Abstract
Background
Numerous studies have been performed to evaluate the efficacy of intralesional bleomycin for the treatment of warts with inconsistent result. Nevertheless, it is well known that the cytotoxicity of bleomycin can be enhanced in vivo by 300 to 700-fold by electroporation.
Objective and Methods
In this article, we present an interventional, one-center, prospective case series, clinical trial of the effectiveness of intralesional bleomycin combined with electroporation for the treatment of plantar warts, in comparison to the use of intralesional bleomycin alone.
Results
The study’s cohort included 12 men and 10 women, with a mean age of 53.8 years. A total of 22 warts were treated. In dividing the patients in two groups (complete remission against all the others) and analyzing the different outcomes in the two arms of patients, a statistical significant difference was found (p=0.0015), proving a greater efficacy of the treatment with bleomycin combined with ECT as opposed to bleomycin alone. Electroporation was always well tolerated by the patients with no discomfort.
Conclusions
This study serves as a basis for the application of novel protocols in the treatment of different benign and locally malignant skin lesion by means of electroporation.
Keywords: warts, electroporation, bleomycin
Introduction
Cutaneous warts are very common among dermatological diseases and are of benign nature. However, they can be extremely difficult to treat and can significantly impact quality of life [1,2]. Human papillomavirus, a double-stranded DNA virus, is the etiologic agent of warts. The most common sites of infection are the hands, feet, face, and the anogenital area [3]. Several different therapeutic approaches are possible, depending on lesion size, number and location, patient age and comorbidities, as well as adverse reactions associated with therapy [4]. Numerous studies have been performed to evaluate the efficacy of intralesional bleomycin for the treatment of warts with inconsistent result [5].
The uptake of this drug by the cells is slow and limited, because bleomycin can pass the cell membrane only through protein receptors due to its lipophobic nature [6]. In vitro studies, indeed, show evidence that less than 0.1% of bleomycin added to a culture medium becomes associated with the cell. Therefore, the high toxicity of bleomycin is weakened by its incapacity to freely diffuse through the cytoplasmic membrane [6]. Several studies have proved that the cytotoxicity of bleomycin can be enhanced in vivo by 300- to 700-fold by electroporation [7]. Electrochemotherapy (ECT) is a loco-regional therapy that is based on the application of permeabilizing electric pulses on tumors or tumor beds after the administration (either systemic or intralesional) of a chemotherapy agent [6]. In veterinary medicine, ECT is currently adopted as first-line therapy, generally in an adjuvant fashion, to improve the chemotherapeutic agent uptake by the neoplastic cells, thus resulting in better local control of the neoplastic disease [7]. In humans, its use is actually focused on palliation of cutaneous metastases of melanoma [8], but it is going to prove to be a valuable skin-directed therapy for a range of malignancies [9]. Among the numerous electroporation protocols implemented, our research group recently proposed a novel protocol involving the adoption of bursts of rectangular and biphasic pulses with a selected period of repetition [10]. This schedule enabled decreased morbidity of the treated animals and human beings as well as improving the clinical outcome [10].
In this study, we investigate the potential benefits of combining intralesional bleomycin with ECT for the treatment of plantar warts of big dimensions, with respect to the treatment with bleomycin alone.
Material and Methods
Study Description
This study is an interventional, one-center, prospective case series, clinical trial on the effectiveness of intralesional bleomycin combined with ECT for the treatment of plantar warts, in comparison to the use of intralesional bleomycin alone (EUDRACT N° 2014-003339-21).
Patients
Twenty-two patients with shave biopsy proven warts were recruited to participate in this study. Participation was on a volunteer basis, according to the principles of the Declaration of Helsinki. After detailed clinical assessment of the patient, information of the patient on all available alternative treatment options for her/his disease, information on ECT (application and expected results in comparison to other modalities, expected side effects and their management), and the aim of the present study, written informed consent was obtained and a structured follow-up program was discussed. Patients were evaluated for eligibility to participate in this study according to the criteria listed in Table 1. There were no demographic restrictions for the inclusion. All the patients were recruited from the Dermatology Service, Pius Hospital de Valls, Tarragona, Spain. Patients were randomly assigned to one of the two arms of the study (bleomycin alone and bleomycin combined with ECT). Of note, we did not test and stratify for HPV subtype the patients.
TABLE 1.
Selection criteria for the patients with warts
| Inclusion Criteria | Exclusion criteria |
|---|---|
| Histologically confirmed | Previous Reynaud phenomenon |
| Minimal size of the wart 0.5 cm | Heart patients |
| Plantar warts | Another wart less than 3 cm |
| Ability of patients to follow the instructions | Previous bleomycin use |
| Patients older than 18 | Patients younger than 18 |
Therapeutic protocol
Each patient signed a consent form. Clinical and dermoscopic images of lesions were taken using a Canon PowerShot G11 (Canon, Inc, Tokyo, Japan) camera followed by shave biopsy. Affected areas were anesthetized with subcutaneous lidocaine; block anesthesia was not performed. Overlying calluses were trimmed with a number 15 blade. Bleomycin in a concentration of 1 mg/cm3 was injected into verrucous foci at a depth of about 1.5 mm with a final volume of 0.1 cc. Patients enrolled in the arm including the ECT treatment, were subjected to trains of 8 biphasic pulses with an interpulse of 10 microseconds and a 50+50 microseconds duration, generated by an electroporator (Onkodisruptor®, Biopulse S.r.l., Naples, Italy). The pulses were delivered at a voltage of 700 V/cm, with 1 Hz frequency (total treatment time: 1 ms per cm2 of treated area). The pulses have been delivered by using caliper electrodes. In Figure 1, panel A, an example of calipers application on a plantar wart is depicted.
Figure 1.
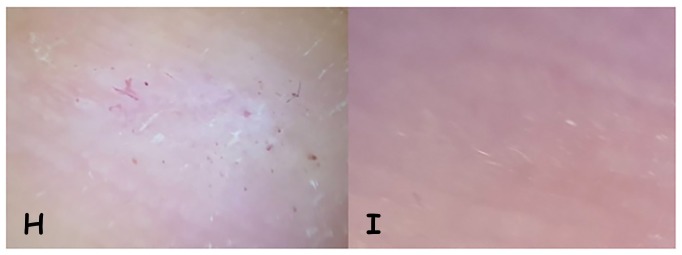
Two cases of plantar wart with partial or complete resolution after one month from the treatment with bleomycin and electroporation. (A) The application of the electrodes on the plantar wart; (B) A plantar wart at presentation; (C) Partial resolution after one month form the treatment; (D) Dermoscopic appearance of the wart at presentation; (E) Dermosocopic appearance of the wart after partial remission; (F) A plantar wart at presentation; (G) Complete resolution after one month form the treatment; (H) Dermoscopic appearance of the wart at presentation; I) Dermosocopic appearance of the wart after complete remission. [Copyright: ©2017 Pasquali et al.]
A pain scale (0, no pain; 10, maximum pain) was passed on each patient to evaluate pain during the procedure.
Data collection
Follow-up of the progress of the treatment process was scheduled at day 30 and day 90 after the treatment. The documentation plan during follow up, including photo-documentation of the treated area, consisted of evaluation of local treatment outcome, de novo appearance of skin warts, development of any disorders from any other organic system, as well as longtime outcome of the scarring process at the site of ECT treatment (“cosmetic result”). Treatment outcome was evaluated according to endpoint results, at the first or second follow-up appointment, 1 or 3 months after the end of treatment. The endpoints were defined as follows:
“Cured” (= complete remission, CR): no wart is detectable
“Partial response” as 50% wart reduction (PR)
“Non-responding”
“Progressive disease”: larger final wart
Statistical analysis
Fisher exact test was used to assess any difference in terms of response rate at the two time points between the control arm and the experimental arm. SPSS software (version 17.00, SPSS, Chicago) was used for statistical analysis. A P-value of less than 0.05 was considered to indicate statistical significance.
Results
Patient demographics
Characteristics of the patients enrolled in the protocol are depicted in Table 2. Briefly, the study’s cohort included 12 men and 10 women with ages ranging from 27 to 85 years, with a mean of 53.8 years. A total of 22 warts were treated, exclusively located on the feet. All patients were non-responders of other treatment modalities and had had a treatment history of more than 6 months.
TABLE 2.
Main clinical characteristics of the patients and outcome after one and three months
| Patient age | Sex | Treatment | Outcome after 30 days | Outcome after 90 days |
|---|---|---|---|---|
| 70 | Male | BL | PR | PR |
| 59 | Female | BL | PR | PR |
| 59 | Female | BL | PR | PR |
| 52 | Female | BL+E | PR | CR |
| 51 | Female | BL | PR | PR |
| 54 | Male | BL | NR | NR |
| 45 | Male | BL | CR | PR |
| 60 | Female | BL+E | PR | PR |
| 62 | Male | BL | PR | PR |
| 62 | Male | BL | PR | PR |
| 39 | Male | BL+E | NR | NR |
| 63 | Female | BL | PR | CR |
| 45 | Male | BL+E | CR | CR |
| 47 | Female | BL+E | CR | CR |
| 61 | Male | BL | PR | PR |
| 48 | Male | BL | PR | CR |
| 85 | Male | BL+E | CR | CR |
| 33 | Female | BL+E | CR | CR |
| 68 | Female | BL | PR | PR |
| 59 | Male | BL | NR | PR |
| 27 | Male | BL+E | PR | CR |
| 21 | Male | BL+E | PR | CR |
Efficacy
Table 2 summarizes the data obtained at 1 month and 3 months follow-up. Indeed, focusing on the 3-month follow-up, 78% (7/9) of patients treated with bleomycin coupled with ECT had complete remission and only 2 patients displayed partial remission or no response. On the other hand, at 3-month follow-up 16% (2/13) of patients treated with bleomycin had complete remission, while 76% (10/13) of patients displayed partial remission and 8% (1/13) had no response. Dividing the two groups of patients (complete remission against all the others) and analyzing the different outcomes in the two arms of treatment, a statistical significant difference was found (p=0.0015), proving a greater efficacy of the treatment with bleomycin combined with ECT with respect to bleomycin alone. In Figure 1 (Panels from B to I) two cases with partial or complete resolution of the wart after one month of treatment are depicted.
Side effects
Not one of the patients had adverse systemic effects. The most notable local side effect was he pain during the injection of local anesthetic. None complained of pain during intralesional bleomycin injection or during ECT. Other side effects were relatively infrequent, occasionally including redness and tenderness, and skin discoloration at the site of injection. One patient of arm A of the study reported pain on the third day after bleomycin injection. Concerning ECT treatment, it was always well tolerated by the patients without any discomfort.
Discussion
Bleomycin has been successfully used for the treatment of recalcitrant warts [11]. The most likely mechanism of action of this drug is the creation of unstable free radicals causing single-strand breaks and apoptosis [12]. Multiple bleomycin administration techniques have been studied with various success rates [11,13]. However, several intralesional bleomycin injections are generally necessary to obtain clearance of the warts [14]. Concerning side effects, injection pain is the most commonly described, while no systemic reactions have been linked with the use of bleomycin for warts [12]. Interestingly, a recent Cochrane meta-analysis has shown that the treatment of choice for warts remains ambiguous, despite the proved efficacy of intralesional bleomycin [15]. Several studies have demonstrated that the efficacy of bleomycin can be greatly improved by coupling its injection with electrical pulses enabling the cells to be more prone to incorporate bleomycin [7]. Indeed, bleomycin is one of the most used drugs in ECT protocols for the treatment of tumors [8].
A major goal of this project was to demonstrate an increased efficacy in the treatment of plantar warts with intralesional bleomycin coupled with electroporation. Indeed, the results of our study show that electroporation coupled with bleomycin significantly improve the outcome of patients with respect to the patients treated with bleomycin alone. Nevertheless, in our experimental protocol, only one intralesional injection of bleomycin was performed and, when coupled with electroporation, was sufficient to get complete remission in the majority of the patients with disappearance of the wart. This further supports the idea that electroporation is able to amplify the effect of bleomycin, since its efficacy in the treatment of warts is generally linked to multiple injections on the site of the wart [15]. The second goal of the project was to demonstrate that the application of electric voltage to the warts had no adverse side effects. Indeed, none of the patients suffered systemic side effects, and the only local adverse effects were the pain at the site of the injection and occasionally redness and tenderness of the skin. Electroporation was well tolerated by the patients without any discomfort.
The main limitation of our study was the small number of patients enrolled in the protocol. Therefore, additional studies are necessary to confirm the efficacy of electroporation coupled with bleomycin in treating plantar warts. Nevertheless, the promising results obtained, together with the fact that the treatment was well tolerated by all the patients, represent the basis for the application of novel protocols for the treatment of different benign and locally malignant diseases of the skin by means of electroporation.
Footnotes
Funding: None.
Competing interests: E.P. Spugnini and A. Baldi are stockholders in Biopulse s.r.l.
All authors have contributed significantly to this publication. P.P., A.F.M., S.G. performed the clinical trial; E.P.S. and A.B. performed the statistical analysis; P.P., E.P.S. and A.B. wrote the manuscript.
References
- 1.Ciconte A, Campbell J, Tabrizi S, Garland S, Marks R. Warts are not merely blemishes on the skin: a study on the morbidity associated with having viral cutaneous warts. Australas J Dermatol. 2003;44:169–173. doi: 10.1046/j.1440-0960.2003.00672.x. [DOI] [PubMed] [Google Scholar]
- 2.Gibbs S, Harvey I, Sterling J, Stark R. Local treatments for cutaneous warts: systematic review. BMJ. 2002;325:461. [PMC free article] [PubMed] [Google Scholar]
- 3.Cardoso JC, Calonje E. Cutaneous manifestations of human papillomaviruses: a review. Acta Dermatovenereol Alp Pannonica Adriat. 2011;20:145–154. [PubMed] [Google Scholar]
- 4.Rivera A, Tyirng SK. Therapy of cutaneous human papillomavirus infections. Dermatol Ther. 2004;17:4411–4418. doi: 10.1111/j.1396-0296.2004.04047.x. [DOI] [PubMed] [Google Scholar]
- 5.Buchanan J, Nieland-Fisher N. Document responses from patients regarding warts and current therapy. Arch Dermatol. 2004;140:487–488. doi: 10.1001/archderm.140.4.487. [DOI] [PubMed] [Google Scholar]
- 6.Spugnini EP, Azzarito T, Fais S, Fanciulli M, Baldi A. Electrochemotherapy as First Line Cancer Treatment: Experiences from Veterinary Medicine in Developing Novel Protocols. Curr Cancer Drug Targets. 2016;16:43–52. doi: 10.2174/156800961601151218155340. [DOI] [PubMed] [Google Scholar]
- 7.Spugnini EP, Baldi A. Electrochemotherapy in veterinary oncology: from rescue to first line therapy. Methods Mol Biol. 2014;1121:247–256. doi: 10.1007/978-1-4614-9632-8_22. [DOI] [PubMed] [Google Scholar]
- 8.Spugnini EP, Melillo A, Quagliuolo L, et al. Definition of novel electrochemotherapy parameters and validation of their in vitro and in vivo effectiveness. J Cell Physiol. 2014;229:1177–1181. doi: 10.1002/jcp.24548. [DOI] [PubMed] [Google Scholar]
- 9.Campana LG, Testori A, Curatolo P, et al. Treatment efficacy with electrochemotherapy: A multi-institutional prospective observational study on 376 patients with superficial tumors. Eur J Surg Oncol. 2016;42:1914–1923. doi: 10.1016/j.ejso.2016.06.399. [DOI] [PubMed] [Google Scholar]
- 10.Spugnini EP, Fais S, Azzarito T, Baldi A. Novel Instruments for the implementation of electrochemotherapy protocols: From bench side to veterinary clinic. J Cell Physiol. 2017;232:490–495. doi: 10.1002/jcp.25505. [DOI] [PubMed] [Google Scholar]
- 11.Kruter L, Saggar V, Akhavan A, et al. Intralesional bleomycin for warts: patient satisfaction and treatment outcomes. J Cutan Med Surg. 2015;19:470–476. doi: 10.1177/1203475415576860. [DOI] [PubMed] [Google Scholar]
- 12.Kollipara R, Ekhlassi E, Downing C, Guidry J, Lee M, Tyring SK. Advancements in pharmacotherapy for noncancerous manifestations of HPV. J Clin Med. 2015;4:832–846. doi: 10.3390/jcm4050832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lee JH, Burm JS, Yang WY, Kang SY, Byun SW. Treatment of verruca vulgaris in both external auditory canals using bleomycin injections. Clin Exp Otorhinolaryngol. 2015;8:295–297. doi: 10.3342/ceo.2015.8.3.295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dhar SB, Rashid MM, Islam A, Bhuiyan M. Intralesional bleomycin in the treatment of cutaneous warts: a randomized clinical trial comparing it with cryotherapy. Indian J Dermatol Venereol Leprol. 2009;75:262–267. doi: 10.4103/0378-6323.48428. [DOI] [PubMed] [Google Scholar]
- 15.Kwok CS, Gibbs S, Bennett C, Holland R, Abbott R. Topical treatments for cutaneous warts. Cochrane Database Syst Rev. 2012;9:CD001781. doi: 10.1002/14651858.CD001781.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]