Abstract
Background
Epstein–Barr virus (EBV) has been found to cause infectious mononucleosis multiple times, but has been associated rarely with EBV encephalitis. Also, whenever it is diagnosed, it is always treated symptomatically.
Case report
A case of confirmed EBV encephalitis is presented, which was treated with antiviral therapy resulting in complete clearance of the virus in cerebrospinal fluid and minimal neurologic symptoms after hospital discharge.
Conclusion
The Infectious Diseases Society of America guidelines state that intravenous acyclovir is not recommended for EBV-related encephalitis. But we reviewed the literature and found similar cases, and we believe that antiviral therapy should be recommended for EBV encephalitis because it is a potentially fatal disease and if left untreated, can lead to raised intracranial pressure, craniotomy and even death.
Keywords: Epstein–Barr virus, intravenous, human immune deficiency virus, HIV
Background
Epstein–Barr virus (EBV) has been usually found to be associated with infectious mononucleosis, but it can also cause encephalitis for which infectious disease guidelines do not recommend any treatment. Herein, we are presenting a case where symptomatic treatment was not sufficient and the patient had multiple neurologic symptoms that required acyclovir for the resolution of symptoms.
Case presentation
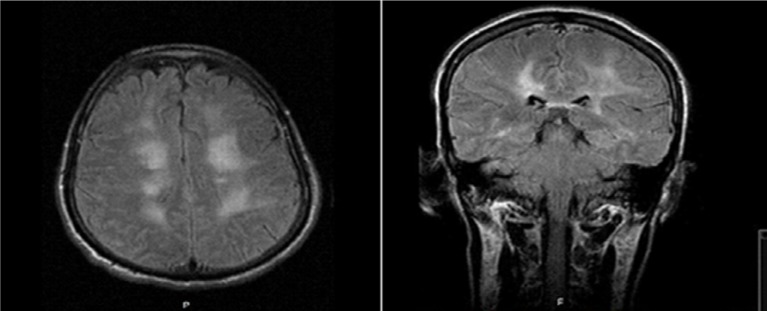
A 44-year-old Hispanic male was brought in with the chief complaints of progressive neurologic deterioration such as paranoid behavior, complete loss of memory, generalized weakness, and urine incontinence for 2 months. The patient was an active smoker, a heavy drinker, an intravenous drug abuser, and was sexually active. He used to work in a restaurant 2 months ago with completely normal mental status. His physical examination showed low-grade fevers and gait ataxia; his level of consciousness was always proper, but the content was altered. Laboratory testing showed he was human immunodeficiency virus (HIV) positive (CD4 count- 348 cells/mm3) with normal complete blood count (white blood cell count 5.4 M/μL, hemoglobin 12 g/dL, and platelet count 176×109/L). His kidney function was persistently normal; urinalysis was normal as well. Lumbar puncture was done and cerebrospinal fluid showed normal white blood cell count with normal glucose and protein levels. The entire HIV-related opportunistic infections including herpes simplex, cytomegalovirus, toxoplasma, tuberculosis, progressive multifocal leukoencephalopathy, and John Cunningham virus were negative, except EBV, which was followed as shown in Table 1. Imaging studies including magnetic resonance imaging and computed tomography scans were performed, which showed lucencies at different levels of brain and around the ventricles (Figure 1).
Table 1.
EBV-PCR results of cerebrospinal fluid on admission and follow up
| Before treatment | After treatment | |
|---|---|---|
| 1 month | 2269 copies/mL | 1635 copies/mL |
| 3 months | 485 copies/mL | |
| 6 months | <200 copies/mL | |
| Immune status | HIV positive | CD4 count 348 cells/mm3 |
Abbreviations: EBV, Epstein–Barr virus; HIV, human immune deficiency virus; PCR, polymerase chain reaction.
Figure 1.
CT scan of brain at two different levels, both show white lucencies in the white matter and around ventricles.
Abbreviation: CT, computed tomography.
This patient was started on antiviral therapy acyclovir 10 mg/kg and his symptoms started resolving day by day. Patient was followed in infectious disease clinic and after 6 months, he was again completely functional.
Consent
Written informed consent has been provided by the patient to have his case details and any accompanying images published.
Discussion
EBV and all other herpes viruses are gamma viruses and are present in >90% of the population. The virus can affect both T and B lymphocytes, but B lymphocytes are the major cellular reservoirs. The virus mainly replicates in the pharynx, nasopharynx, salivary glands, glandular epithelium of the thyroid gland, and stomach.
The pathogenesis of EBV-associated neurologic manifestations is not known clearly. Some studies show that immunotoxicity can be caused by infiltration of CD8+ cells into neural tissue. Alternatively, deposition of antigen–antibody complexes is considered as a cause of endothelial changes leading to tissue damage. Meningitis and encephalitis are the most common neurologic manifestations even with chronic infectious mononucleosis.1 A recent literature review has shown that 70% of infected patients with neurologic symptoms recovered completely, 20% lived with sequelae, and 10% died.
There is no significant research showing association of EBV encephalitis and HIV or any other immunocompromised status such as transplant or carcinoma patients.2,3 Usually, opportunistic infections are seen in HIV patients when their CD4 count is <200, but EBV has not been documented as one of those opportunistic infections. More research is needed to study the association between HIV, EBV, and CD4 count.
Few cases of EBV encephalitis have been reported in HIV-positive patients and antiviral therapy has been used in all those cases irrespective of their CD4 counts.2,4,5
The effectiveness of antiviral therapy in this case was proved by the decreasing number of viral DNA and improvement in neurologic symptoms. Though the patient was receiving symptomatic treatment for almost 2 months at home, he was worsening day by day to the point of becoming delirious, forgetful, and having ataxia with urine incontinence. He was a fully working person, but after 2 months, he was totally dependent on others, which proved that symptomatic treatment alone was not enough. Similarly, there are more case reports and scholarly activities in which mere symptomatic therapy was not sufficient.1–7 Table 2 shows a few more examples and a literature review of successful treatment of EBV encephalitis with antiviral therapy.
Table 2.
Literature review and analysis after antiviral therapy use
| Year | No. of cases diagnosed | Sequelae after antiviral therapy use | Deaths |
|---|---|---|---|
| 20144 | 1 | Excellent | None |
| 20132,6 | 2 | Excellent | None |
| 20128 | 2 | Excellent | None |
| 20117 | 1 | Excellent | None |
| 20105 | 1 | Not good | Craniotomy and death |
| 20099 | 1 | Excellent | None |
| 2000–2009 Helsinki study3 | 13 | Good | None |
| 1984–2002 Kurume university study1 | 4 | Good | None |
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Fujimoto H, Asaoka K, Imaizumi T, Ayabe M, Shoji H, Kaji M. Epstein-Barr virus infections of the central nervous system. Intern Med. 2003;42(1):33–40. doi: 10.2169/internalmedicine.42.33. [DOI] [PubMed] [Google Scholar]
- 2.Trevillyan JM, Mahony AA, McLean C, Hoy JF. Successful treatment of Epstein-Barr virus encephalitis in the setting of HIV-associated neurocognitive disorder: a diagnostic and therapeutic challenge. Antivir Ther. 2013;18(2):257–261. doi: 10.3851/IMP2451. [DOI] [PubMed] [Google Scholar]
- 3.Martelius T, Lappalainen M, Palomäki M, Anttila VJ. Clinical characteristics of patients with Epstein-Barr virus in cerebrospinal fluid. BMC Infect Dis. 2011;11:281. doi: 10.1186/1471-2334-11-281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Raman L, Nelson M. Cerebral vasculitis and encephalitis due to Epstein–Barr virus in a patient with newly diagnosed HIV infection. J Clin Virol. 2014;59(4):264–267. doi: 10.1016/j.jcv.2014.01.018. [DOI] [PubMed] [Google Scholar]
- 5.Polilli E, Sozio F, Mazzotta E, et al. Rapidly progressive and fatal EBV-related encephalitis in a patient with advanced HIV-1 infection at presentation: a case report and review of the literature. New Microbiol. 2010;33(3):275–280. [PubMed] [Google Scholar]
- 6.Akkoc G, Kadayifci EK, Karaaslan A, et al. Epstein-Barr virus encephalitis in an immunocompetent child: a case report and management of Epstein-Barr virus encephalitis. Case Rep Infect Dis. 2016;2016:7549252. doi: 10.1155/2016/7549252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Di Carlo P, Trizzino M, Titone L, et al. Unusual MRI findings in an immunocompetent patient with EBV encephalitis: a case report. BMC Med Imaging. 2011;11:6. doi: 10.1186/1471-2342-11-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yang X, Wada T, Imadome K, et al. Characterization of Epstein-Barr virus (EBV)-infected cells in EBV-associated hemophagocytic lymphohistiocytosis in two patients with X-linked lymphoproliferative syndrome type 1 and type 2. Herpesviridae. 2012;3(1):1. doi: 10.1186/2042-4280-3-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Abul-Kasim K, Palm L, Maly P, Sundgren PC. The Neuroanatomic Localization of Epstein-Barr Virus Encephalitis May be a Predictive Factor for its Clinical Outcome: A Case Report and Review of 100 Cases in 28 Reports. J Child Neurol. 2009;24(6):720–726. doi: 10.1177/0883073808327842. [DOI] [PubMed] [Google Scholar]