The Editor,
Iatrogenic diversion of inferior vena cava (IVC) to left atrium had been reported many times.[1,2,3,4,5,6,7,8] In few reported cases, this complication was detected years after surgery.[2] Transesophageal echocardiography (TEE) is instrumental in timely diagnosis of such surgical errors and helps in immediate correction of such complication.[3] We describe a case of ostium secundum atrial septal defect (ASD) repair surgery where intraoperative TEE has helped in diagnosis and correction of the complication, on operation table itself. TEE is said to be critically important for the open heart surgeries. A 27-year-old female patient who was diagnosed to have ostium secundum ASD with absent IVC rim was referred to cardiac surgery department for surgical repair. ASD device closure was not possible due to absent IVC rim.
This patient was taken to the operation room for surgery. Anesthesia was induced uneventfully. Pulse oximeter, electrocardiography, end-tidal carbon dioxide, arterial blood pressure, temperature, and urine output were monitored. TEE probe was inserted through mouth for intraoperative echo monitoring. Large 32 mm ostium secundum ASD with right atrium (RA) and right ventricle (RV) volume overload was noted on TEE. Left ventricle (LV) was small. Pulmonary veins were draining to the left atrium. Cardiopulmonary bypass (CPB) was instituted and RA was opened after cardioplegic arrest of heart. ASD was located posteroinferiorly. IVC rim was absent. Right pulmonary veins were identified. They were opening into the left atrium. Pericardial patch repair was done. The patient was weaned from CPB. RA and RV were empty and contracting very well. There was dramatic improvement in heart size and contractility. Superior vena caval and IVC cannulae were removed. Saturation on pulse oximeter dropped down to 75% with FiO20.6. We searched for lung pathology like lung collapse or pneumothorax but both the lungs were getting ventilated. Airway pressures were normal. FiO2 increased to one, but there was no improvement in saturation. TEE showed empty RA and RV while LV was full. Mid-esophageal bicaval view at 100° with color Doppler showed IVC flowing into LA instead of RA [Figure 1a]. Iatrogenic right to left shunt was recognized. This finding explained empty right heart and desaturation. The patient was again cannulated; CPB was reinstituted. After cardioplegic arrest, RA was opened. Pericardial patch was removed, and anatomy of ASD was again inspected. The patch was again revised. The patient was weaned from CPB. Successful correction was confirmed by TEE examination [Figure 1b].
Figure 1.
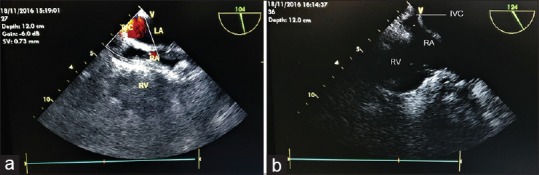
(a) Mid-esophageal bicaval view shows inferior vena cava flowing into the left atrium on color Doppler mode after initial atrial septal defect repair. (b) Mid-esophageal bicaval view shows inferior vena cava flowing into right atrium (after correction of error)
Discussion
ASD repair is considered as relatively a short and easy procedure by many.
Inadvertent diversion of IVC to the left atrium is a very rare complication. Bjork et al. (1958) described this complication during and after operation when hypothermia had been used along with occlusion of inflow to RA.[4] This complication happens in cases when ASD is located posteroinferiorly near IVC, and inferior margin near IVC is deficient or absent.[5] If this valve is wrongly taken as the lower margin of the defect and used when repairing the defect, the IVC would then be connected to the left atrium and not to the right.[1,3,5,6,7,8] It may cause acute or chronic hypoxemia and stroke. This complication is also seen in case of IVC type of sinus venosus ASD.[1,5] In the presence of a large Eustachian valve, valve rim is mistaken for the margin of ASD.[1] There is one more possibility of inadvertent diversion when the lower parts of defect are too low to be seen.[1,5,6] In the presence of a large Eustachian valve, surgeon may mistakenly close the gap from the valve toward the upper septal margin rather than posterior ASD itself.[6] Ross and Johnson described that a distortion of the IVC orifice by a snare may lead to mistake in identifying lower edge of atrial septum.[8] Same thing had happened in this case also. In previously reported cases, cardiac catheterization had been used to diagnose this complication.[1,2,8] Contrast like 5% dextrose saline injected from veins of lower extremities, had been used to diagnose this complication with the help of Transthoracic Echocardiography.[2,5,6] Hybrid cath laboratory, a new emerging trend, where operation theater and catheterization laboratory exist in the same room, can be very useful in such situations.
In this case, defect was located posteroinferiorly near IVC. It was very difficult to appreciate anatomy of ASD because of lack of IVC rim. After weaning from CPB, dramatic improvement in heart size was noted. RA and RV were collapsed because IVC was not flowing to the RA. However, LV was well filled because it was getting filled from IVC. This iatrogenic diversion of right to left shunt had led to fall in saturation. Diversion of the blood from the IVC into the left atrium is a serious complication. Many patients in whom the mistake has not been corrected had died on table.[4] Many of such catastrophes had not been reported.[4] Few cases had been diagnosed after few years also.[2,4] Whenever desaturation is noticed in ASD repair, this type of complication should be suspected. TEE was very helpful in diagnosing the error and helped in immediate correction without morbidity and mortality. Transcatheter ASD device closure may avoid such complications, but whenever IVC rim is absent, patients are deferred from device closure and sent for open heart surgery.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Lee YW, Lee WC, Chua S. Identifying diversion of inferior vena cava after repair of atrial septal defect. Int J Cardiovasc Imaging. 2015;31:1447–9. doi: 10.1007/s10554-015-0695-x. [DOI] [PubMed] [Google Scholar]
- 2.Jain SA, Pinto R, Dalvi B. Iatrogenic diversion of IVC to left atrium after surgical closure of ASD. Ann Pediatr Cardiol. 2012;5:72–4. doi: 10.4103/0974-2069.93716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tempe Deepak K, Sonal S. The utility of transoesophageal echocardiography for detecting residual shunt in a patient undergoing atrial septal defect repair. Anaesth Analg. 2007;104:777–8. doi: 10.1213/01.ane.0000256913.47302.c7. [DOI] [PubMed] [Google Scholar]
- 4.Bjork VO, Johansson L, Jonsson B, Norlander O, Nordenstrom B. The operation and management of a case after diversion of the inferior vena into the left atrium after the open repair of an atrial septal defect. Thorax. 1958;13:261–6. doi: 10.1136/thx.13.4.261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Thompson E, Moritz D, Perdue R, Cansino S. Diversion of the inferior vena cava following repair of atrial septal defect causing hypoxemia. Echocardiography. 2004;21:329–32. doi: 10.1111/j.0742-2822.2004.02089.x. [DOI] [PubMed] [Google Scholar]
- 6.Beitzke D, Koestenberger M, Knez I, Beitzke A. Anomalous connection of the inferior vena cava to the left atrium: A surgical error in closing an atrial septal defect. Clin Res Cardiol. 2008;97:191–3. doi: 10.1007/s00392-007-0628-3. [DOI] [PubMed] [Google Scholar]
- 7.Zhang Y, Song H, Qiao X, Xiao X, Liu J, Wang X. Detection and diagnosis of iatrogenic inadvertent diversion of partial inferior vena cava into the left atrium by transesophageal echocardiography during large posteroinferior surgical atrial septal defect closure. J Anesth. 2015;29:442–5. doi: 10.1007/s00540-014-1925-4. [DOI] [PubMed] [Google Scholar]
- 8.Ross JK, Johnson DC. Complications following closure of atrial septal defects of the inferior vena caval type. Thorax. 1972;27:754–8. doi: 10.1136/thx.27.6.754. [DOI] [PMC free article] [PubMed] [Google Scholar]


