Abstract
Background:
Renal cell carcinoma (RCC) is the most common type of malignant renal tumors with a growing incidence in the recent years. This study aimed to investigate the influencing factors and variation trend of hospitalization expenditures among RCC patients in a single-centered hospital in Beijing during 5 consecutive years and to find the major cost items and fluctuation tendency of inpatient medical expenditures.
Methods:
The information of medical expenditures among RCC patients in a Grade-A tertiary hospital during the years 2012–2016 was investigated to find the main cost items and changes affecting the medical cost structure. Gray correlation method was adopted in quantitative analysis to analyze the composition of medical expenditures, and the variation of hospitalization expense structure during the five years was studied by analyzing the degree of structural variation.
Results:
The cost item constitution of the hospitalization expenditures among RCC patients was relatively stable in the sample hospital during the past five years. To be specific, drug costs accounted for the largest proportion of medical expenditures each year, with the highest of 37.81% in 2012, and showed a slowly declining tendency in the coming years. The cost item with the highest correlation degree was drug costs, with the value of 1.0000; followed by the costs of surgeries, 0.8423. Furthermore, drug costs shared the largest proportion (40.95%) of structural variation, followed by the costs of surgeries (18.35%).
Conclusions:
Drug costs are the major influencing factors of the hospitalization expenditures among RCC patients. Thus, reasonable control on excessive drugs as well as the standardization of the diagnosis and treatment behaviors is conducive in reducing medical expenditures as well as easing patients’ economic burdens. Besides, the positive growth on surgery costs suggests that the labor value of medical staffs has been gradually recognized.
Keywords: Degree of Structural Variation, Health Expenditure, Renal Cell Carcinoma
INTRODUCTION
Renal cell carcinoma (RCC) accounts for about 80% of malignant renal tumors. According to an epidemiological study in 2016, the incidence of RCC is about 3.2% in China and is still on the rise. At present, radical surgical operations combined with postoperative comprehensive treatments (such as immunotherapy and chemotherapy) are the mainstreams for treating RCC.[1] Due to the growth of its incidence and the increasing medical costs in the recent years, studies on the economics of RCC are continuously developing around the world.[2] However, systematic researches on inpatient health expenditures of RCC are still rare in China.
Gray correlation method is the methodology of analyses on the correlation degree between the development and change of the internal factors within a gray system.[3] Researchers are able to find the main factors that affect the development and changing trends of the original sequence of the system in which the influencing factors are yet to be clarified through the method.[4] It shares the advantages of the unlimitedness of sample sizes, the explicitness of principles, the extensity of application scopes, as well as the intuitiveness of the results so that the influence of dimensionless on the size of the index can be overcome.[5] Gray correlation method was first applied in the field of economics, now it is widely adopted in the research of health-care areas in the recent years since the concept of medical expenditures shared gray characteristics in a degree.[6] In this study, we aimed to evaluate the correlation degree between each cost item using gray correlation method to find the main factors that affect total medical costs of RCC and analyze the structural variation of hospitalization expenses to provide suggestion and reference for hospitals and health administrative departments in reducing medical costs and releasing patients’ economic burdens.[7]
METHODS
Acquisition and preprocessing of data and materials
The basic information of inpatients whose first diagnosis was labeled as RCC from January 1, 2012, to December 31, 2016, in a Grade-A tertiary hospital (Beijing Hospital, China) was collected through the medical record management system. We preprocessed the data and materials by eliminating the cases with missing cost items and basic information in medical records. Totally, 200 cases were randomly selected by stratified sampling of age groups each year and the number of valid samples summed up 1000 in total. The inpatient medical expenditures were composed of eight items according to the medical information system as follows: bed charges, costs of examinations, costs of treatments, costs of surgeries, costs of laboratory tests, costs of nursery, costs of drugs as well as the costs of other items.[8] The costs of drugs mainly include the costs of organic and inorganic chemical drugs, costs of biological products, and the costs of Chinese herbal medicine and patent medicine; surgery costs include the labor charges during the operation as well as the related materials and supply costs; costs of treatment mainly refer to the expenditures on noninvasive treatment in clinical setting, which include the costs of hyperbaric oxygen, blood purification, and physical therapy.[9] The medical expenditure in the year 2016 was set as the basis of this research, and the index of Beijing residents’ consumer price was used to adjust the influence of time span on the average medical expenditures in previous years.[10]
Statistical analysis
In the study, Deng's gray correlation method was adopted in combination with the characteristics of medical expenditures to analyze the correlation degree and the dynamic trends of each cost item toward the total.[11] Meanwhile, the degree of structural variation (DSV) was used to analyze the contribution of each cost item toward the total. All the data and materials collected were entered into Excel 2010 software for Microsoft (Microsoft Corporation, Washington, USA), and statistical analyses were performed using SPSS 14.0 (SPSS Inc., Chicago, IL, USA).
Gray correlation analysis
The total average medical cost was set as the reference sequence and each individual cost item as the comparative sequence to construct the matrix (X1, X2, X3, X4, and X5). Decide whether or not to nondimensionalize the original data in the light of gray correlation analysis principle in combination with the dimensions of the original data. Δi(k) was calculated according to the below-mentioned formula, and the maximum (Δmax) and the minimum (Δmin) absolute differences were determined.
Δi(k) = |Xi(k) − X0(k)| (k = 1 − 5, representing the years 2012–2016, respectively).
Where Xi(k) represents the value of column i of year k and X0(k) represents the reference value of the column of year k.
Calculation of correlation coefficient
The correlation coefficient was calculated as follows:
i(k) = Δmin+ ρΔmax/(Δi(k) + ρΔmax) (i = 1, 2,……5; k = 1, 2,……5), where ρ represents the distinguishing coefficient. Set ρ = 0.5 and construct the relationship matrix.
Calculation of the value of structural variation
Value of structural variation (VSV) refers to the difference between the proportion of the final value and the initial value of a certain item in a given period of time. When VSV > 0, it indicates that the proportion of the item increases with time, otherwise it shows the trend of reduction. The basic formula is as follows: VSV = Xi1 − Xi0 (i represents the serial number of a certain cost item; 0 refers to the initial stage and 1 refers to the final stage). DSV refers to the sum of absolute value between the final value and the initial value of the proportion of a certain item in a given time period. The concept is used to reflect the comprehensive transformation of the internal structure within a system in a certain period of time. Moreover, the average annual DSV is calculated as follows: DSV/n,
Where n refers to the number of comparative periods.
DSV = Σ|Xi1–Xi0|i=1, 2,......5).
Structural contribution rate is used to indicate the magnitude of the impact on the change of certain cost item toward the overall structure of health expenditures. It represents the proportion of the absolute VSV of each cost item toward the overall DSV. The expression is as follows:
Structural contribution rate = 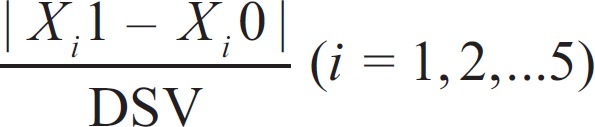
RESULTS
Basic information of patients with renal cell carcinoma over five consecutive years
To obtain an overall perspective of the general condition of RCC patients within the five consecutive years, we collected the basic information (including gender, average age, health insurance type, geographic location, comorbidities and complications, and average length of hospital stay) of the sample cases [Table 1].
Table 1.
Basic information of RCC patients in a Grade-A tertiary Hospital within the years 2012–2016
| Year | Genders of the sampled patients (n/%) | Average age of the sampled patients (years) | Health insurance types of the sampled patients (n/%) | Geographic locations of the sampled patients (n/%) | Comorbidities and complications of the sampled patients (n/%) | Average length of hospital stay of the sampled patients (days) |
|---|---|---|---|---|---|---|
| 2012 | Male (113/56.5) Female (87/43.5) |
62.7 | Insured patients (135/67.5) Uninsured patients (65/32.5) |
Local patients (162/81.0) Off-site patients (38/19.0) |
Yes (21/10.5) None (179/89.5) |
8.51 |
| 2013 | Male (118/59.0) Female (82/41.0) |
61.9 | Insured patients (132/66.0) Uninsured patients (68/34.0) |
Local patients (159/79.5) Off-site patients (41/20.5) |
Yes (23/11.5) None (177/88.5) |
8.25 |
| 2014 | Male (107/53.5) Female (93/46.5) |
62.3 | Insured patients (129/64.5) Uninsured patients (71/35.5) |
Local patients (158/79.0) Off-site patients (42/21.0) |
Yes (20/10.0) None (180/90.0) |
8.06 |
| 2015 | Male (110/55.0) Female (90/45.0) |
60.8 | Insured patients (118/59.0) Uninsured patients (82/41.0) |
Local patients (155/77.5) Off-site patients (45/22.5) |
Yes (18/9.0) None (182/91.0) |
7.96 |
| 2016 | Male (106/53.0) Female (94/47.0) |
59.9 | Insured patients (121/60.5) Uninsured patients (79/39.5) |
Local patients (158/79.0) Off-site patients (42/21.0) |
Yes (21/10.5) None (179/89.5) |
7.74 |
RCC: Renal cell carcinoma.
Composition of medical expenditures among patients with renal cell carcinoma
According to the statistics, drug costs accounted for the largest proportion of RCC medical expenditures each year, with the highest of 37.81% and 35.63% in the years 2012 and 2013, and showed a slowly declining tendency in the following years, but still remained >30% of the total expenditures. The cost of surgeries accounted for about 30% during the consecutive years, ranking the second. The constitutions of different cost items are shown in Table 2.
Table 2.
Constitution of average RCC inpatient health expenditures in a Grade-A tertiary Hospital within the years 2012–2016 (RMB, Yuan/%)
| Cost items | 2012 | 2013 | 2014 | 2015 | 2016 |
|---|---|---|---|---|---|
| Drug costs | 12,608.85/37.81 | 10,589.76/35.63 | 10,065.34/34.75 | 9304.56/33.91 | 10,117.83/32.88 |
| Surgery costs | 9120.66/27.35 | 9076.93/30.54 | 8153.65/28.15 | 7850.30/28.61 | 9096.22/29.56 |
| Treatment costs | 2947.96/8.84 | 2781.93/9.36 | 2800.92/9.67 | 2949.69/10.75 | 3178.75/10.33 |
| Examination costs | 2504.43/7.51 | 2663.04/8.96 | 2630.02/9.08 | 2859.14/10.42 | 2960.27/9.62 |
| Laboratory test costs | 2200.96/6.60 | 1807.06/6.08 | 1946.45/6.72 | 1821.95/6.64 | 2095.58/6.81 |
| Other costs | 1984.20/5.95 | 1426.63/4.80 | 1636.52/5.65 | 1303.35/4.75 | 1772.47/5.76 |
| Bed charges | 1594.03/4.78 | 974.86/3.28 | 1445.35/4.99 | 1075.61/3.92 | 1221.65/3.97 |
| Nursery costs | 386.83/1.16 | 371.52/1.25 | 286.76/0.99 | 299.09/1.09 | 329.26/1.07 |
| Total costs | 33,347.93/100 | 29,721.46/100 | 28,965.54/100 | 27,439.29/100 | 30,772.05/100 |
RCC: Renal cell carcinoma.
Results of gray correlation analysis
Absolute difference of sequence and correlation coefficient
By subtracting the annual costs of each cost item from the total costs, we were able to obtain the absolute difference sequence of the five years. By selecting the minimum and maximum values of the absolute difference each year, the study found that the position of minimum value and maximum value of cost items remained unchanged during the five years, with costs of nursery and drugs, respectively, as shown in Table 3. The correlation coefficient of each cost item is shown in Table 4.
Table 3.
Sequence difference of average RCC inpatient medical expenditures in a Grade-A tertiary Hospital within the years 2012–2016 (RMB, Yuan)
| Year | Drug costs | Surgery costs | Treatment costs | Examination costs | Laboratory test costs | Other costs | Bed charges | Nursery costs | ∆Maximum | ∆Minimum |
|---|---|---|---|---|---|---|---|---|---|---|
| 2012 | 19,335.89 | 20,898.80 | 26,738.11 | 27,280.81 | 27,540.13 | 28,217.94 | 28,295.06 | 29,306.35 | 29,306.35 | 19,335.89 |
| 2013 | 17,278.11 | 18,623.47 | 23,692.98 | 24,300.90 | 24,559.92 | 25,162.57 | 25,300.01 | 26,100.88 | 26,100.88 | 17,278.11 |
| 2014 | 17,245.67 | 18,069.96 | 23,007.96 | 23,165.09 | 24,009.99 | 24,561.23 | 24,749.28 | 25,503.99 | 25,503.99 | 17,245.67 |
| 2015 | 16,441.89 | 17,103.17 | 21,615.05 | 22,022.56 | 22,781.46 | 23,242.64 | 23,450.07 | 24,155.29 | 24,155.29 | 16,441.89 |
| 2016 | 18,773.06 | 19,276.60 | 24,265.42 | 24,459.72 | 25,584.46 | 25,814.33 | 26,285.03 | 27,103.27 | 27,103.27 | 18,773.06 |
RCC: Renal cell carcinoma.
Table 4.
Correlation coefficient of average RCC medical expenditures in a Grade-A tertiary Hospital within the years 2012–2016
| Correlation coefficient | Drug costs | Surgery costs | Treatment costs | Examination costs | Laboratory test costs | Other costs | Bed charges | Nursery costs |
|---|---|---|---|---|---|---|---|---|
| Xi(1) | 1.0000 | 0.8149 | 0.7291 | 0.7182 | 0.7149 | 0.7038 | 0.7015 | 0.6911 |
| Xi(2) | 1.0000 | 0.8228 | 0.7314 | 0.7220 | 0.7172 | 0.7065 | 0.7045 | 0.6937 |
| Xi(3) | 1.0000 | 0.8306 | 0.7355 | 0.7264 | 0.7206 | 0.7102 | 0.7080 | 0.6975 |
| Xi(4) | 1.0000 | 0.8607 | 0.7634 | 0.7551 | 0.7400 | 0.7291 | 0.7275 | 0.7172 |
| Xi(5) | 1.0000 | 0.8824 | 0.7844 | 0.7792 | 0.7559 | 0.7462 | 0.7446 | 0.7337 |
RCC: Renal cell carcinoma.
Degree and order of correlation
The correlation degree of drug costs was the highest among the cost items, while nursery costs was the lowest within the five years. The order of correlation degree ranked as drug costs, surgery costs, treatment costs, examination costs, laboratory test costs, other costs, bed charges, and nursery costs [Table 5].
Table 5.
Correlation degree and order of the cost items of the average RCC medical expenditures in a Grade-A tertiary Hospital within the years 2012–2016
| Correlation indicators | Drug costs | Surgery costs | Treatment costs | Examination costs | Laboratory test costs | Other costs | Bed charges | Nursery costs |
|---|---|---|---|---|---|---|---|---|
| Correlation degree | 1.0000 | 0.8423 | 0.7488 | 0.7402 | 0.7297 | 0.7192 | 0.7172 | 0.7066 |
| Correlation order | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
RCC: Renal cell carcinoma.
Analysis of structural variation
Value and degree of structural variation
During the period of 2012–2016 years, the highest DSV was between 2012 and 2013, which accounted for 10.60%, followed by the year 2013–2014, which accounted for 7.16%. The value and degree showed a slight decreasing trend over the following years. Moreover, the DSV of inpatient medical expenditures within the years 2012–2016 in total was 12.04%, with the average annual structural variation of 3.01% [Table 6].
Table 6.
Degree and value of structural variation of average RCC medical expenditures in a Grade-A tertiary Hospital within the years 2012–2016 (%)
| Year | Value of structural variation | Degree of structural variation | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Drug costs | Surgery costs | Treatment costs | Examination costs | Laboratory test costs | Other costs | Bed charges | Nursery costs | ||
| 2012–2013 | −2.18 | 3.19 | 0.52 | 1.45 | −0.52 | −1.15 | −1.50 | 0.09 | 10.60 |
| 2013–2014 | −0.88 | −2.39 | 0.31 | 0.12 | 0.64 | 0.85 | 1.71 | −0.26 | 7.16 |
| 2014–2015 | −0.84 | 0.46 | 1.08 | 1.34 | −0.08 | −0.90 | −1.07 | 0.10 | 5.87 |
| 2015–2016 | −1.03 | 0.95 | −0.42 | −0.80 | 0.17 | 1.01 | 0.05 | −0.02 | 4.45 |
| 2012–2016 | −4.93 | 2.21 | 1.49 | 2.11 | 0.21 | −0.19 | −0.81 | −0.09 | 12.04 |
RCC: Renal cell carcinoma.
Proportion and orientation of structural variation contribution of each cost item
According to the results, the proportion of structural variation contribution of each cost item between the several year periods showed a different orientation. While in total, the highest proportion of structural variation contribution in the years 2012–2016 was constituted by drug costs, which accounted for 40.95%, followed by the costs of surgeries, which accounted for 18.35%. Thus, in an overall perspective, the main factors for the variation in RCC medical expenditures were the costs of drugs as well as surgeries. Nevertheless, drug costs had been showing a negative changing trend during the time period, indicating that the proportion of drug costs was decreasing with time whereas the costs of surgeries showed a slight positive changing trend, indicating that the proportion of surgery costs was increasing with time [Table 7].
Table 7.
Proportion of structural variation contribution of each cost item toward total RCC medical expenditures in a Grade-A tertiary Hospital within the years 2012–2016 (%)
| Year | Drug costs | Surgery costs | Treatment costs | Examination costs | Laboratory test costs | Other costs | Bed charges | Nursery costs | Total |
|---|---|---|---|---|---|---|---|---|---|
| 2012–2013 | 20.57 | 30.08 | 4.91 | 13.68 | 4.91 | 10.85 | 14.15 | 0.85 | 100 |
| 2013–2014 | 12.29 | 33.38 | 4.33 | 1.68 | 8.94 | 11.87 | 23.88 | 3.63 | 100 |
| 2014–2015 | 14.31 | 7.84 | 18.40 | 22.83 | 1.36 | 15.33 | 18.23 | 1.70 | 100 |
| 2015–2016 | 23.15 | 21.34 | 9.44 | 17.98 | 3.82 | 22.70 | 1.12 | 0.45 | 100 |
| 2012–2016 | 40.95 | 18.35 | 12.38 | 17.52 | 1.74 | 1.58 | 6.73 | 0.75 | 100 |
RCC: Renal cell carcinoma.
DISCUSSION
Influence of drug costs on total medical expenditures among patients with renal cell carcinoma
In this study, drug costs accounted for the largest proportion of total medical expenditures. Besides, the analysis on the DSV showed that drug cost was also the major cost item that resulted to the structural change of total medical expenditures. We speculated that the cause was most Chinese hospitals largely relied on incomes of drug sales for the past few decades. The results of this study were consistent with the economic characteristics of RCC since chemotherapy and immunotherapy for cancers involved various high-value drugs.[12] According to the four basic principles of clinical medication, the choice on drugs should follow the criteria of safety, effectiveness, economy, and rationality.[13] However, the results showed a good sign that the proportion of drug costs among RCC patients was gradually decreasing, which might be largely attributed to the implementation of the new medical reform policy, and the profits of drug makeup were gradually substituted by dispensing fees.[14] Besides, the National Development and Reform Commission had adjusted the drug price within the range of government pricing and adopted a unified bidding policy to regulate drug prices. Though the proportion and correlation degree of drug costs are still the highest at present, it is believed that, with the full implementation of new health reform policy in canceling medical profits, more emphasis will be paid to the rational utilization of clinical medication by the hospital, and drug costs will be further reduced.[15]
Influence of surgery cost on total medical expenditures among patients with renal cell carcinoma
The results showed that surgery cost accounted for a great proportion of inpatient health expenditures of RCC patients, at around 30% for the consecutive years and was increasing with time. Also, the correlation degree of surgery costs ranked second after drug costs, indicating that the cost of surgery was another major factor affecting the inpatient medical expenditures. This was consistent with the characteristics of RCC since its first-line therapeutic plan is the combination of surgical operation and postoperative treatments.[16] We believe that it is a good sign since surgery costs symbolize the occupational value of medical staffs to a certain extent. Thus, the reasonable growth in surgery costs is conducive in upgrading the motivation of hospital staffs and improving the quality of medical service within the hospital so as to maintain the sustainable and healthy development of medical economics.[17]
Influence of treatment costs on total medical expenditures among patients with renal cell carcinoma
In regard to the characteristics of RCC, it was also explicable that treatment costs took up a great proportion of inpatient health expenditures and that the correlation degree was relatively high with the category since the combination of various adjunctive therapies (such as postoperative radiotherapy and immunotherapy) might be involved in the treating process.[18] Besides, the maintenance therapy costs for tumor also constitute an unneglectable proportion of the overall medical costs.
Influence of examination and laboratory test costs on total medical expenditures among patients with renal cell carcinoma
Routine monitoring and follow-up examinations are crucial for the prognosis of tumor patients, those led to an increase in the costs of examination and laboratory tests.[19] It is widely known that repeated and redundant examinations will not only increase the financial burdens among patients, but might also impede the process in recovery. Thus, it is important for doctors to master the indications of diagnoses and prescriptions, and to control unnecessary auxiliary examinations, that should be further emphasized and strengthened by the management departments of hospitals in regulating the inpatient medical expenditures.
Extensive researches show that the applications of gray correlation method should be carried out according to the practical situation among different areas. The price level, consumption level as well as the characteristics of RCC in different areas might have direct or indirect impacts on medical costs.[20] Since the research was performed based on the samples of a single-center hospital in a given period of time, considering the different situations in various regions as well as the limitations of the data and materials, the generalization of the results should be made more carefully in other circumstances.
In conclusion, it is crucial for medical institutions to emphasize the standardization in diagnosis and treatment behaviors and to strengthen the control on medical quality. Meanwhile, it is also conducive for health administrative departments to reinforce the management of drugs and medical materials in policymaking, as well as to strengthen the supervision on medical institutions to control the growth of medical expenditures and release the economic burdens of patients.
Financial support and sponsorship
This study was supported by a grant of Beijing Municipal Commission of Science and Technology (No. Z151100004015083).
Conflicts of interest
There are no conflicts of interest.
Footnotes
Edited by: Yuan-Yuan Ji
REFERENCES
- 1.Fadl Elmula FE, Jin Y, Yang WY, Thijs L, Lu YC, Larstorp AC, et al. Meta-analysis of randomized controlled trials of renal denervation in treatment-resistant hypertension. Blood Press. 2015;24:263–74. doi: 10.3109/08037051.2015.1058595. doi: 10.3109/08037051.2015.1058595. [DOI] [PubMed] [Google Scholar]
- 2.Chen XH, Kim S, Zeng XX, Chen ZB, Cui TL, Hu ZX, et al. Account for clinical heterogeneity in assessment of catheter-based renal denervation among resistant hypertension patients: Subgroup meta-analysis. Chin Med J. 2017;130:1586–94. doi: 10.4103/0366-6999.208238. doi: 10.4103/0366-6999.208238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lin YH, Lee PC, Chang TP. Practical expert diagnosis model based on the grey relational analysis technique. Expert Syst Appl. 2009;36:1523–8. doi: 10.1016/j.eswa.2007.11.046. [Google Scholar]
- 4.Collins AJ, Foley RN, Herzog C, Chavers BM, Gilbertson D, Ishani A, et al. Excerpts from the US Renal Data System 2009 Annual Data Report. Am J Kidney Dis. 2010;55(1 Suppl 1):S1. doi: 10.1053/j.ajkd.2009.10.009. doi: 10.1053/j.ajkd.2009.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Annette F. Kidney cancer: Creating a molecular atlas of clear cell renal cell carcinoma genetics. Nat Rev Urol. 2013;9:489–92. doi: 10.1038/nrurol.2013.151. doi: 10.1038/nrurol.2013.151. [DOI] [PubMed] [Google Scholar]
- 6.Collins AJ, Foley RN, Herzog C, Chavers B, Gilbertson D, Herzog C, et al. US Renal Data System 2012 Annual Data Report. Am J Kidney Dis. 2013;61(1 Suppl 1):A7. doi: 10.1053/j.ajkd.2012.11.031. e1-476. doi: 10.1053/j.ajkd.2012.11.031. [DOI] [PubMed] [Google Scholar]
- 7.Dor A, Pauly MV, Eichleay MA, Held PJ. End-stage renal disease and economic incentives: The International Study of Health Care Organization and Financing (ISHCOF) Int J Health Care Finance Econ. 2007;7:73–111. doi: 10.1007/s10754-007-9024-9. doi: 10.1007/s10754-007-9024-9. [DOI] [PubMed] [Google Scholar]
- 8.Bansal N, Lin F, Vittinghoff E, Peralta C, Lima J, Kramer H, et al. Estimated GFR and subsequent higher left ventricular mass in young and middle-aged adults with normal kidney function: The Coronary Artery Risk Development in Young Adults (CARDIA) study. Am J Kidney Dis. 2016;67:227–34. doi: 10.1053/j.ajkd.2015.06.024. doi: 10.1053/j.ajkd.2015.06.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pilar, L Re: Positron emission tomography/computed tomography identification of clear cell renal cell carcinoma: Results from the REDECT trial. J Urol. 2013;190:493–8. doi: 10.1016/j.juro.2013.04.067. doi: 10.1016/j.juro. 2013.04.067. [DOI] [PubMed] [Google Scholar]
- 10.Daratha KB, Short RA, Corbett CF, Ring ME, Alicic R, Choka R, et al. Risks of subsequent hospitalization and death in patients with kidney disease. Clin J Am Soc Nephrol. 2012;7:409–16. doi: 10.2215/CJN.05070511. doi: 10.2215/CJN.05070511. [DOI] [PubMed] [Google Scholar]
- 11.Roderick PJ, Atkins RJ, Smeeth L, Mylne A, Nitsch DD, Hubbard RB, et al. CKD and mortality risk in older people: A community-based population study in the United Kingdom. Am J Kidney Dis. 2009;53:950–60. doi: 10.1053/j.ajkd.2008.12.036. doi: 10.1053/j.ajkd.2008.12.036. [DOI] [PubMed] [Google Scholar]
- 12.Just PM, de Charro FT, Tschosik EA, Noe LL, Bhattacharyya SK, Riella MC. Reimbursement and economic factors influencing dialysis modality choice around the world. Nephrol Dial Transplant. 2008;23:2365–73. doi: 10.1093/ndt/gfm939. doi: 10.1093/ndt/gfm939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ng LJ, Chen F, Pisoni RL, Krishnan M, Mapes D, Keen M, et al. Hospitalization risks related to vascular access type among incident US hemodialysis patients. Nephrol Dial Transplant. 2011;26:3659–66. doi: 10.1093/ndt/gfr063. doi: 10.1053/j.ajkd.2011.07.020. [DOI] [PubMed] [Google Scholar]
- 14.Collins AJ, Foley RN, Chavers B, Gilbertson D, Herzog C, Johansen K, et al. United States Renal Data System 2011 Annual Data Report: Atlas of chronic kidney disease and end-stage renal disease in the United States. Am J Kidney Dis. 2012;59:A7. doi: 10.1053/j.ajkd.2011.11.015. e1-420. doi: 10.1186/1471-2369-14-221.20. [DOI] [PubMed] [Google Scholar]
- 15.Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. doi: 10.1136/bmj.d5928. doi: 10.1136/bmj. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539–58. doi: 10.1002/sim.1186. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 17.McMillan DC. Inflammatory prognostic markers in clear cell renal cell carcinoma - Preoperative C-reactive protein does not improve predictive accuracy. BJU Int. 2013;111:E19–20. doi: 10.1111/bju.12020_12. doi: 10.1111/bju.12020_12. [DOI] [PubMed] [Google Scholar]
- 18.Gupta S, Kang HC, Ganeshan DM, Bathala TK, Kundra V. Diagnostic approach to hereditary renal cell carcinoma. AJR Am J Roentgenol. 2015;204:1031–41. doi: 10.2214/AJR.14.13514. doi: 10.2214/AJR.14.13514. [DOI] [PubMed] [Google Scholar]
- 19.Fadl Elmula FE, Hoffmann P, Larstorp AC, Fossum E, Brekke M, Kjeldsen SE, et al. Adjusted drug treatment is superior to renal sympathetic denervation in patients with true treatment-resistant hypertension. Hypertension. 2014;63:991–9. doi: 10.1161/HYPERTENSIONAHA.114.03246. doi: 10.1161/HYPERTENSIONAHA.114.03246. [DOI] [PubMed] [Google Scholar]
- 20.Kario K, Ogawa H, Okumura K, Okura T, Saito S, Ueno T, et al. SYMPLICITY HTN-Japan-First randomized controlled trial of catheter-based renal denervation in Asian patients. Circ J. 2015;79:1222–9. doi: 10.1253/circj.CJ-15-0150. doi: 10.1253/circj.CJ-15-0150. [DOI] [PubMed] [Google Scholar]


