Abstract
Introduction
In January 2009, Taiwan broadened smoke-free legislation, requiring mass transportation systems, indoor public areas and indoor workplaces with 3 or more people, to become smoke-free. We investigated the secondhand smoke (SHS) exposure at home for children aged 3–11 years in Taiwan before and after the implantation of the legislation.
Methods
We studied 7911 children from the 2005, 2009 and 2013 National Health Interview Surveys (cross-sectional, nationally representative household surveys). Logistic regression modelling estimated adjusted ORs (AOR) and 95% CIs for children's SHS exposure at home in 2009 and 2013 (2005 as reference) for the overall sample and for each category of household socioeconomic status (SES) and household composition.
Results
Prevalence of children SHS exposure at home decreased from 51% (2005) to 32% (2009) and 28% (2013). Compared to 2005, children in 2009 and 2013 had lower likelihoods of SHS exposure at home with AOR of 0.45 (95% CI 0.41 to 0.51) and 0.41 (95% CI 0.36 to 0.46), respectively. All children had reduced SHS exposure at home after the legislation, irrespective of household SES and compositions. Low household income, low parental education level, living with grandparents or living with other adults was individually associated with increased SHS exposure.
Discussion
The proportion of children exposed to SHS at home in Taiwan declined substantially from 2005 to 2009 after smoke-free legislation, and fell further by 2013, irrespective of SES and household compositions. Still, inequality in SHS exposure at home by SES and household composition warrants future research.
Keywords: Secondhand smoke, Public policy, Disparities
Introduction
The WHO has urged countries to adopt and enforce comprehensive smoke-free policies to protect people from the harms of secondhand smoke (SHS) as part of its Framework Convention on Tobacco Control.1 Accordingly, Taiwan implemented a Tobacco Hazards Prevention Act Amendment in January 2009; this required mass transportation systems, indoor public areas and indoor workplaces with three or more people, to become smoke-free.2 The Taiwan government also used various methods (eg, mass-media campaigns and community programmes) to raise awareness about the smoke-free legislation.2 The impact of the smoke-free legislation on reducing SHS exposure in workplace and homes in Taiwan has been investigated among smokers and non-smokers aged 15 upwards,3 and in non-smokers aged 18 or older.4 Both studies suggested that the 2009 smoke-free legislation had a short-term effect on reducing SHS in 2009,3 4 but SHS exposure at home rebounded in 2010 and 2011.4 However, the influence of smoke-free legislation in Taiwan on children's SHS exposure at home remained unknown.
Supporters of tobacco-smoke-free legislation argue that this increases public awareness about tobacco harms and encourages voluntary smoking restrictions at home, and many studies have affirmed decreased SHS exposure at home among adults after such legislation was implemented.5–7 However, others found that smoke-free legislation displaced public smoking to the home and thus increased SHS exposure at home among adults.8–10 Studies on children's SHS exposure at home also had contradictory results; for example, studies in England and Scotland found that smoke-free legislation reduced SHS exposure at home among children,11–14 but another in Hong Kong reported that smoke-free legislation had displaced smoking to young children's homes.15 US researchers found that more comprehensive smoking bans decreased children's SHS exposure, whereas bans limited to public recreational places increased their SHS exposure.16
Children from households with low socioeconomic status (SES) are more likely to be exposed to SHS;9 10 17–24 therefore, different impacts of smoke-free legislation on SHS exposure depending on household SES may affect existing inequalities in SHS exposure. Studies on the impact of smoke-free legislation on children's SHS exposure at home according to their household SES were equivocal. Some reported a decline in children's SHS exposure at home after smoke-free legislation, irrespective of household SES,20 25 and in one study children from households with the lowest SES had the greatest absolute reduction in SHS exposure at home.25 In other studies, children from low SES households or those with high SHS exposure levels before legislation did not benefit from smoke-free legislation as much as children from high SES households or with lower SHS exposure,26–28 which might worsen existing inequalities in SHS exposure. Despite these mixed findings, children from households with low SES still had high levels of SHS exposure, and inequality in SHS exposure at home did not decrease after smoke-free legislation was implemented.20 23 25–27
Although the main source of children's SHS exposure at home is parental smoking,29 non-parent household members or visitors may also expose children to SHS at home.30 Research in the USA found that children living in households headed by grandparents or non-parent adults were more likely than those living with parents to reside with at least one smoker.31 In Asia, multigenerational and extended families are common domestic structures and interpersonal relationships with frequent and reciprocal visitations are the norm.32–36 Therefore, Asian children may be more likely to be affected by non-parental smoking in their home.
It is uncertain how smoke-free legislation in Taiwan has affected children's SHS exposure at home. Moreover, there is a lack of empirical evidence regarding the influence of smoke-free legislation on children's SHS by their household SES in Asia. To the best of our knowledge, no studies in Asia have examined the contribution of non-parent household members to children's SHS exposure. Our objectives were to examine (1) children's SHS exposure at home before and after the implementation of the 2009 smoke-free legislation in Taiwan, overall and by household SES and household composition and (2) the association between household composition and children's SHS exposure at home.
Methods
Data source and sample
This study excerpted data on all participants aged 3–11 years from the 2005, 2009 and 2013 National Health Interview Survey (NHIS) in Taiwan. Each NHIS selected a nationally representative sample of non-institutional residents in Taiwan, using a multistage, stratified systemic sampling scheme with probability proportional to size.37 The response rates in 2005, 2009 and 2013 were 81%, 84%, and 75%, respectively, with sample sizes of 24 725, 25 636 and 23 296 individuals.37 Trained interviewers questioned participants to elicit sociodemographic, health-related, diet and lifestyle information.37 The NHIS used different questionnaires for participants younger than 12 years (reported by the caregiver) and 12 or older (self-reported). The final sample comprised 7911 participants aged 3–11 years (n=3200 in 2005; n=2657 in 2009 and n=2054 in 2013) after 287 (4%) participants with missing information were excluded (household income, n=266; SHS exposure, n=19; health status, n=2). All participants provided signed informed consent.
SHS exposure at home
The NHIS assessed children's exposure to SHS at home by asking primary caregivers: “During the last week, did anyone smoke in the child's presence when the child was at home?” The binary variables of SHS exposure at home were 1 for a ‘yes’ response, and 0 for ‘no’. Other responses, such as ‘unknown’ or ‘refused to answer’, were coded as missing. There were 19 participants with missing information on SHS exposure at home.
The 2009 smoke-free legislation and covariates
The primary independent variable was survey year: 2005, 2009 and 2013. The NHIS survey year was used as an instrumental variable to examine prevalence of children's SHS exposure at home before and after the implementation of the 2009 smoke-free legislation. SES included the highest parental education level and monthly household income (in New Taiwan Dollars, NTD). Categorical education levels included middle school or below, high school and college or above. Monthly household income (in nominal value) bands were ≤30 000, 30 001–50 000, 50 001–70 000, 70 001–100 000, and ≥100 001. Household composition included (1) number of parents living in the household (0 or 1 vs 2); (2) grandparents living in the household (yes or no) and (3) other adults living in the household (yes or no). Other adults referred to non-parental, non-grandparental relatives or unrelated adults. Other covariates included sex (male or female), age (3–5, 6–8 and 9–11 years) and binary health status (fair/poor/very poor and good/very good).
Statistical analysis
Multivariable logistic regression modelling was performed to investigate ORs and 95% CIs for children's SHS exposure at home in 2009 and 2013, respectively, using prevalence in 2005 as reference. Models included survey year, age, sex, health status, monthly household income, highest parental education level, number of parents, grandparents living in household and other adults living in household. We also performed stratified analyses by household SES and composition variables to examine changes of SHS exposure by survey years within each group (using prevalence in 2005 as reference). All estimates were weighted to each individual's probability of being sampled. Participants with any missing information were excluded for analysis. Data were analysed using STATA/IC (V.11.1, College Station, Texas, USA).
Results
Sample characteristics
Table 1 shows the demographic characteristics of participants in the 2005, 2009 and 2013 NHIS who were aged 3–11 years. The study sample comprised similar proportions of men and women across survey years. Proportionally less participants in 2005 than those in 2009 or 2013 were aged 9–11 years (34%, 37%, and 36%, p=0.028). The highest monthly household income and parental education levels were reported in 2013, when 38% of households had income >70 000 NTD, compared to 29–30% in the previous two surveys (p<0.001); 57% of household in 2013 had highest parental education of college or above, compared to 42–45% in 2005 and 2009 (p<0.001). Except for the proportions of children living with grandparents, household composition differed by survey year. In 2005, 2009 and 2013, respectively, there were 13%, 18% and 15% of children living with 0 or 1 parent (p<0.001) and 22%, 23%, and 26% living with other adults (p=0.008). About 43–45% of children lived with grandparents (p=0.547).
Table 1.
Demographic characteristics of 2005, 2009 and 2013 NHIS participants aged 3–11 years
| NHIS year: | Total (n=7911) | 2005 (n=3200) | 2009 (n=2657) | 2013 (n=2054) | |
|---|---|---|---|---|---|
| Variable | % (95% CI) | % (95% CI) | % (95%CI) | % (95% CI) | p Value* |
| Year | |||||
| 2005 | 40.6 (39.1 to 41.7) | ||||
| 2009 | 33.8 (33.1 to 34.5) | ||||
| 2013 | 25.6 (24.6 to 26.7) | ||||
| Sex | 0.465 | ||||
| Female | 47.8 (42.2 to 48.3) | 46.9 (46.0 to 47.9) | 48.0 (46.6 to 49.4) | 48.7 (46.5 to 50.9) | |
| Male | 52.2 (51.7 to 52.8) | 53.1 (52.1 to 54.0) | 52.0 (50.6 to 53.4) | 51.3 (49.1 to 53.5) | |
| Age (years) | 0.028 | ||||
| 3–5 | 31.7 (30.7 to 32.8) | 32.0 (30.2 to 33.8) | 30.9 (29.2 to 32.6) | 32.5 (30.8 to 34.3) | |
| 6–8 | 32.8 (32.0 to 33.6) | 34.5 (33.0 to 35.9) | 31.9 (30.1 to 33.7) | 31.4 (29.4 to 33.4) | |
| 9–11 | 35.5 (34.4 to 36.5) | 33.6 (31.9 to 35.3) | 37.2 (35.6 to 38.9) | 36.2 (34.0 to 38.4) | |
| Health status | 0.201 | ||||
| Fair/poor/very poor | 21.9 (20.1 to 23.7) | 22.9 (20.9 to 25.0) | 21.1 (18.4 to 24.1) | 21.2 (18.2 to 24.5) | |
| Good/very good | 78.2 (76.3 to 79.7) | 77.1 (75.0 to 79.1) | 78.9 (75.9 to 81.6) | 78.8 (75.5 to 81.8) | |
| Monthly household income (NTD) | <0.001 | ||||
| ≤30 000 | 16.0 (12.9 to 19.8) | 14.9 (11.2 to 19.6) | 19.7 (16.4 to 23.4) | 13.1 (10.0 to 16.9) | |
| 30 001–50 000 | 28.4 (25.3 to 31.7) | 30.1 (27.0 to 33.5) | 28.1 (24.4 to 32.1) | 26.0 (22.7 to 29.7) | |
| 50 001–70 000 | 23.7 (21.8 to 25.8) | 25.8 (22.9 to 28.9) | 22.0 (20.0 to 24.2) | 22.5 (19.5 to 25.8) | |
| 70 001–100 000 | 17.1 (14.8 to 19.7) | 16.6 (13.8 to 19.8) | 15.6 (13.0 to 18.5) | 20.1 (16.8 to 23.9) | |
| ≥100 001 | 14.7 (11.2 to 19.1) | 12.7 (9.3 to 17.0) | 14.6 (10.8 to 19.5) | 18.3 (14.1 to 23.4) | |
| Highest parental educational level | <0.001 | ||||
| Middle school or below | 11.1 (9.1 to 13.6) | 13.4 (11.2 to 16.0) | 10.3 (8.0 to 13.0) | 8.6 (6.4 to 11.5) | |
| High school | 41.2 (36.7 to 45.8) | 44.0 (39.6 to 48.5) | 43.6 (38.1 to 49.2) | 33.5 (29.0 to 38.4) | |
| College or above | 46.9 (40.5 to 53.4) | 42.0 (36.0 to 48.3) | 45.1 (37.5 to 53.0) | 57.0 (50.6 to 63.3) | |
| Other | 0.8 (0.5 to 1.2) | 0.5 (0.4 to 0.8) | 1.0 (0.6 to 1.9) | 0.8 (0.4 to 1.6) | |
| Household composition | |||||
| Number of parents | <0.001 | ||||
| 0 or 1 | 15.2 (13.6 to 16.9) | 13.3 (11.4 to 15.6) | 17.7 (15.8 to 19.8) | 14.7 (12.6 to 17.1) | |
| 2 | 84.8 (83.1 to 86.4) | 86.7 (84.4 to 88.6) | 82.3 (80.3 to 84.2) | 85.3 (82.9 to 87.4) | |
| Grandparents living in household | 0.547 | ||||
| No | 56.4 (51.4 to 61.3) | 56.8 (51.7 to 61.9) | 56.9 (52.4 to 61.3) | 55.2 (48.5 to 61.7) | |
| Yes | 43.6 (38.7 to 48.6) | 43.2 (38.1 to 48.4) | 43.1 (38.7 to 47.6) | 44.8 (39.3 to 51.5) | |
| Other adults living in household?† | 0.008 | ||||
| No | 76.9 (74.5 to 79.1) | 78.5 (75.9 to 81.0) | 76.7 (74.6 to 78.7) | 74.4 (70.6 to 77.9) | |
| Yes | 23.1 (20.9 to 25.5) | 21.5 (19.1 to 24.1) | 23.3 (21.3 to 25.4) | 25.6 (22.1 to 29.4) | |
*χ2 test.
†Other adults referred to non-parental, non-grandparental relatives or unrelated adults.
NHIS, National Health Interview Survey; NTD, New Taiwan Dollars.
Associations with SHS exposure at home
Survey year
Prevalence of children SHS exposure at home decreased from 51% in 2005 (prelegislation) to 32% in 2009 and 28% in 2013 (postlegislation) (table 2). Compared to year 2005, children in 2009 and 2013 had lower odds of SHS exposure at home, with multivariable-adjusted OR of 0.45 (95% CI 0.41 to 0.51) and 0.41 (95% CI 0.36 to 0.46), respectively.
Table 2.
Prevalence of and multivariable-adjusted ORs from logistic regression model for children SHS at home
| Prevalence of children SHS exposure at home (%) |
Multivariable-adjusted OR* (95% CI) |
|||
|---|---|---|---|---|
| NHIS year | 2005 | 2009 | 2013 | |
| Total proportion of children exposed | 51 | 32 | 28 | NA |
| Year | ||||
| 2005 | NA | NA | NA | Reference |
| 2009 | NA | NA | NA | 0.45 (0.41 to 0.51) |
| 2013 | NA | NA | NA | 0.41 (0.36 to 0.46) |
| Sex | ||||
| Female | 52 | 31 | 26 | Reference |
| Male | 49 | 34 | 30 | 1.01 (0.92 to 1.11) |
| Age (years) | ||||
| 3–5 | 47 | 33 | 25 | Reference |
| 6–8 | 49 | 33 | 30 | 1.06 (0.90 to 1.26) |
| 9–11 | 55 | 32 | 29 | 1.09 (0.95 to 1.24) |
| Health status | ||||
| Fair/poor/very poor | 54 | 38 | 35 | Reference |
| Good/very good | 49 | 31 | 26 | 0.82 (0.69 to 0.97) |
| Monthly household income (NTD) | ||||
| ≤30 000 | 60 | 50 | 44 | Reference |
| 30 001–50 000 | 57 | 38 | 35 | 0.88 (0.77 to 1.01) |
| 50 001–70 000 | 52 | 27 | 27 | 0.79 (0.66 to 0.96) |
| 70 001–100 000 | 40 | 19 | 17 | 0.61 (0.49 to 0.77) |
| ≥100 001 | 36 | 21 | 19 | 0.65 (0.53 to 0.78) |
| Highest parental education level | ||||
| Middle school or below | 68 | 59 | 45 | Reference |
| High school | 61 | 41 | 43 | 0.71 (0.55 to 0.92) |
| College or above | 33 | 18 | 17 | 0.26 (0.19 to 0.36) |
| Other | 83 | 63 | 42 | 1.06 (0.61 to 1.83) |
| Household composition | ||||
| Number of parents | ||||
| 0 or 1 | 57 | 39 | 38 | Reference |
| 2 | 51 | 31 | 28 | 1.15 (1.00 to 1.33) |
| Grandparents living in household? | ||||
| No | 45 | 27 | 22 | Reference |
| Yes | 58 | 40 | 36 | 1.44 (1.23 to 1.69) |
| Other adults living in household?† | ||||
| No | 47 | 29 | 25 | Reference |
| Yes | 62 | 46 | 38 | 1.41 (1.13 to 1.76) |
*Results from multivariable logistic regression model. Model included all covariates in the table.
†Other adults referred to non-parental, non-grandparental relatives or unrelated adults.
NA, not applicable; NTD, New Taiwan Dollars; SHS, secondhand smoke.
Household income
Children from families with household income below 30 000 NTD had the greatest SHS exposure in each survey (table 2). In 2005, 60% of children in the lowest household income group (≤30 000) were exposed to SHS at home, and the prevalence had dropped to 44% by 2013, which was still higher than the prevalence among the children in the highest income group in 2005 (36%) and prevalence in the two highest income groups in 2013 (17% and 19%). Household income >50 000 NTD was associated with lower likelihoods of SHS exposure at home, compared to the lowest income group, when controlled for survey year and other covariates.
Parental education level
Prevalence of children's SHS exposure at home in 2005, 2009 and 2013 was consistently high in families with parental education no higher than middle school (68%, 59% and 45%, respectively) and was lowest in families of parents with college education or above (33%, 18% and 17%, respectively) (table 2). Compared with children whose parents did not progress further than middle school, those whose parents had education of high school or college level or above were less likely to be exposed to SHS at home, with respective ORs of 0.71 (95% CI 0.55 to 0.92) and 0.26 (95% CI 0.19 to 0.36).
Household composition
Children SHS exposure at home was associated with household compositions (table 2). Children who lived with two parents had a lower prevalence of SHS exposure than children who lived with 0–1 parent. However, multivariable regression modelling suggested children lived with two parents had an insignificant higher odd of SHS exposure than those lived with 0–1 parent (OR 1.15, 95% CI 1.00 to 1.33). Children from households with grandparents were 44% (OR 1.44, 95% CI 1.23 to 1.69) more likely to be exposed to SHS compared with those with no grandparents. Having other adults living in household was also associated with higher children's SHS at home (OR 1.41, 95% CI 1.13 to 1.76).
Postlegislation SHS exposure by household SES and compositions
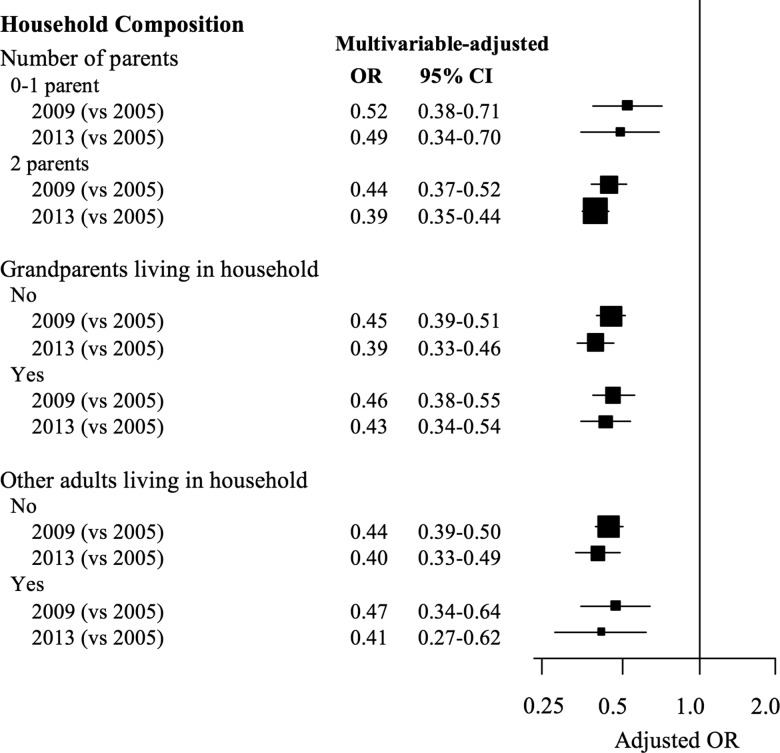
Prevalence of children SHS exposure at home decreased over time across categories of household income, highest parental education or household composition (table 2). Moreover, children in 2009 and 2013 had significantly lower odds of SHS exposure at home compared to children in 2005, irrespective of their household income, highest parental education level or household composition (figures 1 and 2), with two exceptions. That is, among children whose parents had no higher than middle school education, the OR estimate suggested lower SHS exposure in 2009 compared to 2005 although such an association did not reach statistical significance (OR 0.70, 95% CI 0.39 to 1.25; figure 1). Among children from households with income ≤30 000 NTD, the odds of SHS exposure at home in 2009 was lower than the comparable group in 2005 (OR 0.73, 95% CI 0.53 to 0.99; figure 1). In each category of household composition, SHS exposure in 2009 and 2013 was significantly lower than that in 2005, with ORs ranged from 0.39 to 0.52 (figure 2).
Figure 1.
Multivariable-adjusted OR (95% CI) for SHS exposure at home among children aged 3–11 years in 2009 and 2013 (compared with 2005) in each level of monthly household income, and highest parental education. Models included age, sex, heath status, monthly household income*, highest parental education*, number of parents, household with grandparents and household with other adults. Other adults included non-parental, non-grandparental relatives or unrelated adults. *The variable was excluded for stratified analysis by the variable. Bracket size is proportional to study sample size. SHS, secondhand smoke.
Figure 2.
Multivariable-adjusted OR (95% CI) for SHS exposure at home among children aged 3–11 years in 2009 and 2013 (compared with 2005) in each level of household composition, including number of parents, (yes/no) grandparents living in household or (yes/no) other adults living in household. Other adults included non-parental, non-grandparental relatives or unrelated adults. Models included age, sex, heath status, monthly household income, highest parental education, number of parents*, household with grandparents* and household with other adults*. *The variable was excluded for stratified analysis by the variable. Bracket size is proportional to study sample size.
Discussion
The 2009 smoke-free legislation
Using data excerpted from the Taiwan NHIS in 2005, 2009 and 2013, we found that children's exposure to SHS at home decreased significantly over these 8 years, during which smoke-free legislation was enacted in 2009. Before this smoke-free legislation, one in two children were exposed to SHS at home. SHS exposure at home among children subsequently fell by 19% in the year of the legislation (2009) and by 23% in 2013. Our findings suggested that estimated 1 353 108 children in 2005, 710 755 children in 2009 and 526 041 children in 2013 were potentially exposed to SHS at home in Taiwan. No evidence showed displacement of smoking from public places to home consequent to smoke-free legislation, implying that Taiwan's smoke-free legislation had a spillover effect in protecting children from SHS exposure at home. Similar to studies from other countries,11–15 this study provides evidence of a consistent population-level decline in prevalence of children's SHS exposure at home after introducing smoke-free legislation.
Interestingly and in contrast to adults, among whom the beneficial effect of smoke-free legislation on SHS exposure at home waned rapidly, the effect in children appeared to be sustained. According to the 2014 Annual Report on Tobacco Control in Taiwan, SHS exposure at home among adults decreased from 27% in 2008 to 21% in 2009, but has rebounded since 2010 and continued to rise to 25% in 2013.38 The differential impacts of smoke-free legislation on SHS exposure at home between children and adults might be explained by denormalisation of smoking in enclosed spaces with children present.13 23 That is, smoking adults residing with children may either avoid smoking near children or practice voluntary smoking restrictions at home to protect children. Such voluntary smoking restrictions may vary by the number and gender of parents who smoke;39 however, the NHIS data did not provide information for parents’ smoking status or type of home-smoking restriction.
Socioeconomic status
Children's exposure to SHS at home was associated with parental SES in this study. The prevalence of SHS exposure at home was highest for children in households with the lowest SES, either stratified by income or by parental educational level. Studies in Denmark and Scotland found that children from lower SES groups were exposed to a higher level of SHS at home, and a decline in SHS exposure at home was observed after the implantation of the smoke-free legislation among all children across SES groups.20 25 Similar to these studies, our study found a consistent reduction in SHS exposure at home for all children, regardless of household SES categories. For instance, the prevalence of SHS exposure at home reduced from 60% (2005, prelegislation) to 44% (2013, postlegislation) for children in the lowest household income group. The Scottish study further observed that children from households with the lowest SES experienced the greatest absolute reduction in SHS exposure at home.25 Our study, however, did not observe the greatest decline in children from the lowest household income group. Despite children from different household SES groups all experienced a reduction of SHS exposure at home after the implantation of the smoke-free legislation, children from low SES households in Taiwan still had a greater chance to be exposed to SHS than those from high SES households. Reducing the SHS exposure among children from low SES backgrounds remains a priority.
Interventions to promote voluntary smoking restrictions, particularly among lower SES households, may help to reduce children's SHS exposure at home. Current smoke-free legislation in Taiwan only prohibits smoking in public places and at work. Legislation against smoking at home is unlikely to prove acceptable or viable.40 41 At home, protection of children from SHS may rely on denormalisation of smoking near children and voluntary smoking restriction initiated by adults. Adults with high SES voluntarily restrict smoking more rapidly than adults of lower SES.13 24 Unequal responses to smoke-free legislation may lead to widening inequalities in children's health between households with higher versus lower SES. Governments should consider using national public health campaigns to raise awareness about the adverse effects of SHS for children and to encourage voluntary smoking restriction at home, especially among disadvantaged households.
Asian household structure
Kinship ties are particularly strong in most areas in Asia, the Middle East, South America and Sub-Saharan Africa. Large households that include relatives from outside the nuclear families are commonplace.34 Most western studies, mainly discussing the contribution of parental smoking to children's SHS exposure, have suggested that smoking parents, single-parent families and small dwelling size were associated with increased SHS exposure at home among children.24 Children's exposure to SHS at home in Asia may also be influenced by the presence of non-parent or non-grandparent smokers, such as extended family members and unrelated visitors. Different from previous studies,22 24 we found that children living with two parents had insignificantly greater odds of SHS exposure at home than children who lived with 0– 1 parent. Moreover, children who lived with grandparents or other adults are more likely to be exposed to SHS at home, compared with children who did not. These findings highlight the complexities of Asian household compositions and their associations with children's SHS exposure at home. On the other hand, after the smoke-free legislation, children from any household composition all experienced a reduction in SHS exposure at home, supporting the beneficial impact of this policy. Future studies and policy interventions should take into account extended family members and social networks.
Limitations and future research
This study of large, nationally representative samples provided prevalence of children's SHS exposure at home before, immediately after and 4 years following the implementation of smoke-free legislation in Taiwan. However, there were limitations. First, this study lacked objective measurements of SHS exposure, such as cotinine level in the urine and saliva, and used reports provided by primary caregivers. Although children's SHS exposure reported by parents was deemed reliable and valid,42–44 biases may still exist. For example, parents may hesitate to admit smoking near children due to denormalisation, which would underestimate exposure levels particularly after the implantation of smoke-free legislation and potentially overestimate the association between smoke-free legislation and SHS exposure among children. Second, we could not rule out a naturally decreasing trend in SHS exposure at home. Taiwanese government implemented graphic warning labels on cigarette packs and increased the earmarked tax in 2009. These policies may influence smoking prevalence and raise awareness of SHS harm on children's health, as one study suggested more comprehensive tobacco control policies, including smoke-free bans at work and in public, were associated with high prevalence of smoke-free homes in 27 European countries.45 Therefore, the reduction of SHS exposure at home among children might be a composite effect of three policies initiated in 2009. Third, income inflation was not adjusted for because household income was collected in category in questionnaires. Compared to 2005, the inflation rate in Taiwan was 5.08% in 2009 and 10.66% in 2013.46 Therefore, children in household with income ≤30 000 NTD in 2005 may be ‘richer’ than households with ≤30 000 NTD in 2009 and 2013. Fourth, the prevalence of SHS exposure was >20% and logistic regression modelling may overestimate associations. We tried to perform log-binomial regression modelling but models would not converge. Fifth, smoking behaviours of household members were unavailable in our data. Future research could examine prevalence of children's SHS exposure at home in non-smoking versus smoking households. Finally, it would be interesting to compare the SHS exposure in children aged 3–11 years versus those aged 12–18 years, although these two groups received different questionnaires to assess SES in the NHIS. Research of spillover effect of smoke-free legislation (voluntary smoking restriction at home) on SHS exposure by household characteristics in children of different age groups is warranted.
Conclusions
Our results show that SHS exposure at home among children in Taiwan has decreased substantially over 8 years since 2005, following smoke-free legislation in 2009 and subsequently. These trends are encouraging; displacement of SHS at home among children was not observed. Children from any group of household SES and compositions experienced a decreased SHS exposure at home. Nevertheless, children in low SES households and children living with grandparents and/or other adults still had greater SHS exposure at home. Public health workers and policymakers should be aware of these disparities. Overall, our study highlights essential factors to consider for tobacco control and reducing SHS exposure in children. Our results also provide empirical evidence for multiple international societies with extended family structures.
What this paper adds.
The 2009 smoke-free legislation in Taiwan reduced non-smoking adults’ exposure to secondhand tobacco smoke in 2009, yet this protective effect disappeared after 2010.
The impact of the smoke-free legislation in Taiwan on children's exposure to secondhand smoke (SHS) at home remained unknown.
Prevalence of children SHS exposure at home declined substantially from 2005 (51%) to 2009 (32%) after smoke-free legislation and fell further in 2013 (28%). Children from various household socioeconomic status (SES) and compositions all experienced a reduction in SHS exposure. Low SES and residing with grandparents or with other adults was individually associated with greater prevalence of exposure to SHS at home.
Footnotes
Contributors: All authors conceived the study, contributed to drafts and approved of the final version of the paper. Y-TW wrote the introduction section and revised the manuscript. Y-WT undertook the data analysis and completed the method section. T-IT wrote the discussion section. P-YC led the study design, completed the result section and revised the manuscript.
Funding: National Yang-Ming University received research funding from the tobacco health and welfare surcharges by the Health Promotion Administration for the project titled ‘International Collaborative Project for the Evaluation of Medical Services for Smoking Cessation’ (G1031227-105).
Disclaimer: The content of this article is solely the responsibility of the authors and does not necessarily represent the official views of the funding agency.
Competing interests: None declared.
Ethics approval: The study was approved by the Institutional Review Board (IRB) of National Yang-Ming University (YM104027E). Informed consent form was waived.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. World Health Organization. WHO report on the global tobacco epidemic, 2009: implementing smoke-free environments. World Health Organization, 2009. http://whqlibdoc.who.int/publications/2009/9789241563918_eng_full.pdf?ua=1 (accessed 7 Mar 2016). [Google Scholar]
- 2. Health Promotion Administration, Ministry of Health and Welfare ROC (Taiwan). Taiwan tobacco control annual report 2010. Health Promotion Administration, 2011. http://health99.hpa.gov.tw/media/public/pdf/21661.pdf (accessed 7 Mar 2016). [Google Scholar]
- 3. Chang FC, Chung CH, Chuang YC, et al. . Effect of media campaigns and smoke-free ordinance on public awareness and secondhand smoke exposure in Taiwan. J Health Commun 2011;16:343–58. 10.1080/10810730.2010.535110 [DOI] [PubMed] [Google Scholar]
- 4. Tsai YW, Chang LC, Sung HY, et al. . The impact of smoke-free legislation on reducing exposure to secondhand smoke: differences across gender and socioeconomic groups. Tob Control 2015;24:62–9. 10.1136/tobaccocontrol-2013-051004 [DOI] [PubMed] [Google Scholar]
- 5. Cheng KW, Glantz SA, Lightwood JM. Association between smokefree laws and voluntary smokefree-home rules. Am J Prev Med 2011;41:566–72. 10.1016/j.amepre.2011.08.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Lee JT, Agrawal S, Basu S, et al. . Association between smoke-free workplace and second-hand smoke exposure at home in India. Tob Control 2014;23:308–12. 10.1136/tobaccocontrol-2012-050817 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Mons U, Nagelhout GE, Allwright S, et al. . Impact of national smoke-free legislation on home smoking bans: findings from the International Tobacco Control Policy Evaluation Project Europe Surveys. Tob Control 2013;22:e2–9. 10.1136/tobaccocontrol-2011-050131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Erazo M, Iglesias V, Droppelmann A, et al. . Secondhand tobacco smoke in bars and restaurants in Santiago, Chile: evaluation of partial smoking ban legislation in public places. Tob Control 2010;19:469–74. 10.1136/tc.2009.035402 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. López MJ, Nebot M, Schiaffino A, et al. , Spanish Smoking Law Evaluation Group. Two-year impact of the Spanish smoking law on exposure to secondhand smoke: evidence of the failure of the ‘Spanish model’. Tob Control 2012;21:407–11. 10.1136/tc.2010.042275 [DOI] [PubMed] [Google Scholar]
- 10. Yao T, Lee AH, Mao Z. Potential unintended consequences of smoke-free policies in public places on pregnant women in China. Am J Prev Med 2009;37(2 Suppl):S159–64. 10.1016/j.amepre.2009.05.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Akhtar PC, Currie DB, Currie CE, et al. . Changes in child exposure to environmental tobacco smoke (CHETS) study after implementation of smoke-free legislation in Scotland: National Cross Sectional Survey. BMJ 2007;335:545 10.1136/bmj.39311.550197.AE [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Jarvis MJ, Feyerabend C. Recent trends in children's exposure to second-hand smoke in England: cotinine evidence from the Health Survey for England. Addiction 2015;110:1484–92. 10.1111/add.12962 [DOI] [PubMed] [Google Scholar]
- 13. Jarvis MJ, Sims M, Gilmore A, et al. . Impact of smoke-free legislation on children's exposure to secondhand smoke: cotinine data from the Health Survey for England. Tob Control 2012;21:18–23. 10.1136/tc.2010.041608 [DOI] [PubMed] [Google Scholar]
- 14. Sims M, Bauld L, Gilmore A. England's legislation on smoking in indoor public places and work-places: impact on the most exposed children. Addiction 2012;107:2009–16. 10.1111/j.1360-0443.2012.03924.x [DOI] [PubMed] [Google Scholar]
- 15. Ho SY, Wang MP, Lo WS, et al. . Comprehensive smoke-free legislation and displacement of smoking into the homes of young children in Hong Kong. Tob Control 2010;19:129–33. 10.1136/tc.2009.032003 [DOI] [PubMed] [Google Scholar]
- 16. Adda J, Cornaglia F. The effect of bans and taxes on passive smoking. Am Econ J Appl Econ 2010;2:1–32. 10.1257/app.2.1.1 [DOI] [Google Scholar]
- 17. Borland R, Yong HH, Cummings KM, et al. . Determinants and consequences of smoke-free homes: findings from the International Tobacco Control (ITC) Four Country Survey. Tob Control 2006;15(Suppl 3):iii42–50. 10.1136/tc.2005.012492 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Farkas AJ, Gilpin EA, White MM, et al. . Association between household and workplace smoking restrictions and adolescent smoking. JAMA 2000;284:717–22. 10.1001/jama.284.6.717 [DOI] [PubMed] [Google Scholar]
- 19. Gartner CE, Hall WD. Is the socioeconomic gap in childhood exposure to secondhand smoke widening or narrowing? Tob Control 2013;22:344–8. 10.1136/tobaccocontrol-2011-050297 [DOI] [PubMed] [Google Scholar]
- 20. Pisinger C, Hammer-Helmich L, Andreasen AH, et al. . Social disparities in children's exposure to second hand smoke at home: a repeated cross-sectional survey. Environ Health 2012;11:65 10.1186/1476-069X-11-65 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Sims M, Tomkins S, Judge K, et al. . Trends in and predictors of second-hand smoke exposure indexed by cotinine in children in England from 1996 to 2006. Addiction 2010;105:543–53. 10.1111/j.1360-0443.2009.02805.x [DOI] [PubMed] [Google Scholar]
- 22. Orton S, Jones LL, Cooper S, et al. . Predictors of children's secondhand smoke exposure at home: a systematic review and narrative synthesis of the evidence. PLoS One 2014;9:e112690 10.1371/journal.pone.0112690 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Moore GF, Moore L, Littlecott HJ, et al. . Prevalence of smoking restrictions and child exposure to secondhand smoke in cars and homes: a repeated cross-sectional survey of children aged 10–11 years in Wales. BMJ Open 2015;5:e006914 10.1136/bmjopen-2014-006914 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Bolte G, Fromme H, GME Study Group. Socioeconomic determinants of children's environmental tobacco smoke exposure and family's home smoking policy. Eur J Public Health 2009;19:52–8. 10.1093/eurpub/ckn114 [DOI] [PubMed] [Google Scholar]
- 25. Akhtar PC, Haw SJ, Levin KA, et al. . Socioeconomic differences in second-hand smoke exposure among children in Scotland after introduction of the smoke-free legislation. J Epidemiol Community Health 2010;64:341–6. 10.1136/jech.2008.084178 [DOI] [PubMed] [Google Scholar]
- 26. Moore GF, Currie D, Gilmore G, et al. . Socioeconomic inequalities in childhood exposure to secondhand smoke before and after smoke-free legislation in three UK countries. J Public Health (Oxf) 2012;34:599–608. 10.1093/pubmed/fds025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Moore GF, Holliday JC, Moore LAR. Socioeconomic patterning in changes in child exposure to secondhand smoke after implementation of smoke-free legislation in Wales. Nicotine Tob Res 2011;13:903–10. 10.1093/ntr/ntr093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Holliday JC, Moore GF, Moore LA. Changes in child exposure to secondhand smoke after implementation of smoke-free legislation in Wales: a repeated cross-sectional study. BMC Public Health 2009;9:430 10.1186/1471-2458-9-430 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Wakefield MA, Chaloupka FJ, Kaufman NJ, et al. . Effect of restrictions on smoking at home, at school, and in public places on teenage smoking: cross sectional study. BMJ 2000;321:333–7. 10.1136/bmj.321.7257.333 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Schuster MA, Franke T, Pham CB. Smoking patterns of household members and visitors in homes with children in the United States. Arch Pediatr Adolesc Med 2002;156:1094–100. 10.1001/archpedi.156.11.1094 [DOI] [PubMed] [Google Scholar]
- 31. King K, Martynenko M, Bergman MH, et al. . Family composition and children's exposure to adult smokers in their homes. Pediatrics 2009;123:e559–e64. 10.1542/peds.2008-2317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Cartier M. Nuclear versus quasi-stem families: the new Chinese family model. J Fam Hist 1995;20:307–27. 10.1177/036319909502000305 [DOI] [Google Scholar]
- 33. Zeng Y. A demographic analysis of family households in China, 1982–1995. J Comp Fam Stud 2002;33:15–34. [Google Scholar]
- 34. Ryberg R, Lippman LH, Wilcox WB, and DeRose L. World family indicators. In World Family Map 2015: mapping family change and child well-being outcomes. Child Trends, 2015. http://www.childtrends.org/wp-content/uploads/2015/09/2015-39WorldFamilyMap2015.pdf (accessed Mar 2016). [Google Scholar]
- 35. Chang HC, Holt GR. More than relationship: Chinese interaction and the principle of Kuan-Hsi. Commun Quart 1991;39:250–71. 10.1080/01463379109369802 [DOI] [Google Scholar]
- 36. King AYC. Kuan-Hsi and network building: a sociological interpretation. Daedalus 1991;120:63–84. [Google Scholar]
- 37. Health Promotion Administration, Ministry of Health and Welfare ROC (Taiwan). National Health Interview Survey (NHIS). http://www.hpa.gov.tw/English/ClassShow.aspx?No=200803270010 (accessed 7 Mar 2016).
- 38. Health Promotion Administration, Ministry of Health and Welfare ROC (Taiwan). Taiwan Tobacco Control Annual Report 2014. Health Promotion Administration, 2015. (accessed 7 Mar 2016) http://www.hpa.gov.tw/English/file/ContentFile/201503030535456577/Taiwan%20Tobacco%20Control%20Annual%20Report%202014.pdf [Google Scholar]
- 39. Akhtar PC, Haw SJ, Currie DB, et al. . Smoking restrictions in the home and secondhand smoke exposure among primary schoolchildren before and after introduction of the Scottish smoke-free legislation. Tob Control 2009;18:409–15. 10.1136/tc.2009.030627 [DOI] [PubMed] [Google Scholar]
- 40. Chapman S. The future of smoke-free legislation. BMJ 2007;335:521–2. 10.1136/bmj.39315.616169.BE [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Greaves LJ, Hemsing NJ. Sex, gender, and secondhand smoke policies: implications for disadvantaged women. Am J Prev Med 2009;37(2 Suppl):S131–7. 10.1016/j.amepre.2009.05.012 [DOI] [PubMed] [Google Scholar]
- 42. Avila-Tang E, Elf JL, Cummings KM, et al. . Assessing secondhand smoke exposure with reported measures. Tob Control 2013;22:156–63. 10.1136/tobaccocontrol-2011-050296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Matt GE, Hovell MF, Zakarian JM, et al. . Measuring secondhand smoke exposure in babies: the reliability and validity of mother reports in a sample of low-income families. Health Psychol 2000;19:232 10.1037/0278-6133.19.3.232 [DOI] [PubMed] [Google Scholar]
- 44. Matt GE, Wahlgren DR, Hovell MF, et al. . Measuring environmental tobacco smoke exposure in infants and young children through urine cotinine and memory-based parental reports: empirical findings and discussion. Tob Control 1999;8:282–9. 10.1136/tc.8.3.282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Martínez-Sánchez JM, Blanch C, Fu M, et al. . Do smoke-free policies in work and public places increase smoking in private venues? Tob Control 2014;23:204–7. 10.1136/tobaccocontrol-2012-050877 [DOI] [PubMed] [Google Scholar]
- 46. Directorate-General of Budget, Accounting and Statistics, Executive Yuan, ROC (Taiwan). National Statistics Website http://win.dgbas.gov.tw/dgbas03/latestind-pca.asp?i=21 (accessed 1 Jul 2016).