Abstract
Background:
Pharmacist/nurse-led clinics are an established model for many chronic diseases but not yet for HIV. At our centre, patients with HIV are seen by a multidisciplinary team (physician, nurse, pharmacist, social worker) at least yearly. Some attend an HIV-specialist pharmacist/nurse clinic (or “nonphysician clinic,” NPC) for alternate biannual visits. Our objective was to assess patient satisfaction with care received through both clinics.
Methods:
The Patient Satisfaction Survey for HIV Ambulatory Care (assesses satisfaction with access to care, clinic visits and quality of care) was administered by telephone to adults who attended either clinic between January and July 2014. Descriptive statistics described patient characteristics and satisfaction scores. Fisher’s exact test compared satisfaction scores between the NPC and multidisciplinary clinic (MDC). Multivariate logistic regression examined associations between overall satisfaction with care and clinic type and patient characteristics (e.g., age, disease duration).
Results:
Respondents were very satisfied with the overall quality of HIV care in both the NPC and MDC (89% vs 93%, respectively, p = 0.6). Patients from both clinics expressed satisfaction with access to care, treatment plan input, their provider’s knowledge of the newest developments in HIV care and explanation of medication side effects, with no significant differences noted. Significantly more MDC patients reported being asked about housing/finances, alcohol/drug use and whether they needed help disclosing their status. Patient characteristics were not significantly associated with satisfaction with overall quality of care.
Conclusion:
Patients are satisfied with both clinics, supporting NPC as an innovative model for chronic HIV care. Comparison of outcomes between clinics is needed to ensure high-quality care.
Knowledge Into Practice.
Pharmacists and nurse practitioners increasingly play a larger role in chronic disease management. Pharmacist- and nurse-run clinics have previously been demonstrated to be effective in managing many chronic diseases but not HIV care.
Chronic HIV management has become largely a primary care issue. Nonphysician clinics are not commonplace for HIV care, and there is a lack of evidence of patient acceptance and effectiveness for this model of care in HIV.
Pharmacists have an established role in HIV care and with an expanded scope of practice are well positioned to collaborate with nurses to provide chronic HIV management to patients.
This is the first study to demonstrate patient acceptance of a pharmacist- and nurse-managed clinic model for chronic HIV management. Further study is needed to ensure patient outcomes are comparable to the current standard—multidisciplinary, physician-inclusive clinic care.
Mise En Pratique Des Connaissances.
Les pharmaciens et les infirmières praticiennes jouent un rôle de plus en plus grand dans la prise en charge des maladies chroniques. Il a déjà été démontré que des cliniques dirigées par des pharmaciens et des infirmières sont efficaces dans la prise en charge de nombreuses maladies chroniques, mais aucune étude n’a porté sur le VIH.
La prise en charge de l’infection chronique par le VIH est essentiellement devenue une question de soins primaires. Les cliniques sans médecin sont peu répandues dans le domaine du VIH, et on possède peu de données sur l’efficacité de ce modèle de soins pour le VIH et sur son acceptation par les patients.
Les pharmaciens jouent un rôle établi dans les soins des patients infectés par le VIH et, grâce à l’élargissement de leur champ de pratique, ils sont bien placés pour collaborer avec les infirmières pour assurer la prise en charge des patients atteints d’une infection chronique par le VIH.
Il s’agit de la première étude à démontrer l’acceptation par les patients d’un modèle de clinique géré par des pharmaciens et des infirmières pour la prise en charge de l’infection chronique par le VIH. D’autres études devront être menées pour s’assurer que les résultats chez les patients sont comparables à ceux obtenus avec le modèle standard actuel de clinique multidisciplinaire avec médecins.
Background
Due to the effectiveness of antiretroviral therapy, people living with HIV infection (HIV+) are living longer, healthier lives. Chronic care for HIV+ patients has shifted to maintaining control of HIV infection, supporting long-term adherence to therapy and managing primary care issues (e.g., cardiovascular risk reduction). With limited health care resources, creative solutions are needed to ensure that patients receive quality care from HIV-specialized providers. HIV specialist pharmacists and nurses have shown positive outcomes in HIV treatment advice clinics1 and drug optimization clinics,2 in addition to their roles in multidisciplinary care of HIV+ patients alongside physicians.3 However, a pharmacist- and nurse-managed clinic for provision of holistic care for stable HIV+ patients has not been described in the literature.
Programs expanding the scope of pharmacists’ practice are being established across the country and worldwide as a means of improving access to care and patient outcomes. The development of nonphysician clinics (NPCs) is an emerging strategy to help meet the demands of priority health initiatives, such as access to HIV care.4 Key to supporting this shift is ensuring that quality of care and patient outcomes are not compromised in any new care model.
Patient satisfaction has emerged as a useful factor to assess the quality of health care delivery, alongside more traditional health outcomes and quality measures. The patient’s perception of care has a direct influence on treatment success. Patients with higher satisfaction levels maintain more stable relationships with health care providers, comply more closely with medical advice and treatment and have improved health outcomes.5,6 Patient satisfaction also provides insight into the strengths and weakness of a health care program from a user perspective, which is useful for quality assurance and to assess program effectiveness.
Several tools exist to measure patient satisfaction with care. The Patient Satisfaction Survey for HIV Ambulatory Care (PSS-HIV) was created specifically to assess care provided to HIV+ patients in outpatient settings.6 This survey has undergone a rigorous validation process to ensure each item measures the aspect of patient satisfaction intended.
A collaborative NPC model, consisting of an HIV specialist clinical pharmacist and nurse practitioner, has been used to provide care to patients with HIV in Newfoundland and Labrador (NL) since 2009, when the infectious diseases (ID) physician responsible for HIV care left the province. Once a new ID specialist was hired, the NPCs were continued in addition to full multidisciplinary clinics (MDCs), as this was found to be an effective way to reduce wait times for clinic appointments and patients expressed satisfaction with the care provided. The standard of care in NL is for patients to be seen every 6 months for chronic HIV care. Patients attend the MDC, consisting of an HIV specialist physician, nurse, pharmacist and social worker, at least once per year. Some patients attend the NPC for their next follow-up visit, while others attend the MDC, as appointment scheduling permits. The HIV clinic in NL is a provincial program, providing care to all patients with HIV infection throughout the province (approximately 160 patients), and has a high rate of retention in care (>95%).
The objective of this study was to assess patient satisfaction with care received through the NPC and MDC groups.
Methods
A telephone survey of adults seen at the HIV clinic from January 1 to July 31, 2014, was conducted. The PSS-HIV was administered in English, so patients requiring an interpreter were not eligible to participate. Patients were initially contacted by HIV clinic staff to determine their interest in participating and, if interested, their preferred contact time.
Interested patients were assigned a study number and were contacted by an undergraduate pharmacy student from Memorial University, who was not a member of the HIV team. The student underwent training in interview protocol, the telephone script and real-time computerized data entry. Verbal consent was obtained at the beginning of each call, and the survey was then administered using a standardized telephone script. Data were entered directly into a database during the call. Informed consent and reasons for refusing participation were recorded. Calls were completed over a 4-week period (July-August 2014).
The PSS-HIV questions were modified slightly to reflect practice in Canada and to improve readability over the telephone. The modified survey was pretested on a small group of patients from the NL clinic for face and content validity prior to widespread dissemination. To boost response rate, participants were invited to enter their name for a draw to receive 1 of 4 grocery gift cards. Names for the draw were recorded separately from the survey responses to maintain confidentiality. The study received approval from the Human Research Ethics Committee at Memorial University.
The survey was comprised of several sections pertaining to satisfaction with access to HIV care, the HIV clinic visit, psychosocial issues and overall quality of care. Patients were asked to respond to questions based on their most recent clinic experience. Responses to each question were categorical. When questioned about overall satisfaction with care, patients were asked whether they ever felt treated poorly at the clinic and to rate provider knowledge of HIV treatment and quality of care at the HIV clinic compared to other clinics they attend. In addition, patients were provided a list of descriptors and asked to identify which ones reflected how they felt about their clinic care. The final section collected information on patient demographics.
Patients were grouped according to the last clinic (NPC or MDC) they attended. Descriptive statistics (frequencies, means and standard deviations) were used to describe the characteristics of the sample. Fisher’s exact test was used to compare responses from patients who attended the NPC and MDC. Multivariate logistic regression examined associations between overall satisfaction with care and type of clinic and patient characteristics (e.g., age, sex, race, sex orientation, geographic location, disease duration, overall health and time receiving care from each clinic). Data were analyzed using STATA, version MP (StataCorp LP, College Station, TX).
Results
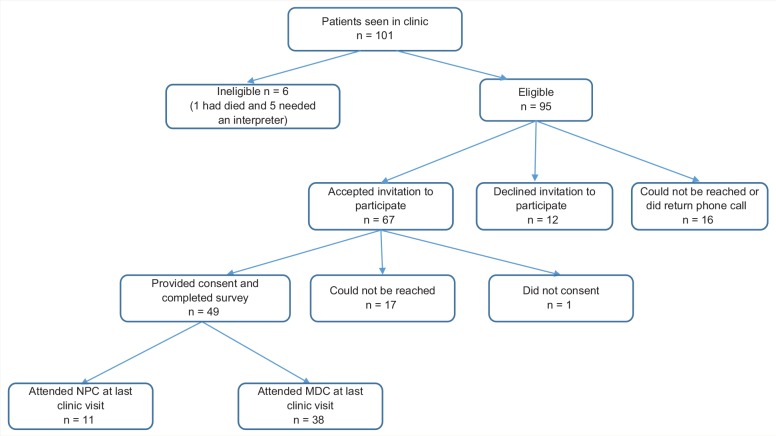
A total of 101 patients were seen in clinic during the study period, 95 of whom were eligible for study inclusion (Figure 1). Through initial contact by HIV clinic staff, 67 of the eligible patients accepted the invitation to participate in the study. Forty-nine patients provided consent and completed the survey, for a response rate of 73%. The majority of patients, 38 of 49 (78%), who completed the survey attended the MDC at their last clinic visit, while 22% attended the NPC.
Figure 1.
Survey sample
MDC, multidisciplinary clinic; NPC, nonphysician clinic
Of the 49 respondents, 78% were males and 88% were ≥40 years old (Table 1). Respondents were mainly white (90%), with 55% reporting their sexual orientation as gay/lesbian/homosexual. Overall, respondents were quite used to receiving care through the NL HIV program (65% reported receiving care for more than 5 years), although newly diagnosed patients (HIV+ for less than 2 years) were more likely to have received care through the MDC than the NPC at their last clinic visit (22% vs 0%, p < 0.045).
Table 1.
Patient characteristics (n = 49)*
| Descriptor | NPC result,n = 11 (%) | MDC result, n = 38 (%) | Total, n (%) |
|---|---|---|---|
| Male | 9 (82) | 29 (76) | 38 (78) |
| Age range, years | |||
| • <39 | 0 (0) | 6 (16) | 6 (12) |
| • 40-49 | 6 (55) | 15 (39) | 21 (43) |
| • >50 | 5 (45) | 17 (44) | 22 (45) |
| Race | |||
| • White | 9 (82) | 35 (92) | 44 (90) |
| • Other | 2 (18) | 3 (8) | 5 (10) |
| Geographic location | |||
| • Rural | 2 (18) | 16 (42) | 18 (37) |
| • Urban | 9 (82) | 22 (58) | 31 (63) |
| Sexual orientation | |||
| • Straight/heterosexual | 5 (45) | 15 (39) | 20 (41) |
| • Gay/lesbian/homosexual | 6 (55) | 21 (55) | 27 (55) |
| Time since HIV diagnosis | |||
| • <2 years | 0 | 7 (18) | 7 (14) |
| • 3-5 years | 2 (18) | 4 (11) | 6 (12) |
| • >5 years | 9 (82) | 27 (71) | 36 (74) |
| Time receiving care at the clinic | |||
| • <2 years | 0 | 11 (29) | 11 (22) |
| • 3-5 years | 2 (18) | 4 (11) | 6 (12) |
| • >5 years | 9 (82) | 23 (60) | 32 (65) |
| Participants’ self-rated health status at the time of survey | |||
| • Excellent | 4 (36) | 13 (34) | 17 (35) |
| • Good/very good | 6 (55) | 20 (53) | 26 (53) |
| • Fair/poor | 1 (9) | 3 (8) | 4 (8) |
Not all respondents answered all questions.
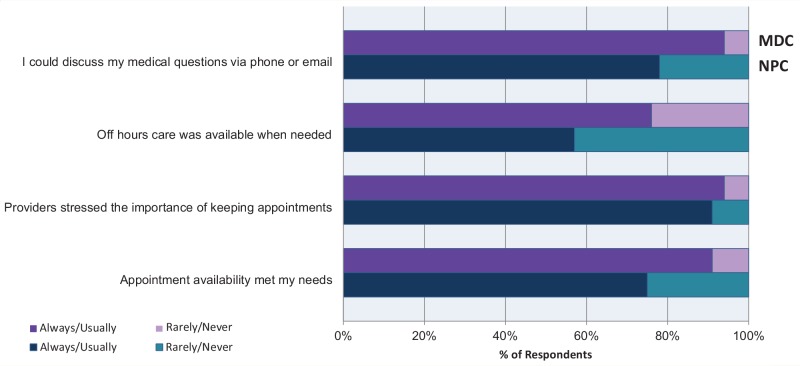
The majority of respondents indicated they were satisfied with access to HIV care (Figure 2), with no differences noted between NPC and MDC patient responses. Patients from both clinics said they could schedule appointments when needed and reach a member of their health care team by phone/email if they had a medical question. Similarly, the majority of patients from both clinics indicated that their health care providers stressed the importance of keeping appointments. Few patients stated that they had tried to reach a member of the team during off hours (NPC, n = 7; MDC, n = 17), but of those who had, the majority indicated they could do so.
Figure 2.
Access to HIV care: MDC vs NPC patient satisfaction*
*Responses of “did not apply” or “don’t know” are excluded. MDC, multidisciplinary clinic; NPC, nonphysician clinic
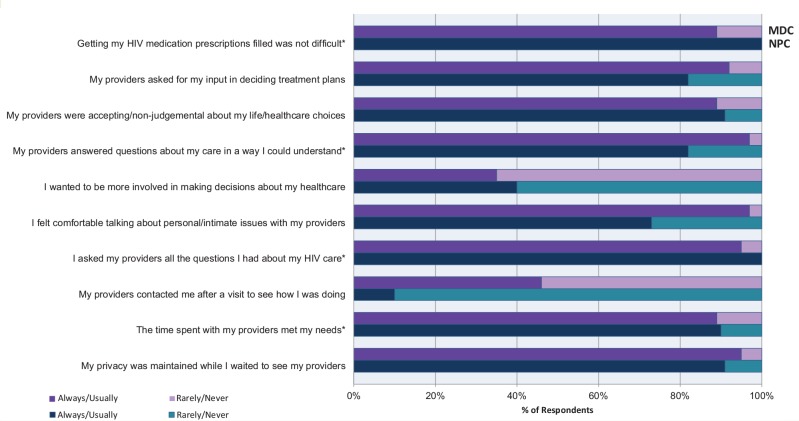
Respondents indicated a high level of satisfaction with their HIV clinic visit (Figure 3). When asked whether health care providers ensured they understood their lab results and were offered options when starting/changing medications, 100% of patients responded with “always” or “usually.” Similarly, 100% of respondents agreed their visits were uninterrupted (e.g., by phone calls, other patients, etc.) and complaints about their health care were not ignored. Patients from both clinics were also satisfied with the amount of time spent with providers, their ability to fill HIV medication prescriptions and input into treatment plans, with no significant differences between groups. Fewer patients in the NPC group indicated they “always” or “usually” felt comfortable talking about personal/intimate issues with their providers (73% NPC vs 97% MDC, p < 0.033). However, the majority of patients from both clinics agreed that providers were accepting and nonjudgmental of their life and health care choices and that their privacy was maintained while waiting to see their providers. When asked whether providers contacted them after a visit to see how they were doing, fewer patients in the NPC group responded with “always” or “usually” (10% NPC vs 46% MDC, p < 0.028).
Figure 3.
The HIV clinic visit: MDC vs NPC patient satisfaction*†‡
*Statement wording was changed from negative to positive for presentation of results. †Responses of “did not apply” or “don’t know” are excluded. ‡Questions with response rates of 100% were excluded from the figures. Please see the figure details for more information on these parameters. MDC, multidisciplinary clinic; NPC, nonphysician clinic
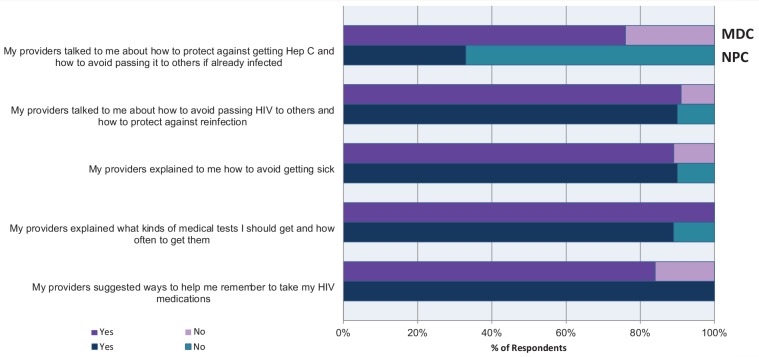
All patients responded “yes” when asked whether the side effects of their HIV medications were explained in a way they could understand. Likewise, there was strong agreement that providers suggested ways to help them remember to take their HIV medications and explained the kinds of medical tests they should have done and how often they should be done (Figure 4). The majority of patients from both clinics also agreed that providers explained how to avoid getting sick and how to avoid passing HIV to others and getting reinfected with a different HIV strain. However, significantly fewer patients in the NPC group noted that providers talked to them about protection against hepatitis C infection and how to avoid passing it to others (33% NPC vs 76% MDC, p < 0.025).
Figure 4.
Patient education: MDC vs NPC patient satisfaction*†
* Responses of “did not apply” or “don’t know” are excluded. †Questions with response rates of 100% were excluded from the figures. Please see the figure details for more information on these parameters. MDC, multidisciplinary clinic; NPC, nonphysician clinic
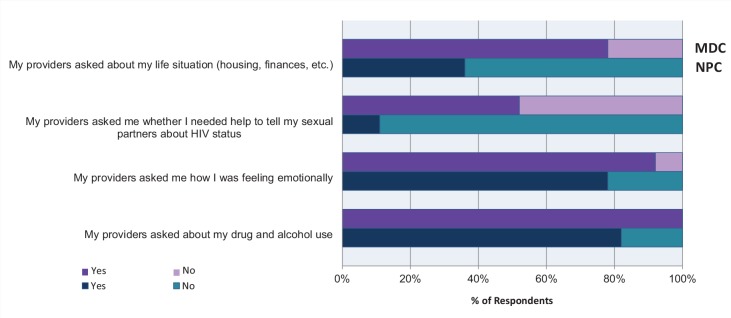
A number of differences were observed in patient responses to questions pertaining to social and psychological issues (Figure 5). MDC patients were more likely to have been asked about housing and finances (78% vs. 36%, p < 0.013), alcohol and drug use (100% vs 82%, p < 0.049) and whether they needed help telling their sexual partners about their HIV status (52% vs 11%, p < 0.036). However, a majority of patients in both groups indicated they were asked about their emotional health during their last clinic visit, with no difference noted between groups.
Figure 5.
Social/psychological issues: MDC vs NPC patient satisfaction*
*Responses of “did not apply” or “don’t know” are excluded. MDC, multidisciplinary clinic; NPC, nonphysician clinic
Respondents expressed a high level of satisfaction with the overall quality of their HIV care in both NPC and MDC clinics (89% vs 93%, respectively, p = 0.6). There were no significant differences in satisfaction with the overall quality of their HIV care between the 2 clinics. Patients rated their providers’ knowledge of the newest developments in HIV care very high in both NPC and MDC clinics (100% vs 83%, respectively, p = 0.3). The majority rated the quality of care received as “better” or “much better” than that of other medical clinics, with 90% of MDC and 97% of NPC patients agreeing they would recommend the clinic to their friends with similar needs. The most common descriptors that respondents from both clinics identified as reflecting their feelings about their HIV care were “caring,” “friendly,” “warm” and “understanding.” Fisher’s exact test did not identify any significant differences between clinics in the reporting of these descriptors.
Multivariate logistic regression did not find that any patient characteristic (age, sex, race, sex orientation, geographic location, disease duration, overall health and time receiving care at their respective clinic) was significantly associated with satisfaction with overall quality of care among respondents.
Discussion
The role of pharmacists in the management of patients with HIV infection is well established.7,8 In the outpatient setting, long-term care of HIV+ patients is shifting from specialist to primary care in many areas. Clinical pharmacists and nurse practitioners have been suggested as a means to improve efficiency of care in patients with HIV.9 In NL, an NPC consisting of an HIV specialist pharmacist and nurse practitioner was implemented out of necessity in the absence of an ID specialist. However, system efficiency and apparent patient acceptance led to sustaining this model of care, in addition to offering full multidisciplinary team care. We undertook this study to more formally assess patient acceptance of receiving care through either clinic, as a lack of acceptance could compromise continuity of care and patient outcomes.
In this study, there was a high level of satisfaction with care received through both the NPC and the MDC. Patients from both clinics were satisfied with their access to care, their clinic visit, the education provided and their overall HIV care. Patients felt they could make appointments that suited their needs and discuss medical questions with their providers by phone/email outside of clinic. Patients were satisfied with their time spent with providers and felt their providers were knowledgeable about new developments in HIV care. Overall, patients viewed their quality of care favourably compared to other clinics.
Patient satisfaction was high for both clinics on questions pertaining to responsibilities and care within the scope of the HIV clinic pharmacist, which was expected since they participate in both the NPC and MDC visits. These included asking for input into treatment plans and giving options when starting/changing medications, explaining HIV medication side effects clearly and suggesting ways to increase medication compliance and facilitating medication refills on prescriptions.
While satisfaction with both clinics was high, some differences were noted, particularly related to social and psychological issues. Some of these differences may be explained by the different complement of health providers who participate in each clinic. Specifically, a social worker does not attend the NPC, although patients have access to her services by appointment outside of their regular clinic visits. Since the survey instructions asked respondents to reflect on their most recent clinic visit experience, ratings from those who last attended the NPC were lower than from those who attended the MDC (which is attended by the social worker), in areas traditionally assessed by the social worker. These topics typically include personal and intimacy issues, finances, housing and HIV disclosure issues.
Similarly, fewer NPC patients noted that their providers discussed hepatitis C infection with them. Counselling about hepatitis C prevention is typically done at the initial intake visit into the program with the nurse practitioner or by the HIV physician in the NL clinic. Interestingly, fewer patients attending the NPC noted their providers asked about drug and alcohol use or contacted them after a visit to see how they were doing. Only 2 patients indicated they had not been asked about this, and both were in the NPC group. Questions about drug and alcohol use are routinely asked at each visit by any team member, including the pharmacist and the nurse practitioner. Response to the question regarding being contacted after the visit for follow-up was not surprising. Contact with a patient after a clinic visit is not routine unless specific issues arise during the visit that require follow-up. As the NPC often serves to accommodate patients with emergent issues between MDC follow-up visits, fewer patients would require follow-up after these visits if their issues were the reason for and addressed at the NPC visit.
Results from this study provide assurance that the NPC is an acceptable model of care to patients and also provide valuable information to inform areas where consistency of care may be improved. This will ensure that each patient receives an optimal care experience, irrespective of the clinic he or she attends.
Studies have suggested that the quality and cost-effectiveness of primary care provided by certain NPCs are similar to that provided by physicians.4 Literature examining whether similar results can be achieved in HIV care continues to grow. Authors of a recent meta-analysis concluded that nonphysician-provided HIV care results in equivalent outcomes (mortality, increase in CD4 levels at 1 year, viral failure at 1 year) to care provided by physicians and may result in decreased patient loss to follow-up.6 Our study is the first descriptive assessment of an NPC comprising a pharmacist and nurse practitioner providing chronic HIV care that we are aware of. Patient satisfaction and acceptance have been demonstrated; however, next steps must include an assessment of clinical outcomes.
This study has several limitations, most notably the small sample size, particularly in the NPC group (n = 11). The survey was conducted over the summer months, which may have limited patient availability, contributing to the small number of respondents. Small sample size could lead to an over- or underrepresentation of patient satisfaction. There is also the possibility of recall bias among respondents. Survey instructions asked that patients answer questions based on their last clinic visit. Since patients attend both the NPC and MDC, alternating every 6 months, it may be difficult to accurately recall their last clinic visit. The same clinic pharmacist and nurse practitioner also attend both clinics, which may further complicate the patient’s ability to accurately recall the last visit. As a result, patients may have responded based on their overall experience with the HIV program rather than their last visit specifically.
The aim of the study was to assess patient satisfaction with the care provided by both the NPC and the MDC. The study was not designed or powered to demonstrate a difference between clinics (i.e., to show superiority or equivalency between clinics). The PSS-HIV underwent a rigorous validation process to help make sure that each item measures the aspect of patient satisfaction intended. We made some minor changes to the survey and while we assessed the face validity of the revised tool, it is possible it may have affected the content validity of the survey. Finally, despite pretesting the survey, the wording of some questions from the PSS-HIV may not have been entirely applicable to our patient population or may have been difficult to understand. For example, the response rate to the question asking patients about their satisfaction with the availability of off-hours care was quite low (n = 7/11 NPC, n = 17/38 MDC). A high number of patients responded “Don’t know” to this question and indicated that they have not had to access off-hours HIV care. More informative responses may have been obtained had the question been asked differently (i.e., “Have you ever needed off-hours HIV care?” “If yes, was this care available when needed?”).
Conclusion
The scope of pharmacy practice has expanded rapidly over the past number of years. In line with this, the development of specialized NPCs to help meet increasing health care demands for a variety of chronic medical conditions is becoming increasingly common. Evidence to support the effectiveness of such clinics continues to grow. A collaborative NPC consisting of an HIV clinic pharmacist and nurse practitioner has provided care to HIV+ patients in NL, as an adjunct to regular MDC visits, for more than 5 years. Patients indicated high satisfaction with the care they receive from both clinics, lending support to the NPC as an innovative model for chronic HIV care. The few differences found underscore the importance of ensuring that care provided by the NPC remains holistic, including referrals to other health professionals as necessary to ensure consistency of care and improve the clinic experience for patients. Comparison of clinical outcomes between clinics is needed to ensure high quality of care for all patients. ■
Footnotes
Author Contributions:J. Kielly and D. V. Kelly conceived the study, oversaw data collection, assisted in data analysis and drafted the manuscript. S. Asghari conducted data analysis and drafted the manuscript. K. Burt assisted with patient recruitment and presentation of data. J. Biggin conducted literature searches, pilot-tested the survey tool, collected data and participated in the interpretation and presentation of data.
Declaration of Conflicting Interests:The authors declare no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Funding:This study was funded by the CIHR Health Professional Student Research Award, Memorial University School of Pharmacy Summer Research Fellowship and the CIHR-funded Living with HIV Innovation Team grant.
References
- 1. Griffiths C, Miles K, Adlam D, et al. A nurse- and pharmacist-led treatment advice clinic for patients attending an HIV outpatient clinic. J Adv Nursing 2007;58(4):320-6. [DOI] [PubMed] [Google Scholar]
- 2. March K, Mak M, Louie S. Effects of pharmacists’ interventions on patient outcomes in an HIV primary care clinic. Am J Health Syst Pharm 2007;64:2574-8. [DOI] [PubMed] [Google Scholar]
- 3. Horberg MA, Hurley LB, Towner WJ, et al. Determination of optimized multidisciplinary care team for maximal antiretroviral therapy adherence. J Acquir Immune Defic Syndr 2012;60:183-90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Sherr KH, Micek MA, Gimbel SO, et al. Quality of HIV care provided by non-physician clinicians and physicians in Mozambique: a retrospective cohort study. AIDS 2010;24(Suppl 1):59-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Agu KA, Oqua D, Agada P, et al. Assessment of satisfaction with pharmaceutical services in patients receiving antiretroviral therapy in outpatient HIV treatment setting. Int J Clin Pharm 2014;36:636-47. [DOI] [PubMed] [Google Scholar]
- 6. New York State Department of Health AIDS Institute. Patient Satisfaction Survey for HIV Ambulatory Care. March 2002. Available: http://nationalqualitycenter.org/resources/patient-satisfaction-survey-for-hiv-ambulatory-care-pdf/ (accessed Aug. 14, 2016).
- 7. Tseng A, Foisy M, Hughes CA, et al. Role of the pharmacist in caring for patients with HIV/AIDS: clinical practice guidelines. Can J Hosp Pharm 2012;65(2):125-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Schafer JJ, Gill TK, Sherman EM, McNicholl IR. ASHP guidelines on pharmacist involvement in HIV care. Am J Health Syst Pharm 2016;73:e72-98. [DOI] [PubMed] [Google Scholar]
- 9. Dave SS, Miles K, Griffiths C, et al. Is it time to rethink the roles of health professionals in the HIV outpatient setting? Sex Transm Infect 2004;80:153. [DOI] [PMC free article] [PubMed] [Google Scholar]