Abstract
AIM:
To determine average personal exposure to nitrous oxide for anaesthesiologists and nurses working in operating rooms (ORs) and intensive care units (ICU) in Clinical Hospital in Shtip, ENT University Clinic in Skopje and General Hospital in Kochani.
METHODS:
To determine TWA exposure nitrous oxide concentration was continuously measured over 8 hours shift within breathing zone of the subjects involved, using the handheld electrochemical instrument with data logging option. Results obtained were statistically processed.
RESULTS:
Highest TWA exposures (well above RELs) were found for nurses and anaesthesiologists in ORs in CH – Shtip, because of high workload in substandard conditions. TWA exposures in CH – Kochani were found to be significantly lower although in substandard conditions, mostly due to lower workload. TWA exposures found in ORs in ENT UC – Skopje is within RELs due to good work practices and proper ORs equipment.
CONCLUSIONS:
Study indicated significant exposure of personal working in substandard ORs in CH – Shtip. Applying proper work practices and maintain control equipment (general ventilation and scavenging systems) in operation, could provide for safe work environment.
Keywords: nitrous oxide, TWA exposure, anaesthesiologists, nurses, substandard
Introduction
Past studies worldwide suggest that chronic exposure to anaesthetic gases of the health care personnel in the operating rooms affect the health of medical staff. The levels of exposure and associated health effects, are subject to different debates in scientific societies at national and international levels. This is especially considered for the oldest and widely used anaesthetic gas N2O (nitrous oxide), continuously used during general anaesthesia in combination with O2. During the long history of wide usage, it has been proven that safe exposure levels are feasible and can be achieved if proper control techniques are in place and properly used [1-7]. On the other side, high exposures are commonly encountered in underequipped hospitals without proper or no ventilation and exhausting system [1, 2, 5, 6].
Considering the lack of scientific data on levels of exposure and associated health effects, especially in smaller and usually under equipped medical centres in Macedonia, the authors has initiated targeted measurement campaign in order to determine average personal exposure to nitrous oxide for anaesthesiologists and nurses working in operating rooms (ORs) and intensive care units (ICU) in underequipped Clinical Hospital (CH) in Shtip. Data obtained were compared with average exposure of same staff operating in fully equipped ENT University Clinic (ENT-UC) in Skopje and General Hospital (GH) in Kochani as local hospital with lower operating procedures frequency (low work burden). Additional set of data collected (work organisation, ventilation and scavenging equipment status) were used to determine the factors leading to higher exposure and recommend improvements.
Materials and Methods
As per definition time-weighted average (TWA) is the average exposure over a specified period, usually a nominal eight hours. To determine TWA exposure for anaesthesiologists and nurses, nitrous oxide concentration was continuously measured over 8 hours shift within breathing zone of the subjects involved, using the handheld electrochemical instrument with data logging option.
The study involved 8 MD anaesthesiologists and 13 nurses, randomly selected and monitored during the period of 18 workdays starting from 01.01 and ending 28.02.2014.
Measurements were taken with specifically designed nitrous oxide analyser G 200 from Bedfont Scientific Ltd, England, equipped with a highly sensitive infrared sensor with a measurement range from 0 to 1.000 ppm, 1 ppm resolution and precision of ± 5 ppm for 0-100 ppm range and ± 1.5% for 101ppm and above. The instrument was calibrated with span gas before the start of each measurement (shift).
Subjects involved wearing the instrument placed in a side bag with special belt and support for tube attachment within wearer breathing zone, thus allowing for continuous 8 hours monitoring in their real microenvironment, regardless of the conditions and activities performed.
Results obtained were statistically processed. Quantitative data distribution was determined using Kolmogorov-Smirnov test and Shapiro-Wilks W tests for normality.
Data were described using central tendency parameters (arithmetic mean/average) and dispersion parameters (standard deviation).
Differences between the arithmetic mean for two independent variables with a normal distribution (anaesthesiologist/nurses) were tested for significance using Student - t-test. For not normally distributed variables a non-parametric Mann-Whitney - u - test was used. Differences between three and more arithmetic mean for independent variables were tested for significance using Kruskal-Wallis ANOVA. Results having p < 0.05 with confidence interval CI = 95% were taken as significant.
Results
Results obtained from all measurements were presented in tables and figures below.
Table 1 presents measured N2O (ppm) concentrations and TWA for anaesthesiologists and nurses in ORs of CH-Shtip during the first measurement campaign. Results presented indicate that are no statistical differences for lowest measured concentrations in ORs between anaesthesiologists and nurses (Mann-Whitney U Test: Z = - 0.475; p = 0.6350). However, data shows that nurses are exposed to significantly higher maximal nitrous oxide concentrations when compared to anaesthesiologists (Student t-test: t = - 1.997; p = 0.0479).
Table 1.
Results obtained in ORs during the measurement campaign January - February 2014 in CH – Shtip
| N2O (ppm) | Operating Rooms | |||||
|---|---|---|---|---|---|---|
| Doctors | Nurses | |||||
| Min | Max | Mean ± SD | Min | Max | Mean ± SD | |
| The lowest values | 0 | 23 | 4.89 ± 7.95 | 0 | 41 | 7.61 ± 12.03 |
| The highest values | 174 | 3771 | 1536.61 ± 911.18 | 167 | 3814 | 2100.17 ± 827.39 |
| TWA | 138 | 908 | 478.11 ± 236.25 | 295 | 921 | 677.44 ± 192.41 |
Table 2 presents measured N2O (ppm) concentrations and TWA for anaesthesiologists and nurses in ICUs in CH-Shtip. Data obtained indicate lower exposures compared to ORs, but there are statistically significant differences between exposures of nurses and anaesthesiologists, for minimal measured concentrations (Student t-test: t = - 4.090; p = 0.00025), maximal concentrations (Student t - test: t = - 3.987; p = 0.00034) and TWA exposures (Student t-test: t = - 3.912; p = 0.00041). In general nurses are significantly more exposed than anaesthesiologists (Table 2).
Table 2.
Results obtained in ICU during the measurement campaign January-February 2014 in RCH- Shtip
| N2O (ppm) | Intensive Care Units | |||||
|---|---|---|---|---|---|---|
| Doctors | Nurses | |||||
| Min | Max | Mean ± SD | Min | Max | Mean ± SD | |
| The lowest values | 2 | 22 | 11.50 ± 5.70 | 5 | 41 | 21.83 ± 9.07 |
| The highest values | 12 | 57 | 32.17 ± 12.53 | 23 | 79 | 52.89 ± 18.20 |
| TWA | 9 | 34 | 20.06 ± 7.56 | 17 | 51 | 31.94 ± 10.45 |
Figure 1 presents characteristic exposure profile of anaesthesiologists and nurses during one operative session in ORs in CH–Shtip. Data presented are based on measurements from 16.01.2014, and all other measurement sessions during the first campaign give similar profiles.
Figure 1.
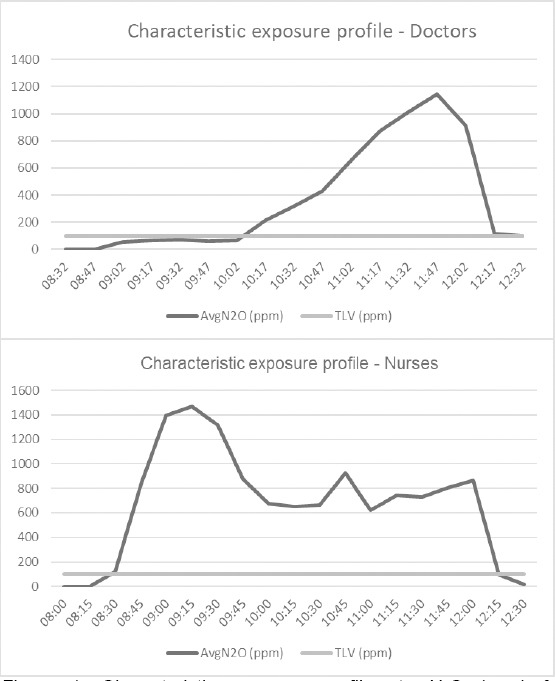
Characteristic exposure profiles to N2O (ppm) for anaesthesiologist and nurses during one operative session in ORs in CH-Shtip
Table 3 gives comparison of N2O (ppm) concentrations and TWA exposures for anaesthesiologists and nurses, measured in ORs in CH–Shtip, GH–Kochani and ENT UC-Skopje. Variance analysis has shown statistically significant differences between TWA exposures of anaesthesiologists and nurses to N2O (ppm) in ORs in all hospitals involved (Kruskal-Wallis ANOVA: H = 20.741, p = 0.009).
Table 3.
TWA exposures of anaesthesiologists to N2O (ppm) in ORs in CH – Shtip, GH – Kochani and ENT UC - Skopje
| Operating rooms | ||||||
|---|---|---|---|---|---|---|
| N2O (ppm) | Doctors | Nurses | ||||
| TWA | Min | Max | Mean ± SD | Min | Max | Mean ± SD |
| Shtip | 138 | 908 | 478.11 ± 236.25 | 295 | 921 | 677.44 ± 192.40 |
| Kochani | 116 | 210 | 163.00 ± 66.47 | 453 | 577 | 512.67 ± 62.13 |
| Skopje | 55 | 72 | 63.50 ± 12.02 | 69 | 89 | 77.50 ± 12.02 |
TWA exposure differences between anaesthesiologists in CH - Shtip and GH - Kochani (Mann-Whitney U Test: Z = -3.340; p = 0.00083), CH - Shtip and ENT UC - Skopje (Mann-Whitney U Test: Z = -4.304; p = 0.00001) and GH - Kochani and ENT UC - Skopje (Mann-Whitney U Test: Z = - 2.285; p = 0.0223) was statistically significant. Also a difference between exposures of nurses in CH - Shtip and GH - Kochani was noted, but it was found not to be statistically significant (Mann-Whitney U Test: Z = -1.889, p = 0.0589).
Discussion
Concentrations measured in all hospitals during our study were within the values measured elsewhere as reported in the literature [1-3, 6, 7]. Highest concentrations of N2O in ORs were measured within nurses breathing zone. There is a statistically significant difference between TWA exposure of nurses and anaesthesiologists in CH-Shtip and nurses are found to be more exposed than doctors (p < 0.05).
Concentrations found in ICUs are significantly lower compared to ORs, and therefor TWA exposure for personnel in ICUs is significantly lower (p < 0.05), but also here nurses are found to be more exposed compared to anaesthesiologists (p < 0.05).
Higher exposure of nurses is probably due to work organisation within the hospitals, as due to lack of personnel, the anaesthesiologists usually cover 2 ORs, therefore moving between them, while nurses stay during all procedure near the source (patient head).
Evaluating TWA exposure to N2O (ppm) study found a similar level of exposure for nurses and anaesthesiologists (p > 0.05), but values found are significantly higher than recommended exposure values (REL). REL varies in different countries starting from 25 ppm in USA (NIOSH) and Australia (Safe Works), 50 ppm in Belgium, Denmark, New Zealand, Singapore, Bulgaria, Columbia, Argentina and South Korea and up to 100 ppm in Deutschland, Italy, Norway, Sweden, Switzerland, UK and Finland [6, 8-14]. TWA exposures found within the study were from 2 to 12 times higher that highest REL.
A comparative study between CH – Shtip, GH – Kochani and ENT UC – Skopje show significant differences (p = 0.009) for TWA exposures in ORs of different hospitals. Highest TWA exposures (well above RELs) were found for nurses and anaesthesiologists in ORs in CH – Shtip, because of high workload in substandard conditions as the ORs were not equipped with general ventilation systems nor with local exhaust scavenging. TWA exposures in CH – Kochani were found to be significantly lower although in substandard conditions, mostly due to lower workload (frequency and duration of procedures performed). On the other side, TWA exposures found in ORs in ENT UC – Skopje are within RELs due to good work practices and proper ORs equipment (general ventilation and scavenging equipment operational).
In conclusion, study undoubtedly indicated significant exposure of personal working in substandard ORs in CH – Shtip were TWA reach up to 12 times above highest REL. Significant workload and luck of personnel only worsen the situation, leading directly to higher exposure for nurses and doctors altogether. Nurses were found to be more exposed compared to anaesthesiologists due to specific work organisations. Applying proper work practices and maintain control equipment (general ventilation and scavenging systems) in operation, could provide for safe work environment as of ENT UC – Skopje has shown.
Footnotes
Funding: This research did not receive any financial support.
Competing Interests: The authors have declared that no competing interests exist.
References
- 1.Maroufi ShS, Gharavi M, Behnam M, Samadikuchaksaraei A. Nitrous oxide levels in operating and recovery rooms of Iranian hospitals. Iran J Public Health. 2011;40(2):75–9. PMid:23113075 PMCid:PMC3481765. [PMC free article] [PubMed] [Google Scholar]
- 2.Krajewski W, Kucharska M, Wesolowski W, Stetkiewicz J, Wronska-Nofer T. Occupational exposure to nitrous oxide –the role of scavenging and ventilation systems in reducing the exposure level in operating rooms. International Journal of Hygiene and Environmental Health. 2007;210:133–38. doi: 10.1016/j.ijheh.2006.07.004. https://doi.org/10.1016/j.ijheh.2006.07.004 PMid:17045524. [DOI] [PubMed] [Google Scholar]
- 3.Changi WP, Kaui C-W, Hseu S-S. Exposure to nitrous of Anaesthesiologists during Paediatric Anaesthesia. Industrial Health. 1997;35:112–118. doi: 10.2486/indhealth.35.112. https://doi.org/10.2486/indhealth.35.112. [DOI] [PubMed] [Google Scholar]
- 4.Hoerauf K, Funk W, Harth M, Hobbhahn J. Occupational exposure to sevoflurane, halothane and nitrous oxide during paediatric anaesthesia. Anaesthesia. 1997;52(3):215–9. doi: 10.1111/j.1365-2044.1997.070-az0061.x. https://doi.org/10.1111/j.1365-2044.1997.070-az0061.x PMid:9124660. [DOI] [PubMed] [Google Scholar]
- 5.Grey WA. Occupational exposures to nitrous oxide in four hospitals. Anaesthesia. 1989;44:511–514. doi: 10.1111/j.1365-2044.1989.tb11383.x. https://doi.org/10.1111/j.1365-2044.1989.tb11383.x. [DOI] [PubMed] [Google Scholar]
- 6.Henderson KA, Matthews IP. An environmental survey of compliance with Occupational Exposure Standards (OES) for anaesthetic gases. Anaesthesia. 1999;54(10):941–947. doi: 10.1046/j.1365-2044.1999.01032.x. https://doi.org/10.1046/j.1365-2044.1999.01032.x PMid:10540057. [DOI] [PubMed] [Google Scholar]
- 7.Davenport HT, Halsey MJ, Wardley-Smith B, Bateman PE. Occupational exposure to anaesthetics in 20 hospitals. Anaesthesia. 1980;35:354–9. doi: 10.1111/j.1365-2044.1980.tb05116.x. https://doi.org/10.1111/j.1365-2044.1980.tb05116.x PMid:7435894. [DOI] [PubMed] [Google Scholar]
- 8.Borm PJA, Kant I, Houben G, van Rijssen-Moll M, Henderson PT. Monitoring of nitrous oxide in operating rooms:Identification of sources and estimation of occupational exposure. Journal of Occupational Medicine. 1990;32:1112–6. doi: 10.1097/00043764-199011000-00014. https://doi.org/10.1097/00043764-199011000-00014 PMid:2258770. [DOI] [PubMed] [Google Scholar]
- 9.Wood C, Ewen A, Goresky G. Exposure of operating room personnel to nitrous oxide during paediatric anaesthesia. Canadian Journal of Anaesthesiology. 1992;39:682–6. doi: 10.1007/BF03008230. https://doi.org/10.1007/BF03008230 PMid:1394756. [DOI] [PubMed] [Google Scholar]
- 10.Khine HH, Corddry DH, Kettrick RG, et al. Comparison of cuffed and uncuffed endotracheal tubes in young children during general anaesthesia. Anaesthesiology. 1997;86:627–31. doi: 10.1097/00000542-199703000-00015. https://doi.org/10.1097/00000542-199703000-00015. [DOI] [PubMed] [Google Scholar]
- 11.Sonander H, Stenqvist O, Nilsson K. Nitrous oxide exposure during routine automated method. Anaesthesiology. 1980;53:424–6. [Google Scholar]
- 12.McGill WA, Rivera O, Howard R. Time-weighted averaging for nitrous oxide:An automated method. Anaesthesiology. 1980;53:424–6. doi: 10.1097/00000542-198011000-00008. https://doi.org/10.1097/00000542-198011000-00008. [DOI] [PubMed] [Google Scholar]
- 13.Baum VC, Willschke H, Marciniak B. Is nitrous oxide necessary in the future? Paediatric Anaesthesia. 2012;22(10):981–7. doi: 10.1111/pan.12006. https://doi.org/10.1111/pan.12006 PMid:22967156. [DOI] [PubMed] [Google Scholar]
- 14.Panni MK, Corn SB. The use of a uniquely designed anesthetic scavenging hood to reduce operating room anesthetic gas contamination during general anesthesia. Anesthesia & Analgesia. 2002;95(3):656–60. doi: 10.1097/00000539-200209000-00030. PMid:12198055. [DOI] [PubMed] [Google Scholar]


