Abstract
Background:
Chronic kidney disease (CKD) in reproductive-age women is accompanied by menstrual and fertility disorders and premature menopause.
Objective:
We sought to determine nephrologists’ and allied health care providers’ perceptions on management of sex hormone status in women with CKD.
Methods:
An anonymous, Internet-based survey was sent to nephrology society members from Canada, Australia, New Zealand, and the United Kingdom, and the Canadian Association of Nephrology Nurses and Technologists (February-November 2015). We assessed reported perceptions and management of sex hormone status in women with CKD.
Results:
One hundred seventy-five nephrologists (21% response rate) and 121 allied health care providers (30%; 116 nurses, 5 pharmacists) responded. Sixty-eight percent of nephrologists and 46% of allied providers were between the ages of 30 and 50 years, and 38% of nephrologists and 89% of allied workers were female. Ninety-five percent of nephrologists agreed that kidney function impacts sex hormone status, although only a minority of nephrologists reported often discussing fertility (35%, female vs male nephrologists, P = .06) and menstrual irregularities with their patients (15%, female vs male nephrologists,P = .02). Transplant nephrologists reported discussing fertility more often than did nontransplant nephrologists (53% vs 30%, P = .03). Physicians were more likely to report discussing fertility (33% vs 7.5%, P < .001) and menstrual irregularities (15% vs 9%, P = .04) with patients than allied health care providers. Forty-three percent of physicians reported uncertainty about the role for postmenopausal hormone therapy in women with CKD.
Conclusion:
Nephrologists and allied health care providers recognize an impact of CKD on sex hormones in women but report not frequently discussing sex hormone–related issues with patients. Our international survey highlights an important knowledge gap in nephrology.
Keywords: chronic kidney disease, nephrologist, survey, estradiol, sex hormone, hormone therapy, women
Abrégé
Contexte:
Chez les femmes en âge de procréer, l’insuffisance rénale chronique (IRC) peut être associée à des irrégularités du cycle menstruel, des problèmes de fertilité et à la survenue d’une ménopause précoce.
Objectifs de l’étude:
Cette étude visait deux objectifs. D’abord, on a voulu connaître la manière dont les néphrologues et les autres professionnels de la santé perçoivent les troubles hormonaux associés à l’IRC chez les femmes en âge de procréer. Ensuite, nous souhaitions établir comment ces perceptions influencent la prise en charge des patientes.
Méthodologie:
Entre février et novembre 2015, nous avons fait parvenir un sondage Web anonyme aux membres de la Société de néphrologie du Canada, de l’Australie, de la Nouvelle-Zélande et du Royaume-Uni, de même qu’aux membres de l’Association canadienne des infirmières et infirmiers et des technologues de néphrologie (ACITN/CANNT). Nous avons compilé et analysé les réponses obtenues au sujet des perceptions et de la prise en charge de l’activité hormonale dans le suivi des femmes atteintes d’IRC.
Résultats:
Un total de 175 néphrologues (taux de réponse de 21 %) et de 123 autres professionnels de la santé, soit 116 infirmières et 5 pharmaciens (taux de réponse de 30 %) ont répondu au sondage. Les répondants étaient majoritairement âgés de 30 à 50 ans (68 % des néphrologues et 46 % des autres professionnels de la santé). Un peu plus du tiers des néphrologues étaient des femmes (38 %) alors que ces dernières représentaient la très grande majorité (89 %) des autres professionnels de la santé ayant répondu au sondage. La plupart des néphrologues (95 %) ont admis que la fonction rénale perturbe l’activité des hormones sexuelles chez leurs patientes, bien qu’une minorité reconnaissait discuter des enjeux liés à la fertilité (35 %) et des irrégularités du cycle menstruel (15 %) avec elles. Dans les deux cas, bien que les différences ne soient pas statistiquement significatives, les néphrologues féminines étaient plus nombreuses que leurs collègues masculins à aborder ces sujets de façon régulière avec leurs patientes (ratio homme-femme p=0,06 pour l’infertilité, et p=0,02 pour les irrégularités du cycle menstruel). De plus, le sondage indique que les néphrologues transplantologues abordent plus souvent les questions de fertilité avec leurs patientes que les néphrologues qui ne pratiquent pas de greffes (53 % contre 30 %, p=0,03). De manière générale, les médecins se montraient plus enclins à discuter des problèmes de fertilité (33 % contre 7,5 %, p<0,001) et des irrégularités du cycle menstruel (15 % contre 9 %, p=0.04) avec les patientes atteintes d’IRC que les autres professionnels de la santé. Enfin, en ce qui concerne le suivi des cas de ménopause précoce, 43 % des médecins se sont dits incertains quant au rôle que pourrait jouer l’hormonothérapie post-ménopausique pour les femmes atteintes d’IRC.
Conclusion:
De manière générale, les néphrologues et les autres professionnels de la santé admettent que l’activité des hormones sexuelles est influencée par la fonction rénale chez les femmes atteintes d’IRC. Néanmoins, ils reconnaissent ne pas aborder d’emblée les enjeux de fertilité et les irrégularités du cycle menstruel associés à l’IRC avec leurs patientes. Ainsi, ce sondage mené à l’international témoigne d’un écart important entre les connaissances et les pratiques dans le domaine de la néphrologie.
What was known before
Chronic kidney disease (CKD) is commonly associated with menstrual disorders, infertility, and premature menopause. Nephrologists are often considered as the primary care providers by their patients, but perceptions of nephrologists and renal allied health care providers on management of these issues are currently unknown.
What this adds
While nephrologists and allied health care providers recognize the impact of CKD on sex hormone status in women, they reported not frequently discussing menstrual disorders, fertility, and menopause with their female patients with CKD, highlighting an important knowledge gap in nephrology.
Introduction
Chronic kidney disease (CKD) affects 8% to 16% of individuals globally.1 In women with CKD, disruptions in gonadotropin-releasing hormone (GnRH) production result in an abnormal sex hormone profile, ultimately resulting in low levels of estradiol2-4 and commonly leading to early menopause, menstrual disorders, and infertility in women with both dialysis and non-dialysis-dependent CKD.5 Fertility rates among women of childbearing age with CKD are low,6-9 and complications to both mother and fetus are high when pregnancy occurs,9,10 highlighting the importance of discussion of the potential risks of contraception11-13 compared with the risks of pregnancy. The mean age at menopause is 4 years earlier in women with end-stage kidney disease (ESKD) compared with the general population.14
International guidelines suggest that women with premature menopause in the general population use hormone therapy (HT) until the median age of natural menopause for symptom management,15-18 although this has never been addressed in guidelines relevant to the CKD population. Studies on the role of HT in the CKD population are limited.19-25 Given the high prevalence of menstrual, pregnancy, and fertility disorders coupled with the early menopause observed in the CKD population, we sought to determine how health care providers in nephrology approach management of sex hormone status in women with CKD.
Methods
Survey Development
A survey instrument (Appendix 1) was developed with input from a group of 15 physicians (experts in the field of nephrology [n = 13], endocrinology [n = 1], and cardiology [n = 1]) and nephrology nurses (n = 3). Item generation was developed through a combination of literature review and consultation with experts in the field as outlined above. An assessment of the face validity, clarity, length, and completeness of the survey was performed through semistructured interviews (pre-testing) with nephrologists. The instrument was pilot tested on 6 nephrologists.
Survey Administration
An e-mail cover letter explaining the purpose of the study and a link providing access to the secure, web-based survey were sent to 2441 members of the Canadian (n = 285) and Australia and New Zealand (n = 850) Nephrology Societies, the British Renal Society (n = 1306), and the Canadian Association of Nephrology Nurses and Technologists (n = 456) between February and November 2015. All physicians and allied health care providers (nurses and pharmacists) were recruited through memberships to these organizations. The study remained open 2 months after the initial e-mail contact. Reminder e-mails were sent up to 3 times, each at least 2 weeks apart. In addition, the survey was included in the monthly International Society of Nephrology (n = 9000) electronic newsletter for July and September 2015. The survey was disseminated in June 2015 and again in August 2015 via Twitter by the International Society of Nephrology.
Information was collected on demographics, type of nephrology practice, perceptions on discussion of fertility, menstrual cycle irregularities and menopause with patients, and opinions on use of postmenopausal HT in women with CKD. The responses for questions were assessed for frequency (never, rarely, sometimes, often, or always) or agreement (strongly disagree, disagree, neither agree nor disagree, agree, strongly agree, or I do not know). In addition, each question included an optional free form comment section. Clinical sensibility was assessed by reviewing the comments from the survey sent to the Canadian Society of Nephrology, and the survey was modified to include a question to further assess type of practice (adult, pediatric, or both) such that the survey link to the British Renal Society, Australian and New Zealand Society of Nephrology, the International Society of Nephrology, and the Canadian Association of Nephrology Nurses and Technologists included a question regarding pediatric versus adult nephrology practice.
Ethics approval for the study was obtained from the University of Calgary Conjoint Health Research Ethics Board. Participation in the study was voluntary, and informed consent was obtained electronically as part of the survey.
Data Analysis
The primary goal was to describe the perceptions of nephrologists and allied health care providers on the importance and frequency of discussing sex hormone status with their female patients with CKD, and their opinions on use of HT in women with CKD. We compared the responses from female and male nephrologists, as it has been reported that physicians use fewer resources to treat the genital-specific conditions of same-sex patients.26 All data were used to conduct stratified statistical analyses using the Pearson chi-squared test. Further comparisons were made between transplant and nontransplant nephrologists, physicians, and allied health care workers and geographical location using ordinal logistic and logistic regressions. For the qualitative analysis, each free form response was analyzed collectively by 2 reviewers (S.R. and S.B.A.), comments were reduced to broader themes by inductively developing categories, and recurrent ideas were grouped into themes which were then reported. There was consensus between the 2 reviewers.
Results
Demographics
There were 296 respondents (158 nephrologists, 17 medical trainees in nephrology, 121 nephrology allied health care providers [116 nurses and 5 pharmacists]) to the survey. The average response rate was 21.2% (47%, 8.4%, 1.3%, and 28%, respectively, for the Canadian Society of Nephrology, British Renal Society, Australian and New Zealand Society of Nephrology, and Canadian Association of Nephrology Nurses and Technologists). In addition, 0.2% of the membership from the International Society of Nephrology responded to the survey, though the low response rate was expected due to the fact that the Canadian and Australia and New Zealand Societies of Nephrology also form part of the International Society of Nephrology.
Table 1 summarizes the demographic characteristics of the respondents. Sixty-eight percent of the nephrologists were between the ages of 30 and 50 years, and 38% of nephrologists were female. There was a broad range in terms of length of practice with the majority practicing nephrology in a clinical and academic setting. Twenty percent of the physicians were transplant nephrologists. Of the 55 nephrologists and trainees in nephrology respondents where this information was available, 4% of nephrologist respondents were primarily involved in pediatric practice.
Table 1.
Baseline Characteristics of All Respondents.
| Nephrologist and medical trainees |
Allied health care provider |
||||||
|---|---|---|---|---|---|---|---|
| All (N = 296) | % Female (n = 67) |
% Male (n = 108) |
P value (χ2) | % Female (n = 108) |
% Male (n = 13) |
P value (χ2) | |
| Age, y | .04 | .18 | |||||
| <30 | 5.74 | 4.63 | 13.43 | 1.85 | 7.69 | ||
| 30-40 | 25.34 | 34.33 | 31.48 | 14.81 | 15.38 | ||
| 41-50 | 34.12 | 35.82 | 36.11 | 28.7 | 53.85 | ||
| 51-60 | 30.07 | 10.45 | 22.22 | 50.93 | 23.08 | ||
| 61-70 | 3.38 | 5.97 | 1.85 | 3.7 | 0 | ||
| >70 | 1.35 | 0 | 3.7 | 0 | 0 | ||
| Years of practice | .528 | .01 | |||||
| <5 | 15.88 | 29.85 | 19.44 | 2.78 | 23.08 | ||
| 5-10 | 16.55 | 20.9 | 23.15 | 6.48 | 23.08 | ||
| 10-15 | 19.59 | 23.88 | 24.07 | 12.96 | 15.38 | ||
| 15-20 | 11.15 | 11.94 | 10.19 | 12.04 | 7.69 | ||
| 20-25 | 10.47 | 4.48 | 8.33 | 16.67 | 7.69 | ||
| > 25 | 26.35 | 8.96 | 14.81 | 49.07 | 23.08 | ||
| Type of practicea | |||||||
| Clinical | 65.54 | 61.19 | 63.89 | 72.22 | 46.15 | ||
| Academic | 61.73 | 50.75 | 68.52 | 9.26 | 23.08 | ||
| Community | 12.84 | 11.94 | 12.96 | 13 | 15.38 | ||
| Research | 19.93 | 32.84 | 20.37 | 12.03 | 15.38 | ||
| Education | 27.36 | 31.34 | 22.22 | 30.56 | 23.08 | ||
| Administrative | 11.49 | 14.93 | 12.04 | 8.33 | 15.38 | ||
| Transplant | .351 | .2 | |||||
| Yes | 11.82 | 16.42 | 22.22 | 1.85 | 7.69 | ||
| No | 88.18 | 83.58 | 77.78 | 98.15 | 92.31 | ||
| Patient population | (n = 168) | (n = 26) | (n = 31) | .086 | (n = 103) | (n = 8) | .351 |
| Adult | 93.45 | 92.31 | 90.32 | 95.15 | 87.5 | ||
| Pediatric | 2.38 | 0 | 9.68 | 1.94 | 0 | ||
| Both | 4.17 | 7.69 | 0 | 2.91 | 12.5 | ||
Categories not mutually exclusive.
Forty-six percent of the allied health care providers (nurses and pharmacists) were between the ages of 30 and 50 years and 89% of them were female. Fifty-six percent of the allied health care respondents reported being in nephrology practice for greater than 25 years. None of the allied health care respondents worked primarily with a transplant population, and 2% reported being primarily involved in pediatric practice.
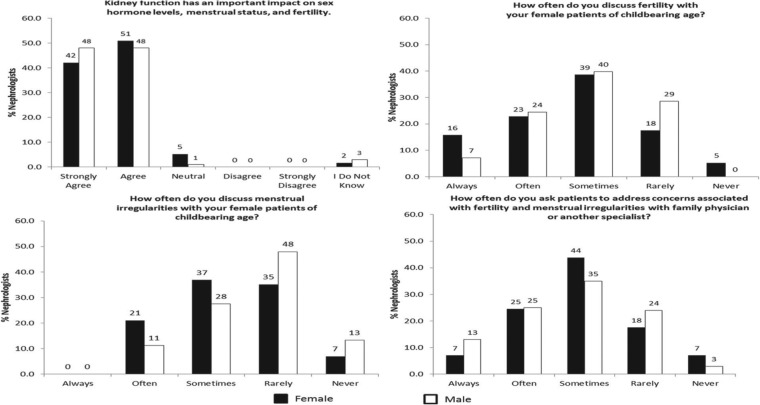
Impact of Kidney Disease on Sex Hormones and Discussion of Symptoms
The perceptions of nephrologists on sex hormone status and kidney function are summarized in Figures 1 to 4. Ninety-five percent of the respondents strongly agreed or agreed that kidney function has an important effect on sex hormone status, but only a third of respondents reported often or always discussing fertility and even fewer (15%) reported always or often discussing menstrual irregularities with their female patients of childbearing age. Although there were no statistically significant differences between female and male nephrologists in how often they reported discussing fertility (P = .06), female nephrologists reported more frequently discussing menstrual irregularities with their patients (P = .02) (Figure 1). Transplant nephrologists were more likely to report discussing fertility with their female patients (53% transplant vs 30% nontransplant nephrologist, P = .03). There were no differences based on geographical location of the respondents. As only 4% of the nephrologists reported having a mainly pediatric practice, we were unable to analyze the difference between adult and pediatric nephrologists.
Figure 1.
Nephrologists’ impressions of sex hormone status in chronic kidney disease.
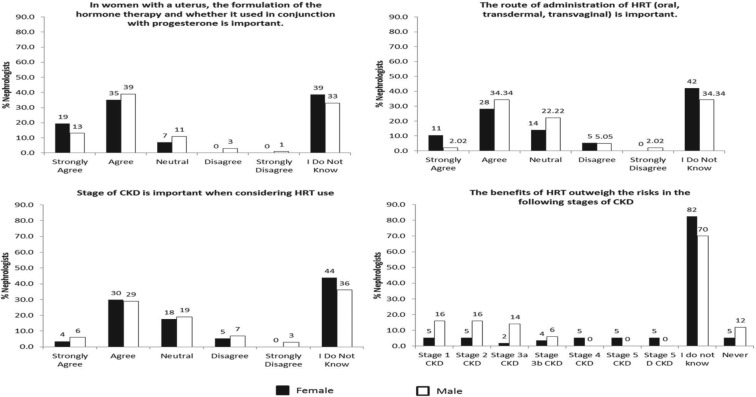
Figure 4.
Nephrologist impression on factors to consider for hormone therapy in CKD.
Note. CKD = chronic kidney disease; HRT = hormone replacement theory.
Thirteen percent of respondents provided optional comments. The main themes that emerged from qualitative analyses were that discussions regarding fertility were focused on either contraception counseling in the setting of use of teratogenic drugs or pre–kidney transplant, or when prescribing drugs associated with the potential to cause ovarian failure. In addition, some physicians outlined that discussion of fertility with their patients was not warranted because the female patients in their practice were mainly older women.
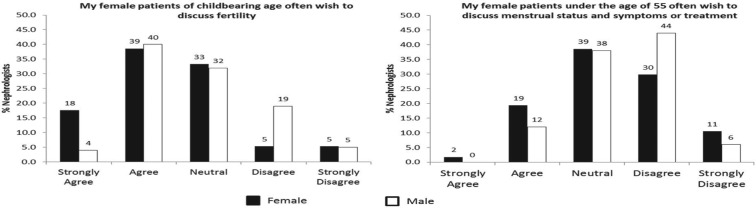
Forty-eight percent of the nephrologists believed their female patients of childbearing age wished to discuss fertility and 15% to discuss menstrual status and menopause. Female nephrologists stated that their female patients brought up issues about fertility with them more frequently than did male nephrologists (P = .03); however, this gender difference was not observed for patients discussing menstrual status or menopause (P = .14; Figure 2). Female patients were reported to bring up issues about fertility more often by transplant than nontransplant nephrologists (67% transplant vs 45% nontransplant nephrologist, P = .01). Despite respondents reporting that patients wished to discuss concerns associated with fertility and menstrual irregularities, only 35% of the respondents asked patients to address these concerns with their family physician or another physician (endocrinologist or gynecologist). This was not different between female and male nephrologists (P = .53).
Figure 2.
Nephrologists’ impressions of patient discussion of sex hormone status in chronic kidney disease.
Among allied health care providers, 87% agreed or strongly agreed that kidney function has an important impact on sex hormone status; however, very few reported always or often discussing fertility (7.5%) or menstrual irregularities (9%) with their female patients. This was significantly different from that reported by physicians (fertility: P < .001; menstrual irregularities: P = .04). Twenty-seven percent of allied health care providers agreed or strongly agreed that their female patients of childbearing age wished to discuss fertility often and 30% wished to discuss menstrual abnormalities or menopause. Allied health care providers were less likely to report that their female patients wished to discuss fertility (P < .001) but more likely to report that female patients wished to discuss menstrual irregularities (P = .003) compared with physicians.
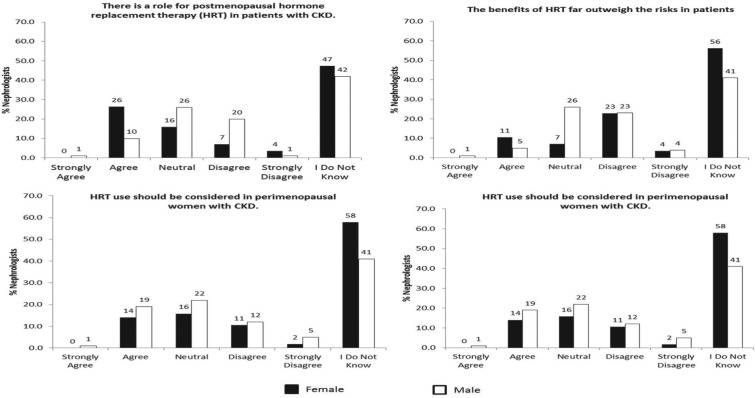
Postmenopausal HT
Forty-three percent of the physicians reported an uncertainty for the role for postmenopausal HT in women with CKD; 17% agreed or strongly agreed that there is a role for HT in women with CKD. When asked whether the benefits of HT outweigh the risks in patients with CKD, 46% of the physicians reported they did not know (Figure 3). Furthermore, 47% and 45% reported they did not know whether HT should be considered in perimenopausal and postmenopausal women with CKD, respectively.
Figure 3.
Nephrologists’ impressions of hormone therapy in CKD.
Note. CKD = chronic kidney disease; HRT = hormone replacement therapy.
Fifty-three percent of the respondents agreed or strongly agreed that the formulation of HT and whether it is used in conjunction with progesterone are important in women with a uterus, and 35% reported they did not know. Similarly, 37% agreed or strongly agreed that the route of HT administration is important, and 37% reported they did not know. Thirty-four percent of the physicians agreed or strongly agreed that the stage of CKD should be considered for HT use while 39% reported they did not know. When asked at what stage of CKD the benefits of HT outweigh the risks, 75% reported they did not know (Figure 4).
Among allied health care professionals, 57% reported they did not know whether there is a role for HT in women with CKD and 58% reported they did not know whether the formulation of HT should be taken into consideration for women with CKD. Forty-one percent reported they did not know whether the route of administration is important to take into consideration for women with CKD.
When asked about HT prescription practice prior to the publication of the Women’s Health Initiative (WHI) trials in 2002,27 47% of the physicians reported they were not in nephrology practice prior to 2002, 5.8% reported they often prescribed HT, and 37% reported they did not prescribe HT. In contrast, 83% stated they did not prescribe HT after the WHI trials were published. Among the 5% of physicians who provided written comments on HT prescription practice, some suggested that they were likely to recommend HT for symptom relief in their female patients with CKD (Appendix 2). Thematic analysis of the comments from the survey is presented in Appendix 2.
Discussion
This cross-sectional survey examined the views of nephrologists and allied health care professionals on the impact of kidney disease on sex hormone status. We found that while nephrologists and allied health care professionals recognize the important effects of kidney disease on sex hormone status in women with CKD, reported discussion of the sequelae of low estradiol levels such as infertility, menstrual disorders, or premature menopause with their patients was limited. In addition, there was a high level of uncertainty in the nephrology community regarding the role of HT.
There was significant variability in the responses stratified by gender, transplant and nontransplant nephrologists, and physicians and allied health care providers. Female nephrologists were more likely to report discussing menstrual irregularities with their patients, and transplant nephrologists reported discussing fertility more often than nontransplant nephrologists. Physicians were more likely to report discussing fertility and menstrual irregularities with their female patients than allied health care providers. In addition, while only 35% of clinicians asked patients to address concerns associated with fertility and menstrual irregularities with their family doctor or refer them to another physician, this could be because few reported often discussing issues regarding fertility and menstrual irregularities with their patients.
Despite awareness that kidney disease–mediated abnormalities in sex hormone levels are common, nephrologists and allied health care workers reported uncertainties regarding the role for HT in the CKD population. The results of this study suggest that while the nephrology community is aware of the impact of CKD on sex hormone status with patients, incorporation of this knowledge into clinical practice is more limited.
In women with CKD, disruptions in GnRH production result in an abnormal sex hormone profile leading to low levels of estradiol, though the pathophysiology remains unclear.2-4,28,29 Low levels of estradiol result in symptoms such as decrease in fertility and sexual desire, menstrual abnormalities, hot flashes, sleep disturbances, and mood changes which are associated with a decrease in quality of life, at least in women without CKD.30-32 Fertility rates among women of childbearing age with CKD are low6-8; however, complications to both mother and fetus are high when pregnancy occurs.10 A study of 100 women with CKD reported that 88% had menstrual problems or were menopausal, with 20% of menopausal women being <40 years of age.5 A previous cross-sectional study examining gynecological issues in 76 women on dialysis showed that 59% of women reported irregular menses.33 In addition, a meta-analysis of women with CKD found that the prevalence of sexual dysfunction as defined by decreased sexual desire ranged from 30% to 80%.34 This suggests that women with CKD have a significant burden of signs and symptoms associated with low estradiol levels.
There may be several reasons why nephrologists reported not often discussing fertility, menstrual irregularities, and menopause with their female patients. First, they may feel this falls outside their domain of expertise or the primary purpose of their clinical encounter with the patient. Second, it has been shown that in patients with chronic conditions with multiple comorbidities, disease states not prominently related to the primary condition are often not addressed.35 Given the disease burden of the average CKD patient, there may be inadequate time to address issues related to sex hormone status.36,37 Third, as suggested by Cochrane and Regan,5 although nephrologists are often considered the primary care provider by their patients,38 women with CKD may not raise gynecological issues for discussion with their nephrologists as these concerns may appear less important in comparison with other kidney-related health issues. Transplant nephrologists reported discussing fertility with their female patients of childbearing age more often than nontransplant nephrologists. This could be due to the younger age of patients receiving transplant39 and the recommendation to avoid pregnancy within the first 1 to 2 years of transplant, coupled with the necessary prescription of potentially teratogenic medications in this setting.
Women with kidney disease experience cessation of menses significantly earlier than do the general population, and while there are no CKD-specific recommendations, international guidelines suggest that women with premature menopause initiate HT until the natural age of menopause.15-18 Our survey highlights that nephrologists and other allied health care providers are not confident discussing or prescribing HT in women with CKD. The knowledge gap on this issue likely reflects the paucity of literature on HT in this population; few studies have examined the role of HT specifically in women with kidney disease.19-25 It is possible that discussion of clinical sequelae of low estrogen levels is limited due to lack of evidence for a viable treatment option in this population. Further clinical trials are required to determine the effectiveness and safety of postmenopausal HT in women with CKD.
When and how to incorporate discussion regarding contraception, fertility, and menopause with the female CKD patient is beyond the scope of this study. However, raising these issues common to all women as part of the initial consult would ensure that patients and their health care providers recognize that kidney disease has an important impact on sexual, hormonal, and gynecologic aspects to their care.
Limitations
The limitations of our survey include the self-reported nature of the data, as well as the possibility of differences in practice between respondents and nonrespondents. The generalizability of our study may be limited. First, the physician sample self-identified as mainly nephrologists in academic practice and was derived through membership to nephrology societies of high-income countries, which may not accurately capture global practice. Second, the survey response rate was low; however, our average response rate of 21% is comparable with the typical 20% response rate to online surveys of clinicians.40,41 Third, the majority of respondents were from the Canadian societies, and thus, the results of the survey primarily reflect perceptions from a Canadian perspective. Our sample may be enriched for female nephrologists, because 38% of the nephrologist respondents were women, as compared with a recent estimate of the proportion of female nephrologists (34%).42 This was a preliminary survey designed to determine the initial impressions of nephrologists on the impact of sex hormones on CKD; as such, questions exploring reasons for the lack of discussion on CKD and sex hormones in a clinical setting were not explored. Further studies are required to better understand the conclusions of this study. This study is also limited by the lack of objective definitions of options like often and rarely; however, to avoid floor and ceiling effects of this Likert scale, we included several options in the Likert scale and an open-ended comment section. Nephrology practices commonly include elderly populations, and it is possible that increased patient age may play a role in the reported lack of discussion of sex hormone status and its sequelae; however, the survey questions were specific to age-appropriate patient populations. Lastly, studies have suggested that social desirability bias results in the tendency of survey respondents to answer questions in a manner that will be viewed favorably by others43; thus, actual discussion rates of issues related to sex hormone status in women with CKD may be lower. However, a recent meta-analysis has suggested that computer-based survey may limit social desirability bias,44 though this has been disputed.43
Conclusion
In an international survey of nephrologists and renal allied health care providers, we found that while physicians and allied health care providers were aware of the impact of CKD on sex hormone levels, discussion and management of menstrual irregularities, fertility, and menopausal status were reported to be relatively infrequent. There was a high level of uncertainty among nephrologists with regard to the role of HT in women with CKD. In identifying this important knowledge and practice gap, we have highlighted the need for further study of this common clinical issue in women with CKD and the need for education for clinicians and allied health care providers on advising women with CKD on infertility and menopause.
Appendix 1: Survey
Sex Hormones in Chronic Kidney Disease
I understand the above stated purpose of this survey and consent to the use of my responses for the purpose of academic research:
○ Yes
○ No
Demographic Information
1. Age
○ 30-40 Years
○ 41-50 Years
○ 51-60 Years
○ 61-70 Years
○ >70 Years
2. Sex
○ Male
○ Female
3. Years of Practice
○ 5-10 Years
○ 10-15 Years
○ 15-20 Years
○ 20-25 Years
○ 25 Years
4. How are you involved in nephrology practice?
○ Nephrologist
○ Medical trainee in nephrology
○ Nurse practitioner
○ Nurse
○ Other (please specify) ______________________
5. Type of Practice (check all that apply)
⧠ Academic
⧠ Community
⧠ Clinical
⧠ Education
⧠ Administrative
⧠ Research
⧠ Other (Please Specify) ______________________
6. Are you a transplant nephrologist?
○ Yes
○ No
7. What type of patients are in your practice?
○ Pediatric
○ Adult
○ Both
Please answer the following based on your personal clinical practice
1. How often do you discuss fertility with your female patients of childbearing age? (Number of comments: 31)
○ Never
○ Rarely
○ Sometimes
○ Often
○ Always
Comments (optional)

2. How often do you discuss menstrual irregularities with your female patients of childbearing age? (Number of comments: 17)
○ Never
○ Rarely
○ Sometimes
○ Often
○ Always
Comments (optional)

3. How often do you ask patients to address concerns associated with fertility and menstrual irregularities with their family doctor or refer them to another physician (endocrinologists or gynecologists)? (Number of comments: 13)
○ Never
○ Rarely
○ Sometimes
○ Often
○ Always
Comments (optional)

To what extent do you agree or disagree with the following statements:
4. Kidney function has an important impact on sex hormone levels, menstrual status, and fertility. (Number of comments: 3)
○ Strongly Agree
○ Agree
○ Neutral
○ Disagree
○ Strongly Disagree
○ I Do Not Know
Comments (optional)

5. My female patients of childbearing age often wish to discuss fertility. (Number of comments: 15)
○ Strongly Agree
○ Agree
○ Neutral
○ Disagree
○ Strongly Disagree
Comments (optional)

6. My female patients under the age of 55 often wish to discuss menstrual status and symptoms or treatment of menopause. (Number of comments: 13)
○ Strongly Agree
○ Agree
○ Neutral
○ Disagree
○ Strongly Disagree
Comments (optional)

7. There is a role for postmenopausal hormone replacement therapy (HRT) in patients with CKD. (Number of comments: 15)
○ Strongly Agree
○ Agree
○ Neutral
○ Disagree
○ Strongly Disagree
○ I Do Not Know
Comments (optional)

8. The benefits of HRT far outweigh the risks in patients with CKD. (Number of comments: 12)
○ Strongly Agree
○ Agree
○ Neutral
○ Disagree
○ Strongly Disagree
○ I Do Not Know
Comments (optional)

9. In women with a uterus, the formulation of the hormone therapy and whether it used in conjunction with progesterone is important. (Number of comments: 6)
○ Strongly Agree
○ Agree
○ Neutral
○ Disagree
○ Strongly Disagree
○ I Do Not Know
Comments (optional)

10. The route of administration of HRT (oral, transdermal, transvaginal) is important. (Number of comments: 2)
○ Strongly Agree
○ Agree
○ Neutral
○ Disagree
○ Strongly Disagree
○ I Do Not Know
Comments (optional)

11. I often prescribed HRT PRIOR to the Women’s Health Initiative (WHI) trials (JAMA 2002). (Number of comments: 18)
○ Strongly Agree
○ Agree
○ Neutral
○ Disagree
○ Strongly Disagree
○ I Do Not Know
○ I was not in nephrology practice prior to 2002
Comments (optional)

12. I often prescribe HRT AFTER the Women’s Health Initiative (WHI) trials (JAMA 2002). (Number of comments: 28)
○ Strongly Agree
○ Agree
○ Neutral
○ Disagree
○ Strongly Disagree
○ I Do Not Know
Comments (optional)

13. Stage of CKD is important when considering HRT use. (Number of comments: 6)
○ Strongly Agree
○ Agree
○ Neutral
○ Disagree
○ Strongly Disagree
○ I Do Not Know
Comments (optional)

14. The benefits of HRT outweigh the risks in the following stages of CKD (check all that apply). (Number of comments: 9)
⧠ Stage 1 CKD
⧠ Stage 2 CKD
⧠ Stage 3a CKD
⧠ Stage 3b CKD
⧠ Stage 4 CKD
⧠ Stage 5 CKD
⧠ Stage 5 D CKD
⧠ I do not know
⧠ HRT should never be prescribed to CKD patients
Comments (optional)

15. HRT use should be considered in perimenopausal women with CKD. (Number of comments: 12)
○ Strongly Agree
○ Agree
○ Neutral
○ Disagree
○ Strongly Disagree
○ I Do Not Know
Comments (optional)

16. HRT use should be considered in postmenopausal women with CKD. (Number of comments: 17)
○ Strongly Agree
○ Agree
○ Neutral
○ Disagree
○ Strongly Disagree
○ I Do Not Know
Comments (optional)

Appendix 2: Thematic Analysis
1. How often do you discuss fertility with your female patients of childbearing age? (n = 31)
| Fertility discussed if prescribing angiotensin converting enzyme inhibitor or angiotension receptor blocker |
| Fertility discussed if patient was undergoing a transplant or post transplant |
| Fertility discussed if patient was having immunosuppression |
2.How often do you discuss menstrual irregularities with your female patients of childbearing age? (n = 17)
| Patient asked to discuss this with general practitioner |
| If patient has dysmenorrhea |
3. How often do you ask patients to address concerns associated with fertility and menstrual irregularities with their family doctor or refer them to another physician (endocrinologists or gynecologists)? (n = 13)
| Referred for discussing birth control |
| Referred based on patient concerns |
4. Kidney function has an important impact on sex hormone levels, menstrual status, and fertility. (n = 3)
| Not aware of any associations |
5. My female patients of childbearing age often wish to discuss fertility. (n = 15)
| Patient dependent |
| Patients want to talk post-transplant |
| Depends on stage of CKD |
6. My female patients under the age of 55 often wish to discuss menstrual status and symptoms or treatment of menopause. (n = 13)
| Patients only bring it up if significant symptoms occur |
| Patients bring it up in pre-dialysis clinic |
7. There is a role for postmenopausal hormone replacement therapy (HRT) in patients with CKD. (n = 16)
| Only in symptomatic women |
| Lack of strong evidence supporting HRT |
| Have to take cardiovascular risk into consideration |
8. The benefits of HRT far outweigh the risks in patients with CKD. (n = 12)
| Not according to recommendations or evidence |
| CKD patients have a higher risk than the general population |
| Dependent on quality of life versus heart disease |
9. In women with a uterus, the formulation of the hormone therapy and whether it used in conjunction with progesterone is important. (n = 10)
| Similar to the general population |
| Have to consider long term risk of malignancy |
| Not aware for CKD population |
10. The route of administration of HRT (oral, transdermal, transvaginal) is important. (n = 2)
| Patient dependent |
11. I often prescribed HRT PRIOR to the Women’s Health Initiative (WHI) trials (JAMA 2002). (n = 18)
All comments regarding not being licensed to prescribe
12. I often prescribe HRT AFTER the Women’s Health Initiative (WHI) trials (JAMA 2002). (n = 28)
All comments regarding not being licensed to prescribe
13. Stage of CKD is important when considering HRT use. (n = 6)
| There is a lack of evidence |
14. The benefits of HRT outweigh the risks in the following stages of CKD (check all that apply). (n = 9)
| They may for the short term |
| If patients are symptomatic |
| Dependent on outcome – quality of life versus cardiovascular risk |
15. HRT use should be considered in perimenopausal women with CKD. (n = 12)
| If the patient is symptomatic |
| Dependent on patient preference |
| Dependent on risk of cardiovascular disease and osteoporosis |
16. HRT use should be considered in postmenopausal women with CKD. (n = 17)
| Dependent on symptoms |
| Insufficient evidence |
Footnotes
Author Contributions: SR, MTJ, SBW, JMH-L, EWS, DCW, and SBA conceived the research idea and designed the study; SR and SBA performed statistical analyses; and MTJ, SBW, JMH-L, EWS, DCW, and SBA edited the draft. Each author provided important inputs during the manuscript drafting and revision.
Ethics Approval and Consent to Participate: This research project was approved by the University of Calgary Conjoint Health Research Ethics.
Consent for Publication: We have the authors consent for publication.
Availability of Data and Materials: The web based survey instrument is available at online appendix 1. The data is available upon request.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: S.R. is supported by the Canadian Institutes of Health Research, William Davies Scholarship, and the Roy and Vi Baay Chair in Kidney Research. J.M.H.-L. is funded as the Scientific Director of the Seniors Health Strategic Clinical Network within Alberta Health Services. S.B.W. is supported by a grant from St. Jude Medical and Alberta Health Services. M.T.J. is supported by a KRESCENT new investigator award. E.W.S. is supported by a National Institutes of Health grant. DCW is currently funded by the UK National Kidney Research Fund, the British Heart Foundation, the British Renal Society, and the Baxter Healthcare Extramural Grant Program. He has also received research funding from Merck and Amgen, has undertaken consultancy work for Fresenius, serves on the UK and European Advisory Boards of Genzyme, and has been paid lecture fees by Bristol-Myers Squibb, Novartis, Wyeth, and Fujisawa. S.B.A. is supported by Alberta Innovates: Health Solutions. Funding sources had no role in the study design, in the writing of the report, and in the decision to submit the article for publication.
References
- 1. Jha V, Garcia-Garcia G, Iseki K, et al. Chronic kidney disease: global dimension and perspectives. Lancet. 2013;382:260-272. [DOI] [PubMed] [Google Scholar]
- 2. Swamy AP, Woolf PD, Cestero RV. Hypothalamic-pituitary-ovarian axis in uremic women. J Lab Clin Med. 1979;93:1066-1072. [PubMed] [Google Scholar]
- 3. Zingraff J, Jungers P, Pelissier C, Nahoul K, Feinstein MC, Scholler R. Pituitary and ovarian dysfunctions in women on haemodialysis. Nephron. 1982;30:149-153. [DOI] [PubMed] [Google Scholar]
- 4. Morley JE, Distiller LA, Epstein S, et al. Menstrual disturbances in chronic renal failure. Horm Metab Res. 1979;11:68-72. [DOI] [PubMed] [Google Scholar]
- 5. Cochrane R, Regan L. Undetected gynaecological disorders in women with renal disease. Hum Reprod. 1997;12:667-670. [DOI] [PubMed] [Google Scholar]
- 6. Bagon JA, Vernaeve H, De Muylder X, Lafontaine JJ, Martens J, Van Roost G. Pregnancy and dialysis. Am J Kidney Dis. 1998;31:756-765. [DOI] [PubMed] [Google Scholar]
- 7. Okundaye I, Abrinko P, Hou S. Registry of pregnancy in dialysis patients. Am J Kidney Dis. 1998;31:766-773. [DOI] [PubMed] [Google Scholar]
- 8. Chao AS, Huang JY, Lien R, Kung FT, Chen PJ, Hsieh PC. Pregnancy in women who undergo long-term hemodialysis. Am J Obstet Gynecol. 2002;187:152-156. [DOI] [PubMed] [Google Scholar]
- 9. Hladunewich MA, Hou S, Odutayo A, et al. Intensive hemodialysis associates with improved pregnancy outcomes: a Canadian and United States cohort comparison. J Am Soc Nephrol. 2014;25(5):1103-1109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Kendrick J, Sharma S, Holmen J, Palit S, Nuccio E, Chonchol M. Kidney disease and maternal and fetal outcomes in pregnancy. Am J Kidney Dis. 2015;66:55-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Ahmed SB, Hovind P, Parving H-H, et al. Oral contraceptives, angiotensin-dependent renal vasoconstriction, and risk of diabetic nephropathy. Diabetes Care. 2005;28:1988-1994. [DOI] [PubMed] [Google Scholar]
- 12. Odutayo A, Cherney D, Miller J, et al. Transdermal contraception and the renin-angiotensin-aldosterone system in premenopausal women. Am J Physiol Renal Physiol. 2015;308:F535-F540. [DOI] [PubMed] [Google Scholar]
- 13. Watnick S. Pregnancy and contraceptive counseling of women with chronic kidney disease and kidney transplants. Adv Chronic Kidney Dis. 2007;14:126-131. [DOI] [PubMed] [Google Scholar]
- 14. Gold EB, Bromberger J, Crawford S, et al. Factors associated with age at natural menopause in a multiethnic sample of midlife women. Am J Epidemiol. 2001;153:865-874. [DOI] [PubMed] [Google Scholar]
- 15. De Villiers T, Pines A, Panay N, et al. Updated 2013 International Menopause Society recommendations on menopausal hormone therapy and preventive strategies for midlife health. Climacteric. 2013;16:316-337. [DOI] [PubMed] [Google Scholar]
- 16. Shifren JL, Gass ML, NAMS Recommendations for Clinical Care of Midlife Women Working Group. The North American Menopause Society recommendations for clinical care of midlife women. Menopause. 2014;21:1038-1062. [DOI] [PubMed] [Google Scholar]
- 17. Panay N, Hamoda H, Arya R, Savvas M, British Menopause Society and Women’s Health Concern. The 2013 British Menopause Society & Women’s Health Concern recommendations on hormone replacement therapy. Menopause Int. 2013;19:59-68. [DOI] [PubMed] [Google Scholar]
- 18. Gynaecologists TRAaNZCoOa. Management of the menopause. 2014. [Google Scholar]
- 19. Ramesh S, Mann MC, Holroyd-Leduc JM, et al. Hormone therapy and clinical and surrogate cardiovascular endpoints in women with chronic kidney disease: a systematic review and meta-analysis. Menopause. 2016;23:1028-1037. [DOI] [PubMed] [Google Scholar]
- 20. Monster TB, Janssen WM, de Jong PE, de Jong-van den Berg LT, Prevention of Renal and Vascular End-Stage Disease Study Group. Oral contraceptive use and hormone replacement therapy are associated with microalbuminuria. Arch Intern Med. 2001;161:2000-2005. [DOI] [PubMed] [Google Scholar]
- 21. Schopick EL, Fisher ND, Lin J, Forman JP, Curhan GC. Post-menopausal hormone use and albuminuria. Nephrol Dial Transplant. 2009;24:3739-3744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Agarwal M, Selvan V, Freedman BI, Liu Y, Wagenknecht LE. The relationship between albuminuria and hormone therapy in postmenopausal women. Am J Kidney Dis. 2005;45:1019-1025. [DOI] [PubMed] [Google Scholar]
- 23. Manning PJ, Sutherland WH, Allum AR, de Jong SA, Jones SD. HRT does not improve urinary albumin excretion in postmenopausal diabetic women. Diabetes Res Clin Pract. 2003;60:33-39. [DOI] [PubMed] [Google Scholar]
- 24. Ishani A, Blackwell T, Jamal SA, Cummings SR, Ensrud KE; MORE Investigators. The effect of raloxifene treatment in postmenopausal women with CKD. J Am Soc Nephrol. 2008;19:1430-1438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Melamed ML, Blackwell T, Neugarten J, et al. Raloxifene, a selective estrogen receptor modulator, is renoprotective: a post-hoc analysis. Kidney Int. 2011;79:241-249. [DOI] [PubMed] [Google Scholar]
- 26. Boulis AK, Long JA. Gender differences in the practice of adult primary care physicians. J Womens Health (Larchmt). 2004;13:703-712. [DOI] [PubMed] [Google Scholar]
- 27. Rossouw JE, Anderson GL, Prentice RL, et al. Risks and benefits of estrogen plus progestin in healthy postmenopausal women: principal results from the Women’s Health Initiative randomized controlled trial. JAMA. 2002;288:321-333. [DOI] [PubMed] [Google Scholar]
- 28. Lim VS, Henriquez C, Sievertsen G, Frohman LA. Ovarian function in chronic renal failure: evidence suggesting hypothalamic anovulation. Ann Intern Med. 1980;93:21-27. [DOI] [PubMed] [Google Scholar]
- 29. Lim VS, Kathpalia SC, Frohman LA. Hyperprolactinemia and impaired pituitary response to suppression and stimulation in chronic renal failure: reversal after transplantation. J Clin Endocrinol Metab. 1979;48:101-107. [DOI] [PubMed] [Google Scholar]
- 30. Dennerstein L, Dudley EC, Hopper JL, Burger H. Sexuality, hormones and the menopausal transition. Maturitas. 1997;26:83-93. [DOI] [PubMed] [Google Scholar]
- 31. Gold EB, Colvin A, Avis N, et al. Longitudinal analysis of the association between vasomotor symptoms and race/ethnicity across the menopausal transition: study of women’s health across the nation. Am J Public Health. 2006;96:1226-1235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Bromberger JT, Kravitz HM, Chang Y-F, Cyranowski JM, Brown C, Matthews KA. Major depression during and after the menopausal transition: Study of Women’s Health Across the Nation (SWAN). Psychol Med. 2011;41:1879-1888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Holley JL, Schmidt RJ, Bender FH, Dumler F, Schiff M. Gynecologic and reproductive issues in women on dialysis. Am J Kidney Dis. 1997;29:685-690. [DOI] [PubMed] [Google Scholar]
- 34. Navaneethan SD, Vecchio M, Johnson DW, et al. Prevalence and correlates of self-reported sexual dysfunction in CKD: a meta-analysis of observational studies. Am J Kidney Dis. 2010;56:670-685. [DOI] [PubMed] [Google Scholar]
- 35. Redelmeier DA, Tan SH, Booth GL. The treatment of unrelated disorders in patients with chronic medical diseases. N Engl J Med. 1998;338:1516-1520. [DOI] [PubMed] [Google Scholar]
- 36. Chiu YW, Teitelbaum I, Misra M, de Leon EM, Adzize T, Mehrotra R. Pill burden, adherence, hyperphosphatemia, and quality of life in maintenance dialysis patients. Clin J Am Soc Nephrol. 2009;4:1089-1096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Bailie GR, Eisele G, Liu L, et al. Patterns of medication use in the RRI-CKD study: focus on medications with cardiovascular effects. Nephrol Dial Transplant. 2005;20:1110-1115. [DOI] [PubMed] [Google Scholar]
- 38. Bender FH, Holley JL. Most nephrologists are primary care providers for chronic dialysis patients: results of a national survey. Am J Kidney Dis. 1996;28:67-71. [DOI] [PubMed] [Google Scholar]
- 39. Matas AJ, Smith JM, Skeans MA, et al. OPTN/SRTR 2013 Annual Data Report: Kidney. Am J Transplant. 2015;15:1-34. [DOI] [PubMed] [Google Scholar]
- 40. Chiu HH, Tangri N, Djurdjev O, et al. Perceptions of prognostic risks in chronic kidney disease: a national survey. Can J Kidney Health Dis. 2015;2:53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Dykema J, Jones NR, Piche T, Stevenson J. Surveying clinicians by web: current issues in design and administration. Eval Health Prof. 2013;36:352-381. [DOI] [PubMed] [Google Scholar]
- 42. McMahon GM, Thomas L, Tucker JK, Lin J. Factors in career choice among US nephrologists. Clin J Am Soc Nephrol. 2012;7:1786-1792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Gnambs T, Kaspar K. Socially desirable responding in Web-based questionnaires: a meta-analytic review of the candor hypothesis. Assessment. 2016;24:746-762. [DOI] [PubMed] [Google Scholar]
- 44. Gnambs T, Kaspar K. Disclosure of sensitive behaviors across self-administered survey modes: a meta-analysis. Behav Res Methods. 2015;47:1237-1259. [DOI] [PubMed] [Google Scholar]