Abstract
Background:
Medications are commonly used in suicide attempts. Pharmacists are inextricably linked to medications and may have roles in helping those at risk of suicide. We conducted a scoping review to characterize the existing literature and make recommendations about future research.
Methods:
We used a 6-step approach based on an existing scoping review methodological framework, including identifying the research question; identifying relevant studies and other literature; study and literature selection; data charting; collating, summarizing and reporting results; and dissemination of results. We searched electronic databases, various grey literature sources and mobile app stores.
Results:
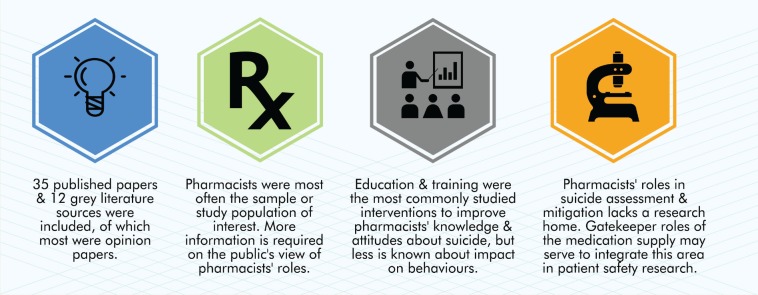
Thirty-five articles were included following screening of 1013 database citations. Of 1085 results from grey literature searches, we included 12. Most publications were opinion pieces (n = 22), followed by survey studies (n = 9), primarily assessing pharmacists’ knowledge and attitudes. Themes included education and training to impact knowledge and attitudes, gatekeeping of medication supply, collaboration and integration, and role perception. Public perspectives on pharmacists’ roles were limited.
Conclusions:
Research regarding pharmacists’ roles in the care of people at risk for suicide is limited. The areas that have dominated the literature include legal liability, especially with respect to gatekeeping medications, ethical decision making and education and training. Research is needed to determine what methods, outcomes and measures are required to best serve in building the evidence base for policy and practice decisions in this area.
Knowledge into Practice.
Medications are commonly used in suicide attempts, and pharmacists are the gatekeepers of the medication supply and as such have an inherent role and responsibility regarding patient safety.
Pharmacists frequently care for people at risk of suicide and have the opportunity to intervene in screening and risk management.
Pharmacists’ roles and interventions for people at risk of suicide have not been adequately researched, and more testing of interventions is required to determine the impact.
Mise En Pratique Des Connaissances.
Des médicaments sont souvent administrés aux personnes qui font des tentatives de suicide. En tant que contrôleurs de l’accès aux médicaments, les pharmaciens ont un rôle inhérent à jouer et des responsabilités à assumer pour assurer la sécurité des patients.
Les pharmaciens doivent souvent prendre en charge des personnes qui présentent un risque de suicide et ils ont la possibilité d’intervenir dans le dépistage et la gestion du risque.
Les rôles et les interventions des pharmaciens auprès des personnes qui présentent un risque de suicide ont été peu étudiés, et d’autres recherches s’imposent pour préciser les effets des interventions.
Introduction
Suicide is a major cause of preventable and premature death globally.1-3 The World Health Organization estimates that over 800,000 people die annually by suicide.3 Suicide attempts are estimated to be 10 to 40 times more frequent than death by suicide and create a significant burden on society and the health system.4
Most individuals who die by suicide have had contact with primary or psychiatric health services in the year prior to suicide, including accessing interventions such as medications.5-8 Despite increased health care service utilization and contact with health providers for medication-related needs prior to suicide-related attempts or death, thoughts and plans related to suicide can often go undetected in clinical practice.6,7
Community pharmacists are accessible and trusted health care professionals9-11 who routinely encounter and provide care and services to people living with chronic multimorbidity, mental illnesses, some of whom present in crisis situations and others who experience substance abuse disorders. Many of these patient groups have higher risk for suicide. This places pharmacists in a unique position for potential interventions, including roles that pertain to stewardship and management of the medication supply used for treating these conditions. Self-poisoning with prescription and nonprescription medications is commonly used in suicide attempts and accounts for a significant number of suicide deaths, especially in women (42% of suicide deaths) versus men (20% of suicide deaths).12 Limiting access to the means for a suicide attempt is a mechanism used in suicide prevention.13
A preliminary search of the published literature on the topic of pharmacists in suicide risk assessment and mitigation suggested limited information was available. We therefore determined it was necessary to conduct a scoping review to map and characterize the existing body of literature around pharmacists’ roles and interventions in suicide risk assessment and mitigation toward developing future interventions, identifying research gaps and making recommendations for future research to better care for those at risk of suicide.
Methods
We followed a 6-stage approach for scoping reviews based on the methodological framework of Arksey and O’Malley14 and as applied by others.15-20 These stages included identifying the research question; identifying relevant studies and other literature; study and literature selection; data charting21,22; collating, summarizing and reporting results; and dissemination of results with relevant stakeholders. A detailed description of this approach is available in Appendix 1 to this article online at www.cpjournal.ca.
Results
Electronic database search results
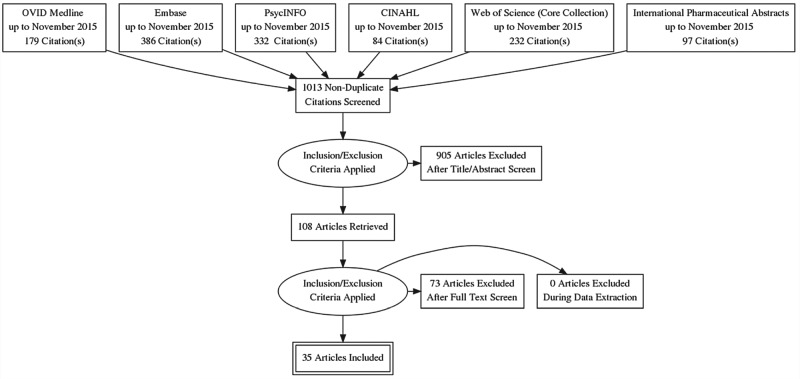
Following removal of duplicates, we found 1013 articles from electronic database searches (Figure 1). During title and abstract screening, we included 66 citations immediately; 33 were available in title only and the full texts were required, and 9 were screened as uncertain. We identified 108 articles that were advanced for full-text screening, of which 35 were retained for abstraction (Figure 2). Reasons for exclusion, in descending order, included lack of relevance (n = 58), non-English (n = 6), available as a conference abstract only (n = 6) and lack of availability for full-text review (n = 3). Of the 35 papers we included, 22 articles were opinion pieces, 9 used survey methods and 5 were characterized as “other.”
Figure 1.
Database search flow diagram for studies of pharmacists’ roles and interventions in suicide*
*Diagram based on the recommended reporting from PRISMA75
Figure 2.
Summary of scoping review of pharmacists and patients at risk of suicide
Opinion articles
The majority of publications (n = 22)23-44 that were classified as opinion pieces included articles such as commentaries and letters to the editor. Within these articles, 7 had a significant focus on pharmacists’ legal liability and professional ethics related to suicide.23,26,27,32,39,41,42
Survey methods
We characterized 9 of 35 studies as using survey methods (Table 1).45-53 Surveys were administered to measure changes in knowledge and attitudes of suicide of pharmacists and pharmacy students with (n = 4)45,49,51,53 or without (n = 2)48,52 a concomitantly implemented education and/or training program. Pre- and posttesting were used in all 4 studies that implemented an education or training program. Surveys were also used to characterize other topics such as curricula content in professional programs,47 public health literacy46 and use of resources by those who had attempted suicide.50
Table 1.
Nonopinion articles regarding pharmacists and patients at risk of suicide
| Author | Objectives | Design | Sample | Sample Size | Country | Summary of Results |
|---|---|---|---|---|---|---|
| Coppens et al.45 | (1) To improve community facilitators’ attitudes toward depression, knowledge on suicide and confidence to detect suicidal behaviour and (2) to identify specific training needs across regions and community facilitator groups | Survey | Community facilitators including pharmacists | Total (n = 1276) Pharmacist initial (n = 28) Pharmacist follow-up (n = 58) Pharmacist dropout (n = 70) |
Portugal, Germany, Ireland and Hungary | Effects of gatekeeper training in the community setting were measured using a questionnaire assessing attitude toward depression (Depression Stigma Scale), knowledge about suicide (Intervention Knowledge Test) and confidence in identifying suicidal behaviour (Morris Confidence Scale). Training improved knowledge, reshaped attitudes and increased confidence among community gatekeepers. |
| Goldney and Fisher46 | To examine whether broad-based community and professional education programs, which were introduced 6 years prior, have influenced mental health literacy and treatment seeking in those with depression and suicidal ideation | Survey | Patients | Participants with major depression (n = 241) and suicidal ideation (n = 79) | Australia | The effect of broad-based community and professional education programs was measured via survey questions administered during interviews. Pharmacists were perceived as potentially helpful in 37.4% of patients with major depression with no suicidal ideation and 32.4% of people with major depression and suicidal ideation. |
| Hare et al.54 | To develop a depression screening model that can be replicated by other community pharmacists; conduct a depression screening in a community pharmacy; identify and appropriately refer patients with symptoms consistent with depression and suicide | Non-comparative study | Pharmacists | Supermarket shoppers (n = 18) Community pharmacists (n = 6) Psychiatric pharmacy specialists (n = 4) |
United States | Administration of the Harvard Department of Psychiatry/National Depression Screening Day Scale (HANDS) to patients in community pharmacies effectively identified patients at risk of suicide and allowed for appropriate third-party referral. |
| Hazell et al.47 | To survey courses offered to students of medicine, nursing, psychology, social work, theology, education, pharmacy, law and journalism at Australian universities to identify the knowledge, attitudes and skills content of the courses and the teaching methods used regarding suicide and suicide prevention | Survey | Curricula coordinators (professionals and disciplines including pharmacy) | Schools/departments responded to the survey (n = 165) Responding pharmacy schools (n = 5) |
Australia | The penetrance of suicide and suicide prevention knowledge skills and attitude items into university curriculum programs was measured via survey responses. Pharmacy schools fell into the “high” or “medium” penetrance in 100% of the 5 programs surveyed. |
| Herings and Erkens57 | To examine patients at risk of dying by suicide through their drug refill patterns | Observational-retros-pective cohort | Patients | Linked medical records (medication dispensations and hospital discharge records) of 865,000 community inhabitants. 204/603 people prescribed risperidone or olanzapine experienced treatment interruption for at least 30 days. | Netherlands | Incidence rates regarding medication holidays and suicide attempts were estimates from the number of hospitalizations and follow-up time (person years). Patients who interrupted or stopped medication treatment with antipsychotics for at least 30 days resulted in 4-fold increase in suicide attempt rate. |
| Kodaka et al.48 | To explore demographic, occupational and personal factors associated with attitudes of pharmacists toward suicide | Survey | Pharmacists | Useable questionnaires from pharmacists (n = 327) | Japan | Information about pharmacists regarding demographic, occupational and personal factors that influence their attitudes toward suicide was gathered in a nondisclosed way and the Attitudes Towards Suicide (ATTS) questionnaire was used to assess pharmacists’ attitudes toward suicide. Seventy-seven percent of pharmacists had experience with a suicidal patient; 35.8% had received formal training for suicide mitigation. Those with previous training were more likely to view suicide as a common behaviour and recognize threats of suicide as a serious concern, believe suicide could be prevented and were prepared to help a suicidal person. |
| Lavigne et al.49 | To report the results of a national program to train US Department of Veterans Health Affairs pharmacy staff and other employees with direct patient contact to serve as suicide prevention “guides” | Survey | Pharmacists | Total responses (n = 7431) Pharmacist responses (n = 290) |
United States | Pre- and posttest evaluation questionnaires were used to measure attitude items toward suicide. Pharmacists and pharmacy staff improved in all attitudinal measures after training implementation. They felt they knew enough about suicide and felt it was their job to help suicidal veterans more than other suicide prevention guides. |
| Nguyen et al.50 | To determine the incidence of suicide attempts, describe methods used and assess use of health care services, including mental health care, after a suicide attempt in a rural area of Vietnam | Survey | Patients | Individuals who attempted suicide (n = 104) Suicide attempts including recurrences (n = 116) |
Vietnam | In face-to-face interviews, it was determined that 35 of 104 patients sought/accepted help from a health care provider after the suicide attempt; of those 35 patients, 22.9% reached out to a pharmacist. |
| O’Reilly et al.51 | To assess the impact of delivering Mental Health First Aid (MHFA) training for third-year pharmacy students on their mental health literacy and stigma toward mental illness | Survey | Pharmacy students | Baseline survey completion (n = 258/272) Six-week postintervention survey with MHFA training (n = 53) Six-week postintervention survey, no MHFA (n = 170) |
Australia | The impact of MHFA training on pharmacy students’ mental health literacy and stigma was measured via a survey instrument that contained a 7-item social distance scale (stigma toward mental disorders), a measure of mental health literacy and 16 items on participation in medication counselling and identification of drug-related problems. MHFA training improved participants’ ability to correctly identify mental illness and significantly reduced levels of stigma and the ability to recognize what interventions are helpful to suicidal persons. |
| O’Reilly et al.52 | To assess the beliefs of pharmacists about the helpfulness of interventions for schizophrenia and depression | Survey | Pharmacists | Pharmacist responses (n = 391) | Australia | A survey instrument containing a measure of mental health literacy was used to assess the beliefs of pharmacy students about the helpfulness of interventions for schizophrenia and depression. Many pharmacists did not recognize risk of suicide in schizophrenia and depression patients. While female and younger pharmacists were more likely to rate the likelihood of suicide as more likely in these populations, the response was not consistent across the profession. |
| Read et al.53 | To conduct a pre- and postevaluation of a project developed as an educational and evaluation method associated with preparing undergraduate pharmacy students to deal with potentially suicidal patients | Survey | Pharmacy students | Third-year pharmacy students pretest (n = 112), posttest (n = 104) Visual pretest (n = 113), visual posttest (n = 97) |
United States | A series of pre- and posttraining tests were used to measure the impact of the educational unit for pharmacists on suicide prevention. Overall, students improved knowledge of suicide, were better able to detect suicidal intent in a simulated situation, were better able to react to simulated suicidal intent and were better able to recognize adequate handling of a suicidal crisis situation. |
| Rosser et al.55 | To develop, implement and evaluate a depression screening program performed by pharmacists in the community setting; to determine the ability of this screening to identify and refer patients with symptoms of depression; to determine whether physician referral results in initiation or modification of treatment | Noncomparative study | Pharmacists | Total patients screened (n = 3726) Positive Patient Health Questionnaire (PHQ)–2 (n = 67) Positive PHQ-9 (n = 17) |
United States | The PHQ-9 enabled pharmacists to quickly identify undiagnosed patients and monitor for inadequate antidepression treatment. The PHQ-9 screening also enabled pharmacists to successfully identify and refer suicidal individuals. Sixty percent of positive screenings led to an initiation or modification of therapy. |
| Sinyor et al.56 | To identify the substances used by people who die from suicide by overdose in Toronto and to determine the correlates of specific substances used; pharmacist role discussed very briefly | Noncomparative study (retrospective review of coroners’ reports) | Deceased patients | Documented deaths by suicide (n = 397) | Canada | Coroners’ records for all cases of suicide by overdose in Toronto, Ontario, from 1998-2007 were examined to determine substances that were used by those who died by suicide from overdose. It was found that psychotropic medications,* other prescription medications† and over-the-counter medications were used most frequently in that order. |
Antidepressants, sedative hypnotics or anxiolytics, mood stabilizers and antipsychotics.
Opioids, beta-blockers and antiarrhythmics.
Three studies also included participants who were not classified as practising pharmacists or pharmacy students (e.g., patients or the public,46,50 other community members and health care professionals in addition to pharmacists).45 These studies looked at opinions about mental health literacy programs,46 whether people had used pharmacists as a resource when in crisis previously50 and whether community facilitators (e.g., pharmacists, nurses, teachers) had changes in knowledge and attitudes about depression and suicide after a training program.
Other designs
Of the remaining studies not using survey methods, 2 reported findings of pharmacists’ screening of depression, which included a review of those patients who screened positive on 1 or more questions for suicide.54,55 Screening tools included the Harvard Department of Psychiatry/National Depression Screening Day Scale54 and the Patient Health Questionnaire 2 and 9.55 Other designs included a retrospective review on coroners’ data from a Canadian province56 for prescription and nonprescription overdose deaths and a time-series analysis of antipsychotic interruption and suicide attempts (Table 1).57 There were no studies reporting on suicide-related outcomes in relation to pharmacist-led or pharmacist-participant interventions.
Location and dates of publications
Articles primarily originated from North America (United States [n = 19], Canada [n = 4]) and Australia (n = 5). Publication number varied across decades, with 11 in 2010 to the present, 6 from 2000 to 2010, 11 in the 1990s, 4 in the 1980s and 3 in the 1970s. With the exception of 2 papers,47,53 all studies that were characterized as designs other than opinion were published from 2003 onward.
Patient populations
The majority of papers focused on suicide, presumptively in the general population, but several articles had a specific focus (e.g., elderly,25,37,38,44,49 or rural24). Adolescent populations were absent, with the exception of reporting on cases related to consumption of medications for overdose (e.g., a young girl asking for an emetic following overdose23; a legal case in which a young girl took medications intended for a parent32).
Grey literature search results
We obtained 1085 results from our grey literature searches (e.g., Google Advanced, OpenGrey). After screening, there were 23 potentially relevant sites, of which 11 were excluded (Appendix 2, available online at www.cpjournal.ca). Exclusions were based on lack of relevancy, as per the electronic database searches. We found 1 study58 that was a survey of pharmacists in 1 Canadian province regarding their roles in health promotion. We were unable to find this study through our database searches because it lacked inclusion of suicide as a keyword or MeSH heading. Pharmacist respondents (44%) reported making referrals to external resources as one of the more common activities in people at risk of suicide. Nearly 28% surveyed did nothing related to suicide screening, and approximately 29% perceived that pharmacists should have little to no involvement in screening for suicide.
The remaining grey literature resources included variable content regarding statistics, and most focused on discussing roles for pharmacists in risk assessment and stratification (Appendix 2).
We had 456 hits in ProQuest, and after removal of duplicates, 447 were screened. We found that none of the articles were relevant.
Mobile app stores search results
Thirty-six (18%) of 211 apps were deemed potentially relevant and evaluated, with none meeting the criteria for inclusion.
Themes
We developed several themes from the published and grey literature. Themes included education and training to impact knowledge and attitudes, gatekeeping of medication supply, collaboration and integration, and role perception.
Education and training to impact knowledge and attitudes
In many of the opinion papers, education and training were suggested as a means to improve the knowledge, attitudes, capabilities and confidence of pharmacists in assessing for suicide risk, risk factors and those with intentions of suicide. This theme also occurred in papers evaluating various education and training programs for pharmacists. Several papers also discussed the role of pharmacists in educating the general public about suicide and educating patients and families about toxicities of medications and warning signs of suicide.23,28-30,44 Knowledge and attitudes were most commonly assessed as a result of education and training, with fewer studies attempting to focus on practice change.
Gatekeeping of medication supply
Pharmacists and other groups (e.g., lawyers, physicians) perceived gatekeeping of medication supply to be an essential role that pharmacists should and do fulfill. Pharmacists’ duties in medication supply management are also inherently tied to clinical activities that require them to recognize risk factors so they can adequately decide on appropriateness of the supply. Several articles suggested roles for pharmacists in managing the quantity of medications through mechanisms such as managing refill frequency,33 preventing stockpiling,25,43 monitoring the refill rates for adherence to medications in those with lived experience of mental illness57 and maintaining adequate medication history records,25 along with medication conditions and other clinically relevant variables38,43,56 that may put people at risk. Although clinical judgment around the supply of medication is required, several components of the process are largely technical in nature. The concept of pharmacist accessibility was also brought forward and highlighted as important in relation to refills and the potential for interaction with pharmacists based on the frequency of getting medications.25,34,43
Several legal liability cases were focused on whether the pharmacists had performed their duties in managing the patients’ supply of medications in either refilling a prescription or the amount given. This was often discussed in the context of the clinical abilities of the pharmacists to recognize whether the underlying conditions (e.g., depression) and medications dispensed should have alerted the pharmacists to assess whether suicide was a risk.26,27,41,42
Refill and prescription records of medication supply could also serve as a method for a proxy for suspected interactions with pharmacy staff in those who had been successful with a suicide attempt. In 1 study, overdose deaths were reviewed56 from coroners’ reports and examined for the type of prescription and nonprescription medications used.
Collaboration and integration
Collaboration is necessary for pharmacists’ participation in suicide risk assessment and mitigation. Pharmacists were encouraged through several articles to collaborate with other health care professionals when they identified someone at risk of suicide, in educating the public and in working with other providers to find referral mechanisms and sources for people in crisis. Specific clinical activities and roles were mentioned, such as pharmacists’ assisting physicians in selecting the most appropriate antidepressants in patients with suicidal ideation.28 There were also clear examples of adverse consequences (e.g., patient suicide, litigation against a pharmacist) that resulted when factors such as good communication were not in place to support collaboration.41,42
Role perception
There was nearly unanimous support that pharmacists should and can have roles in suicide risk assessment and mitigation in opinion articles and in the majority of studies in which the sample was pharmacists. Information on public perceptions and their engagement in defining and describing pharmacists’ roles, however, is lacking. From a small number of publications regarding the public’s views, there are perceived limitations in the roles and helpfulness of pharmacists based on survey results. Few people may seek help from pharmacists,50 or patients may perceive that pharmacists are not a helpful resource.46 This is juxtaposed against survey results from pharmacists in 1 Canadian province in which 72% of the sample indicated that pharmacists should be involved in screening, with the remainder stating there should be little to no involvement by pharmacists in screening for suicide.59
Discussion
Our findings indicate that current narratives and themes surrounding pharmacists’ roles in suicide risk assessment and mitigation remain similar to those offered in the 1970s. There is an expressed need and willingness to increase pharmacists’ roles in suicide risk assessment and mitigation, yet currently, evidence of pharmacist involvement in this role and its impact is lacking. Interventions that have been studied are directed toward pharmacists and usually in the form of education and training around suicide. Recommendations regarding pharmacist-delivered interventions to patients have centred on medication supply monitoring. The methodological approaches have been advancing, with more nonopinion articles published since 2000 onward, but overall are limited to survey methods. The overall number and types of publications point to significant gaps in research despite compelling arguments from authors of opinion pieces regarding the potential roles and opportunities for pharmacists in caring for those at risk of suicide. We found significant gaps in various areas, including in education and training, suicide-related outcomes, collaboration and integration, and the home for suicide research within pharmacy practice.
Education and training
The existing evidence base of published and grey literature seems to support that interventions such as education and training can positively change pharmacists’ and pharmacy students’ knowledge and attitudes, at least temporarily, toward those at risk of suicide. This finding is not unique to pharmacists, as improvements in knowledge, attitudes and confidence with suicide risk assessment and management have been demonstrated with other groups such as physicians60 and nurses61 following education and training interventions. There was no standard education or training program used for pharmacists or pharmacy students across studies, and therefore replication of results in the clinical setting and comparison of findings in other forms of syntheses would not be possible. This is important to consider, since suicide education and training programs are increasingly under scrutiny due to limited or no evidence of benefits for the intended patient groups.62,63 The educational methods and techniques may also require further research, as the use of contact-based or first voice involvement in the education may be necessary to create meaningful change in attitudes, as shown in some literature of pharmacy students regarding stigma toward those with mental illness.64,65
None of the studies used objective measures in assessing the impact of education and training programs on pharmacists’ behaviours in the clinical context; pharmacist self-report in surveys was typically used. Although it is challenging to assess quality of care in the practice setting, using simulated patient or mystery/secret shoppers as a research tool has gained in popularity and credibility in pharmacy practice research for assessing pharmacists’ care in many therapeutic areas.66-71 This method may hold promise for evaluating pharmacists’ behaviours following suicide-related education and training and is an approach commonly employed to assess prelicensure learners and trainees in pharmacy curricula in other therapeutic areas. Simulated patients have been used with learners in other disciplines and primarily in medicine, to evaluate suicide risk assessments and care.60,72,73 Use of this method may also address another research gap that we identified, which was an overall absence of patients’ perspectives of pharmacists’ roles and quality of care for those with significant risk factors or with current thoughts of suicide. In our recent work exploring perceptions of pharmacy services with people with lived experience of mental illness and addictions, it was identified that pharmacists should be trained in suicide risk assessment, including risk factor assessment and how to respond in a crisis.74 This was discussed in the context of positive encounters, including trust and rapport in the patient-pharmacist and patient-pharmacy staff relationships, but also contrasted with experiences of stigma around suicide attempts.74 This information, alongside a potential lack of perceived helpfulness of pharmacists by the public in 1 study,46 provides justification for closer examination of patients’ perspectives and for developing engagement strategies to leverage patient knowledge in improving pharmacists’ care of people at risk of suicide.
Suicide-related outcomes
We found no studies reporting on suicide-related outcomes such as deaths or hospitalizations following any kind of pharmacist-led or pharmacist-participant interventions, including education and training sessions. As mentioned in several opinion pieces found in this review, measuring suicide attempt–related deaths and hospitalizations is extremely challenging, given the rare occurrence and imperfect reporting practices and tools. This highlights unanswered questions surrounding what outcomes are most important to measure with respect to the effectiveness, efficiency and safety of pharmacists’ interventions related to suicide risk assessment and mitigation. In this scoping review, self-reports via survey methods (often administered at one point in time) were commonly used as a source of data among studies. Although useful in describing patterns and descriptions of experiences, many important patient-oriented and health system outcomes are invariably neglected and beyond the scope of studies using survey methods.
Coroners’ data and other retrospective administrative database studies may be useful in identifying patterns of care prior to a suicide attempt, including refilling prescriptions and presumably interacting with pharmacy team members. The gatekeeper role in the medication supply could be monitored and leveraged as a research tool when using and triangulating information from administrative and linked data such as health services utilization and diagnoses. However, the antecedent patterns of care are not definitively known through use of these methods, and data such as interventions provided by pharmacists that result in patients avoiding hospitalizations, suicide attempts and death are unlikely to be captured. Methods that include a mechanism to record suicide risk assessments and other interventions by pharmacists combined with the continued and safe return of the patient to the pharmacy for refills are required. We identified technology (e.g., computerized dispensing systems to alert for refill frequencies) and use of other pharmacy staff members (e.g., pharmacy assistants, technicians) as enabling factors in fulfilling these roles related to technology and thus freeing the pharmacist to engage in more clinical activities in risk assessment, but there was little to no mention of the contributions of technology or other pharmacy staff in the literature. More work is also needed to determine appropriate methods for assessing pharmacists’ roles and the impact of interventions in clinical scenarios in which patients are not actively receiving prescription or nonprescription pharmacotherapy but engaging with pharmacists or pharmacy staff for assistance regarding thoughts of suicide.
Collaboration and integration
Although collaboration with other health care professionals was discussed as an important mechanism in reducing suicide and related outcomes, there was little to no discussion in the literature regarding the “how to” for pharmacists’ integration or mechanisms to establish effective and efficient collaborative relationships in suicide risk assessment and mitigation. Collaborative models and team functioning in suicide care and the roles for pharmacists have not been investigated.
A home for suicide research in pharmacy practice
From the available literature, the issue of suicide and pharmacists’ practice lacks a consistent home within the research enterprise. Based on the number and type of papers we found, the gatekeeper role regarding the medication supply may serve as a mechanism to integrate pharmacists’ roles in current and future research in patient safety and mental health. Through consultations for medications, both prescription and nonprescription, pharmacists have a unique position for case identification, assessment, management, triage and follow-up. Much of the current patient safety theories and frameworks include adverse events, which would include incidents that result in harm to the patient.1,2 Intentional ingestions of medications could be classified as medication incidents that are potentially preventable. Existing theories in patient safety and medication safety may be useful and transferable to pharmacists’ care of patients at risk of suicide and especially in relation to gatekeeping and stewardship of the medication supply.
Limitations
The searches were limited to English-only articles. Searches of grey literature, databases and app stores were not conducted simultaneously but in a staggered nature.
Our search terms included those related to suicide and not those focused on serious mental illnesses (e.g., schizophrenia). Roles for pharmacists may be described in the literature discussing serious mental illnesses, which are a risk factor for death by suicide. Our searches would not have captured these articles in which suicide was implied unless it was directly mentioned.
Several authors were involved in the scoping review process, but each received the same training on the process by 1 team member, who also oversaw the entire research process.
Our review focused on the community pharmacist, and therefore the roles of pharmacists in other settings would not be recognized in our review.
Conclusion
Pharmacists’ roles in suicide assessment and risk mitigation have been studied to a limited extent with specific areas of focus, including legal liability, ethical decision making, education and training, collaboration and role in medication safety. To date, there has been a lack of advancements in methodological approaches in this content area and an overall paucity of patient and other health care provider perspectives. More research is required to determine how best to educate and train pharmacists in suicide risk assessment and mitigation and what methods, outcomes and measures are required to best serve in building the evidence base for policy and practice decisions in this area. ■
Acknowledgments
We thank Drs. Stan Kutcher, Fred Burge, Timothy F. Chen and Ruth Martin-Misener for their contributions to the concept and initial design of the study. Melissa Helwig, MLI, was instrumental in conducting the database searches and guiding the trainees in their conduct of searches for grey literature and related materials.
Footnotes
Author Contributions:ALM developed the idea and research proposal and all authors contributed feedback. KH and PT conducted the searches under the direction of a medical librarian and the research team. ALM, KH, RA and PT carried out various stages of the scoping review. ALM and KH drafted the manuscript. AMW, COR and DG provided critical review and feedback. All authors approved the draft and final versions of the manuscript.
Declaration of Conflicting Interests:The authors have no financial or other conflicts of interest related to this work.
Funding:This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
References
- 1. Brickell TA, Nichols TL, Procyshyn RM, et al. Patient safety in mental health. Edmonton (AB): Canadian Patient Safety Institute and Ontario Hospital Association; 2009:1-60. [Google Scholar]
- 2. Capriotti T. Update on depression and antidepressant medications. Medsurg Nurs 2006;15(4):241-6. [PubMed] [Google Scholar]
- 3. World Health Organization. Suicide data. 2016. Available: www.who.int/mental_health/prevention/suicide/suicideprevent/en/ (accessed June 12, 2016).
- 4. Bertolote JM, Fleischmann A, De Leo D, et al. Suicide attempts, plans and ideation in culturally diverse sites: the WHO SUPRE-MISS community survey. Psychol Med 2005;35(10):1457-65. [DOI] [PubMed] [Google Scholar]
- 5. Ahmedani BK, Simon GE, Stewart C, et al. Health care contacts in the year before suicide death. J Gen Intern Med 2014;29(6):870-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Smith EG, Kim HM, Ganoczy D, et al. Suicide risk assessment received prior to suicide death by Veterans Health Administration patients with a history of depression. J Clin Psychiatry 2013;74(3):226-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Vannoy SD, Robins LS. Suicide-related discussions with depressed primary care patients in the USA: gender and quality gaps: a mixed methods analysis. BMJ Open 2011;1(2):e000198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Finkelstein Y, Macdonald EM, Hollands S, et al. Risk of suicide following deliberate self-poisoning. JAMA Psychiatry 2015;72(6):570-5. [DOI] [PubMed] [Google Scholar]
- 9. Law MR, Dijkstra A, Douillard JA, et al. Geographic accessibility of community pharmacies in ontario. Healthc Policy 2011;6(3):36-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Law MR, Heard D, Fisher J, et al. The geographic accessibility of pharmacies in Nova Scotia. Can Pharm J (Ott) 2013;146(1):39-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Doucet G. CPhA National Survey: Canadians trust pharmacists and support their enhanced role in the delivery of quality care and services. Can Pharm J (Ott) 2015;148(3):160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Navaneelan T. Suicide rates: an overview. Ottawa: Statistics Canada; 2012. [Google Scholar]
- 13. Mann JJ, Apter A, Bertolote J, et al. Suicide prevention strategies: a systematic review. JAMA 2005;294(16): 2064-74. [DOI] [PubMed] [Google Scholar]
- 14. Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol 2005;8(1):19-32. [Google Scholar]
- 15. Bragge P, Clavisi O, Turner T, et al. The Global Evidence Mapping Initiative: scoping research in broad topic areas. BMC Med Res Methodol 2011;11:92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Brien SE, Lorenzetti DL, Lewis S, et al. Overview of a formal scoping review on health system report cards. Implement Sci 2010;5:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Kastner M, Tricco AC, Soobiah C, et al. What is the most appropriate knowledge synthesis method to conduct a review? Protocol for a scoping review. BMC Med Res Methodol 2012;12:114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Levac D, Colquhoun H, O’Brien KK. Scoping studies: advancing the methodology. Implement Sci 2010;5:69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Rumrill PD, Fitzgerald SM, Merchant WR. Using scoping literature reviews as a means of understanding and interpreting existing literature. Work 2010;35(3):399-404. [DOI] [PubMed] [Google Scholar]
- 20. Valaitis R, Martin-Misener R, Wong ST, et al. Methods, strategies and technologies used to conduct a scoping literature review of collaboration between primary care and public health. Prim Health Care Res Dev 2012;13(3):219-36. [DOI] [PubMed] [Google Scholar]
- 21. Saldaña J. The coding manual for qualitative researchers. Los Angeles: Sage; 2013. [Google Scholar]
- 22. Braun V, Clarke V. What can “thematic analysis” offer health and wellbeing researchers? Int J Qual Stud Health Well-being 2014;9:26152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Daly MJ, Bower A, Fitzpatrick J, et al. You can’t make me go to the hospital! Pharm Pract 1999;9:186, 188. [Google Scholar]
- 24. Ball P, Quaass M. Removing the noose from rural communities. Aust J Pharm 2007;88(1047):24. [Google Scholar]
- 25. Benson RA, Brodie DC. Suicide by overdoses of medicines among the aged. J Am Geriatr Soc 1975;23(7):304-8. [DOI] [PubMed] [Google Scholar]
- 26. Brushwood DB. Pharmacist liability for suicide by drug overdose. Am J Hosp Pharm 1983;40(3):439-43. [PubMed] [Google Scholar]
- 27. Brushwood DB. Pharmacist’s liability for a patient’s suicide. US Pharm 1984;9:20, 22-23. [Google Scholar]
- 28. Chang F. Late-life depression: people aged 65+ account for relatively high number of suicide deaths. Can Pharm J (Ott) 2005;138(1):31-6. [Google Scholar]
- 29. Docherty M. Depression: it’s time to end the silence. Aust J Pharm 1995;76:1258-60. [Google Scholar]
- 30. Gibson MR, Lott RS. Suicide and the role of the pharmacist. J Am Pharm Assoc 1972;12(9):457-61, 466. [DOI] [PubMed] [Google Scholar]
- 31. Hamilton AC. Detecting and dealing with suicidal patients in the pharmacy. Can Pharm J (Ott) 2012;145(4):172-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. LeBlang TR. What if Rx medication is used for suicide? Am Drug 1989;199:64. [Google Scholar]
- 33. Harris T, Smith F. Psychotropic drug treatment: repeated prescription charges for weekly treatment may be deterrent to patients. Br Med J 1998;316:476-7. [PMC free article] [PubMed] [Google Scholar]
- 34. Kozma C.M. Do we need a more aggressive approach to suicide prevention? Manag Care Interface 2004;17(5):37-8. [PubMed] [Google Scholar]
- 35. McCann J. Pharmacists play an important role in suicide prevention. Drug Topics 1991;135:14-15. [Google Scholar]
- 36. Murphy AL, Gardner DM, Chen TF, et al. Community pharmacists and the assessment and management of suicide risk. Can Pharm J (Ott) 2015;148(4):171-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. NnadiOkolo EE, McReyonds J. Suicide in the elderly: causes and prevention. Consult Pharm 1995;10:355-60. [Google Scholar]
- 38. Rhodes RS, Adamcik BA. Elderly suicide: pharmacists’ role in detection and referral. Drug Store News Pharm 1994;4:33-40. [Google Scholar]
- 39. Soares MS, Warnock AC, Barham B, et al. Pharmacist’s obligation to hold confidential patient’s intent to commit suicide. Am J Hosp Pharm 1992;49(4):864-9. [PubMed] [Google Scholar]
- 40. Veatch RM. Pharmacists obligation to hold confidential patients intent to commit suicide—analysis and commentary. Am J Hosp Pharm 1992;49(4):867-9. [PubMed] [Google Scholar]
- 41. Vivian JC. Suicide liability. US Pharm 1997;22:54, 56,, 61. [Google Scholar]
- 42. Warnock AC, Barham B. Pharmacists obligation to hold confidential patients intent to commit suicide—position 2—patient confidentiality should be breached. Am J Hosp Pharm 1992;49(4):865-7. [PubMed] [Google Scholar]
- 43. Weiss B. Rx suicides: pharmacists can help stop them. Drug Topics 1987;131:34-6, 38,, 42,, 46,, 48. [Google Scholar]
- 44. Zanni GR, Wick JY. Understanding suicide in the elderly. Consult Pharm 2010;25(2):93-102. [DOI] [PubMed] [Google Scholar]
- 45. Coppens E, Van Audenhove C, Iddi S, et al. Effectiveness of community facilitator training in improving knowledge, attitudes and confidence in relation to depression and suicidal behavior: results of the OSPI-Europe intervention in four European countries. J Affect Disord 2014;165:142-50. [DOI] [PubMed] [Google Scholar]
- 46. Goldney RD, Fisher LJ. Have broad-based community and professional education programs influenced mental health literacy and treatment seeking of those with major depression and suicidal ideation? Suicide Life Threat Behav 2008;38(2):129-42. [DOI] [PubMed] [Google Scholar]
- 47. Hazell P, Hazell T, Waring T, et al. A survey of suicide prevention curricula taught in Australian universities. Aust N Z J Psychiatry 1999;33(2):253-9. [DOI] [PubMed] [Google Scholar]
- 48. Kodaka M, Inagaki M, Yamada M. Factors associated with attitudes toward suicide among Japanese pharmacists participating in the Board Certified Psychiatric Pharmacy Specialist Seminar. Crisis 2013;34(6):420-7. [DOI] [PubMed] [Google Scholar]
- 49. Lavigne JE, King DA, Lu NJ, Knox KL, Kemp JE. Pharmacist and pharmacy staff knowledge, attitudes and motivation to refer patients for suicide risk assessment: lessons from Operation S.A.V.E. In: Lavigne JE, editor. Frontiers in suicide risk. New York: Nova Science; 2012. p. 195-202. [Google Scholar]
- 50. Nguyen TV, Dalman C, Le TC, et al. Suicide attempt in a rural area of Vietnam: incidence, methods used and access to mental health care. Int J Ment Health Syst 2010;4(1):3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. O’Reilly CL, Bell JS, Kelly PJ, et al. Impact of mental health first aid training on pharmacy students’ knowledge, attitudes and self-reported behaviour: a controlled trial. Aust N Z J Psychiatry 2011;45(7):549-57. [DOI] [PubMed] [Google Scholar]
- 52. O’Reilly CL, Bell JS, Chen TF. Pharmacists’ beliefs about treatments and outcomes of mental disorders: a mental health literacy survey. Aust N Z J Psychiatry 2010;44(12):1089-96. [DOI] [PubMed] [Google Scholar]
- 53. Read DR, Rosenbluth SA, Ryan MR. Development and evaluation of an educational unit for pharmacists on suicide-prevention. Am J Pharm Educ 1978;42(3):313-6. [Google Scholar]
- 54. Hare SK, Kraenow K. Depression screenings: developing a model for use in a community pharmacy. J Am Pharm Assoc 2008;48(1):46-51. [DOI] [PubMed] [Google Scholar]
- 55. Rosser S, Frede S, Conrad WF, et al. Development, implementation and evaluation of a pharmacist-conducted screening program for depression. J Am Pharm Assoc 2013;53(1):22-9. [DOI] [PubMed] [Google Scholar]
- 56. Sinyor M, Howlett A, Cheung AH, et al. Substances used in completed suicide by overdose in Toronto: an observational study of coroner’s data. Can J Psychiatry 2012;57(3):184-91. [DOI] [PubMed] [Google Scholar]
- 57. Herings RM, Erkens JA. Increased suicide attempt rate among patients interrupting use of atypical antipsychotics. Pharmacoepidemiol Drug Saf 2003;12(5):423-4. [DOI] [PubMed] [Google Scholar]
- 58. Laliberte MC, Perreault S, Damestoy N, et al. Ideal and actual involvement of community pharmacists in health promotion and prevention: a cross-sectional study in Quebec, Canada. BMC Public Health 2012;12:192-203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Laliberte MC, Perreault S, Damestoy N, et al. Ideal and actual involvement of community pharmacists in health promotion and prevention: a cross-sectional study in Quebec, Canada. BMC Public Health 2012;12:192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Fallucco EM, Conlon MK, Gale G, et al. Use of a standardized patient paradigm to enhance proficiency in risk assessment for adolescent depression and suicide. J Adolesc Health 2012;51(1):66-72. [DOI] [PubMed] [Google Scholar]
- 61. Chan SW, Chien WT, Tso S. The qualitative evaluation of a suicide prevention and management programme by general nurses. J Clin Nurs 2008;17(21):2884-94. [DOI] [PubMed] [Google Scholar]
- 62. Kutcher S, Wei Y, Behzadi P. School- and community-based youth suicide prevention interventions: hot idea, hot air, or sham? Can J Psychiatry 2017;62(6):381-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Wei Y, Kutcher SP, LeBlanc JC. Hot idea or hot air: a systematic review of evidence for two widely marketed youth suicide prevention programs and recommendations for implementation. J Can Acad Child Adolesc Psychiatry 2015;24(1):5-16. [PMC free article] [PubMed] [Google Scholar]
- 64. Patten SB, Remillard A, Phillips L, et al. Effectiveness of contact-based education for reducing mental illness-related stigma in pharmacy students. BMC Med Educ 2012;12:120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. O’Reilly CL, Bell JS, Chen TF. Consumer-led mental health education for pharmacy students. Am J Pharm Educ 2010;74(9):167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Watson MC, Cleland JA, Bond CM. Simulated patient visits with immediate feedback to improve the supply of over-the-counter medicines: a feasibility study. Fam Pract 2009;26(6): 532-42. [DOI] [PubMed] [Google Scholar]
- 67. Watson MC, Skelton JR, Bond CM, et al. Simulated patients in the community pharmacy setting—using simulated patients to measure practice in the community pharmacy setting. Pharm World Sci 2004;26(1):32-7. [DOI] [PubMed] [Google Scholar]
- 68. Kippist C, Wong K, Bartlett D, et al. How do pharmacists respond to complaints of acute insomnia? A simulated patient study. Int J Clin Pharm 2011;33(2):237-45. [DOI] [PubMed] [Google Scholar]
- 69. Xu T, de Almeida Neto AC, Moles RJ. A systematic review of simulated-patient methods used in community pharmacy to assess the provision of non-prescription medicines. Int J Pharm Pract 2012;20(5):307-19. [DOI] [PubMed] [Google Scholar]
- 70. Murphy AL, Martin-Misener R, Kutcher SP, et al. Pharmacists’ performance in a telephone-based simulated patient study after a mental health capacity-building program. Int J Clin Pharm 2015;37(6):1009-13. [DOI] [PubMed] [Google Scholar]
- 71. Weiss MC, Booth A, Jones B, et al. Use of simulated patients to assess the clinical and communication skills of community pharmacists. Pharm World Sci 2010;32(3):353-61. [DOI] [PubMed] [Google Scholar]
- 72. Kobus AM, Heintzman J, Garvin RD. Use of standardised patients in the evaluation of a residency mood disorders curriculum: a brief report. Ment Health Fam Med 2013;10(1):45-51. [PMC free article] [PubMed] [Google Scholar]
- 73. Hung EK, Binder RL, Fordwood SR, et al. A method for evaluating competency in assessment and management of suicide risk. Acad Psychiatry 2012;36(1):23-8. [DOI] [PubMed] [Google Scholar]
- 74. Murphy AL, Martin-Misener R, Kutcher SP, et al. From personal crisis care to convenience shopping: an interpretive description of the experiences of people with mental illness and addictions in community pharmacies. BMC Health Serv Res 2016;16(569):1-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol 2009;62(10):1006-12. [DOI] [PubMed] [Google Scholar]
- 76. Stein GC. Assisted suicide: an issue for pharmacists. Am J Health Syst Pharm 1998;55(6):539. [DOI] [PubMed] [Google Scholar]