehabilitative exercise treatment as the foundation of conservative symptom management3. However, the manifestations of knee OA and response to treatment varies4–7. This heterogeneity of clinical presentation and treatment response confounds interpretation of therapeutic clinical trials and complicates the care decisions for clinicians4,5. Thus, identifying clinical factors to define patient profiles most likely to benefit from treatment would help therapeutic decision-making6,8. Prior studies have explored several potential physical and biomechanical predictive factors of non-pharmacological treatment response, including muscle strength, inflammation, and tibiofemoral joint alignment9. However, there are considerably fewer studies on the psychological predictors of response.
Psychological health has a well-established role in perpetuating the cycle of chronic pain10. Because exercise interventions require active patient participation, psychological factors may influence treatment efficacy through its behavioral effect on adherence11,12. One prior study found that absence of depressive symptoms predicted symptomatic response from exercise rehabilitation in OA7. While this study examined traditional (i.e. depression and anxiety) and general (e.g. mental health) constructs of psychological health, there is growing interest in the beneficial role of mindfulness, a relatively newer psychological construct used in biomedical research.
Mindfulness is a psychological state achieved by focusing one’s awareness on the present moment, while acknowledging and non-judgmentally accepting one’s feelings, thoughts, and bodily sensations13. It is also a dispositional characteristic or trait that varies from person to person and has an approximately normal distribution among the general population14. Rapidly accumulating evidence shows that mindfulness interventions enhance physical and psychological health among patients with chronic pain15–17. While these studies have primarily focused on the efficacy of mindfulness treatments, the evidence that mindfulness, as a characteristic, may influence treatment outcomes is scarce.
Research on the characteristic of mindfulness can examine the role of this trait on a variety of commonly-used treatments. For exercise interventions in chronic pain, mindfulness may be associated with improved outcomes because of its link with better pain coping skills18,19 and greater treatment adherence20,21. Among the general population, mindfulness is associated with greater physical activity and greater weight loss from exercise21–24. Investigating the association between mindfulness and exercise treatment outcomes is warranted because poor adherence and low pain-coping skills are both major barriers to exercise in OA11,12. To date, no study has examined longitudinal associations of mindfulness on treatment outcomes among these patients.
The purpose of this study was to examine the association between baseline mindfulness and treatment response from Tai Chi mind-body exercise or exercise-based Physical Therapy among adults with symptomatic, radiographic knee OA. The hypothesis is that greater mindfulness would be associated with increased treatment response.
Methods
Study Design
This study was a secondary analysis of a 52-week National Institutes of Health-funded, single-blind, randomized trial comparing Tai Chi and Physical Therapy among adults meeting the American College of Rheumatology (ACR) Criteria for symptomatic knee OA. Both interventions had similar response rates and pain/function/global health improvements. It was decided to combine data from participants receiving either intervention. A detailed description of the methodology and primary study results for this trial has been previously published25,26.
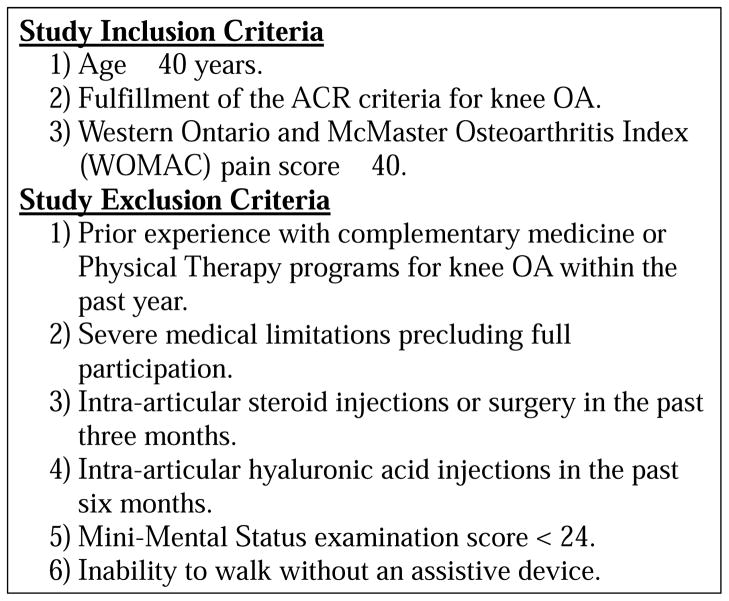
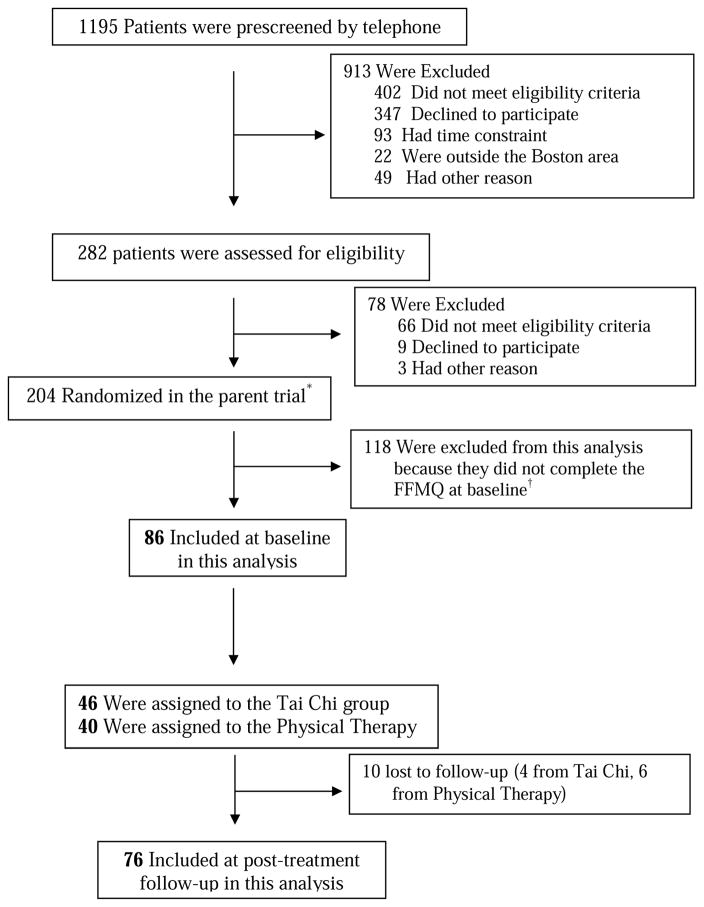
The trial was conducted at a University Medical Center in Boston, Massachusetts, between October 2010 and September 2014. Participants were recruited through multimodal strategies, including print advertisements, online media, a booth at a senior exposition, and a clinical patient database. We obtained informed consent before baseline assessments for eligibility. Study inclusion criteria included: 1)Age ≥40 years, 2)Fulfillment of the ACR criteria for knee OA, and 3)Western Ontario and McMaster Osteoarthritis Index (WOMAC) pain score ≥40. Exclusion criteria included: 1)Prior experience with complementary medicine or Physical Therapy programs for knee OA within the past year, 2)Severe medical limitations precluding full participation, 3)Intra-articular steroid injections or surgery in the past three months, 4)Intra-articular hyaluronic acid injections in the past six months, 5)Mini-Mental Status examination score <24, or 6)inability to walk without an assistive device (Figure 1). Participants were randomly assigned in a 1:1 ratio to Tai Chi or Physical Therapy. The physical function assessors were blinded to the treatment assignments during evaluations and did not have access to the data until data collection was complete. All participants signed an informed consent form before enrollment, and the study was approved by the Institutional Review Board. This study analyzed participants who had mindfulness data at baseline. The Five Facet Mindfulness Questionnaire (FFMQ) was formally implemented in the study after subject recruitment and data collection had already begun. After the FFMQ was included in the parent trial, all subsequent participants had the opportunity to complete the FFMQ at baseline. Therefore, this investigation only reports data from participants who completed the FFMQ at baseline, which was a fixed available sample. Of 204 participants from the parent trial, 86 completed the FFMQ at baseline and, therefore, were analyzed. Seventy-six participants were assessed after 12-week intervention; 10 were lost to follow-up (Figure 2).
Figure 1.
Inclusion/Exclusion Criteria
Figure 2. Sub-study Flow Diagram.
FFMQ = Five Facet Mindfulness Questionnaire.
Interventions
Tai Chi is a traditional Chinese mind-body exercise characterized by lower intensity physical activities, including slow, flowing movements that incorporate muscle strengthening, balance, postural training, meditation, and deep breath training. Accumulating evidence supports Tai Chi as an effective therapeutic exercise option for patients with chronic disease27,28. In this study, each Tai Chi class lasted 60 minutes and occurred twice weekly over 12 weeks. One of 3 Tai Chi instructors (20 combined years of experience) administered a standardized 10-form Yang style Tai Chi protocol for knee OA at each class25. Classes typically involved an initial warm-up and a review of Tai Chi principles and movement, breathing techniques, and relaxation methods.
The Physical Therapy intervention followed national guidelines for knee OA treatment29, and consisted of joint mobilizations, lower limb stretching, active and passive range-of-motion exercises, and strengthening, aerobic, and balance exercises. One of 3 licensed physical therapists (over 20 combined years of experience) offered two 30-minute one-to-one sessions per week for the first 6 weeks. For the second 6 weeks, participants completed four 30-minute sessions per week at home with weekly telephone monitoring. After an initial 1-hour musculoskeletal examination, physical therapists tailored the Physical Therapy regimen toward specific individualized-participant treatment goals. Throughout both interventions, participants were asked to practice for at least 20 minutes daily at home.
Outcome Measures
The FFMQ(39-items; higher scores reflect greater mindfulness) measures total mindfulness and its facets30,31. The 5 Facets: 1)Observing: noticing internal and external stimuli. 2)Describing: mentally labeling observed stimuli with words. 3)Acting-with-Awareness: attending to current actions, as opposed to behaving automatically/absentmindedly. 4)Non-judging: refraining from evaluation of one’s sensations/cognitions/emotions as negative or intolerable. 5)Non-reacting: allowing thoughts and feelings to come and go, without getting carried away by them.(Supplementary Table S1)
The WOMAC, v.3.1, has subscales measuring pain intensity (5 items, 0–500) and physical function (17 items, 0–1700) in knee osteoarthritis32. Higher scores indicate greater pain or poorer physical function, respectively. A 0–10 visual analog scale, the Patient Global Assessment (1-item; higher scores reflect greater disease activity) measures the patient’s perception of disease activity33. The Short Form-36 (36-items; higher scores reflect greater health status) measures health-related quality of life34. Scores were combined to obtain two aggregate scores, ranging from 0 to 100: the Physical Component Summary score and the Mental Component Summary score. The Six-minute Walk measures functional exercise capacity;35 participants walk as far as possible within a six-minute period.
The Beck Depression Inventory (21-items; higher scores reflect greater depressive symptoms) measures the severity of depressive symptoms36. The Perceived Stress Scale (10-items; higher scores reflect a greater stress) measures the degree to which situations over the past month are appraised as uncontrollable/overwhelming37. The Arthritis Self-Efficacy Scale-8 (10-point Likert scale; higher scores indicate higher self-efficacy)38 measures self-efficacy, the belief that one can successfully take action to produce a desired outcome. All measures used in this study have been validated.
Responder Criteria
Treatment response was defined according to the Outcome Measures in Rheumatology- Osteoarthritis Research Society International criteria for OA: 1. ≥50% improvement in pain or function and change of ≥20 points (0 to 100 scale) in WOMAC pain or function; or 2. ≥2 of the following: ≥20% improvement and change >10 points in WOMAC pain, ≥20% improvement and change >10 points in WOMAC function, or ≥20% improvement in Patient Global Assessment and change >10 points (0 to 100 scale)39.
Statistical Analysis
Missing FFMQ items were imputed from the mean of the non-missing items of the respective facet40. All data were examined visually and statistically for normality of distribution and presented as mean ±SD unless otherwise stated. Due to skewed distribution of scores and in the absence of established cut-points for the FFMQ31, participants were stratified into 3 tertiles based on baseline total score: higher, medium, and lower. Differences in characteristics among the three mindfulness groups were tested with analysis of variance or chi-square tests. Where necessary, Fisher’s exact tests compared categorical variables due to small sizes of some subgroups. Psychological variables (i.e. depression, stress, self-efficacy, and quality of life) were compared at baseline to illustrate previously reported associations between mindfulness and greater psychological health among the mindfulness tertiles 41. Significance level was p≤0.05. To examine whether this study sub-sample differed from the parent trial, baseline characteristics were compared using t-tests or chi-square tests.
To check for confounding, logistic regression was performed when baseline demographic variable or treatment response-determining variable (i.e. WOMAC Pain, Function, or Patient Global Assessment) differed significantly among tertiles. Any identified confounding factors were subsequently included in a multivariable logistic model. Because improvements in psychological health may be in the causal pathway, baseline psychological variables were not tested for confounding. It was planned to compare the likelihood of achieving responder criteria among the three mindfulness groups using chi-square tests and either risk ratios or odds ratios (95% CI), depending on whether confounding variables were found. Data were analyzed using SAS statistical software (Version 9.4).
Results
For missing FFMQ items at baseline, 5 people had 1 missing item and 1 person had 2 missing items. Participants were predominantly female (74%), well-educated (85%), and white (48%); mean age: 60 years; and body mass index (BMI): 33 kg/m2 (Table 1). Demographic and clinical variables did not significantly differ between the participant sub-sample and the parent clinical trial (not shown but available from the authors). Significant differences for psychological characteristics were found as expected; wherein greater mindfulness had greater health. There were no significant differences among mindfulness groups for treatment assignment or demographics, except BMI, and no significant baseline differences were found among mindfulness groups for the response-determining variables (i.e. WOMAC Pain, Function, or Patient Global Assessment). Including BMI in a logistic regression model did not change the results. Therefore, no multivariable models were performed, and all results are reported as risk ratios.
Table 1.
Demographic and Clinical Characteristics of Participants by Mindfulness Levels (n = 86)
| Variable | Lower Mindfulness (n = 23) | Medium Mindfulness (n = 26) | Higher Mindfulness (n = 27) | p-value | |
|---|---|---|---|---|---|
| Age, years | 63.1 (10.5) | 57.4 (9.5) | 60.5 (10.8) | 0.11 | |
|
| |||||
| BMI | 29.9 (6.3) | 33.0 (6.3) | 35.3 (7.4) | 0.01 | |
|
| |||||
| Sex, n (%) | Female | 19 (65.5%) | 20 (71.4%) | 25 (86.2%) | 0.18 |
| Male | 10 (34.5%) | 8 (28.6%) | 4 (13.8%) | ||
|
| |||||
| Pain duration, years | 11.2 (16.0) | 8.2 (8.4) | 11.5 (15.1) | 0.61 | |
|
| |||||
| Kellgren | 0-1 | 2 (7.1%) | 5 (17.9%) | 1 (3.6%) | 0.38 |
| Lawrence | 2 | 10 (35.7) | 9 (32.1%) | 12 (42.9%) | |
| Grade†, n (%) | 3 | 14 (50.0%) | 11 (39.3%) | 9 (32.1%) | |
| 4 | 2 (7.1%) | 3 (10.7%) | 6 (21.4%) | ||
|
| |||||
| Race, n (%) | White | 11 (37.9%) | 14 (50.0%) | 16 (55.2%) | 0.37 |
| Black | 11 (37.9%) | 8 (28.6%) | 11 (37.9%) | ||
| Other | 7 (24.1%) | 6 (21.4%) | 2 (6.9%) | ||
|
| |||||
| Education†, n (%) | High school | 7 (24.1%) | 3 (10.7%) | 3 (10.3%) | 0.38 |
| Some College | 9 (31.0%) | 11 (39.3%) | 12 (41.4%) | ||
| College Grad | 5 (17.2%) | 9 (32.1%) | 4 (13.8%) | ||
| Graduate School | 8 (27.6%) | 5 (17.9%) | 10 (34.5%) | ||
|
| |||||
| Intervention, n (%) | Tai Chi | 17 (58.6%) | 13 (46.4%) | 16 (55.2%) | 0.64 |
| Physical Therapy | 12 (41.4%) | 15 (53.6%) | 13 (44.8%) | ||
|
| |||||
| Total Mindfulness [min: max:] | 124 (8.4) | 141 (3.6) | 161 (9.5) | <0.0001 | |
| FFMQ Score Range, 39–195 | |||||
|
| |||||
|
WOMAC Pain* Score Range, 0–500mm |
289.0 (111.6) | 253.7 (93.1) | 253.8 (95.7) | 0.31 | |
|
| |||||
|
WOMAC Function* Score Range, 0-1700mm |
946.4 (387.2) | 930.8 (335.1) | 921.1 (360.6) | 0.96 | |
|
| |||||
|
Patient Global Assessment* Score Range, 0–10cm |
5.2 (2.2) | 5.1 (2.0) | 5.1 (2.2) | 0.98 | |
|
| |||||
|
Perceived Stress Score Range, 0–40 |
17.03(6.72) | 13.43(5.93) | 8.97(5.17) | <0.0001 | |
|
| |||||
|
Self-Efficacy
Score Range, 0-10 |
5.73(1.84) | 5.85(2.21) | 7.35(1.62) | 0.002 | |
|
| |||||
| 6-Minute Walk Test meters | 381.47(94.47) | 399.90(94.75) | 408.94(85.06) | 0.52 | |
|
| |||||
|
SF MCS
Score Range, 0–100 |
47.11(10.30) | 54.43(6.55) | 56.85(6.54) | <0.0001 | |
|
| |||||
|
SF PCS
Score Range, 0–100 |
33.34(7.43) | 35.60(10.11) | 40.34(8.45) | 0.01 | |
|
| |||||
|
Beck Depression
Score Range, 0–63 |
12.76(11.28) | 6.32(6.26) | 3.71(4.21) | 0.0001 | |
All values are mean (SD), unless otherwise stated. FFMQ = Five Facet Mindfulness Questionnaire, higher scores = higher mindfulness; SF = Short Form-36; MCS = Mental Component Summary; PCS = Physical Component Summary.
Higher scores = more pain, worse function, or more global disease.
Fisher’s exact tests were used in place of chi-square tests due to small sample sizes in some sub-groups.
For those with higher mindfulness, 96% responded from Tai Chi or Physical Therapy (Table 2). However, for those with medium or lower mindfulness, only 69% responded. Table 3 summarizes the likelihood of response by total and facet mindfulness. Higher total mindfulness was 38% (95% CI:1.05, 1.83) more likely to respond than lower, but no significant difference was found between medium and lower total mindfulness (1.0; 95% CI:0.69, 1.44). Among the 5 facets, there was a greater magnitude of effect in the Acting-with-Awareness facet than in other facets. Medium Acting-with-Awareness was 46% (95% CI:1.09, 1.96) more likely to respond than lower. Participants with higher Acting-with-Awareness were 34% (95% CI:0.97, 1.86) more likely to respond than lower, which trended toward significance.
Table 2.
Distribution of Treatment Response by Total Mindfulness Levels
| Mindfulness Tertile* | No Treatment Response | Treatment Response† | Row Total |
|---|---|---|---|
|
Lower, N (%) [Score Min: 98; Max: 134] |
7 (30.4%) | 16 (69.6%) | 23 |
|
Medium, N (%) [Score Min: 135; Max: 148] |
8 (30.8%) | 18 (69.2%) | 26 |
|
Higher, N (%) [Score Min: 149; Max: 181] |
1 (3.7%) | 26 (96.3%) | 27 |
| Column Total | 16 | 60 | 76 |
N = number of participants.
Mindfulness as measured by the total Five Facet Mindfulness Questionnaire score; Score Range, 39–195.
Treatment response as defined by the Outcome Measures in Rheumatology- Osteoarthritis Research Society International (OMERACT-OARSI) Responder Criteria.
Table 3.
Relative Risk of Treatment Response by Total and Facet Mindfulness Levels (n = 76)
| FFMQ Variable | Mindfulness Tertiles | Relative Risk (95% Confidence Interval) | p-value (Chi-square) |
|---|---|---|---|
|
Total
Score Range, 39–195 |
Higher | 1.38 (1.05, 1.83) | 0.01 |
| Medium | 1.00 (0.69, 1.44) | 0.98 | |
| Lower | Reference | ||
|
| |||
|
Observing
Score Range, 8–40 |
Higher | 0.91 (0.69, 1.20) | 0.51 |
| Medium | 0.97 (0.74, 1.29) | 0.85 | |
| Lower | Reference | ||
|
| |||
|
Describing
Score Range, 8–40 |
Higher | 1.04 (0.76, 1.41) | 0.82 |
| Medium | 1.12 (0.84, 1.49) | 0.43 | |
| Lower | Reference | ||
|
| |||
|
Acting-with-Awareness
Score Range, 8–40 |
Higher | 1.34 (0.97, 1.86) | 0.09 |
| Medium | 1.46 (1.09, 1.96) | 0.01 | |
| Lower | Reference | ||
|
| |||
|
Non-Judging
Score Range, 8–40 |
Higher | 1.18 (0.88, 1.58) | 0.24 |
| Medium | 1.10 (0.80, 1.51) | 0.56 | |
| Lower | Reference | ||
|
| |||
|
Non-Reacting
Score Range, 7–35 |
Higher | 1.12 (0.85, 1.47) | 0.42 |
| Medium | 1.04 (0.77, 1.41) | 0.78 | |
| Lower | Reference | ||
FFMQ = Five Facet Mindfulness Questionnaire.
Discussion
This study examined the association between baseline mindfulness and treatment response from non-pharmacological exercise interventions among adults with symptomatic knee OA. Participants with higher total mindfulness were 38% more likely to respond to Tai Chi exercise or exercise-based Physical Therapy. Among the 5 mindfulness facets, Acting-with –Awareness facet had the greatest magnitude of effect. Importantly, these results provide a preliminary suggestion that adults with higher mindfulness may represent a novel patient sub-group more likely to respond to these exercise treatments.
These results are consistent with a previous study wherein mindfulness predicted treatment response to exercise intervention for weight loss42, and extend prior observational research showing that mindfulness was associated with reduced stress and disability43, lower pain catastrophizing44, and increased physical activity24. Overall, these results contribute to the evidence indicating that as a characteristic, mindfulness may influence better health outcomes from exercise. Although the rationale underlying this association is not known, it may be that higher mindfulness facilitates greater adherence7,9,23.
Preliminary evidence suggests that cognitive mechanisms of mindfulness involve a better ability to extinguish unhealthy behavioral habits and emotionally adapt to stress45. Indeed, psychological factors did not predict response from pharmacological interventions, which involve a relatively more passive amount of patient participation9,46. However, the overall evidence supporting the link between mindfulness or other psychological factors and exercise response has been inconsistent, primarily due to heterogeneity in study design7,9,47,48. As a complex construct, mindfulness must be disentangled from its associations with other psychosocial variables to better understand how it functions as a predictor.
Baseline mindfulness facets did not predict treatment response, except Acting-with-Awareness: medium levels were significant and higher levels trended toward significance. Importantly, Acting-with-Awareness had a relatively larger magnitude of effect than the other facets, which suggests it may be the most sensitive facet in predicting response. This may be because attending to current actions, as opposed to behaving absentmindedly, facilitates better exercise efficiency or pain coping. Notably, in a cross-sectional investigation, the Acting-with-Awareness facet attenuated the influence of pain on stress in knee OA41. Taken together, these preliminary findings indicate that total mindfulness and its Acting-with-Awareness facet appear most relevant to improved outcomes from exercise interventions in OA. However, further study is needed to distinguish the medical relevance of mindfulness facets49, and the length of the FFMQ limits applicability to patient care settings. Thus, the development of short forms or computer-adaptive mindfulness instruments would enhance the feasibility of its assessment in routine care.
This study has implications for research in OA and exercise science, and responds to the call for further research to identify psychological factors that predict response in OA4,8,9,50,51. Identifying factors that influence treatment response may enhance stratified-randomization strategies that attempt to balance comparator groups of exercise trials to reduce confounding8,52. Current guidelines recommend researchers designing OA exercise trials collect psychosocial variables that may influence the effectiveness of intervention, including outcome expectations and depression53. These findings provide initial support for mindfulness as a confounding variable of exercise trials in OA. If confirmed, mindfulness-cultivating interventions might be used as a preparative adjunct or combined with exercise to enhance the likelihood of treatment response. Discordant from initial hypothesis, however, participants with medium total mindfulness were not significantly more likely to respond to intervention than lower mindfulness. While it cannot be ruled out that sample size influenced this result, it is possible that the association between mindfulness and response is not linear. However, because medium Acting-with-Awareness was significant while higher Acting-with-Awareness was not, further evidence is necessary to clarify the shape of this association and whether it differs by total or facet mindfulness.
In the clinical setting, these results help to advance the understanding of the heterogeneity of patient response to exercise. This may inform clinicians who seek to understand why some patients do not respond, and subsequently consider alternative options. The dearth of evidence explaining this heterogeneity has impeded the use of individualized exercise prescriptions by physicians to promote greater physical activity among these patients8,51,54,55. By expanding the evidence to clarify the heterogeneity of response, these findings help advance the integration of prescriptive exercise by physicians into routine medical care for OA55.
Limitations
This study is a secondary analysis of clinical trial data, and as such the results require confirmation in a further study primarily designed to examine mindfulness as a predictor of response. The sample was not representative of all persons with knee OA because they were symptomatic and knowingly participated in a trial. Although this may influence the study generalizability, the participants had characteristics of patients seen routinely in clinical settings. Furthermore, while the mindfulness level of this sample was skewed towards higher mindfulness, they were comparable to those of highly educated samples30, which is concordant with the educational background of these participants. The second limitation of this study was that the sample size was not large. Some of the non-significant associations could be explained by a lack of power. However, lacking optimal statistical power does not diminish the importance of the significant findings. Namely, that higher total mindfulness was associated with higher response, and that Acting-with-Awareness had the greatest magnitudes of effect among facets. Thirdly, because the parent trial did not include a control group, this study could not disentangle the contributions of placebo or ‘regression-to-the-mean’, which occur in any treatment intervention. Nevertheless, based on recent platinum-quality evidence showing that various exercise-based therapies directly cause benefits in pain and function in OA56, the implicit assumption that treatment response was attributable to the interventions was reasonable. Furthermore, several steps were taken to reduce bias, including the validated, widely-accepted definition of response, the radiographic, symptomatic confirmation of diagnosis, the representative characteristics of the subsample with the parent trial, and the proportionally balanced, randomized intervention assignments among the mindfulness groups. Fourthly, due to sample size, this study did not compare the association magnitudes according to treatment type. As a commonly-cited underlying mechanism of Tai Chi57, mindfulness may have a stronger association with response in Tai Chi than Physical Therapy. However, the parent trial showed that the response rates did not statistically or meaningfully differ by treatment26. If mindfulness therefore had a stronger association with response in Tai Chi, this difference must have been equally counter-balanced by a different factor in Physical Therapy, which is unlikely. Further study in a larger trial is warranted. Finally, the use of tertiles to categorize participants according to a continuous variable can reduce sampling power and is limited as a primarily data-driven approach. It is therefore important to empirically identify clinically relevant cut-points for the FFMQ that can be used to further examine the prognostic value of mindfulness levels among those with chronic diseases.
Despite limitations of this study, the main implication remains that mindfulness may be useful to better understand patient heterogeneity of response from exercise in knee OA. This is the first study known to empirically show this in OA or other chronic musculoskeletal pain conditions. Future studies involving a clinical trial design, larger samples of participants and different types of exercise interventions are needed. Additional exploration of causal pathways underlying this association may further inform how mindfulness can be best examined in research and applied to clinical settings.
Conclusions
In conclusion, higher baseline mindfulness was associated with treatment response from Tai Chi or Physical Therapy exercise interventions among adults with symptomatic knee OA. In addition, Acting-with-Awareness may be the facet driving this association. This investigation underscores the role of psychological health in the heterogeneity of treatment response in OA, and further studies in this area may guide efficient clinical decision-making for non-pharmacological therapy of patients with knee OA.
Supplementary Material
Table S1. Items of the Five Facet Mindfulness Questionnaire (FFMQ)*
Highlights.
Higher baseline mindfulness was associated with treatment response in knee osteoarthritis.
This finding was primarily driven by the Acting-with-Awareness mindfulness facet.
Mindfulness may be a prognostic indicator of treatment response among these patients.
Mindfulness-cultivating interventions might be help as a preparatory adjunct to exercise.
Acknowledgments
Supported by: National Center for Complementary and Integrative Health (R01AT005521 and K24AT007323), and National Center for Advancing Translational Sciences (UL1TR001064) at the National Institutes of Health. The contents of this manuscript are solely the responsibility of the authors and do not necessarily represent the official views of the National Institutes of Health. The investigators are solely responsible for the content of the manuscript and the decision to submit for publication. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
The Authors gratefully appreciate Dr. Emily Holick for assistance with the presentation of the data and Stephanie Hyon for feedback on the written manuscript.
List of Abbreviations
- ACR
American College of Rheumatology
- BMI
Body Mass Index
- FFMQ
Five Facet Mindfulness Questionnaire
- OA
Osteoarthritis
- WOMAC
Western Ontario and McMaster Osteoarthritis Index
Footnotes
Author contributions
All authors were involved in drafting the article or revising it critically for important intellectual content, and all authors approved the final version to be published. Dr. Lee had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study conception and design: Lee, Price, Han, Harvey, Driban, Wong, Chung, McAlindon, Wang.
Acquisition of data: Lee, Price, Han, Harvey, Driban, Wong, Chung, McAlindon, Wang.
Analysis and interpretation of data: Lee, Price, Han, Harvey, Driban, Wong, Chung, McAlindon, Wang.
Trial Registration: Clinicaltrials.gov NCT01258985. Registered 10 December 2010
Conflicts of Interest: JBW has research funding from PCORI (Patient-Centered Outcome Research Institute) for “A Method for Patient-Centered Enrollment in Comparative Effectiveness Trials: Mathematical Equipoise” which is examining total knee replacement for osteoarthritis. The remaining authors report no conflicts of interest. We certify that the full article is an original work and is not being considered for publication elsewhere.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Ma VY, Chan L, Carruthers KJ. Incidence, prevalence, costs, and impact on disability of common conditions requiring rehabilitation in the united states: Stroke, spinal cord injury, traumatic brain injury, multiple sclerosis, osteoarthritis, rheumatoid arthritis, limb loss, and back pa. Arch Phys Med Rehabil [Internet] 2014;95:986–995e1. doi: 10.1016/j.apmr.2013.10.032. Available from: http://dx.doi.org/10.1016/j.apmr.2013.10.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhang Y, Jordan JM. Epidemiology of osteoarthritis. Clin Geriatr Med [Internet] 2010;26:355–69. doi: 10.1016/j.cger.2010.03.001. [cited 2016 Jul 26]; Available from: http://www.ncbi.nlm.nih.gov/pubmed/20699159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nelson AE, Allen KD, Golightly YM, Goode AP, Jordan JM. A systematic review of recommendations and guidelines for the management of osteoarthritis: The Chronic Osteoarthritis Management Initiative of the U.S. Bone and Joint Initiative. Semin Arthritis Rheum [Internet] 2016;43:701–12. doi: 10.1016/j.semarthrit.2013.11.012. Available from: http://dx.doi.org/10.1016/j.semarthrit.2013.11.012. [DOI] [PubMed] [Google Scholar]
- 4.Arden N, Richette P, Cooper C, Bruyère O, Abadie E, Branco J, et al. Can We Identify Patients with High Risk of Osteoarthritis Progression Who Will Respond to Treatment? A Focus on Biomarkers and Frailty. Drugs Aging [Internet] 2015;32:525–35. doi: 10.1007/s40266-015-0276-7. [cited 2016 Feb 13]; Available from: http://www.ncbi.nlm.nih.gov/pubmed/26085027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bruyère O, Cooper C, Arden N, Branco J, Brandi ML, Herrero-Beaumont G, et al. Can we identify patients with high risk of osteoarthritis progression who will respond to treatment? A focus on epidemiology and phenotype of osteoarthritis. Drugs Aging [Internet] 2015;32:179–87. doi: 10.1007/s40266-015-0243-3. [cited 2016 Feb 13]; Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=4366553&tool=pmcentrez&rendertype=abstract. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bennell KL, Hall M, Hinman RS. Osteoarthritis year in review 2015: rehabilitation and outcomes. Osteoarthr Cartil. 2016;24:58–70. doi: 10.1016/j.joca.2015.07.028. [DOI] [PubMed] [Google Scholar]
- 7.Weigl M, Angst F, Aeschlimann A, Lehmann S, Stucki G. Predictors for response to rehabilitation in patients with hip or knee osteoarthritis: a comparison of logistic regression models with three different definitions of responder. Osteoarthr Cartil [Internet] 2006;14:641–51. doi: 10.1016/j.joca.2006.01.001. Available from: http://www.ncbi.nlm.nih.gov/pubmed/16513373. [DOI] [PubMed] [Google Scholar]
- 8.Gierisch JM, Myers ER, Schmit KM, McCrory DC, Coeytaux RR, Crowley MJ, et al. Prioritization of Patient-Centered Comparative Effectiveness Research for Osteoarthritis. Ann Intern Med [Internet] 2014;160:836. doi: 10.7326/M14-0318. [cited 2016 Jul 22] Available from: http://annals.org/article.aspx?doi=10.7326/M14-0318. [DOI] [PubMed] [Google Scholar]
- 9.Eyles J, Lucas BR. Targeting Care: Tailoring Nonsurgical Management According to Clinical Presentation. Rheum Dis Clin North Am. 2013;39:213–33. doi: 10.1016/j.rdc.2012.11.001. [DOI] [PubMed] [Google Scholar]
- 10.Hooten WM. Chronic Pain and Mental Health Disorders: Shared Neural Mechanisms, Epidemiology, and Treatment. Mayo Clin Proc. 2016;91:955–70. doi: 10.1016/j.mayocp.2016.04.029. [DOI] [PubMed] [Google Scholar]
- 11.Bennell KL, Dobson F, Hinman RS. Exercise in osteoarthritis: Moving from prescription to adherence. Best Pract Res Clin Rheumatol [Internet] 2014;28:93–117. doi: 10.1016/j.berh.2014.01.009. Available from: http://linkinghub.elsevier.com/retrieve/pii/S1521694214000102. [DOI] [PubMed] [Google Scholar]
- 12.Dobson F, Bennell KL, French SD, Nicolson PJA, Klaasman RN, Holden MA, et al. Barriers and Facilitators to Exercise Participation in People with Hip and/or Knee Osteoarthritis: Synthesis of the Literature Using Behavior Change Theory. Am J Phys Med Rehabil [Internet] 2016 doi: 10.1097/PHM.0000000000000448. [cited 2016 Mar 23];Available from: http://www.ncbi.nlm.nih.gov/pubmed/26945211. [DOI] [PubMed]
- 13.Stahl B, Goldstein E. A Mindfulness-Based Stress Reduction Workbook. Oakland, California: New Harbinger Publications; 2010. [Google Scholar]
- 14.Walach H, Buchheld N, Buttenmüller V, Kleinknecht N, Schmidt S. Measuring mindfulness—the Freiburg Mindfulness Inventory (FMI) Pers Individ Dif. 2006;40:1543–55. [Google Scholar]
- 15.Bawa FLM, Mercer SW, Atherton RJ, Clague F, Keen A, Scott NW, et al. Does mindfulness improve outcomes in patients with chronic pain? Systematic review and meta-analysis. Br J Gen Pract [Internet] 2015;65:e387–400. doi: 10.3399/bjgp15X685297. [cited 2016 Jun 9] Available from: http://www.ncbi.nlm.nih.gov/pubmed/26009534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chiesa A, Serretti A. Mindfulness-based interventions for chronic pain: a systematic review of the evidence. J Altern Complement Med [Internet] 2011;17:83–93. doi: 10.1089/acm.2009.0546. Available from: http://www.ncbi.nlm.nih.gov/pubmed/21265650. [DOI] [PubMed] [Google Scholar]
- 17.Veehof MM, Oskam M-J, Schreurs KMG, Bohlmeijer ET. Acceptance-based interventions for the treatment of chronic pain: A systematic review and meta-analysis. Pain [Internet] 2011;152:533–42. doi: 10.1016/j.pain.2010.11.002. Available from: http://content.wkhealth.com/linkback/openurl?sid=WKPTLP:landingpage&an=00006396-201103000-00014. [DOI] [PubMed] [Google Scholar]
- 18.Schütze R, Rees C, Preece M, Schütze M, Schutze R, Rees C, et al. Low mindfulness predicts pain catastrophizing in a fear-avoidance model of chronic pain. Pain [Internet] 2010;148:120–7. doi: 10.1016/j.pain.2009.10.030. Available from: http://dx.doi.org/10.1016/j.pain.2009.10.030. [DOI] [PubMed] [Google Scholar]
- 19.Mun CJ, Okun MA, Karoly P. Trait mindfulness and catastrophizing as mediators of the association between pain severity and pain-related impairment. Pers Individ Dif [Internet] 2014;66:68–73. Available from: http://dx.doi.org/10.1016/j.paid.2014.03.016. [Google Scholar]
- 20.Mantzios M. Exploring the relationship between worry and impulsivity in military recruits: the role of mindfulness and self-compassion as potential mediators. Stress Health [Internet] 2014;30:397–404. doi: 10.1002/smi.2617. [cited 2016 Jul 26]; Available from: http://www.ncbi.nlm.nih.gov/pubmed/25476964. [DOI] [PubMed] [Google Scholar]
- 21.Mantzios M, Wilson JC. Making concrete construals mindful: a novel approach for developing mindfulness and self-compassion to assist weight loss. Psychol Health [Internet] 2014;29:422–41. doi: 10.1080/08870446.2013.863883. [cited 2016 Jul 26]; Available from: http://www.ncbi.nlm.nih.gov/pubmed/24215123. [DOI] [PubMed] [Google Scholar]
- 22.Mantzios M, Wilson JC, Linnell M, Morris P. The Role of Negative Cognition, Intolerance of Uncertainty, Mindfulness, and Self-Compassion in Weight Regulation Among Male Army Recruits. Mindfulness (N Y) [Internet] 2015;6:545–52. [cited 2016 Jul 26]; Available from: http://link.springer.com/10.1007/s12671-014-0286-2. [Google Scholar]
- 23.Reel JJ, Lee JJ, Bellows A. Integrating exercise and mindfulness for an emerging conceptual framework: The intuitive approach to prevention and health promotion (IAPHP) Eat Disord [Internet] 2016;24:90–7. doi: 10.1080/10640266.2015.1118951. [cited 2016 Jul 21]; Available from: http://www.tandfonline.com/doi/full/10.1080/10640266.2015.1118951. [DOI] [PubMed] [Google Scholar]
- 24.Gilbert D, Waltz J. Mindfulness and Health Behaviors. Mindfulness (N Y) 2010;1:227–34. [Google Scholar]
- 25.Wang C, Iversen MD, McAlindon T, Harvey WF, Wong JB, Fielding RA, et al. Assessing the comparative effectiveness of Tai Chi versus physical therapy for knee osteoarthritis: design and rationale for a randomized trial. BMC Complement Altern Med [Internet] 2014;14:333. doi: 10.1186/1472-6882-14-333. [cited 2016 May 23] Available from: http://www.biomedcentral.com/1472-6882/14/333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wang C, Schmid CH, Iversen MD, Harvey WF, Fielding RA, Driban JB, et al. Comparative Effectiveness of Tai Chi Versus Physical Therapy for Knee Osteoarthritis: A Randomized Trial. Ann Intern Med [Internet] 2016 doi: 10.7326/M15-2143. [cited 2016 May 18];Available from: http://www.ncbi.nlm.nih.gov/pubmed/27183035. [DOI] [PMC free article] [PubMed]
- 27.Chen Y-W, Hunt MA, Campbell KL, Peill K, Reid WD. The effect of Tai Chi on four chronic conditions—cancer, osteoarthritis, heart failure and chronic obstructive pulmonary disease: a systematic review and meta-analyses. Br J Sports Med [Internet] 2016;50:397–407. doi: 10.1136/bjsports-2014-094388. [cited 2016 Aug 1]; Available from: http://bjsm.bmj.com/lookup/doi/10.1136/bjsports-2014-094388. [DOI] [PubMed] [Google Scholar]
- 28.Wang C, Collet JP, Lau J. The Effect of Tai Chi on Health Outcomes in Patients With Chronic Conditions. Arch Intern Med [Internet] 2004;164:493. doi: 10.1001/archinte.164.5.493. [cited 2017 Feb 10] Available from: http://www.ncbi.nlm.nih.gov/pubmed/15006825. [DOI] [PubMed] [Google Scholar]
- 29.Deyle GD, Allison SC, Matekel RL, Ryder MG, Stang JM, Gohdes DD, et al. Physical therapy treatment effectiveness for osteoarthritis of the knee: a randomized comparison of supervised clinical exercise and manual therapy procedures versus a home exercise program. Phys Ther. 2005;85:1301–17. [PubMed] [Google Scholar]
- 30.Baer RA, Smith GT, Lykins E, Button D, Krietemeyer J, Sauer S, et al. Construct Validity of the Five Facet Mindfulness Questionnaire in Meditating and Nonmeditating Samples. Assessment [Internet] 2008;15:329–42. doi: 10.1177/1073191107313003. Available from: http://asm.sagepub.com/cgi/doi/10.1177/1073191107313003. [DOI] [PubMed] [Google Scholar]
- 31.Park T, Reilly-Spong M, Gross CR. Mindfulness: A systematic review of instruments to measure an emergent patient-reported outcome (PRO) Qual Life Res. 2013;22:2639–59. doi: 10.1007/s11136-013-0395-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol [Internet] 1988;15:1833–40. [cited 2015 Oct 1]; Available from: http://www.ncbi.nlm.nih.gov/pubmed/3068365. [PubMed] [Google Scholar]
- 33.Khan NA, Spencer HJ, Abda EA, Alten R, Pohl C, Ancuta C, et al. Patient’s global assessment of disease activity and patient’s assessment of general health for rheumatoid arthritis activity assessment: are they equivalent? Ann Rheum Dis [Internet] 2012;71:1942–9. doi: 10.1136/annrheumdis-2011-201142. Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=3731741&tool=pmcentrez&rendertype=abstract. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36): I. Conceptual framework and item selection. Med Care. 1992;30:473–83. [PubMed] [Google Scholar]
- 35.Olsson L, Swedberg K. Six minute walk test. Eur Heart J [Internet] 2005;26:2209–2209. doi: 10.1093/eurheartj/ehi452. [cited 2017 Feb 3]; Available from: https://academic.oup.com/eurheartj/article-lookup/doi/10.1093/eurheartj/ehi452. [DOI] [PubMed] [Google Scholar]
- 36.Beck AT, Steer RA, Brown GK. Manual for the Beck Depression Inventory-II 1996. San Antonio, TX: Psychol. Corp; 1996. [Google Scholar]
- 37.Eskildsen A, Dalgaard VL, Nielsen KJ, Andersen JH, Zachariae R, Olsen LR, et al. Cross-cultural adaptation and validation of the Danish consensus version of the 10-item Perceived Stress Scale. Scand J Work Environ Health [Internet] 2015;41:486–90. doi: 10.5271/sjweh.3510. [cited 2016 May 26]; Available from: http://www.ncbi.nlm.nih.gov/pubmed/26111225. [DOI] [PubMed] [Google Scholar]
- 38.Brady TJ. Measures of self-efficacy: Arthritis Self-Efficacy Scale (ASES), Arthritis Self-Efficacy Scale-8 Item (ASES-8), Children’s Arthritis Self-Efficacy Scale (CASE), Chronic Disease Self-Efficacy Scale (CDSES), Parent’s Arthritis Self-Efficacy Scale (PASE), an. Arthritis Care Res. 2011;63(Suppl 1):S473–85. doi: 10.1002/acr.20567. [DOI] [PubMed] [Google Scholar]
- 39.Pham T, Van Der Heijde DVD, Lassere M, Altman RD, Anderson JJ, Bellamy N, et al. Outcome variables for osteoarthritis clinical trials: The OMERACT-OARSI set of responder criteria. J Rheumatol. 2003;30:1648–54. [PubMed] [Google Scholar]
- 40.Yu M, Clark M. Investigating Mindfulness, Borderline Personality Traits, and Well-Being in a Nonclinical Population. Psychology [Internet] 2015;6:1232–48. Available from: http://www.scirp.org/journal/psych%5Cnhttp://dx.doi.org/10.4236/psych.2015.610121%5Cnhttp://creativecommons.org/licenses/by/4.0/ [Google Scholar]
- 41.Lee AC, Harvey WF, Price LL, Morgan LPK, Morgan NL, Wang C. Mindfulness is associated with psychological health and moderates pain in knee osteoarthritis. Osteoarthr Cartil [Internet] 2016;0:1350–2. doi: 10.1016/j.joca.2016.06.017. [cited 2016 Jun 27]; Available from: http://linkinghub.elsevier.com/retrieve/pii/S1063458416301534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Mason AE, Epel ES, Aschbacher K, Lustig RH, Acree M, Kristeller J, et al. Reduced reward-driven eating accounts for the impact of a mindfulness-based diet and exercise intervention on weight loss: Data from the SHINE randomized controlled trial. Appetite [Internet] 2016;100:86–93. doi: 10.1016/j.appet.2016.02.009. Available from: http://dx.doi.org/10.1016/j.appet.2016.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Nyklíèek I, Hoogwegt F, Westgeest T. Psychological distress across twelve months in patients with rheumatoid arthritis: The role of disease activity, disability, and mindfulness. J Psychosom Res [Internet] 2015;78:162–7. doi: 10.1016/j.jpsychores.2014.08.004. Available from: http://linkinghub.elsevier.com/retrieve/pii/S002239991400302X. [DOI] [PubMed] [Google Scholar]
- 44.Schütze R, Rees C, Preece M, Schütze M. Low mindfulness predicts pain catastrophizing in a fear-avoidance model of chronic pain. Pain [Internet] 2010;148:120–7. doi: 10.1016/j.pain.2009.10.030. [cited 2016 Apr 4]; Available from: http://www.ncbi.nlm.nih.gov/pubmed/19944534. [DOI] [PubMed] [Google Scholar]
- 45.Uusberg H, Uusberg A, Talpsep T, Paaver M. Mechanisms of mindfulness: The dynamics of affective adaptation during open monitoring. Biol Psychol. 2016;118:94–106. doi: 10.1016/j.biopsycho.2016.05.004. [DOI] [PubMed] [Google Scholar]
- 46.Snijders GF, van den Ende CHM, van den Bemt BJF, van Riel PLCM, van den Hoogen FHJ, den Broeder AA, et al. Treatment outcomes of a Numeric Rating Scale (NRS)-guided pharmacological pain management strategy in symptomatic knee and hip osteoarthritis in daily clinical practice. Clin Exp Rheumatol [Internet] 2012;30:164–70. [cited 2016 Jul 6]; Available from: http://www.ncbi.nlm.nih.gov/pubmed/22325619. [PubMed] [Google Scholar]
- 47.Wolf S, Foley S, Budiman-Mak E, Moritz T, O’Connell S, Jelinek C, et al. Predictors of weight loss in overweight veterans with knee osteoarthritis who participated in a clinical trial. J Rehabil Res Dev [Internet] 2010;47:171–81. doi: 10.1682/jrrd.2009.08.0136. [cited 2016 Aug 1]; Available from: http://www.ncbi.nlm.nih.gov/pubmed/20665344. [DOI] [PubMed] [Google Scholar]
- 48.Fuller NR, Sainsbury A, Caterson ID, Enarsson M, Denyer G, Manns C, et al. Examining mindfulness as a predictor of weight loss - Findings from the DIABEGG study. Obes Res Clin Pract [Internet] 2016 doi: 10.1016/j.orcp.2016.03.004. [cited 2016 May 12];Available from: http://www.ncbi.nlm.nih.gov/pubmed/27050109. [DOI] [PubMed]
- 49.Bergomi C, Tschacher W, Kupper Z. The Assessment of Mindfulness with Self-Report Measures: Existing Scales and Open Issues. Mindfulness (N Y) 2013;4:191–202. [Google Scholar]
- 50.Karsdal MA, Christiansen C, Ladel C, Henriksen K, Kraus VB, Bay-Jensen AC. Osteoarthritis - a case for personalized health care? Osteoarthr Cartil [Internet] 2014;22:7–16. doi: 10.1016/j.joca.2013.10.018. Available from: http://dx.doi.org/10.1016/j.joca.2013.10.018. [DOI] [PubMed] [Google Scholar]
- 51.Bamman MM, Cooper DM, Booth FW, Chin ER, Neufer PD, Trappe S, et al. Exercise biology and medicine: innovative research to improve global health. Mayo Clin Proc [Internet] 2014;89:148–53. doi: 10.1016/j.mayocp.2013.11.013. [cited 2016 Aug 9]; Available from: http://www.ncbi.nlm.nih.gov/pubmed/24485128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Lohmander LS, Roos EM. Clinical update: treating osteoarthritis. Lancet. 2007;370:2082–4. doi: 10.1016/S0140-6736(07)61879-0. [DOI] [PubMed] [Google Scholar]
- 53.Messier SP, Callahan LF, Golightly YM, Keefe FJ. OARSI Clinical Trials Recommendations: Design and conduct of clinical trials of lifestyle diet and exercise interventions for osteoarthritis. Osteoarthr Cartil. 2015;23:787–97. doi: 10.1016/j.joca.2015.03.008. [DOI] [PubMed] [Google Scholar]
- 54.Marks R. Knee osteoarthritis and exercise adherence: a review. Curr Aging Sci [Internet] 2012;5:72–83. doi: 10.2174/1874609811205010072. [cited 2016 Jan 15]; Available from: http://www.ncbi.nlm.nih.gov/pubmed/21762086. [DOI] [PubMed] [Google Scholar]
- 55.Bamman MM, Wick TM, Carmona-Moran CA, Bridges SL. Exercise Medicine for Osteoarthritis: Research Strategies to Maximize Effectiveness. Arthritis Care Res (Hoboken) [Internet] 2016;68:288–91. doi: 10.1002/acr.22680. [cited 2016 Jul 22]; Available from: http://doi.wiley.com/10.1002/acr.22680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Fransen M, Mcconnell S, Harmer AR, Van der Esch M, Simic M, Bennell KL. Exercise for osteoarthritis of the knee. Cochrane Database Syst Rev [Internet] 2015:CD004376. doi: 10.1002/14651858.CD004376.pub3. [cited 2016 Jan 27] Available from: http://www.ncbi.nlm.nih.gov/pubmed/25569281. [DOI] [PMC free article] [PubMed]
- 57.Wayne PM, Kaptchuk TJ. Challenges Inherent to T’ai Chi Research: Part I— T’ai Chi as a Complex Multicomponent Intervention. J Altern Complement Med [Internet] 2008;14:95–102. doi: 10.1089/acm.2007.7170a. Available from: http://www.liebertonline.com/doi/abs/10.1089/acm.2007.7170A. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Items of the Five Facet Mindfulness Questionnaire (FFMQ)*