Abstract
To assess the long-term effectiveness of antipsychotic medications in facilitating work functioning in patients with schizophrenia we conducted longitudinal multi followup research on 139 initially psychotic patients. The 70 patients with schizophrenia and 69 initially psychotic mood disordered control patients were followed up 6 times over 20 years. We compared the influence on work functioning of patients with schizophrenia continuously prescribed antipsychotics with patients with schizophrenia not prescribed antipsychotics, using statistical controls for inter-subject differences. While antipsychotics reduce or eliminate flagrant psychosis for most patients with schizophrenia at acute hospitalizations, four years later and continually until the 20 year followups, patients with schizophrenia not prescribed antipsychotics had significantly better work functioning. The work performance of the patients who were continuously prescribed antipsychotics was at a low rate and did not improve over time. Multiple other factors also interfere with work functioning. The data suggest that some patients with schizophrenia not prescribed antipsychotics for prolonged periods can function relatively well. Multiple other factors are associated with poor post-hospital work performance. The longitudinal data raise questions about prolonged treatment of schizophrenia with antipsychotic medications.
Keywords: Employment, Psychosis, Outcome, Treatment, Negative Symptoms
1. Introduction
Work functioning and factors related to work functioning in patients with schizophrenia have long been important in regard to outcome for these patients. This includes psychosocial functioning and the economic impact to the country through job loss by patients with schizophrenia (Rosenheck et al., 2006). Programs to enhance social rehabilitation, and facilitate work functioning for patients with schizophrenia have increased in number and in sophistication (Bond et al., 2012; McGurk et al., 2013; McGorry et al., 2013; Mueser et al., 2013).
A major factor is psychopharmacological treatment with the belief that antipsychotic medications may facilitate work functioning for some or many patients with schizophrenia (Tandon et al., 2008; Alonso et al., 2009). However, until recently, the research on antipsychotic medications and work functioning have almost all been based on short-term (under 3-years) studies.
Research on the efficacy of antipsychotics administered to acute schizophrenia with flagrant psychosis has provided data indicating that antipsychotics, during the early most acute phase, are very effective in reducing severity of psychosis of many patients with schizophrenia (Gilbert et al., 1995; Buchanan et al., 2010), although other approaches also have some effectiveness (Ciompi and Hoffmann, 2004; Bola et al., 2009; Seikkula et al., 2011). In addition, there are a very large number of double-blind studies showing that during the first year and a half patients on placebo have a relatively high rate of relapse. However, several major studies, including the double-blind 2-year, Northwich Park Study by Johnstone, Mcmillan, Frith, Benn and Crow (Johnstone et al., 1990) found better work functioning in unmedicated psychotic patients.
The long-term evidence on the effects of antipsychotics beyond the first 3 years of administration is relatively sparse (Barnes and Badre, 2016). A comprehensive meta-analysis by Leucht, Davis and colleagues, noted that “the meta-regression suggested that antipsychotic drugs might lose their effectiveness with time” (Leucht et al., 2012b). They also noted that studies beyond 3-years would be important to the field, observing that “nothing is known about the effects of antipsychotic drugs compared to placebo after 3 years (Leucht et al., 2012a).
Recent longitudinal research has provided evidence of improvement in psychosis and in recovery for some or many unmedicated patients with schizophrenia as one moves past the 2-year period. This long term research on antipsychotic medication treatment includes that of Wunderink (Wunderink et al., 2013), the Northern Finland Birth Cohort Studies (Moilanen et al., 2013), the Danish OPUS trials (Wils et al., 2016) the study of Jung, Lincoln and colleagues (Jung et al., 2016) and our longitudinal research from the Chicago Followup Study (Harrow and Jobe, 2007; Jobe and Harrow, 2010; Harrow et al., 2012; Harrow and Jobe, 2013; Harrow et al., 2014). These and other studies have led to questions by R. Murray (Murray et al., 2016), by Barnes and Badre (2016) and others (Buchsbaum et al., 1992; Howes et al., 2012) concerning the long-term effects of antipsychotics on functioning.
The current longitudinal study directly measures work functioning over prolonged periods for a) patients with schizophrenia in long term antipsychotic treatment vs b) patients with schizophrenia not on antipsychotics, focusing on the long-term effects of antipsychotics on work functioning, using statistical controls and data on symptom level, and on premorbid achievements to control for inter-subject differences.
This study also examines whether the 2 major types of symptoms in schizophrenia, positive and negative symptoms, and whether major prognostic factors, influence work functioning. Previous research provide strong evidence concerning the importance of neurocognitive impairment in schizophrenia for poorer work functioning (Green, 1996; Green et al., 2000).
Since mood disordered patients who are psychotic at the acute phase (e.g., some bipolar patients and some psychotic MDD) are sometimes treated with antipsychotics, the long-term work functioning of these patients, used as a control group, also was assessed.
The following objectives were addressed:
To provide clues on whether long-term use of antipsychotics facilitates work functioning, or in contrast interferes with work functioning in schizophrenia and psychotic mood disorders.
To provide long-term data on whether negative symptoms and/or psychosis interfere with work functioning in schizophrenia.
To provide long-term data on whether patients with schizophrenia not in medication treatment can show effective work functioning.
To study whether long-term treatment of schizophrenia with antipsychotic medications improves their work functioning.
2. Method
The present research, derived from the Chicago Followup Study, involves a prospective, longitudinal multi-followup research program studying functioning, outcome, and recovery in major psychotic disorders (Harrow et al., 1990; Harrow et al., 2005; Harrow and Jobe, 2007; Jobe and Harrow, 2010; Harrow et al., 2012; Harrow and Jobe, 2013; Harrow et al., 2014). The 139 patients included 70 initially psychotic schizophrenia patients (61 patients with schizophrenia and 9 schizoaffective patients) and a control sample of 69 initially psychotic mood disordered patients (38 psychotic bipolar patients and 31 initially psychotic unipolar depressive patients).
At their initial assessment the 139 patients were in a relatively early phase of their disorders during an acute phase of hospitalization and were followed up on 5 or 6 subsequent occasions over a 20 year period. The followups occurred at 2 years, 4.5 years, 7.5 years, 10 years, 15 years and 20 years post-index hospitalization.
Within the limits of studying relatively young patients, the participants were consecutive admissions to two Chicago-area hospitals (a private hospital and a state hospital) and all but 3 were between the ages of 17 and 32 years of age (mean age = 22.9 years). Employing DSM III diagnosis, inter-rater reliability for diagnosis for the sample with schizophrenia was assessed (Kappa = 0.88). The Institutional review board (IRB) approved the research, and signed informed consent was obtained from all patients.
At index hospitalization, 41% of the patients were first admissions, and another 25% had only one previous hospitalization. The median level of education at index hospitalization was 13 years. Sixty percent of the patients with schizophrenia and 42% of the mood disordered patients were males. Using the Hollingshead-Redlich scale for socioeconomic status (Hollingshead and Redlich, 1958) (SES), 53% were from households with SES of 1 to 3 (higher socioeconomic status) and 47% were from households with SES of 4–5 (lower socioeconomic status based on parental SES).
All patients with schizophrenia selected for inclusion met the 6 month duration of illness criterion (none were schizophreni form patients). From among the 70 patients with schizophrenia, 58 were followed up at the 20-year period, with 30 schizophrenia patients assessed at all 6 followups. Another 32 were assessed at 5 of the 6 followup periods. Two patients with schizophrenia were assessed at 4 followups and 6 at less than 4 followups. The assessments were done by trained interviewers who were not informed of the results of the previous followups and not aware of any focus on the effectiveness of antipsychotics.
2.1 Antipsychotic medications
Table 1 reports the percentage of patients with schizophrenia in treatment at each of the 6 followup assessments.
Table 1.
PERCENT OF SCHIZOPHRENIA PATIENTS ON ANTIPSYCHOTIC MEDICATIONS AND PERCENT NOT IN TREATMENT
| Antipsychotics | In Treatment No Antipsychotics |
No Mental Health Treatment | |
|---|---|---|---|
| 2 Year FU | 67% (38) | 16% (9) | 18% (10) |
| 4.5 Year FU | 66% (43) | 14% (9) | 20% (13) |
| 7.5 Year FU | 63% (40) | 16% (10) | 22% (14) |
| 10 Year FU | 62% (38) | 13% (8) | 25% (15) |
| 15 Year FU | 66% (38) | 9% (5) | 26% (15) |
| 20 Year FU | 62% (36) | 14% (8) | 24% (14) |
At the 2-year assessment 67% of the patients were prescribed antipsychotics with, or without other medications, and at the subsequent 5 followups over 20 years between 62% and 67% of the patients with schizophrenia received antipsychotic prescriptions. In that this was a naturalistic study, there was no single uniform treatment plan for all patients. The sample included a number of patients who left treatment on their own, often against medical advice.
Twenty-five of the patients with schizophrenia were prescribed antipsychotic medications at every one of the followup assessments (group 1). Another 24 schizophrenia patients were prescribed antipsychotic medications at some but not all, of the followup years (group 2) and 15 of the patients with schizophrenia were not on antipsychotics at any one of the followup assessments (starting at the 2 year followups) over the 20 years (group 3). Six other patients with schizophrenia received a 20-year followup, but had fewer than four followup assessments where definitive data on work functioning was obtained. Their data on medications and work functioning were not included in comparisons of group 1 with group 3, but were included in comparisons of work functioning at those individual followups for which they had definitive data.
Other characteristics of the sample of schizophrenia patients are reported in Supplemental Table 1. The sample of 25 patients with schizophrenia always prescribed antipsychotics and the sample of 15 schizophrenia patients not prescribed antipsychotics from the 2 year followups onward allow long-term, multi-year, comparisons of patients with schizophrenia not on antipsychotics for many years with patients with schizophrenia continuously prescribed antipsychotics over a 20 year period. Longitudinal data on work functioning (greater than 3 years) have rarely been available to the field before (Wunderink et al., 2013).
2.2 Followup assessments
Patients were assessed with standardized research instruments at each followup for work functioning, positive symptoms, negative symptoms, re-hospitalization, periods of recovery, and antipsychotic drug treatment. The SADS (Schedule for Affective Disorders and Schizophrenia) (Endicott and Spitzer, 1978) was administered at each followup interview to assess potential delusions and hallucinations. At each interview the Behavior Rating Scale of the Psychiatric Assessment Interview (Carpenter et al., 1976) was scored by trained raters to assess negative symptoms (Herbener and Harrow, 2004).
2.3 Assessment of work functioning
Work and social functioning for the 139 patients was assessed using a structured interview (the Harrow Functioning Interview) (Herbener and Harrow, 2004). Both the SADS and the functioning interview were administered by trained interviewers blind to the patients’ diagnosis, with the interviews used successfully in a series of longitudinal studies. Examples of questions from the functioning interview on employment during the past year included “Are you employed at present?,” “What jobs have you had?,” “How long have you been unemployed?” These and similar questions were used to score the 5-point (scores of 0–4) S-C Scale (Strauss and Carpenter, 1972) on work functioning.
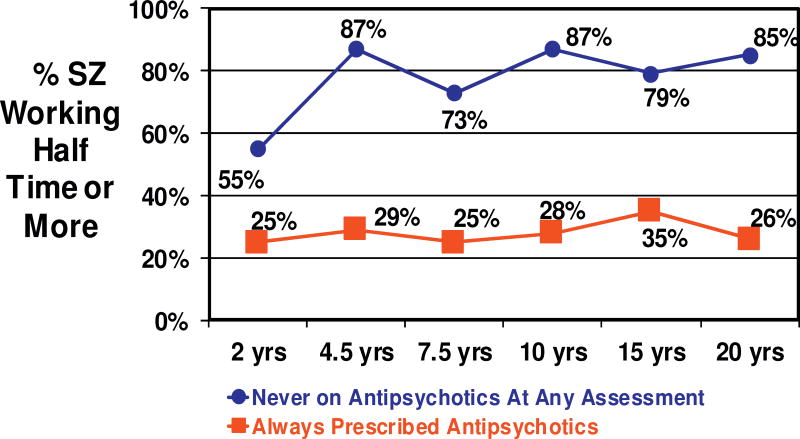
The 5-point scale for work adjustment was scored for each patient at each followup. The subsample of schizophrenia patients who were scored as working (a score of “2” for half-time work, or “3” or “4” for more than half-time work) were compared according to whether they had been prescribed antipsychotics (Figure 1).
FIGURE 1.
20 Year Longitudinal Assessment Of Work Functioning In Schizophrenia: Medicated And Unmedicated Patients
Patients who during the last year were working half time or more (paid work) were viewed as working. This included working half-time or more for the full year, and working full time for half a year or more.
Favorable scores for work were given to those taking care of children or other dependents (often, but not always, women). Patients who were responsible for the welfare of one or more children or other dependents (i.e., a relative needing a live-in caregiver) were scored as working. Patients who kept house only for themselves and/or a live-in partner were not scored as working. Additionally, students who attended school ½ time or more were scored as working.
2.5 Assessment of major prognostic factors (Vaillant, 1964; Vaillant, 1978; Westermeyer and Harrow, 1984; Zigler and Glick, 2001)
To control for key premorbid factors that might influence posthospital work adjustment and other posthospital functioning, we collected information on a series of important variables during index hospitalization, prior to the posthospital assessments. The first scale is from the studies of Vaillant (Vaillant, 1962; Vaillant, 1978) and Stephens (Westermeyer and Harrow, 1984; Stephens et al., 1997). It assesses the influence of prognostic characteristics related to later outcome for schizophrenia patients. These include the absence of acute onset, the absence of precipitating events, blunted affect, poor prehospital social adjustment, poor prehospital work adjustment, no confusion on hospital admission, no depression on hospital admission, and other major variables. The second scale from the research of Zigler (2001) evaluates the influence of premorbid developmental achievements, including prehospital work history, education, marital status and age at first break.
2.6 Major Comparisons and Potential Confounding Factors
The data from the 139 patients were used to assess how many were prescribed antipsychotic medications at each followup and how many of these patients were working at that followup.
The confounding factors we consider in the logistic regression are: Prognosis (0=good; 1=poor); Premorbid Functioning (0=good; 1=poor); Positive Symptoms (0=not has; 1=has); and Negative Symptoms (0=not has; 1=has). Due to longitudinal observation of data, the indicators Positive and Negative Symptoms can vary over time, while Prognosis and Premorbid Functioning are measured at baseline time and therefore are constant over time. We consider logistic and proportional odds regressions for two types of response variable: (1) logistic model is used when working function is recorded as a binary variable (1=not working; 2=working); (2) proportional odds model is used when working function is recorded as an ordered multi-categorical variable (0 to 4, higher score for better work performance). All the data obtained from all the follow-up points are used in both analysis. The generalized estimating equation (GEE) method (Liang and Zeger, 1986) is applied in both models to deal with the dependence caused by longitudinal observations over time.
The probabilities associated with all statistical tests reported are two-tailed.
3. Results
3.1 Work functioning: Patients with schizophrenia prescribed antipsychotic medications versus those not on antipsychotic medications
Figure 1 presents data on work adjustment for patients with schizophrenia continuously prescribed antipsychotic medications (group 1, n=25) and for those not on antipsychotic medications throughout the last 18 years (group 3, n=15).
Table 2 reports the detailed data on work functioning, presenting the chi-square and effect sizes-odds ratios at the 6 followups over 20 years for the patients with schizophrenia continually prescribed antipsychotics vs those schizophrenia patients not prescribed antipsychotics at any of the 6 followups. There are large significant differences and large effect sizes in work functioning in favor of the unmedicated schizophrenia patients over the last 18 years.
Table 2.
SCHIZOPHRENIA PATIENTS ALWAYS VS NEVER PRESCRIBED ANTIPSYCHOTIC MEDICATIONS: WORK FUNCTIONING
| X2 | df | Sig | Odds Ratio | 95% CI | |
|---|---|---|---|---|---|
| 2 Year FU | 2.92 | 1 | .087 | 3.60 | .80–16.20 |
| 4.5 Year FU | 12.22 | 1 | .000 | 15.79 | 2.80–88.99 |
| 7.5 Year FU | 8.77 | 1 | .003 | 8.25 | 1.90–35.91 |
| 10 Year FU | 12.91 | 1 | .000 | 16.71 | 2.98–93.89 |
| 15 Year FU | 5.81 | 1 | .016 | 6.72 | 1.33–33.91 |
| 20 Year FU | 10.49 | 1 | .001 | 15.40 | 2.50–95.05 |
Further detailed data on work functioning, negative symptoms and psychosis at each followup assessment are reported in Supplemental Tables 2, 3, and 4.
Looking at individual followup assessments, there were no significant differences between these 2 groups at the 2-year followups. However, rather surprisingly, after the 2-year assessments, the patients with schizophrenia not on antipsychotic medications over the last 18 years showed improvement and showed a higher rate of employment. Starting at the 4.5 year assessments and continuing until the 20-year assessments over 65% of these patients were working half-time or more. Thus, starting at the 4.5 year assessments and continuing over the 5 assessments to the 20-year followups, significantly more of the patients with schizophrenia continuously not on antipsychotics were working, compared to those prescribed antipsychotics. The 5 chi-squares (over 18 years) comparing patients with schizophrenia with the 2 different medication schedules ranged from χ2=5.81 to χ2=12.91, with 1 df, p<0.02.
3.2 Work functioning at each assessment for all patients with schizophrenia prescribed antipsychotics vs. not prescribed antipsychotics
To include the group of patients with schizophrenia sometimes prescribed antipsychotics (group 2) we conducted comparisons of work functioning of all patients with schizophrenia prescribed antipsychotics with all patients with schizophrenia not on antipsychotics at each particular followup, regardless of whether these patients were continuously on antipsychotics throughout the 20 years. This produced similar results. There were no significant differences at the 2-year followups on work adjustment. After the 2-year followups, at each of the next 5 followups over 20-years significantly more of the patients with schizophrenia not on antipsychotics were working. These latter results at each followup assessment include the 6 patients with schizophrenia who had a 20-year followup but had less than 4 followup assessments. Thus 9 of 36 patients with schizophrenia prescribed antipsychotics at the 20-year assessments were working (25%) as compared to 16 of the 22 schizophrenia patients not on antipsychotics (73%) (χ2=12.683, 1 df, p<0.001).
3.3 Work functioning in patients with schizophrenia looking separately at patients with schizophrenia with negative symptoms
In general, patients with schizophrenia continuously prescribed antipsychotics were significantly more likely to have negative symptoms than those not prescribed antipsychotics at the 4.5 year followups (χ2=5.72, 1 df, p<0.02) and at the 20 year followups (χ2=5.25, 1 df, p<0.05). After the first followup, patients with schizophrenia with negative symptoms were significantly less likely to be working at 4 of the 6 followup assessments (χ2=4.20 to χ2=8.39, with 1 df, p<0.05). In addition, negative symptoms were a potential hindrance to working. The data indicating that at the 2-year followups only one schizophrenia patient with negative symptoms was working, at the 7.5 year followups only 2 schizophrenia patients were working, at the 15-year followups only 3 schizophrenia patients working and at the 20-year followups only 2 schizophrenia patients were working.
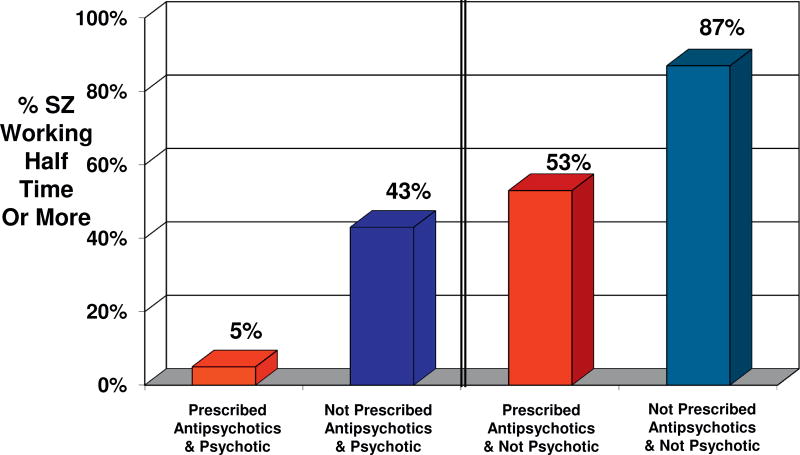
3.4 Work functioning in patients with schizophrenia prescribed antipsychotic medications vs. patients with schizophrenia not on antipsychotics, controlling for psychosis
Figure 2 reports the data comparing work functioning in patients with schizophrenia prescribed antipsychotics who were psychotic with schizophrenia patients not on antipsychotics who were psychotic at the 20-year followups. Similarly, we compared work functioning in patients with schizophrenia prescribed antipsychotics who were not psychotic with patients with schizophrenia not on antipsychotics who were not psychotic.
FIGURE 2.
Combination Of Antipsychotic Medications And Psychosis In Schizophrenia: Relation To Work Functioning At 20 Year Assessments
For patients with schizophrenia, psychosis is one of the major measures of illness. The comparison of schizophrenia patients with psychosis allows comparison of work functioning with partial controls for this measure of illness.
The presence of psychosis was a strong influence on work adjustment after the 2-year followups. At the last 5 assessments (4½ years to 20 years) patients with schizophrenia with psychotic symptoms showed significantly poorer work functioning (χ2=5.55 to χ2=22.0, 1 df, p<0.02) than patients who did not have psychotic symptoms. After the 2 year assessment over 60% of the schizophrenia patients who did not have psychotic activity were working half-time or more.
The results in Figure 2 indicate that when the patients with schizophrenia prescribed antipsychotics at the 20-year followups were compared to those not prescribed antipsychotics at the 20-year followups the patients with schizophrenia not prescribed antipsychotics were significantly more likely to be working. The results on antipsychotics prior to the 20 year followups were similar. Thus at each of the last 4 followups significantly more patients with schizophrenia who were not prescribed antipsychotics and were not psychotic were working as compared to those who were prescribed antipsychotics who were not psychotic at the parallel followup. Similarly, at 3 of the last 5 followups significantly more of the patients with schizophrenia who were not on antipsychotics and were psychotic were working as compared to the patients with schizophrenia who were prescribed antipsychotics and were psychotic.
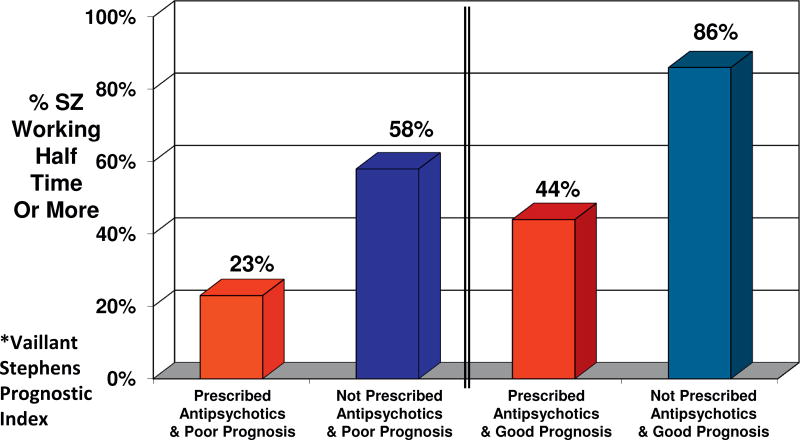
3.5 Work functioning in patients with schizophrenia prescribed antipsychotics, controlling for prognostic factors
Figure 3 reports the data on work functioning at the 20 year followups when the patients with schizophrenia prescribed antipsychotics were compared to the patients with schizophrenia not on antipsychotics. The figure presents the data while controlling for prognostic potential (Vaillant, 1978). The results indicate that patients with schizophrenia with poor prognostic potential who were not on antipsychotics had significantly better work functioning than patients with schizophrenia prescribed antipsychotics who had poor prognostic potential (χ2=4.31, p < .01).
FIGURE 3.
Do Antipsychotics Influence Work Functioning In Schizophrenia? Controlling For Potential Favorable Prognosis* at 20 Year Assessments
Partly because of the small number of patients with schizophrenia with good prognostic potential there were not significant differences in work functioning between patients with schizophrenia prescribed antipsychotics and those not prescribed antipsychotics, although 40% more of patients with schizophrenia not prescribed antipsychotics were working.
3.6 Work functioning in patients with schizophrenia prescribed antipsychotics, controlling for premorbid developmental achievements
Figure 4 reports data on work functioning at the 20 year followups when the patients with schizophrenia prescribed antipsychotics were compared to the patients with schizophrenia not on antipsychotics. The figure presents the data while controlling for premorbid developmental achievements (Zigler and Glick, 2001). The results indicate that patients with schizophrenia with poor premorbid developmental achievements who were not on antipsychotics had significantly better work functioning than patients with schizophrenia prescribed antipsychotics who had poor premorbid developmental achievements (χ2=6.87, p < .05). Again, at the 20-year followups, within the very small subsample of patients with schizophrenia with good premorbid achievements prior to becoming ill, more of the patients with schizophrenia who were prescribed antipsychotics were not working as compared to the patients with schizophrenia who were not prescribed antipsychotics. However, because of the very small sample size of patients with schizophrenia with good premorbid developmental achievements the differences just missed achieving statistical significance (p=.06).
FIGURE 4.
Do Antipsychotics Influence Work Functioning In Schizophrenia? Controlling For Premorbid Developmental Achievements* at 20 Year Assessments
3.7 Antipsychotics and work functioning, controlling for a combination of different factors using logistic regression
While each of the factors that could influence the comparisons of posthospital work functioning in patients with schizophrenia prescribed antipsychotics vs those not prescribed antipsychotics was examined separately, we also examined these factors in combination with other potential factors to control for the combined effects of these variables on posthospital work functioning. Thus there are multiple potential factors which could influence posthospital work functioning for patients with schizophrenia, and these were assessed. These include prehospital work history, prehospital social adjustment, education, marital status, acute onset, precipitating events, and blunted affect from the scales of Vaillant and Stephens (Vaillant, 1962; Vaillant, 1978; Westermeyer and Harrow, 1984; Stephens et al., 1997), and the scales of Zigler (Zigler and Glick, 2001), as well as posthospital positive symptoms and posthospital negative symptoms. The goal was to control or parcel out the combined influence of these factors when studying work functioning over time in medicated vs unmedicated patients with schizophrenia.
To make the best use of the data, we included the results on symptoms and functioning from all of the 70 patients with schizophrenia using the combined data from all of the six followups in the logistic and proportional odds models analysis. The p values and odds ratios are from the joint models after adjusting for symptoms and other potential confounding factors. The results which emerged using logistic regression (McCullagh and Nelder, 1989; Hanley et al., 2003) with GEE method, do not support the use of antipsychotics to increase work functioning. Employing the odds ratio, the patients with schizophrenia not on antipsychotics at any of the followups were 1.76 times more likely (p=0.17) to have adequate work functioning compared to those schizophrenia patients prescribed antipsychotics throughout the 20-years. The more refined proportional odds model using generalized estimating equation method (GEE) (Liang and Zeger, 1986) generates much more significant results with the odds ratio for effects size being 2.39 and p=0.0273. The data indicate that any hypothesis based on the view that antipsychotics facilitate work functioning are extremely doubtful since the results for work functioning were running strongly (at significant levels) in the opposite direction.
3.8 Work functioning for mood disordered psychotic patients
The data on employment for the initially psychotic mood disordered patients showed a higher level of work functioning for those patients, compared to the relatively poor work functioning of many patients with schizophrenia (repeated measures ANOVA F= 17.92, df=1,62 p < .001). Over 60% of the initially psychotic mood disordered patients were working (half-time or more) at each of the 6 followup assessments over the 20 years.
After the 2-year followups, at each of the last five followups over the next 18 years the mood disordered patients who were not prescribed antipsychotics showed significantly better work functioning than those prescribed antipsychotic medications (e.g., at the 20 year followups t=2.40, 54 df, p=.02). At each of the last 5 followup assessments, over 75% of the mood disordered patients who were not on antipsychotics were working ½ time or more.
3.9 Work functioning for the combined sample of initially psychotic patients
The two major samples of initially psychotic patients (the patients with schizophrenia and the initially psychotic mood disordered patients) were combined to provide a general estimate of posthospital work performance for these 2 initially psychotic groups. A series of 2×2 ANOVAs were performed, one at each followup with the 2 dimensions assessing work performance: 1) antipsychotic medications (prescribed antipsychotics vs not prescribed antipsychotics) and 2) diagnosis (schizophrenia patients vs mood disordered patients). The data assessing the relationship between better work performance and not being prescribed antipsychotics were significant at each of the 6 followups, with the significance level at the last 5 followups (year 4.5 to year 20) being beyond p < .001.
4. Discussion
Recent summaries of the literature by Leucht and colleagues (Leucht et al., 2012b) have noted that there is still not strong evidence of positive effects of treatment with antipsychotic medications beyond the first 3 years of treatment (Leucht et al., 2012a). Despite this, the great majority of workers in the field view antipsychotics positively for both short-term and long-term treatment.
However, important theoretical discussions by major theorists have questioned the long-term efficacy of antipsychotic medications (Harding et al., 1987a; Healy, 2002; Moncrieff, 2009a; Moncrieff, 2009b; Whitaker, 2010; Whitaker, 2011; Murray et al., 2016). Negative evidence on the long-term efficacy of antipsychotics have emerged from our own longitudinal studies (Harrow et al., 2012; Harrow et al., 2014; Harrow and Jobe, 2007) and the longitudinal studies of Wunderink (Wunderink et al., 2013) of Moilanen, Jääskeläinena and colleagues (Moilanen et al., 2013) using data from the Northern Finland Birth Cohort Study, by data from the Danish OPUS trials (Wils et al., 2016), the study of Lincoln and Jung in Germany (Jung et al., 2016), and the studies of Bland in Canada (Bland et al., 1978). These longitudinal studies have not shown positive effects for patients with schizophrenia prescribed antipsychotic for prolonged periods. In addition to the results indicating the rarity of periods of complete recovery for patients with schizophrenia prescribed antipsychotics for prolonged intervals, our research has indicated a significantly higher rate of periods of recovery for patients with schizophrenia who have gone off antipsychotics for prolonged intervals (Harrow et al., 2012; Harrow et al., 2014). Other studies across the globe also have raised questions about the long-term necessity of antipsychotic medications (Bleuler, 1978; Fenton and McGlashan, 1987; Harding et al., 1987b; Jablensky and Sartorius, 2008; McGorry et al., 2013), although the research of Ioannidis and colleagues (2005) on statistical effects should also be considered.
4.1 Antipsychotic medication and the longitudinal course
A pattern has begun to emerge that suggests progressive loss of efficacy with the length of antipsychotic drug treatment such that the non-medicated group begins to improve and approach the medicated group at about, or slightly after, 2–3 years. The lack of positive results after 2 years for antipsychotics may be influenced by a) a natural improvement for some unmedicated patients with schizophrenia 2–3 years after the most acute phase, b) the blocking of DA receptors by antipsychotic medications may reduce incentive, and reduces drive states and motivations (Berridge, 2007) which might otherwise activate patients towards sustained employment and, c) over time there may be a medication-generated build up of supersensitive dopamine receptors, or excess dopamine receptors for some or many patients with schizophrenia. Both animal research (Seeman et al., 2006) and human research (Chouinard and Jones, 1980; Fallon et al., 2012; Seeman and Seeman, 2014; Suzuki et al., 2015; Silvestri et al., 2000) have found evidence which could support this latter view. d) It is possible that for some patients successful work could encourage them and help them gain energy and purpose, with the increased motivation reducing the subjective impact of their disorder and even reducing the presence of some major symptoms.
Of key importance, the data indicate that there is a low level of work functioning for patients with schizophrenia prescribed antipsychotics for prolonged periods, and a relatively higher level of work employment for patients with schizophrenia off antipsychotics for prolonged periods. In our sample of patients with schizophrenia, the period of 2–3 or more years seem to be when the improvement in work functioning for the unmedicated patients became apparent.
The data which emerged using logistic regression do not prove that antipsychotics interfere with work functioning, since multiple other factors may be involved. But the significant differences in favor of the nonmedicated schizophrenia patients which emerged casts considerable doubt on any hypothesis based on the view that antipsychotics facilitate work functioning. Since several other studies with similar results are beginning to emerge this negative conclusion on antipsychotics should be considered.
Overall, our data indicate that a proportion of patients with schizophrenia can work, without antipsychotics. For schizophrenia patients on continuous antipsychotics, a large percentage of these continuously treated patients have been rehospitalized multiple times. Some in the field have encouraged continual use of antipsychotic medications, on the basis of it maintaining or improving the favorable work outcome of some patients with schizophrenia (Tandon et al., 2008). Our data for the first 20 years did not support this assumption about antipsychotic medications, and even indicate that the opposite may be true for many patients with schizophrenia. However, work functioning is a complex area and multiple factors can influence it. These include the strong influence of cognitive impairment (Green, 1996) as well as negative symptoms. In addition, previous research has indicated at least some persisting psychotic activity for many medicated schizophrenia patients prescribed antipsychotics (Harrow et al., 2014). The current data (Figure 2) indicate a high level of unemployment for the patients with schizophrenia with psychotic activity prescribed antipsychotics.
Undoubtedly the concern of some patients about losing disability payments may also have contributed to the relatively low rate of work for some patients with schizophrenia. However, the high rate of working for patients with schizophrenia not on antipsychotics suggests that some subgroups of patients with schizophrenia will work when their symptoms are reduced and they are not hindered by negative symptoms. Further, the longitudinal data suggest that the relatively high rate of unmedicated schizophrenia patients who are working indicate that these differences are not just a function of potential increased ease of obtaining disability payments, although it is one additional factor.
Overall, the data indicate that just as short-term studies of the efficacy of antipsychotic medications have shown an impact in reducing symptoms severity, it is important to assess the results of longer term exposure to antipsychotics on level of symptomatology, work functioning, cognition, and quality of life.
It is important to underscore that the results presented, based on a naturalistic design, are in agreement with other studies that used more controlled designs, including random assignment, which support the cautionary statements about the effect of long-term exposure to antipsychotic medications (Wunderink et al., 2013).
4.2 Work functioning of the initially psychotic mood disordered and the schizophrenia patients
The analysis of work functioning for the initially psychotic mood disordered patients as compared to work functioning for the patients with schizophrenia showed large significant differences over the 20 years in favor of the mood disordered patients. These data would support current views about the greater vulnerability to work dysfunction over time by patients with schizophrenia and to more psychopathology and poorer functioning for them.
The data indicated that after the 2 year followups the mood disordered patients not on antipsychotics had significantly better work functioning at each of the next 5 followup assessments over the successive 18 year period. This pattern of significant differences in work functioning in favor of those not treated with antipsychotics starting after the 2 year followups, and continuing for the next 16–18 years is similar to the pattern found for the patients with schizophrenia.
Viewed longitudinally, the combined sample of patients with schizophrenia and mood disordered patients prescribed antipsychotics were significantly less likely to be working. This included the patients with schizophrenia when analyzed alone, the mood disordered patients when analyzed without the patients with schizophrenia, and the combined sample when analyzed together. Long-term results for patients who are prescribed antipsychotics are important to assess, since they are prescribed (at times by non-psychiatrists) to many different types of people, including children and older people to prevent disruptive behavior (Olfson et al., 2012; Stefanacci et al., 2014). While administered widely, we still do not have clear knowledge of all of the effects. Further questions and study of it would seem critical.
Supplementary Material
Highlights.
After the first 3 years, antipsychotic treatment for schizophrenia is less effective
20 years sustained of antipsychotic treatment does not improve work function in schizophrenia
Many non-medicated schizophrenia patients show adequate work functioning after the acute phase of illness.
Acknowledgments
Funding Information:
Supported, in part, by USPHS Grants MH-26341 and MH-068688 from the National Institute of Mental Health, USA (Dr. Harrow) and a Grant from the Foundation for Excellence in Mental Health Care (Dr. Harrow).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Alonso J, Croudace T, Brown J, Gasquet I, Knapp MR, Suárez D, Novick D. Health related quality of life (HRQL) and continuous antipsychotic treatment: 3 year results from the schizophrenia health outcomes (SOHO) study. Value Health. 2009;12:536–543. doi: 10.1111/j.1524-4733.2008.00495.x. [DOI] [PubMed] [Google Scholar]
- Barnes SS, Badre N. Is the evidence strong enough to warrant long-term antipsychotic use in compulsory outpatient treatment? Psychiatric Services. 2016 doi: 10.1176/appi.ps.201500408. [DOI] [PubMed] [Google Scholar]
- Berridge K. The debate over dopamine’s role in reward: the case for incentive salience. Psychopharmacology. 2007;191:391–431. doi: 10.1007/s00213-006-0578-x. [DOI] [PubMed] [Google Scholar]
- Bland R, Parker J, Orn H. Prognosis in schizophrenia: prognostic predictors and outcome. Arch Gen Psychiatry. 1978;35:72–77. doi: 10.1001/archpsyc.1978.01770250074007. [DOI] [PubMed] [Google Scholar]
- Bleuler M. The Schizophrenic Disorders: Long-Term Patient and Family Studies. Yale University Press; New Haven: 1978. [Google Scholar]
- Bola JR, Lehtinen K, Cullberg J, Ciompi L. Psychosocial treatment, antipsychotic postponement, and low dose medication strategies in first episode psychosis: A review of the literature. Psychosis. 2009;1:4–18. [Google Scholar]
- Bond GR, Drake RE, Becker DR. Generalizability of the individual placement and support (ips) model of supported employment outside the US. World Psychiatry. 2012;11:32–39. doi: 10.1016/j.wpsyc.2012.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buchanan R, Kreyenbuhl J, Kelly D, Noel J, Boggs D, Fischer B, Himelhoch S, Fang B, Peterson E, Aquino P, Keller W. The 2009 Schizophrenia PORT psychopharmacological treatment recommendations and summary statements. Schizophr. Bull. 2010;36:71–93. doi: 10.1093/schbul/sbp116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buchsbaum MS, Potkin SG, Siegel BV, Lohr J, Katz M, Gottschalk LA, Gulasekaram B, Marshall JF, Lottenberg S, Teng CY. Striatal metabolic rate and clinical response to neuroleptics in schizophrenia. Arch. Gen. Psychiatry. 1992;49:966–974. doi: 10.1001/archpsyc.1992.01820120054008. [DOI] [PubMed] [Google Scholar]
- Carpenter WT, Jr, Sacks MH, Strauss JS, Bartko JJ, Rayner J. Evaluating signs and symptoms: comparison of structured interview ans clinical approaches. Br. J. Psychiatry. 1976;128:397–403. doi: 10.1192/bjp.128.4.397. [DOI] [PubMed] [Google Scholar]
- Chouinard G, Jones BD. Neuroleptic-induced supersensitivity psychosis: clinical and pharmacologic characteristics. Am. J. Psychiatry. 1980;137:16–21. doi: 10.1176/ajp.137.1.16. [DOI] [PubMed] [Google Scholar]
- Ciompi L, Hoffmann H. Soteria Berne: an innovative milieu therapeutic approach to acute schizophrenia based on the concept of affect-logic. World Psychiatry. 2004;3:140–146. [PMC free article] [PubMed] [Google Scholar]
- Endicott J, Spitzer R. A diagnostic interview. Arch Gen Psychiat. 1978;35:837–844. doi: 10.1001/archpsyc.1978.01770310043002. [DOI] [PubMed] [Google Scholar]
- Fallon P, Dursun S, Deakin B. Drug-induced supersensitivity psychosis revisited: characteristics of relapse in treatment-compliant patients. Ther Adv Psychopharmacol. 2012;2:13–22. doi: 10.1177/2045125311431105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fenton W, McGlashan T. Sustained remission in drug-free schizophrenic patients. Am J Psychiatry. 1987;144:1306–1309. doi: 10.1176/ajp.144.10.1306. [DOI] [PubMed] [Google Scholar]
- Gilbert PL, Harris MJ, Jeste DV, McAdams LA. Considering neuroleptic maintenance and taper on a continuum: need for individual rather than dogmatic approach. Arch Gen Psychiatry. 1995;52:209–212. doi: 10.1001/archpsyc.1995.03950150041008. [DOI] [PubMed] [Google Scholar]
- Green M. What are the functional consequences of neurocognitive deficits in schizophrenia? Am J Psychiatry. 1996;153:321–330. doi: 10.1176/ajp.153.3.321. [DOI] [PubMed] [Google Scholar]
- Green M, Kern R, Braff D, Mintz J. Neurocognitive deficits and functional outcome in schizophrenia: are we measuring the "right stuff"? Schizophr. Bull. 2000;26:119–36. doi: 10.1093/oxfordjournals.schbul.a033430. [DOI] [PubMed] [Google Scholar]
- Hanley JA, Negassa A, Edwardes MD, Forrester JE. Statistical analysis of correlated data using generalized estimating equations: an orientation. Am. J. Epidemiol. 2003;157:364–375. doi: 10.1093/aje/kwf215. [DOI] [PubMed] [Google Scholar]
- Harding CM, Strauss JS, Hafez H, Lieberman PB. Work and mental illness: I. Toward an integration of the rehabilitation process. J. Nerv. Ment. Dis. 1987a;175:317–326. [PubMed] [Google Scholar]
- Harding C, Brooks G, Ashikiga T, Strauss J, Breier A. The Vermont longitudinal study of persons with severe mental illness: II. Long-term outcome of subjects who retrospectively met DSM-III criteria for schizophrenia. Am J Psychiat. 1987b;144:727–735. doi: 10.1176/ajp.144.6.727. [DOI] [PubMed] [Google Scholar]
- Harrow M, Jobe T, Faull R. Does treatment of schizophrenia with antipsychotic medications eliminate or reduce psychosis? A 20-year multi-follow-up study. Psychol. Med. 2014;44:3007–3016. doi: 10.1017/S0033291714000610. [DOI] [PubMed] [Google Scholar]
- Harrow M, Jobe TH. Does long-term treatment of schizophrenia with antipsychotic medications facilitate recovery? Schizophr. Bull. 2013;39:962–965. doi: 10.1093/schbul/sbt034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrow M, Goldberg J, Grossman L, Meltzer H. Outcome in manic disorders: a naturalistic followup study. Arch Gen Psychiat. 1990;47:665–671. doi: 10.1001/archpsyc.1990.01810190065009. [DOI] [PubMed] [Google Scholar]
- Harrow M, Grossman L, Jobe T, Herbener E. Do patients with schizophrenia ever show periods of recovery?: A 15 year multi-followup study. Schizophr. Bull. 2005;31:723–734. doi: 10.1093/schbul/sbi026. [DOI] [PubMed] [Google Scholar]
- Harrow M, Jobe TH, Faull RN. Do all schizophrenia patients need antipsychotic treatment continuously throughout their lifetime? A 20-year longitudinal study. Psychol. Med. 2012;42:2145–2155. doi: 10.1017/S0033291712000220. [DOI] [PubMed] [Google Scholar]
- Harrow M, Jobe T. Factors involved in outcome and recovery in schizophrenia patients not on antipsychotic medications: A 15-year multi-followup study. J Nerv Ment Dis. 2007;195:406–414. doi: 10.1097/01.nmd.0000253783.32338.6e. [DOI] [PubMed] [Google Scholar]
- Healy D. The Creation of Psychopharmacology. Harvard University Press; 2002. [Google Scholar]
- Herbener E, Harrow M. Are negative symptoms associated with functioning deficits in both schizophrenic and non-schizophrenic patients? A ten-year longitudinal analysis. Schizophr. Bull. 2004;30:813–825. doi: 10.1093/oxfordjournals.schbul.a007134. [DOI] [PubMed] [Google Scholar]
- Hollingshead A, Redlich F. Social Class and Mental Illness. John Wiley & Sons; New York: 1958. [Google Scholar]
- Howes OD, Kambeitz J, Kim E, Stahl D, Slifstein M, Abi-Dargham A, Kapur S. The nature of dopamine dysfunction in schizophrenia and what this means for treatment: meta-analysis of imaging studies. Arch Gen Psychiatry. 2012;69:776–786. doi: 10.1001/archgenpsychiatry.2012.169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ioannidis JP. Why most published research findings are false. PLos med. 2005;2:e124. doi: 10.1371/journal.pmed.0020124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jablensky A, Sartorius N. What did the WHO studies really find? Schizophr. Bull. 2008;34:253–255. doi: 10.1093/schbul/sbm151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jobe T, Harrow M. Schizophrenia course, long-term outcome, recovery, and prognosis. Curr Dir Psychol Sci. 2010;19:220–225. [Google Scholar]
- Johnstone EC, Macmillan JF, Frith CD, Benn DK, Crow TJ. Further investigation of the predictors of outcome following first schizophrenic episodes. Br. J. Psychiatry. 1990;157:182–189. doi: 10.1192/bjp.157.2.182. [DOI] [PubMed] [Google Scholar]
- Jung E, Wiesjahn M, Wendt H, Bock T, Rief W, Lincoln TM. Symptoms, functioning and coping strategies in individuals with schizophrenia spectrum disorders who do not take antipsychotic medication: a comparative interview study. Psychol. Med. 2016 doi: 10.1017/S0033291716000775. Advanced Access. [DOI] [PubMed] [Google Scholar]
- Leucht S, Tardy M, Komossa K, Heres S, Kissling W, Davis JM. Maintenance treatment with antipsychotic drugs for schizophrenia. Cochrane Database Syst. Rev. 2012a;5 doi: 10.1002/14651858.CD008016.pub2. [DOI] [PubMed] [Google Scholar]
- Leucht S, Tardy M, Komossa K, Heres S, Kissling W, Salanti G, Davis JM. Antipsychotic drugs versus placebo for relapse prevention in schizophrenia: a systematic review and meta-analysis. Lancet. 2012b doi: 10.1016/S0140-6736(12)60239-6. [DOI] [PubMed] [Google Scholar]
- Liang K, Zeger S. Longitudinal data analysis using Generalized Linear Models. Biometrika. 1986;73:13–22. [Google Scholar]
- McCullagh P, Nelder J. Generalized Linear Models. 2. Chapman & Hall; New York, NY: 1989. [Google Scholar]
- McGorry P, Alvarez-Jimenez M, Killackey E. Antipsychotic medication during the critical period following remission from first-episode psychosis: less is more. JAMA Psychiatry. 2013;70:898–900. doi: 10.1001/jamapsychiatry.2013.264. [DOI] [PubMed] [Google Scholar]
- McGurk SR, Mueser KT, Covell NH, Cicerone KD, Drake RE, Silverstein SM, Medialia A, Myers R, Bellack AS, Bell MD. Mental health system funding of cognitive enhancement interventions for schizophrenia: Summary and update of the New York Office of Mental Health expert panel and stakeholder meeting. Psychiatr. Rehabil. J. 2013;36:133–145. doi: 10.1037/prj0000020. [DOI] [PubMed] [Google Scholar]
- Moilanen J, Haapea M, Miettunen J, Jääskeläinen E, Veijola J, Isohanni M, Koponen H. Characteristics of subjects with schizophrenia spectrum disorder with and without antipsychotic medication–A 10-year follow-up of the Northern Finland 1966 Birth Cohort study. Eur Psychiatry. 2013;28:53–58. doi: 10.1016/j.eurpsy.2011.06.009. [DOI] [PubMed] [Google Scholar]
- Moncrieff J. A critique of the dopamine hypothesis of schizophrenia and psychosis. Harv. Rev. Psychiatry. 2009a;17:214–225. doi: 10.1080/10673220902979896. [DOI] [PubMed] [Google Scholar]
- Moncrieff J. The Myth of the Chemical Cure: A Critique of Psychiatric Drug Treatment. Palgrave Macmillan; Basingstoke, UK: 2009b. [Google Scholar]
- Mueser KT, Deavers F, Penn DL, Cassisi JE. Psychosocial Treatments for Schizophrenia. Annu Rev Clin Psychol. 2013;9:465–497. doi: 10.1146/annurev-clinpsy-050212-185620. [DOI] [PubMed] [Google Scholar]
- Murray RM, Quattrone D, Natesan S, van Os J, Nordentoft M, Howes O, Di Forti M, Taylor D. Should psychiatrists be more cautious about the long-term prophylactic use of antipsychotics? Br. J. Psychiatry. 2016;209:361–365. doi: 10.1192/bjp.bp.116.182683. [DOI] [PubMed] [Google Scholar]
- Olfson M, Blanco C, Liu S, Wang S, Correll CU. National trends in the office-based treatment of children, adolescents, and adults with antipsychotics. Arch. Gen. Psychiatry. 2012;69:1247–1256. doi: 10.1001/archgenpsychiatry.2012.647. [DOI] [PubMed] [Google Scholar]
- Rosenheck R, Leslie D, Keefe R, McEvoy J, Swartz M, Perkins D, Stroup S, Hsiao JK, Lieberman J. Barriers to employment for people with schizophrenia. Am. J. Psychiatry. 2006;163:411–417. doi: 10.1176/appi.ajp.163.3.411. [DOI] [PubMed] [Google Scholar]
- Seeman MV, Seeman P. Is schizophrenia a dopamine supersensitivity psychotic reaction? Prog. Neuro-Psychopharmacol. Biol. Psychiatry. 2014;48:155–160. doi: 10.1016/j.pnpbp.2013.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seeman P, Schwarz J, Chen JF, Szechtman H, Perreault M, McKnight GS, Roder JC, Quirion R, Boksa P, Srivastava LK. Psychosis pathways converge via D2 high dopamine receptors. Synapse. 2006;60:319–346. doi: 10.1002/syn.20303. [DOI] [PubMed] [Google Scholar]
- Seikkula J, Alakare B, Aaltonen J. The Comprehensive Open-Dialogue Approach in Western Lapland: II. Long-term stability of acute psychosis outcomes in advanced community care. Psychosis. 2011;3:192–204. [Google Scholar]
- Silvestri S, Seeman MV, Negrete J, Houle S, Shammi C, Remington GJ, Kapur S, Zipursky RB, Wilson AA, Christensen BK. Increased dopamine D2 receptor binding after long-term treatment with antipsychotics in humans: a clinical PET study. Psychopharmacology (Berl) 2000;152:174–180. doi: 10.1007/s002130000532. [DOI] [PubMed] [Google Scholar]
- Stefanacci RG, Arnicar R, Clark TR, Gerber J, Haimowitz D, Kuhlor A, Scanland S. Improving the management of disruptive behavior and reducing antipsychotic medications in nursing facility residents. The Consultant Pharmacist®. 2014;29:797–812. doi: 10.4140/TCP.n.2014.797. [DOI] [PubMed] [Google Scholar]
- Stephens J, Pascal R, McHugh P. Long-term follow-up of patients hospitalized for schizophrenia, 1913 to 1940. J Nerv Ment Dis. 1997;185:715–721. doi: 10.1097/00005053-199712000-00001. [DOI] [PubMed] [Google Scholar]
- Strauss J, Carpenter W. The prediction of outcome in schizophrenia: I characteristics of outcome. Arch Gen Psychiatry. 1972;27:739–746. doi: 10.1001/archpsyc.1972.01750300011002. [DOI] [PubMed] [Google Scholar]
- Suzuki T, Kanahara N, Yamanaka H, Takase M, Kimura H, Watanabe H, Iyo M. Dopamine supersensitivity psychosis as a pivotal factor in treatment-resistant schizophrenia. Psychiatry Res. 2015;227:278–282. doi: 10.1016/j.psychres.2015.02.021. [DOI] [PubMed] [Google Scholar]
- Tandon R, Belmaker R, Gattaz WF. World Psychiatric Association Pharmacopsychiatry Section statement on comparative effectiveness of antipsychotics in the treatment of schizophrenia. Schizophr. Res. 2008;100:20–38. doi: 10.1016/j.schres.2007.11.033. [DOI] [PubMed] [Google Scholar]
- Vaillant G. A 10-year followup of remitting schizophrenics. Schizophr. Bull. 1978;4:78–85. doi: 10.1093/schbul/4.1.78. [DOI] [PubMed] [Google Scholar]
- Vaillant G. Prospective prediction of schizophrenic remission. Arch Gen Psychiatry. 1964;11:509–518. doi: 10.1001/archpsyc.1964.01720290051007. [DOI] [PubMed] [Google Scholar]
- Vaillant G. The prediction of recovery in schizophrenia. J Nerv Ment Dis. 1962;135:448–457. doi: 10.1097/00005053-196212000-00006. [DOI] [PubMed] [Google Scholar]
- Westermeyer J, Harrow M. Prognosis and outcome using broad DSM-II and narrow DSM-III concepts of schizophrenia. Schizophr. Bull. 1984;10:624–637. doi: 10.1093/schbul/10.4.624. [DOI] [PubMed] [Google Scholar]
- Whitaker R. Anatomy of an Epidemic: Magic Bullets, Psychiatric Drugs, and the Astonishing Rise of Mental Illness in America. Broadway Books; New York: 2011. [DOI] [PubMed] [Google Scholar]
- Whitaker R. Mad in America: Bad Science, Bad Medicine, and the Enduring Mistreatment of the Mentally Ill. Basic Books; Cambridge, MA: 2010. [PubMed] [Google Scholar]
- Wils RS, Gotfredsen DR, Hjorthøj C, Austin SF, Albert N, Secher RG, Thorup AAE, Mors O, Nordentoft M. Antipsychotic medication and remission of psychotic symptoms 10 years after a first-episode psychosis. Schizophr. Res. 2016 doi: 10.1016/j.schres.2016.10.030. [DOI] [PubMed] [Google Scholar]
- Wunderink L, Nieboer RM, Wiersma D, Sytema S, Nienhuis FJ. Recovery in remitted first-episode psychosis at 7 years of follow-up of an early dose reduction/discontinuation or maintenance treatment strategy long-term follow-up of a 2-year randomized clinical trial recovery in remitted first-episode psychosis. JAMA Psychiatry. 2013;70:913–920. doi: 10.1001/jamapsychiatry.2013.19. [DOI] [PubMed] [Google Scholar]
- Zigler E, Glick M. The developmental approach to adult psychopathology. Clin Psychol. 2001;54:2–11. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.