Abstract
Introduction
This study investigated outcomes in critically unwell acute kidney injury patients and the role of the National Early Warning Score and other factors in identifying patients who experience negative outcomes.
Methods
Retrospective cohort study investigating 64 patients seen by Critical Care Outreach between November 2014 and February 2015. Mortality at one year was analysed using multivariate regression; all other statistical tests were non-parametric.
Results
Forty-four per cent of patients required escalation to higher level care, 56% failed to survive beyond one year and 30% of those who did survive had a deterioration in renal function. Previous acute kidney injury significantly predicted mortality but the National Early Warning Score did not. A subgroup of patients developed Stage 3 acute kidney injury before a rise in National Early Warning Score.
Conclusions
Acute kidney injury in the Critical Care Outreach patient population is associated with high morbidity and mortality. Previous acute kidney injury and acute kidney injury stage may be superior to the National Early Warning Score at identifying patients in need of Critical Care Outreach review.
Keywords: Acute kidney injury, critical care, critical care outcomes, early diagnosis, mortality
Introduction
Identifying acutely unwell patients early and initiating a timely response with appropriate clinical expertise is crucial to optimising patient outcomes.1 Early warning scores achieve these aims by monitoring various routinely measured physiological parameters and assigning points for abnormal results, triggering escalation to different levels of care. In an attempt to standardise local hospital scoring systems, the Royal College of Physicians (RCP) produced the National Early Warning Score (NEWS).1 The NEWS has been shown to be effective at identifying patients at risk of acute mortality in the general hospital population.2 However, many clinical factors were not included in the NEWS and the RCP recommends that further research evaluating how effective the NEWS is at identifying patients who will go on to experience poor outcomes is required.1
Patients who become acutely unwell with acute kidney injury (AKI) are often identified late and suffer poor outcomes.3 AKI is a syndrome characterised by sudden loss of renal function resulting in disruption to fluid, acid–base and electrolyte homeostasis; it is both a frequent cause and consequence of acute illness.4 It is unsurprising, therefore, that as many as 36% of patients admitted to intensive care units (ICUs) have an AKI.5 The mortality rate associated with AKI in these acutely unwell patients has been estimated to be in excess of 50%.6,7 AKI is both preventable and treatable; however, these patients are frequently poorly identified and managed. In 2009, it was reported that only 43% of the patients with AKI who required a review by critical care received one.3 Furthermore, only half of the patients who died of AKI were judged to have received a good standard of care.3
Critical Care Outreach (CCO) Teams aim to bring ICU expertise to the ward, facilitating earlier identification of unwell patients and prompt escalation of care. Patients with AKI who are reviewed by CCO are a unique patient population: current literature evaluating outcomes in patients with AKI has focussed on patients admitted to general wards or ICUs.8–18 Data on the outcomes and journeys of patients with AKI seen by CCO on the wards are currently lacking. In particular, there is a deficit of literature on the utility of the NEWS and other clinical factors in identifying which of these patients will go on to experience negative outcomes. Furthermore, many of the current studies have used outdated definitions for AKI, reducing the applicability of these studies to current clinical practice.8–15,17 Additionally, the majority of studies have ended follow-up at discharge from hospital, which may have resulted in the morbidity and mortality associated with AKI in critically ill patients being underestimated.8,10–18
Therefore, a study describing the outcomes of critically ill patients with AKI, using the current consensus definition, and evaluating the efficacy of the NEWS and other clinical factors in predicting these outcomes is required.
Aims
To describe the outcomes patients who are critically unwell with AKI experience
To evaluate the role of the NEWS and other clinical factors in identifying patients who will go on to experience negative outcomes
To improve the identification of acutely unwell patients with AKI in need of greater care
Methods
This is a retrospective cohort study using data collected from patients’ electronic health records.
Study population
Patients were recruited if they had been referred to the CCO team at the Leeds Teaching Hospitals NHS Trust (LTHT) between November 2014 and February 2015. Patients were not recruited if they had advanced pre-existing chronic kidney disease (CKD), defined as an estimated Glomerular Filtration Rate ≤30 ml/min/1.73 m2 recorded in the three months prior to referral.
Furthermore, patients referred to CCO without AKI were excluded. Patient’s with AKI were identified using serum creatinine values and staged using the Kidney Disease Improving Global Outcomes criteria.19
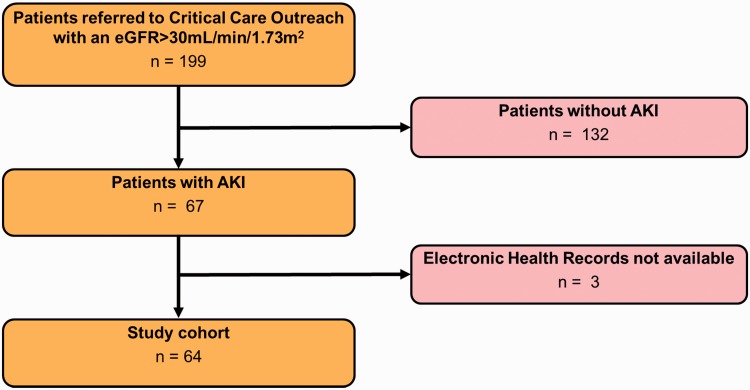
Three patients were lost from the study as their electronic health records were not available. This resulted in a final sample of 64 patients (Figure 1).
Figure 1.
Study recruitment and selection.
Statistical analysis
Prior to analysis the significance level for all statistical tests was set at p<0.05.
Summary statistics are displayed as the number and proportion of patients with a characteristic out of the total number of patients for which there were data available. Biomarker responsiveness to acute illness and deterioration was analysed by plotting the day at which each biomarker reached its peak/nadir, i.e. most abnormal value. This provided frequency data for each day, relative to referral.
Mortality data were analysed using a Cox proportional hazards model. Univariate and multivariate analyses are shown as crude and adjusted hazard ratios with associated p values. The variables included within the multivariate model were selected based on clinical relevance. Kaplan–Meir curves were drawn for variables found to be significantly associated with hazard of death.
The mean change in potassium (K+), bicarbonate (HCO3−) and serum creatinine (SCr) from either four or five days prior to referral to the date of referral was calculated. Likewise, the mean change in C-reactive protein (CRP) and white cell count (WCC) from either nine or 10 days prior to referral to the date of referral was calculated. Where data were available on both dates (day four and five or day nine and 10) the earlier data were used. Results are stratified by mortality. Mann–Whitney U tests were completed to determine whether biochemistry deteriorated significantly more in the patients who died.
Finally, to demonstrate the pattern of biomarker deterioration in patients who survived and those who did not, line charts stratified by mortality and plotting the number of patients against the day when K+, HCO3−, SCr, CRP and WCC became most abnormal were plotted.
Ethics
This study was reviewed by The University of Leeds and classed as a service evaluation, so formal ethics approval was not required. This was confirmed with Leeds Teaching Hospitals Trust.
Results
Patient characteristics
The median age of patients included in the study was 67 (IQR 23–88), with a skew towards increased age. There was an approximately even mix of males and females (53%, 47%).
Most patients were referred from medical rather than surgical specialties (72%, 28%). A significant proportion (27%) of patients had more than one cause for their AKI. Sepsis was a contributing factor in 44% of cases. Nineteen per cent of patients had a cardiogenic contribution (e.g. acute coronary syndrome) and 17% suffered another pre-renal insult (gastrointestinal loss, acute haemorrhage, prolonged hypotension). Renal causes were implicated in 6% of cases (pyelonephritis, NSAID use), and post-renal factors contributed in 10% of patients (urinary stones or retention). Eleven patients had a diagnosis of malignancy (17%), of which five patients were neutropenic (8%). Three patients (5%) had previously received solid organ transplants, and two (3%) had suffered a previous cardiac arrest. In summary, the study comprised a complex cohort of patients from a large teaching hospital which serves as a tertiary oncology and transplant centre. The resuscitation status of patients within the cohort was not known to the authors.
The higher the NEWS category the greater the proportion of patients; 22% were classed as having a low score (1–4), 23% a medium score (5–6) and 55% a high score (≥7). Around half (53%) of the cohort had a fluid balance chart in place at the time of referral (Table 1).
Table 1.
Patient characteristics at referral.
| Characteristics | n (%) |
|---|---|
| Demographics | |
| Age ≥ 65 | 39/64 (61%) |
| Male | 34/64 (53%) |
| Fluid balance chart present | 34/64 (53%) |
| Chronic kidney disease | |
| CKD Stage 1 | 30/63 (47%) |
| CKD Stage 2 | 20/63 (32%) |
| CKD Stage 3 | 13/63 (21%) |
| Acute kidney injury (AKI) stage | |
| Stage 1 | 32/64 (50%) |
| Stage 2 | 12/64 (19%) |
| Stage 3 | 20/64 (31%) |
| Previous AKI in the last 12 months | 29/64 (45%) |
| NEWS | |
| 1–4 (low) | 14/64 (22%) |
| 5–6 (medium) | 15/64 (23%) |
| ≥7 (high) | 35/64 (55%) |
| Diagnosis of sepsis | 27/62 (44%) |
| Biochemistry | |
| Potassium > 5.5 mmol/la | 10/63 (16%) |
| Bicarbonate < 22 mmol/la | 31/46 (67%) |
| White cell count > 11 × 109 /la | 35/64 (53%) |
| CRP > 10 mg/la | 59/61 (97%) |
| Referring speciality | |
| Medicine | 46/64 (72%) |
| Surgery | 18/64 (28%) |
CKD: chronic kidney disease; CRP: C-reactive protein; NEWS: National Early Warning Score.
Normal ranges taken from Leeds Teaching Hospitals Pathology, Clinical information and support.20
Renal function
Approximately half of the cohort had some level of pre-existing CKD greater than Stage 1 (47%). The number of patients with each stage of CKD fell with increasing severity from those with Stage 2 CKD (32%) to Stage 3 (21%). Patients with Stage 4 and 5 CKD were not included in the study cohort.
Just under half (45%) of the patients had been diagnosed with a previous AKI in the last year.
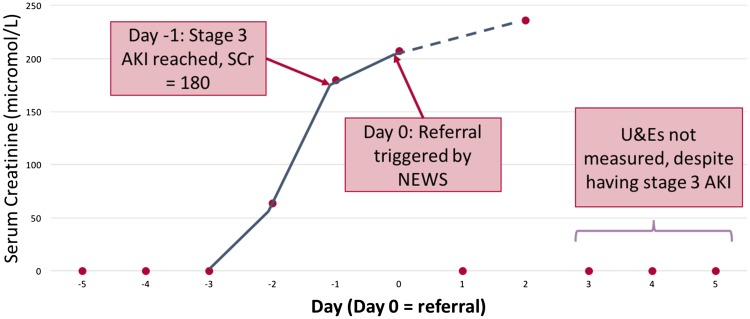
At referral half of the cohort had a Stage 1 AKI (50%). Otherwise, Stage 3 AKI was more frequently diagnosed than Stage 2 (31%, 19%) (Table 1). Of the patients who developed Stage 3 AKI 45% did so before the day of referral. This is demonstrated in a case study of a patient who developed Stage 3 AKI prior to referral (Figure 2).
Figure 2.
Example patient with Stage 3 AKI prior to referral. Patient characteristics: 69 years old, female, baseline serum creatinine = 57. AKI: acute kidney injury.
Biomarkers
A small proportion of patients (16%) fulfilled the criteria for hyperkalaemia (K+ > 5.5 mmol/l) at referral. Conversely, a large proportion (67%) of patients had derangement of acid–base balance and a low (<22 mmol/l) HCO3− level. Almost all (97%) of the patients in this cohort had a raised CRP (>10 mg/l) at referral. Furthermore, over half (53%) of the patients studied had a raised WCC (>11 × 109/l) (Table 1).
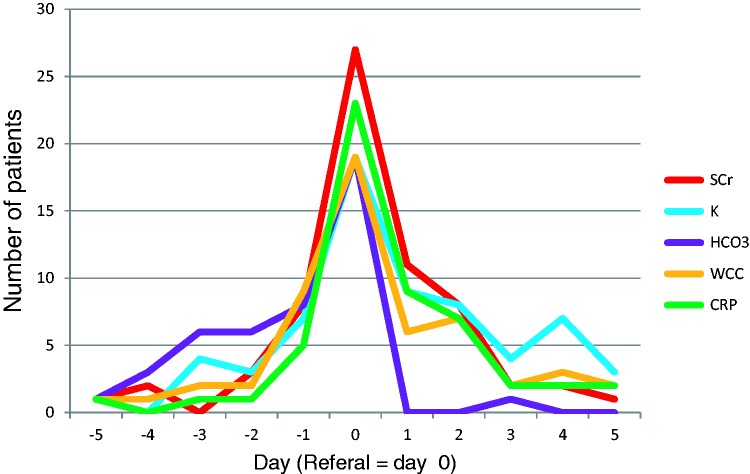
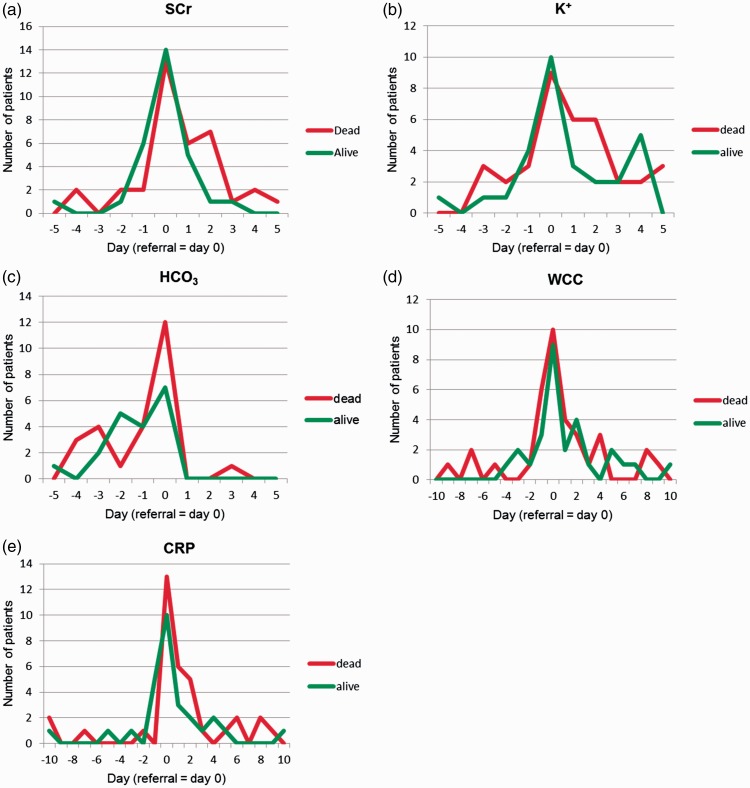
The number of patients experiencing maximal biomarker derangement peaked on the day of referral (Figure 3).
Figure 3.
Timing of maximal biomarker derangement. For SCr, K+, WCC and CRP the number of patients who had their highest recorded levels of these blood components on each day relative to referral have been plotted. For HCO3− the number of patients who had their lowest recorded levels of this blood component on each day relative to referral has been plotted. CRP: C-reactive protein; WCC: white cell count.
Outcomes
A large proportion of patients were escalated to level two or three care (44%). The majority of these patients were escalated to ICUs (68%) rather than high dependency units (32%). Only a small minority of patients required renal replacement therapy (6%).
Over half (56%) of patients died in the year following referral. The majority (72%) of these patients died whilst in hospital. In those patients who survived to discharge, a similar proportion of patients died between discharge and three months as between three and 12 months (11%, 17%).
In those patients who survived a large proportion (30%) suffered a deterioration in long-term renal function and an increase in CKD stage. The proportions of patients progressing to each CKD stage were similar and ranged from 4% (Stage 5) to 11% (Stage 3) (Table 2).
Table 2.
Patient outcomes.
| Outcomes | n (%) |
|---|---|
| Escalation to level 2/3 care | 28/64 (44%) |
| Admitted to the intensive care unit | 19/28 (68%) |
| Admitted to the high dependency unita | 9/28 (32%) |
| Required renal replacement therapy | 4/64 (6%) |
| One-year mortality | 36/64 (56%) |
| Proportion of deaths in hospital | 26/36 (72%) |
| Proportion of deaths from discharge to three months | 4/36 (11%) |
| Proportion of deaths from three to 12 months | 6/36 (17%) |
| Progression to chronic kidney disease | 8/27 (30%) |
| Stage 2 | 2/27 (7%) |
| Stage 3 | 3/27 (11%) |
| Stage 4 | 2/27 (7%) |
| Stage 5 | 1/27 (4%) |
Includes two patients escalated to the respiratory high dependency unit.
Survival analysis
Univariate analysis
The univariate models showed age, previous AKI, higher AKI stage at referral and high WCC to be associated with an increased hazard of death. Conversely, a NEWS ≥ 7, a diagnosis of sepsis, hyperkalaemia and low HCO3− were associated with a decreased hazard of death. The presence of CKD and the use of fluid balance charts were not associated with mortality.
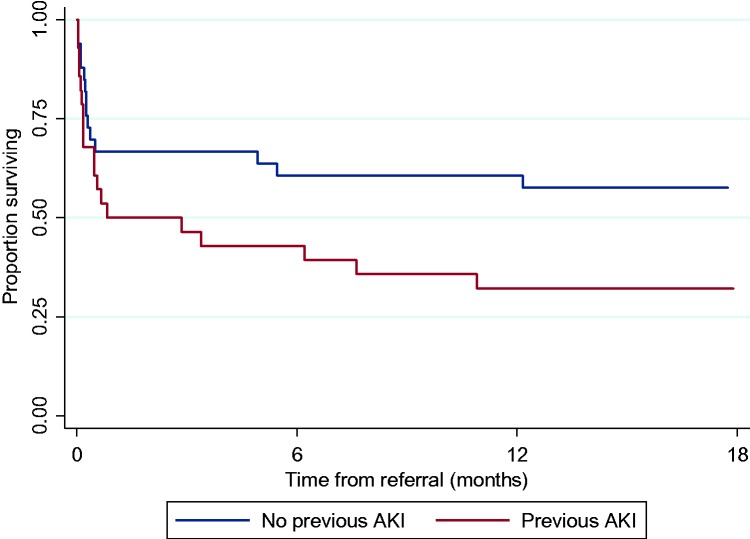
Compared to those patients who did not have a previous AKI, the proportion of patients surviving who have had a previous AKI falls most drastically between one and five months. Otherwise the mortality rate in both groups appears to be similar (Figure 4).
Figure 4.
Survival curves for patients with and without a previous acute kidney injury.
Multivariate analysis
The multivariate model also showed age to be associated with increased hazard of death, albeit with reduced magnitude. AKI stage was not found to be associated with mortality. Conversely, the magnitude of the association between hazard of death and a high WCC increased. In contrast to the univariate analysis, a NEWS ≥ 7 was associated with an increased hazard of death. The presence of CKD became associated with a slight increase in mortality. A diagnosis of sepsis, hyperkalaemia and low HCO3− remained associated with a reduced hazard of death. Unlike the univariate analysis, use of a fluid balance chart was also associated with a reduced hazard of death. These associations, however, did not reach statistical significance. The magnitude of the association between previous AKI and hazard of death increased and became statistically significant (Table 3).
Table 3.
Hazard of death.
| Characteristics | Crude hazard ratio (univariate) (p value) | Adjusted hazard ratio (multivariate) (p value) |
|---|---|---|
| Age ≥ 65 | 1.9 (0.09) | 1.6 (0.34) |
| Fluid balance chart present | 1.0 (0.97) | 0.8 (0.68) |
| Chronic kidney disease | 1.0 (0.65) | 1.1 (0.89) |
| Acute kidney injury (AKI) stage > 1 | 1.5 (0.26) | 1.0 (0.98) |
| Previous AKI in the last 12 months | 1.9 (0.07) | 2.6 (0.04) |
| NEWS ≥ 7 | 0.9 (0.66) | 1.2 (0.67) |
| Diagnosis of sepsis | 0.9 (0.68) | 0.5 (0.14) |
| Potassium > 5.5 mmol/la | 0.7 (0.45) | 0.6 (0.50) |
| Bicarbonate < 22 mmol/la | 0.8 (0.66) | 0.5 (0.20) |
| White cell count > 11 × 109 /la | 1.3 (0.44) | 2.0 (0.23) |
NEWS: National Early Warning Score.
Normal ranges taken from Leeds Teaching Hospitals Pathology, Clinical information and support.20
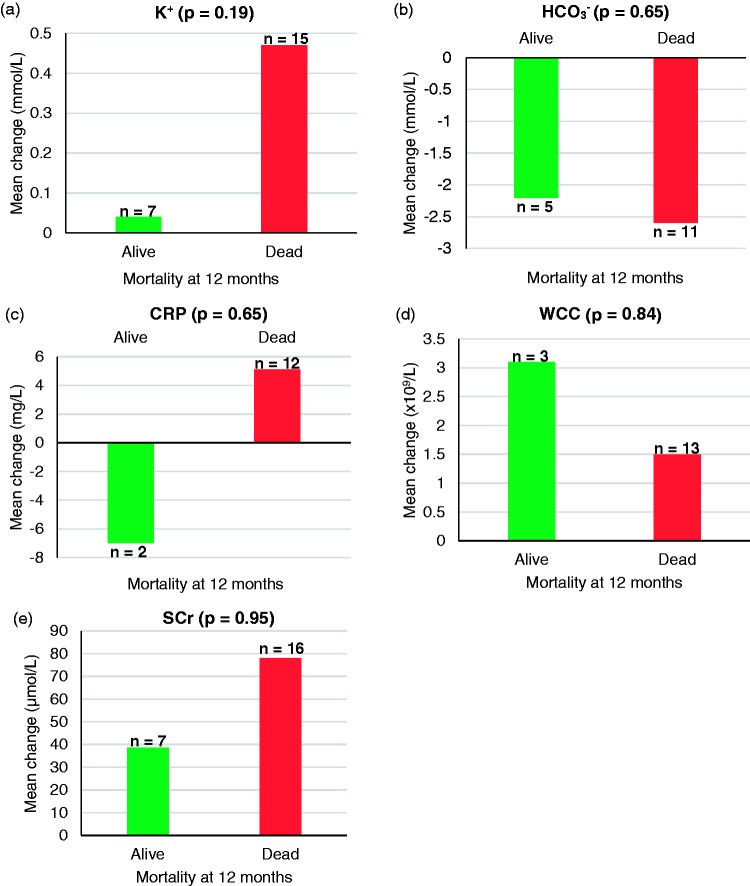
Mean average changes in biomarkers
The mean average increases in K+ and SCr from five days before referral to referral were greater in those patients who did not survive than those who did. Similarly, the mean average fall in HCO3− from five days prior to referral to referral was also greater in those patients who did not survive. Furthermore, the mean average increase in CRP from nine or 10 days before referral to referral was greater in those patients who did not survive; on average CRP levels were lower at referral than at nine or 10 days prior to referral in those patients who survived. Conversely, the mean average increase in WCC from nine or 10 days before referral to referral was greater in those patients who survived than those who did not. None of these results were statistically significant (Figure 5).
Figure 5.
Mean change in biomarkers stratified by mortality. Mean change in biomarkers from day −4/5 (K+, HCO3−, SCr) or −9/10 (WCC, CRP) to referral, stratified by mortality. CRP: C-reactive protein; WCC: white cell count.
Biomarker trends
The majority of patients, both those patients who survived and those that did not, experienced their most abnormal biomarkers on the day of referral (Figure 6).
Figure 6.
Timing of maximal biomarker derangement stratified by mortality. For SCr, K+, WCC and CRP, the number of patients who had their highest recorded levels of these blood components on each day relative to referral has been plotted. For HCO3− the number of patients who had their lowest recorded levels of this blood component on each day relative to referral has been plotted. CRP: C-reactive protein; WCC: white cell count.
In the cohort of patients who did not survive there was a subgroup who experienced their most extreme biomarkers between four and two days prior to referral: this trend is most pronounced with K+ (Figure 6(b)) and HCO3− (Figure 6(c)), but can also be seen with SCr (Figure 6(a)) and WCC (Figure 6(d)).
Conversely, no patients who survived experienced their highest WCC during this time period (Figure 6(d)). There were a series of peaks in patients experiencing their highest CRP in the days leading up to referral in both those patients who survived and those that did not (Figure 6(e)).
In the days following referral, there were several small peaks in the number of patients experiencing their most abnormal biomarkers (Figure 6). In those patients who did not survive these peaks tended to occur at earlier time points and or be greater at earlier time points compared to those patients who survived. This pattern is most evident in SCr at two days post referral, K+ at one to two days post referral and CRP at two days post referral (Figure 6(a), (b) and (e)).
Discussion
This study’s aims was twofold: describe the outcomes of AKI patients seen by CCO, and determine the role of NEWS and other clinical factors in predicting those outcomes to aid the early identification of those patients in need of greater care. The outcomes as described above are predominantly poor, with a large proportion of patients dying, being escalated to higher level care and developing CKD.
The only significant predictor of mortality was previous AKI, although associations were seen with age, AKI stage and WCC. While a high NEWS was associated with increased mortality, this was not significant. No factors were found to be associated with escalation to level 2/3 care.
Outcomes
The literature reveals a wide range of figures for AKI mortality between centres, with in-hospital mortality ranging from 1613 to 73%.16 While there is a paucity of long-term outcomes data, centres report 90-day and one-year mortality as 33.7%18 and 65%,17 respectively. Despite investigating the CCO population, the mortality rate following AKI reported in this study (56%) is consistent with results previously reported in the literature, conducted primarily on patients in the ward or ICU environment. This suggests that the mortality rate for patients with AKI in LTHT is in keeping with other centres, and that existing research also applies to patients seen by CCO teams.
There was an absence of previous literature to compare frequency of escalation to level 2/3 care. Given that critical care teams are only called to see patients who are thought to be very unwell it is unsurprising that a large proportion of patients were escalated to higher level care.
Predictors of mortality
Factors associated with death
This paper found a higher age in patients who died, corroborating the findings in the literature.14,18 Previous AKI was shown to significantly predict mortality at one year; this increase in mortality rate occurred mainly in months 1–5 after admission. This suggests that some of the damage to the kidneys through AKI persists, much like stroke, and renders them more vulnerable to further insult. This would be in keeping with the fact that the elderly and those with CKD, who have less functional reserve, are more susceptible to AKI.21 The authors were unable to find literature to confirm or refute this finding, although a single episode of AKI has been shown to impact long-term mortality in septic patients.22 Interestingly, no association was seen in this study between CKD and mortality from AKI.
Stage of AKI was not shown to be associated with mortality. This contrasts with a body of existing research – with larger samples – who show a positive association between high AKI stage and increased mortality using a variety of definitions.13,14,18,19 Other non-significant predictors of mortality included a raised WCC > 11 × 109 /l and a NEWS ≥ 7. This suggests that patients who are more unwell have a higher mortality rate. This study also found greater aberrations in bicarbonate and potassium values in patients who died, supporting this idea. However, since none of these factors reached significance, they appear to be poor predictors of mortality.
Factors associated with survival
Sepsis
In this sample a large number of patients had a diagnosis of sepsis. This supports established data that in the critically unwell sepsis accounts for 50% of AKI.23 The same study found sepsis – as opposed to other causes of AKI – to be independently associated with mortality. This was not seen in our sample, although an association was seen between WCC and mortality. This is likely a sample effect – our patient group included several with neutropenic sepsis, and also many more with multifactorial AKI. Sepsis-induced AKI is a distinct clinical entity, shown to have its own pathophysiology.24
Fluid balance chart
Both univariate and multivariate analysis showed survival to one year to be independent of fluid balance chart use, as had been found in previous work on the same dataset.25 While there is an argument that documenting fluid balance could allow early intervention to maintain neutral balance – positive fluid balance has been associated with mortality26 – these data indicate that the presence or absence of documentation itself does not prevent or cause AKI.
Early identification of acutely unwell patients
Biomarkers
Generally speaking, patients in this sample were referred when their biomarkers were most abnormal. However, there was a subgroup of patients who showed deranged potassium and bicarbonate readings prior to referral. The explanation for this lies with the creatinine-based definition of AKI. Pharmacokinetic studies show that following a simulated drop in creatinine clearance, there is a delay of up to 72 h before readings satisfied the RIFLE criteria for AKI.27 This effect is especially shown in patients with pre-existing CKD.27 This explains why a group of patients showing aberrant acid–base homeostasis indicative of AKI can have a ‘normal’ creatinine for several days, leading to later referral. Equally, patients promptly identified as having AKI may not show peak SCr readings until after referral. This emphasises the importance of clinical judgement in diagnosing AKI, rather than relying on SCr results or hence AKI staging which may not be the most responsive indicator of renal function. It also indicates that potassium and bicarbonate could be more sensitive to disruptions in renal function and play a pivotal role in early recognition of patients with AKI.
NEWS and stage of AKI
Overall, 45% (9/20) patients who developed Stage 3 AKI did so before referral based on NEWS, almost all of whom suffered poor outcomes. Furthermore, the latest iteration of NEWS excludes urine output measurements, even though oliguria is a key component in the definition of AKI.19 The NEWS was also a poor predictor of mortality in this study, suggesting that NEWS has little role in the escalation of the patient with AKI.
Limitations
This was single-centre study on a heterogeneous, complex group of patients including those with malignancy, neutropenia and transplant recipients. Whilst the cohort is likely to be representative of the patients referred to CCO at LTHT with AKI, the results of this study may not be generalizable to other centres. Furthermore, AKI care has been advancing at a rapid rate and the care received by this sample of patients may now be outdated, possibly further reducing the generalizability of this study’s findings. The findings of this study are not generalizable to patients with Stage 4 or 5 CKD; these patients were excluded as acute-on-chronic renal impairment is a distinct clinical entity. It was felt given the limited sample size, to limit the scope of the study to patients without existing advanced renal impairment, so as not to confound the data and limit the validity of the results. The reliability of this study’s findings may be limited by the relatively small sample size. Finally, reliability may have been further reduced to missing data. In particular, some serum bicarbonate values were missing. It is likely that these, and other blood results, may have been taken from blood gases, and hence were unavailable on the electronic health record.
Pivotally, in such a complex group of patients there may have been a number whose ceiling of care had been predefined or who had been deemed not for resuscitation. The authors did not have access to this information, although this may – along with the exclusion of Stage 4/5 CKD – explain the low dialysis rate (6%).
Conclusion and future prospects
Acute kidney injury has high levels of both in-hospital and long-term mortality and requires appropriate follow up given the large proportion of survivors left with CKD. This may be facilitated by the LTHT AKI Care Bundle, which has been designed to incorporate AKI information into the electronic discharge summary, allowing GPs to follow up patients with AKI. In addition to this, a specialist AKI clinic could ensure that these patients receive the long-term specialised support they need. This could have positive public health implications in that it may prevent readmissions, reducing the overall demand on healthcare resources and lowering morbidity and mortality.
NEWS was found to not be significantly associated with mortality. Furthermore, a subset of patients fulfilled the criteria for Stage 3 AKI prior to referral based on the NEWS. This study supports the introduction of Stage 3 AKI as a stand-alone trigger for CCO review recently introduced in LTHT. Previous AKI was found to be significantly associated with mortality. Future data should be collected using a larger, more up-to-date sample of patients seen by CCO following the introduction of the AKI Care Bundle and automatic Stage 3 AKI referrals. Comparison of the newly collected sample with the patients used in this study would provide robust validation for LTHT’s current policies.
Potassium and bicarbonate were shown to be more responsive markers in AKI than SCr and NEWS. This has important implications: education of foundation year doctors who deal with AKI regularly could lead to more prompt escalation of these patients and involvement of appropriate expertise. Inclusion of bicarbonate testing as standard for U&E results could allow identification of acid–base disturbance where it otherwise would not be tested. A new automated data mining project in LTHT28,29 aims to look at biomarkers in AKI in more detail and on a larger scale.
Declaration of conflicting interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1.Royal College of Physicians. National Early Warning Score (NEWS) – Standardising the assessment of acute-illness severity in the NHS, https://www.rcplondon.ac.uk/projects/outputs/national-early-warning-score-news (2012, accessed 17 September 2016).
- 2.Smith G, Prytherch D, Meredith P, et al. The ability of the National Early Warning Score (NEWS) to discriminate patients at risk of early cardiac arrest, unanticipated intensive care unit admission, and death. Resuscitation 2013; 84: 465–470. [DOI] [PubMed] [Google Scholar]
- 3.National confidential enquiry into patient outcomes and deaths: adding insult to injury, http://www.ncepod.org.uk/2009aki.html (2009, accessed 17 September 2016).
- 4.Lewington A and Kanagasundaram S. Acute kidney injury. Hampshire, UK: The Renal Association, http://www.renal.org/guidelines/modules/acute-kidney-injury#sthash.WDCO962z.7iDEZfhF.dpbs (2011, accessed 17 September 2016).
- 5.Ostermann M, Chang R. Acute kidney injury in the intensive care unit according to RIFLE. Crit Care Med 2007; 35: 1837–1843. [DOI] [PubMed] [Google Scholar]
- 6.Liano F, Junco E, Pascual J, et al. The spectrum of acute renal failure in the intensive care unit compared with that seen in other settings. The Madrid Acute Renal Failure Study Group, http://www.ncbi.nlm.nih.gov/pubmed/9580541 (2016, accessed 17 September 2016).
- 7.Cosentino F, Chaff C and Piedmonte M. Risk factors influencing survival in ICU acute renal failure, http://www.ncbi.nlm.nih.gov/pubmed/7800254 (2016, accessed 17 September 2016).
- 8.Bagshaw S, George C, Bellomo R. Changes in the incidence and outcome for early acute kidney injury in a cohort of Australian intensive care units. Crit Care 2007; 11: R68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gammelager H, Christiansen C, Johansen M, et al. Five-year risk of end-stage renal disease among intensive care patients surviving dialysis-requiring acute kidney injury: a nationwide cohort study. Crit Care 2013; 17: R145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kolhe N, Stevens P, Crowe A, et al. Case mix, outcome and activity for patients with severe acute kidney injury during the first 24 hours after admission to an adult, general critical care unit: application of predictive models from a secondary analysis of the ICNARC Case Mix Programme Database. Crit Care 2008; 12: S2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Clec’h C, Gonzalez F, Lautrette A, et al. Multiple-center evaluation of mortality associated with acute kidney injury in critically ill patients: a competing risks analysis. Crit Care 2011; 15: R128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hoste E, Clermont G, Kersten A, et al. RIFLE criteria for acute kidney injury are associated with hospital mortality in critically ill patients: a cohort analysis. Crit Care 2006; 10: R73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mandelbaum T, Scott D, Lee J, et al. Outcome of critically ill patients with acute kidney injury using the Acute Kidney Injury Network criteria. Crit Care Med 2011; 39: 2659–2664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Park W, Hwang E, Jang M, et al. The risk factors and outcome of acute kidney injury in the intensive care units. Korean J Intern Med 2010; 25: 181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Perinel S, Vincent F, Lautrette A, et al. Transient and persistent acute kidney injury and the risk of hospital mortality in critically ill patients. Crit Care Med 2015; 43: e269–e275. [DOI] [PubMed] [Google Scholar]
- 16.Samimagham HR, Kheirkhah S, Haghighi A, et al. Acute kidney injury in intensive care unit: incidence, risk factors and mortality rate. Saudi J Kidney Dis Transpl 2011; 22: 464–470. [PubMed] [Google Scholar]
- 17.Schiffl H, Lang SM, Fischer R. Long-term outcomes of survivors of ICU acute kidney injury requiring renal replacement therapy: a 10-year prospective cohort study. Clin Kidney J 2012; 5: 297–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nisula S, Kaukonen KM, Vaara ST, et al. Incidence, risk factors and 90-day mortality of patients with acute kidney injury in Finnish intensive care units: the FINNAKI study.[Erratum appears in Intens Care Med 2013; 39: 798]. Intens Care Med 2013; 39: 420–428. [DOI] [PubMed] [Google Scholar]
- 19.Kellum JA, Lameire N, Aspelin P, et al. KDIGO clinical practice guideline for acute kidney injury. Kidney Int Suppl 2012; 2: 1–138. [Google Scholar]
- 20.Leeds Teaching Hospitals NHS Trust Pathology Department, http://www.pathology.leedsth.nhs.uk/Pathology (2014, accessed 16 December 2016).
- 21.Royal College of Physicians. Acute care toolkit 12: acute kidney injury and intravenous fluid therapy, pp.1–8, https://www.rcplondon.ac.uk/guidelines-policy/acute-care-toolkit-12-acute-kidney-injury-and-intravenous-fluid-therapy (2015, accessed 16 December 2016).
- 22.Lopes JA, et al. Long-term risk of mortality after acute kidney injury in patients with sepsis: a contemporary analysis. BMC Nephrol 2010; 11: 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Uchino S, et al. Acute renal failure in critically Ill patients: a multinational, multicentre study. JAMA 2005; 294: 813–818. [DOI] [PubMed] [Google Scholar]
- 24.Zarjou A, Agarwal A. Sepsis and acute kidney injury. J Am Soc Nephrol 2011; 22: 999–1006. [DOI] [PubMed] [Google Scholar]
- 25.Redhead H (unpublished, dissertation) Does a rise in a patient’s serum creatinine occur prior to a rise in their National Early Warning Score (NEWS)? Leeds: University of Leeds, School of Healthcare, 2015.
- 26.Teixeira C, Garzotto F, Piccinni P, et al. Fluid balance and urine volume are independent predictors of mortality in acute kidney injury. Crit Care 2013; 17: R14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Waikar SS, Bonventre JV. Creatinine kinetics and the definition of acute kidney injury. J Am Soc Nephrol 2009; 20: 672–679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Hall P, et al. (unpublished). The future of diagnostic tests of acute kidney injury in critical care: evidence synthesis, care pathway analysis and research prioritisation. Leeds: University of Leeds. Expected publication January 2017. NIHR summary: http://www.nets.nihr.ac.uk/projects/hta/1311613. [DOI] [PMC free article] [PubMed]
- 29.West Yorkshire AKI Network, http://www.aki.org.uk (2013, accessed 16 December 2016).