Abstract
Background
Leptospirosis is a bacterial zoonotic disease with worldwide distribution.
Case presentation
We describe and discuss the clinical course of a leptospirosis outbreak in a running club called the hash house harriers on Guam.
Conclusions
Leptospirosis is a potentialy life threatening disease, and has had a reemergence given the popularity of travel adventure sports, teams, and clubs around the world. This case presentation highlights the robust prescence of leptospirosis on Guam.
Keywords: Infectious disease, Leptospirosis, Travel medicine
Background
Leptospirosis is a bacterial zoonotic disease with worldwide distribution and is an important emerging infectious disease [1, 2]. Many wild and domestic animals serve as reservoirs for pathogenic Leptospira strains and contaminate the environment by shedding the organisms in their urine. Humans are usually infected through abraded skin or mucous membrane contact with water contaminated by this urine [3, 4]. Athletes, military personnel or others exposed to contaminated water are at risk of contracting leptospirosis. Herein, we report an outbreak of leptospirosis that occurred on the island of Guam, and discuss implications for travelers to tropical regions who may have water exposures.
Case Presentation
A 24 year old male service member currently stationed on Guam presented with 3 days of subjective fever, headache, myalgias (specifically lower back), severe fatigue, and insomnia that worsened throughout the day. In addition, he noted drenching night sweats and anorexia associated with variable weight loss. He did not report diarrhea, abdominal pain or vomiting. He denied any rashes. He had no ill contacts at the time of initial presentation, and denied recent travel, insect bites, consumption of unusual foods or unpasteurized milk products. He had been immunized against hepatitis A and B, typhoid, influenza, and took no routine medications.
One day after this patient presented, three other patients presented with almost identical symptoms specifically complaining of the headache, extreme fatigue and lower back pain. By day three, four additional patients had presented; two to the clinic, and two to the local ER - Fig. 1, epidemic curve.
Fig. 1.
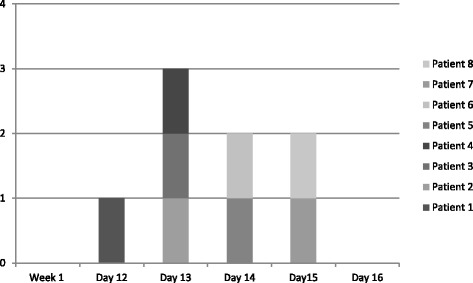
Cases of Leptospirosis by date of onset, Guam
All patients denied recent travel, sick contacts or consumption of unpasteurized or raw food. A point source outbreak was suspected because of the epidemic curve. The cluster of cases presented approximately 2 weeks after a particular water exposure during a hash running event on the south side of Guam where 20 or so hikers had gotten lost and spent the night in the jungle. They noted multiple exposures to wet river banks, mud, and swamps.
On exam, all the patients were ill appearing with most prostrate on the examination table. The majority of their exams were normal, with no hepatosplenomegaly, rashes or conjunctival injection noted. Most patients did have abrasions along either the upper arms, or lower legs. All patients demonstrated a temperatures ranging from 101.2–103 F and all were tachycardia.
The majority of laboratory testing was normal, with the exception of slightly elevated serum creatinine and one patient with elevated liver enzymes and creatinine kinase levels. See Table 1.
Table 1.
Lab results at presentation
| Case | Age | Sex | WBC (x103McL) | H/H | Platelets (x103McL) | Creatinine (mg/dL) | AST/ALT (U/L) | Sodium (mmol/L) | Chloride (mmol/L) | Bilirubin (mg/dL) | CK MB(U/L) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 25 | M | 4.9 | 13.8/40.8 | 139 | 1.6 | 37/29 | 134 | 97 | 1.22 | 8.0 |
| 2 | 24 | F | 7.0 | 14/41.1 | 141 | 1.0 | 34/26 | 131 | 94 | 0.38 | – |
| 3 | 21 | F | 3.4 | 12.4/36.5 | 103 | 1.3 | 45/44 | 135 | 100 | 0.46 | – |
| 4 | 31 | M | 9.4 | 14.8/43.1 | 145 | 1.2 | 40/26 | 130 | 94 | 0.60 | – |
| 5 | 21 | M | 8.5 | 14.7/42.4 | 155 | 1.3 | 203/890 | 135 | 95 | 0.84 | 756.0 |
| 6 | 26 | M | 5.37 | 14.8/43.0 | 235 | 1.3 | 28/26 | 139 | 98 | 1.6 | – |
| 7 | 22 | M | 4.2 | 14.0/41.0 | 153 | 1.4 | 29/26 | 131 | 94 | 1.2 | 7.0 |
| 8 | 34 | M | 4.7 | 13.9/40.0 | 123 | 1.2 | 37/39 | 139 | 93 | 0.5 | – |
Microbiologic testing included negative blood culture and multiple serologic studies, the results of which are shown in Table 2. Of note, all patients demonstrated a seroconversion to leptospirosis on convalescent blood samples. Clinical course: All patients responded well to treatment with intravenous normal saline and antiemetics. All were empirically treated with doxycycline 100 mg twice daily and their symptoms resolved over the course of 3 to 4 days. Anorexia continued well into the third day of treatment with antibiotics, with most reporting weight loss between 5 and 15 lb.
Table 2.
Serologic testing *R: Reactive, NR: Non-reactive, E: Equivocal
| Case | Age | Sex | Initial Leptospira IgM | Leptospira IgM (30 days after initial) | EBV/CMV IgM/IgG | Rickettsia panel IgM/IgG(rickettsia rickettsia, Rickettsia typhi) | Dengue IgM/IgG | Hepatitis A IgM | Rapid Flu |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 25 | M | NR | R | NR | NR | NR | NR | NR |
| 2 | 24 | F | NR | R | NR | NR | E | NR | NR |
| 3 | 21 | F | NR | R | NR | NR | NR | NR | NR |
| 4 | 31 | M | NR | R | NR | NR | NR | NR | NR |
| 5 | 21 | M | NR | R | NR | E | NR | NR | NR |
| 6 | 26 | M | NR | R | NR | NR | NR | NR | NR |
| 7 | 22 | M | NR | R | NR | NR | NR | NR | NR |
| 8 | 34 | M | NR | R | NR | NR | NR | NR | NR |
Discussion
All patients presented with a clinical syndrome consistent with a broad range of tropical illnesses, see Table 3. Leptospirosis was considered because of the common source of exposure of prolonged contact with contaminated ground water with multiple exposures to rivers, and muddy trails after spending an evening in the southern jungles of Guam near Mount Lam Lam. The initial labs were negative for leptospirosis, but convalescent titers revealed 100% had seroconverted. Due to the remote location of the health care facility, confirmatory microagglutination testing (MAT) was not able to be completed.
Table 3.
Differential Diagnosis
| Dengue | |
| Chikungunya | |
| Enterovirus | |
| Hantavirus | |
| Hepatitis A | |
| Rickettsial infection | |
| Brucellosis | |
| Malaria | |
| Meningitis | |
| Q Fever | |
| Rickettsial infection | |
| Viral hemorrhagic fever | |
| Measles | |
| Rubella | |
| Mononucleosis |
Epidemiologically, it is of interest to note a progressive number of outbreaks associated with the increasingly popular sports of international adventuring racing. A 2000 Eco-Challenge in Borneo reports that at least 25% of the participants developed leptospirosis after returning home. Additional outbreaks of leptospirosis have also been investigated in a Triathlon in Springfield, Illinois in 1998, a multisport race in Florida, an endurance jungle race in Martinique, and a triathlon in Langau, Austria, with 15, 12, 9, and 4 confirmed cases respectively [5–9]. Ecotourism, and the popularity of such jungle athletic racing groups and clubs like hashing risk exposing participants to a wide range of pathogens, some of which are only tropical, but also includes pathogens such as leptospirosis, and rickettsia with worldwide distributions. This reinforces the importance of asking a travel history in every patient with a fever, and always practicing engaged preventative medicine by keeping travelers and athletes aware of these bacteria, viruses, and the risks of transmission, and educated about the appropriate barrier, and chemoprophylaxis.
Several studies suggest that doxycycline can be used either as a chemoprophylaxis or as a post exposure prophylaxis and empiric treatment, however the evidence of effectivenss is limited. [10–12]. A study of U.S. Army soldiers participating in a training exercise in Panama, found efficacy of doxycycline administered 200 mg once daily [13]. This case particularly demonstrates that active duty military personnel who travel extensively for their careers, and recreation, also frequently participate in field exercises and tend to be drawn to the active competitive adventure races which can expose them, and heavily impact military readiness encouraging an astute clinician to also always inquire about occupational status.
Cultural context (text box)
Hash House Harriers is a proverbial “drinking club with a running problem” with organized chapters throughout the world [14]. On weekends, the local chapter on Guam frequently explored the jungle with runs over 4–6 miles of remote terrain including rivers, waterfalls, lakes, and muddy swamps.
The chammorrians (the locals) blamed this outbreak on the tutamo’nas. (people before recorded time), the ghostly apparitions of the ancient people of Guam. The taotaomo’nas of Guahan are said to roam the jungles and are present around the ancient latte ruins, large basalt and coral boulders and caves, as well as amongst the thick dense hanging roots of the Banyan Trees. Legend has it that if one enter the jungles and disturbs the taotaomo’nas, particularly around sunset, they may pinch you, leaving red marks or swellings on your body, or they may cause illnesses which are difficult to diagnose by conventional doctors, such as leptospirosis. [13, 15]
Conclusions
Leptospirosis is important reemerging tropical disease, especially in an area with an extensive military population. It highlights the existence of the disease on the island of Guam, and also demonstrates the developing association of leptospirosis case outbreaks among world traveling adventure racers in sports such as hashing. This manuscript is important for epidemiological reasons and to discourse the risk factors, and the clinical signs and symptoms of leptospirosis in Guam.
Acknowledgments
Not applicable.
Funding
No sources of funding were received for this project. DB and I have no funding bodies to declare. The design of the study and collection, analysis, and interpretation of data were independently done per myself and DB.
Availability of data and materials
Date sharing not applicable to this article as no datasets were generated or analysed during the current study.
Authors’ contributions
AB initially saw the patient’s in clinic as the PCM and followed up with the patient’s.She mined the data and drafted the manuscript. DB edited the manuscript through multiple rewrites and helped edit the Tables and Figures. AB conceived of the study. Both authors participated in the design, coordination, and helped to draft, edit, and rewrite the manuscript. All authors read and approved the final manuscript. Out the molecular genetic studies, participated in the sequence alignment and drafted the manuscript.
Ethics approval and consent to participate
The Naval Hospital San Diego ethics committee (acting IRB chair Dr. Shelton Viola) reviewed this retrospective case study involving human subjects, human material, and human data and feel ‘This is an educational activity discussing the course of a group of patients. There is no systematic investigation here (no group comparisons, no scientific question, etc.) and therefore consider this a non-research educational activity, not subject to any IRB scrutiny. The work is exempt research as involving an infectious disease outbreak and being reported as a prevention warning for public health purposes.’
Further information and documentation to support review can be made available to the Editor on request.
Consent for publication
This study has been granted an exemption from requiring ethics approval/determined that the requirement for consent to participate can be waived by the Naval Hospital San Diego ethics committee. Not applicable.
Competing interests
The author declares that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Alyson J. Brinker, Email: brinker.alyson@gmail.com
David L. Blazes, Email: da_blazes@hotmail.com
References
- 1.Bharti AR, Nally JE, Ricaldi JN, Matthias MA, Diaz MM, Lovett MA, Levett PN, Gilman RH, Willig MR, Gotuzzo E, Vinetz JM. Leptospirosis: a zoonotic disease of global importance. Lancet Infect Dis. 2003;3:757–771. doi: 10.1016/S1473-3099(03)00830-2. [DOI] [PubMed] [Google Scholar]
- 2.Palaniappan RU, Ramanujam S, Chang YF. Leptospirosis: pathogenesis, immunity, and diagnosis. Curr Opin Infect Dis. 2007;20(3):284–292. doi: 10.1097/QCO.0b013e32814a5729. [DOI] [PubMed] [Google Scholar]
- 3.Leptospirosis. Levett PN. Clin Microbiol Rev. 2001; 14(2):296–326. [DOI] [PMC free article] [PubMed]
- 4.SMITH DJ, SELF HR. Observations on the survival of Leptospira australis A in soil and water. J Hyg (Lond) 1955;53(4):436–444. doi: 10.1017/S0022172400000942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.CDC From the Centers for Disease Control and Prevention. Update: outbreak of acute febrile illness among athletes participating in Eco-Challenge-Sabah 2000--Borneo, Malaysia, 2000. JAMA. 2001;285(6):728–730. [PubMed] [Google Scholar]
- 6.CDC Update: leptospirosis and unexplained acute febrile illness among athletes participating in triathlons--Illinois and Wisconsin, 1998. MMWR Morb Mortal Wkly Rep. 1998;47(32):673–676. [PubMed] [Google Scholar]
- 7.CDC Outbreak of leptospirosis among white-water rafters--Costa Rica, 1996. MMWR Morb Mortal Wkly Rep. 1997;46(25):577–579. [PubMed] [Google Scholar]
- 8.Radl C, Müller M, Revilla-Fernandez S, Karner-Zuser S, de Martin A, Schauer U, et al. Outbreak of leptospirosis among triathlon participants in Langau, Austria, 2010. Wien Klin Wochenschr. 2011;123(23–24):751–755. doi: 10.1007/s00508-011-0100-2. [DOI] [PubMed] [Google Scholar]
- 9.Hochedez P, et al. Outbreak of Leptospirosis after a Race in the Tropical Forest of Martinique. The American Journal of Tropical Medicine and Hygiene. 2016;84.4(2011):621–626. doi: 10.4269/ajtmh.2011.10-0502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Takafuji ET, Kirkpatrick JW, Miller RN, Karwacki JJ, Kelley PW, Gray MR, et al. An efficacy trial of doxycycline chemoprophylaxis against leptospirosis. N Engl J Med. 1984;310(8):497–500. doi: 10.1056/NEJM198402233100805. [DOI] [PubMed] [Google Scholar]
- 11.Guidugli F, Castro AA, Atallah AN. Antibiotics for preventing leptospirosis. Cochrane Database Syst Rev. 2000:CD001305. [DOI] [PubMed]
- 12.Brett-Major DM, Lipnick RJ. Antibiotic prophylaxis for leptospirosis. Cochrane Database Syst Rev. 2009;(3):CD007342. doi:10.1002/14651858.CD007342.pub2. [DOI] [PubMed]
- 13.Flood B. Marianas Island Legends, Myth and Magic. Hawai’i: The Bess Press; 2001. [Google Scholar]
- 14.Sekula S. A drinker's guide to running the world. CNN International. Retrieved 31 May 2013
- 15.Mitchell R. Ancestral Spirits and Hitchhiking Ghosts: Syncretism on Guam. Midwestern Journal of Language and Folklore. 1976;2(2):45–55. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Date sharing not applicable to this article as no datasets were generated or analysed during the current study.


