Abstract
Objective
Our hypothesis was that hypnotic analgesia reduces pain and anxiety during electromyography [EMG].
Design
Prospective randomized controlled clinical trial at outpatient electrodiagnostic clinics in teaching hospitals. Just prior to EMG, 26 subjects were randomized to one of three 20 minute audio programs: (EDU) education about EMG (n=8); (HYP-C) hypnotic induction without analgesic suggestion (n=10) or; (HYP-ANLG) hypnotic induction with analgesic suggestion (n=8). The blinded electromyographer provided a post-hypnotic suggestion at the start of EMG. After EMG, subjects rated worst and average pain, and anxiety using visual analog scales.
Results
Mean values for the EDU, HYP-C and HYP-ANLG groups were not significantly different (mean ± sd): worst pain 67 ± 25, 42 ± 18, 49 ± 30: average pain 35 ± 26, 27 ± 14, 25 ± 22; anxiety 44 ± 41, 42 ± 23, 22 ± 24. When hypnosis groups were merged [n=18] and compared with the EDU condition [n=8], average and worst pain and anxiety were less for the hypnosis group than EDU, but this was statistically significant only for worst pain [hypnosis - 46 ± 24 vs. EDU - 67 ± 35, p=0.049] with a 31% average reduction.
Conclusions
A short hypnotic induction appears to reduce worst pain during EMG.
Keywords: Electromyography [EMG], Hypnosis, Hypnotic Analgesia
When carried out by trained physicians, needle electromyography (EMG) is a safe and effective diagnostic tool for evaluating neuromuscular disorders. However, EMG and nerve conduction studies [NCS] are frequently reported as painful for many patients. Most electromyographers have experienced patients prematurely discontinuing an EMG before enough studies have been undertaken to make an informed diagnostic conclusion.
Gans and Kraft reported that the most significant factor correlating with pain during electrodiagnostic evaluation was patient gender, with females reporting pain significantly more than men (p<0.001), and that NCS were more often perceived as painful than EMG (p<0.01).1 In a more recent study by Wee et al, during both NCS and EMG, there was no correlation between patient pain and either the needle gauge employed, age of the patient, and or the BMI of the patient. EMG was found to be more painful than NCS.2
There have been some attempts to reduce the pain associated with EMG. La Joie reported that amongst 10 adults undergoing EMG, the use of either 50mg of meperidine or 10mg of methadone combined with 25mg of Phenergan, lead to improved pain and anxiety scores, with an acceptable level of sedation, and no impediment to obtaining patient cooperation during the test when measuring maximum voluntary effort or ascertaining MUAP recruitment patterns.3 However, since most electrodiagnostic evaluations are performed as outpatient procedures, patients often intend to operate an automobile or need to negotiate public transportation following the study, and/or plan to return to social or vocational responsibilities after completing the test. Viewed in this context, oral sedation may not be realistic to provide in the majority of examinations.
As an alternative to pharmacologic approaches, Spence and Guyton employed audio analgesia consisting of music and “white noise” that patients could activate as a counterirritant during perceived pain of the EMG. They additionally employed a two minute instructional segment prior to the music with the purpose of both explaining the procedure and providing a suggestion intended to eliminate fear and pain. This intervention produced “substantial” reduction in pain complaints amongst those patients receiving audio analgesia. Only 1% of patients receiving audio analgesia reported a desire for analgesic injection if they were to undergo an additional EMG versus 27% of patients who did not receive audio analgesia.4 Limitations of this approach are potential 60Hz electrical interference and the need to insure a consistent ability of the patient to hear and follow instructions during the examination.
Hypnotic analgesia has been employed in numerous randomized controlled trials in an attempt to ameliorate pain and the anxiety associated with a wide variety of medical procedures. These studies have consistently demonstrated that treatments described as hypnosis, and those involving suggestion for focused attention are “at least as, and about half the time [even] more effective than other treatments for reducing pain associated the invasive medical procedures in both children and adults”.5 In spite of the success of hypnotic analgesia in a variety of clinical contexts, including its use for percutaneous vascular procedures,6 bone marrow aspirations,7 burn care,8 and labor pain,9 its use has not enjoyed mainstream integration. More recently hypnosis has been used manage pain and anxiety associated with colonoscopy 10 as well as breast cancer 11,12. Patterson and Jensen asserted that while [hypnotic analgesia] might be amenable to the predictable nature of procedural pain, whether the benefits it provides in terms of pain and anxiety reduction reported in the numerous trials would show themselves worth the time needed to train patients in their use remained to be determined.5
In 1977 Barber reported that by employing a short hypnotic induction technique known as rapid induction analgesia (RIA) lasting approximately 11–20 minutes and administered one time to patients undergoing various dental procedures, 99% were reported to complete those treatments with no requirement of chemical anesthetic.13 Additionally, Barber reported that the benefit of the one-time hypnotic intervention could be activated by a dentist via a post-hypnotic cue. The high percentage of responders in this study suggested that hypnotizability was not a key factor in determining efficacy of the treatment and that most people may benefit. Additionally, the fact that a dentist was able to induce the hypnotic state in patients after only one “practice” session suggested that the beneficial effects of hypnosis were not dependent upon the presence of a psychologist’s personal interaction with the patient. If true, the use of hypnosis would be much more cost-effective than it would be if therapists had to be present for all procedures. Finally, the short duration of the hypnotic intervention suggested that it is more likely to be used by patients and busy practitioners.
While the results of Barber’s case series were encouraging, this work did not represent a controlled trial. In a subsequent study, Gillet and Coe employed an audio program to administer either RIA or a shortened version. They reported a 52% success rate vs Barber’s 99% report. Both RIA and a shortened version were found to be equally effective.14 Hypnotic susceptibility [as measured by the Harvard Group Scale of Hypnotic Susceptibility],15 level did not relate significantly to successful hypnotic analgesia.
In the present study, we primarily sought to determine whether a single audio administration of a previously recorded hypnotic induction containing an embedded analgesic suggestion [hypnotic analgesia] would significantly reduce worst or average pain or anxiety associated with the EMG when compared with either a hypnotic induction without analgesic suggestion, or compared to an informational recording regarding the electrodiagnostic evaluation
We additionally tested three secondary hypotheses: (1) The effect of hypnosis is influenced by scores on a measure of absorption; (2) Randomization to hypnosis will result in less time required to complete an essentially standardized portion of the EMG; (3) Physician and patient perception of pain and anxiety will positively correlate.
METHODS
Subjects
Prospective subjects were identified from those individuals referred to the electrodiagnostic clinics at two major rehabilitation facilities located in an urban area of the northwest region of the United States, to rule out the diagnosis of either cervical or lumbosacral radiculopathy. Subjects were contacted via clinic staff as part of routine test scheduling and invited to participate if eligible. Inclusion criteria included: English speaking, able to listen to a twenty minute audio program, and answer four questionnaires to be described below. Patients were excluded if they had an impairment that rendered them insensate to nociceptive stimuli in the limb(s) to be evaluated by EMG. Studies were approved by the Institutional Review Board and participating subjects gave informed consent before randomization.
Randomization Process
Eligible subjects who agreed to participate met with clinic staff in the electrodiagnostic clinic on the day of their scheduled EMG, approximately 45 minutes prior to the EMG.
After obtaining informed consent, subjects were told that they may or may not receive hypnotic induction depending upon the randomization scheme. Research assistants administered the Tellegan Absorption Scale,16 and the Beck Anxiety Inventory® (Beck). Unfortunately, the brief amount of time that patients had to participate in this study did not allow for the administration of a measure of hypnotizability.
Subjects were randomized to one of the three treatment arms;
EDU: educational recording {standard care};
HYP-C hypnotic induction without analgesic suggestion {hypnotic control};
HYP-ANLG: hypnotic induction with analgesic suggestion {hypnotic analgesia},
Subjects were then escorted to a quiet room to listen to the audio program. The programs were administered by a research assistant blinded to the randomization scheme. Subjects heard the program one time just prior to the EMG. They were not told which arm of the study they were in.
Interventions
All three groups listened to an audio program (using CD player and headphones) that was approximately 20 minutes in duration. The standard care condition (EDU) was an audio version of the educational booklet provided to patients prior to an EMG. The two hypnotic conditions (HYP-C and HYP-ANLG) were based upon Barber’s 1977 hypnotic procedure for producing hypnotic analgesia. Within 20 minutes after the administration of the audio program, subjects underwent an appropriate electrodiagnostic evaluation depending upon their clinical presentation. Physicians were blinded to the randomization scheme. Both study subjects and physicians were advised not to discuss the audio program. Copies of these recordings may be obtained by contacting corresponding author.
Electrodiagnostic Examination
The electrodiagnostic procedures were performed by a total of seven physicians, all of whom were either experienced PGY-3 and or PGY-4 level Rehabilitation Medicine residents. Participating physicians were trained in appropriate needle EMG examination, and the evaluations were carried out in a standardized fashion. Needle examinations consisted of a 5 limb muscle plus 3 paraspinal muscle screening evaluation, or alternatively in subjects whom had prior cervical or lumbar surgical intervention, 8 limb muscles and no paraspinal muscles were tested. All needles used were standard Teflon coated 27 gauge monopolar needles. Prior to initiating the EMG, physicians administered a combined auditory and tactile cue in order to induce the hypnotic state. This combined cue consisted of asking the subject to “relax” while simultaneously placing a hand squarely on the subject’s forehead. Subsequently, physicians marked the start time [t0] upon placing the first needle through the skin. At the completion of the EMG, marked by removal of the last EMG needle, physicians marked time of study completion [tn]. Thus total time of the procedure was recorded.
Outcome Measures
After the procedure, subjects completed a 100 mm Visual Analog Scale [VAS] addressing worst pain, average pain, and anxiety during the EMG. Physicians also completed a VAS assessing the subjects, that included these three outcomes in parity with the subject VAS. Lastly, subjects completed 100 mm VAS scales assessing their degree of body perceptual change, mental images experienced, image vividness, sense of relaxation, sense of peace and calm, and ability to focus. These data were collected as both global outcomes of well being and for the purpose of assessing the credibility of the hypnotic control condition, though it is recognized that there may be considerable overlap in these measures and many of them may reflect relaxation.
Statistical Analysis
Prior to proceeding to the main analysis, we performed a reduction plot to assess for significant covariates on the ANOVA assumptions regarding baseline measurements of age, BAI® score, and Absorption score. The non-parametric Kuskal-Wallis test was applied to the three randomization arms on these baseline measures to assess for significant baseline group differences.
The primary comparison tool was the univariate ANOVA assessing group differences between standard care, hypnotic control, and hypnotic analgesia, on the main outcome measures of worst pain, average pain, anxiety, time to completion of the EMG, and experiential outcome measures as described previously.
A subsequent secondary analysis comparing a combined group entitled “Hypnosis” [HYP-C plus HYP-ANLG] versus “No Hypnosis” [EDU] was undertaken on the above main outcomes again employing the univariate ANOVA. This analysis was undertaken in an effort to decrease the likelihood of making a Type 2 error given our small sample size in each group.
Pearson Correlation coefficients were obtained to assess the linear relationship between physician and subject measures of worst pain, average pain, and anxiety.
The level of significance was set at α = 0.05. A power analysis performed a priori with a projected 40 subjects per group was calculated to provide a statistical power of 0.90, accepting a Cohen effect size of d = 0.74.17
Given the number of patients that ended up participating, we regarded the current study as a feasibility study rather than a test of the efficacy of hypnosis.
RESULTS
Twenty-six subjects were enrolled in and completed the study. Of those, 9 were females. Mean age was 53.6 years [sd: 11.7; Range: 30 – 78 years]. Four subjects had previously had an EMG study. Twenty subjects reported suffering from a chronically painful condition and of those, half used daily pain medication for that condition. All of the subjects who took daily analgesic or anxiolytic medications agreed to not change their medication schedule on the day of the study.
The mean BAI ® for the total sample population was 15.7 [range 1 – 46; S.D. +/− 11.6]. Eighteen subjects were in the low anxiety group [<21 cumulative score on the BAI®], six were in the moderate group [cumulative score 22–35] and two were in the high anxiety group [cumulative score >36]. The median score was 10 with 2nd and 3rd inter-quartiles being 6.5 and 19.5, thus the mean BAI® was skewed by 2 high outliers. The mean absorption score for the total sample population was 15.7 [range 0 – 32; S.D. +/− 11.6]. Fourteen subjects had low absorption [a cumulative score of < 20 on the Tellegan Absorption Scale], and n=12 had a high absorption [cumulative score > 20].
As shown in table 1, the analysis of the baseline variables demonstrated no significant covariates on the ANOVA assumptions between the three treatment arms with respect to age [p=0.666], BAI® score [p=0.280], or absorption score [p=0.328] Similarly, the Kruskal-Wallis non-parametric analysis of these same variables yielded non-significant results [p=0.717 for age, p=0.220 for BAI®, and p=0.255 for absorption]. Thus the analysis of the data was completed primarily with the univariate ANOVA.
TABLE 1.
ANOVA analysis of baseline measures
| Group Assignment | N | Age | Absorption Scale | BAI | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| Mean | SD | P | Mean | SD | P | Mean | SD | P | ||
| EDU | 8 | 51 | 6 | 0.66 | 14 | 6 | 0.27 | 16.75 | 13.39 | 0.33 |
| HYP-C | 10 | 56 | 15 | 20 | 9 | 18.8 | 12.66 | |||
| HYP-ANLG | 8 | 53 | 12 | 17 | 10 | 10.63 | 7.170 | |||
BAI, Beck Anxiety Inventory.
On the primary outcomes of worst pain, average pain, anxiety, and time to study completions are reported in Table 2. Both the HYP-C and HYP-ANLG groups reported less worst pain, average pain, and anxiety than did the EDU group, but these results were not statistically significant. Physicians reported similar amounts of time required to complete the EMG without statistically significant differences.
TABLE 2.
One Way ANOVA: Treatment Groups vs. Main Outcomes
| Outcome | Groups (n) | Mean | sd. | 95%CI | P | Fcalc | Fcrit |
|---|---|---|---|---|---|---|---|
|
| |||||||
| Worst Pain | EDU (8) | 67 | 25 | 17 | 0.128 | 2.244 | 3.422 |
| HYP-C (10) | 42 | 18 | 11 | ||||
| HYP-ANLG (8) | 49 | 30 | 21 | ||||
|
| |||||||
| Average Pain | EDU (8) | 35 | 26 | 18 | 0.552 | 0.611 | |
| HYP-C (10) | 27 | 14 | 8 | ||||
| HYP-ANLG (8) | 25 | 22 | 15 | ||||
|
| |||||||
| Anxiety | EDU (8) | 44 | 41 | 28 | 0.295 | 1.285 | |
| HYP-C (10) | 42 | 23 | 14 | ||||
| HYP-ANLG (8) | 22 | 24 | 17 | ||||
|
| |||||||
| Time | EDU (8) | 35 | 16 | 11 | 0.645 | 0.446 | |
| HYP-C (10) | 30 | 13 | 8 | ||||
| HYP-ANLG (8) | 33 | 10 | 7 | ||||
The Pearson correlation coefficients calculated for worst pain, average pain and anxiety are reported in Table 3. These data demonstrate a strong correlation between physician and subject report of worst pain (r=0.60). In contrast for reported average pain and anxiety during the EMG, the correlation while positive is weak at r = 0.31 and r = 0.30, respectively.
TABLE 3.
Physican & Patient Correlations on Worst Pain, Average Pain, and Anxiety.
| PHYSICIAN | ||||
|---|---|---|---|---|
| Worst Pain | Average Pain | Anxiety | ||
| PATIENT | Worst Pain | 0.60 | 0.42 | −0.1 |
| Average Pain | 0.30 | 0.31 | 0.08 | |
| Anxiety | 0.43 | 0.61 | 0.30 | |
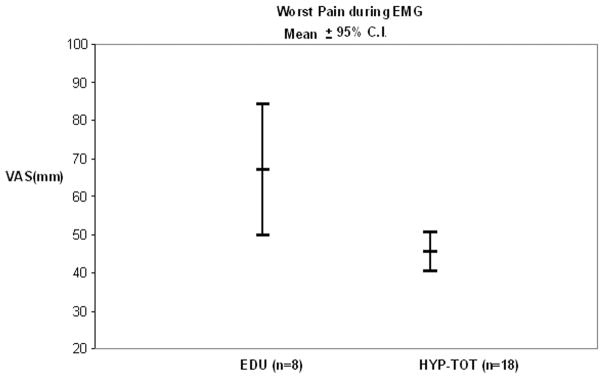
In the secondary analysis we combined the previously described hypnotic control [HYP-C, n=10] and the hypnotic analgesia group [HYP-ANLG, n=8] to form a new group entitled: HYP-TOT [n=18]. We compared the HYP-TOT group against the EDU group. In this instance mean worst pain during the EMG achieved statistical significance: [XHYP-TOT = 46 (C.I. +/− 5), X EDU = 67 (C.I. +/− 17), p=0.0495]. This data is represented in Table 4 and graphically in Figure 1. Additional outcomes of average pain and anxiety in the hypnosis group were consistently reported as less than control on the 100 mm VAS but the differences between groups did not achieve statistical significance.
TABLE 4.
One Way ANOVA: Hypnosis vs. No Hypnosis on Main Outcomes
| Outcome | Groups n=26 | Mean | Std. Dev. | 95%Confidence Interval | P- value | Fcalc | Fcrit |
|---|---|---|---|---|---|---|---|
|
| |||||||
| Worst Pain | HYP-TOT | 46 | 24 | 5 | 0.049 | 4.290 | 4.260 |
| EDU | 67 | 35 | 17 | ||||
|
| |||||||
| Average Pain | HYP-TOT | 26 | 18 | 8 | 0.277 | 1.233 | |
| EDU | 35 | 26 | 18 | ||||
|
| |||||||
| Anxiety | HYP-TOT | 33 | 25 | 15 | 0.432 | 0.637 | |
| EDU | 44 | 41 | 28 | ||||
|
| |||||||
| Time | HYP-TOT | 31 | 12 | 5 | 0.453 | 0.581 | |
| EDU | 35 | 16 | 11 | ||||
Figure 1.
Patient Rating of Worst Pain by Hypnosis vs. No Hypnosis
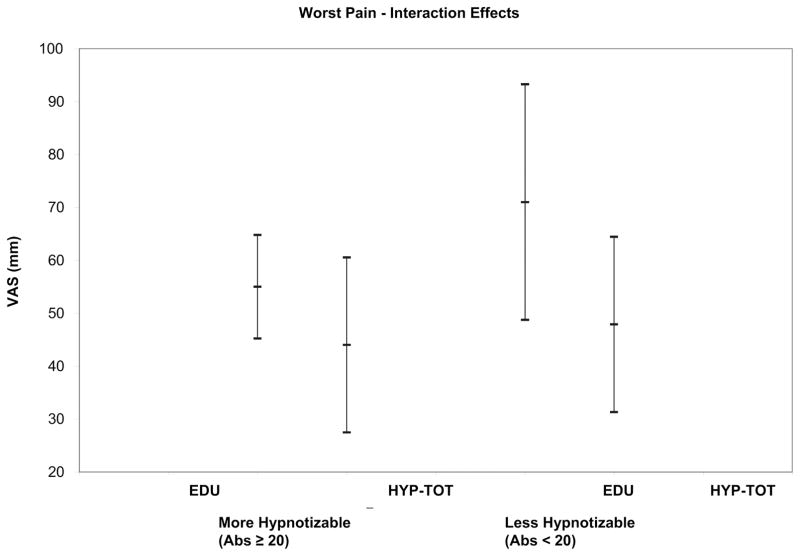
To explore a possible interaction effect between hypnosis and absorption, we divided the entire sample [n=26] into those individuals with absorption <20 [n=14] and those with absorption >20 [n=12]. In a study by Glisky et al, the mean population absorption on the dichotomous [true/false responses] summated version of the Tellegan Absorption Scale, is 20 with a S.D. +/− 6. Those individuals with absorption <20 were entitled “low absorption” and those with absorption >20 high absorption.
As shown in figure 2, the low absorption patients randomized to EDU [n=6] reported greater worst pain than those randomized to HYP-TOT [n=8]: [X EDU <20 = 71, (C.I. 22), X HYP-TOT <20 = 47 (C.I. +/− 17), p=0.13]. While the sample size is small and this result is not statistically significant, the difference between group means is large suggesting that even “low absorption patients” may benefit from hypnosis. Note that in the high absorption patients randomized to no hypnosis [n=2] versus those randomized to hypnosis [n=10], hypnosis appeared to provide a small benefit qualitatively; however, the low number of observations in the no hypnosis group [n=2] limits meaningful comparison. In table 5, the results of this absorption interaction analysis are further reported on the outcome measures of subject reported average pain and anxiety. No statistically significant values were noted in either example.
Figure 2.
Sub-group Analysis: Interaction Effects of Hypnosis and Absorption on Worst Pain
TABLE 5.
Interaction Effects of Hypnosis and Absorption
| Outcome | Groups n=26 |
Mean | Std. Dev. | 95% Confidence Interval | P- value | Fcalc | Fcrit |
|---|---|---|---|---|---|---|---|
|
| |||||||
| Worst Pain |
EDU Abs. <20; n=6 |
71 | 28 | 22 | 0.120 | 2.795 | 4.747 |
|
HYP-TOT Abs. <20; n=8 |
48 | 24 | 17 | ||||
|
|
|||||||
|
EDU Abs.≥20; n=10 |
55 | 7 | 10 | 0.565 | 0.354 | 4.965 | |
|
HYP-TOT Abs. ≥20; n=2 |
44 | 25 | 17 | ||||
| Outcome | Groups n=26 |
Mean | Std. Dev. | 95% Confidence Interval | P- value | Fcalc | Fcrit |
|---|---|---|---|---|---|---|---|
|
| |||||||
| Average Pain |
EDU Abs. <20;n=6 |
36 | 31 | 24 | 0.729 | 0.125 | 4.747 |
|
HYP-TOT Abs. <20; n=8 |
32 | 21 | 16 | ||||
|
|
|||||||
|
EDU Abs. ≥20; n=10 |
32 | 2 | 3 | 0.287 | 1.260 | 4.965 | |
|
HYP-TOT Abs. ≥20; n=2 |
21 | 13 | 8 | ||||
In the analysis of global experiential outcome measures, data was recorded after the subjects had completed the EMG in order to assess overall subject experience and the efficacy of the hypnotic control condition in terms of credibility. These measures were the experience of body change, mental image perception, vividness of image perception [if they occurred], sense of relaxation, sense of peace and calm, and a sense of focus. Table 6 demonstrates that the mean VAS scores for each of the experiential parameters were higher in the hypnosis group when compared to the non-hypnosis group. None achieved statistical significance; however, of the six outcomes “focus” demonstrated the largest difference on mean VAS. [X focus(HYP-TOT) = 53 (C.I. +/− 31) versus X focus(EDU) = 32 (C.I. +/− 35); p=0.117].
TABLE 6.
Interaction Effects of Hypnosis and Absorption; cont’d.
| Outcome | Groups n=26 |
Mean | Std. Dev. | 95% Confidence Interval | P- value | Fcalc | Fcrit |
|---|---|---|---|---|---|---|---|
|
| |||||||
| Anxiety |
EDU Abs. <20; n=6 |
45 | 41 | 33 | 0.715 | 0.140 | 4.747 |
|
HYP-TOT Abs. <20; n=8 |
51 | 24 | 17 | ||||
|
|
|||||||
|
EDU Abs. ≥20; n=10 |
40 | 57 | 78 | 0.221 | 1.486 | 4.965 | |
|
HYP-TOT Abs. ≥20; n=2 |
19 | 14 | 9 | ||||
In Table 7, the analysis of the experiential outcomes between HYP-C and HYP-ANLG are reported. There were no significant differences noted on any of the six experiential outcomes. Additionally, there were no trends noted wherein either HYP-C or HYP-ANLG demonstrated consistently higher mean VAS scores. For example, HYP-C mean scores were higher than HYP-ANLG with respect to: peace and calm, focus, and relaxation during the EMG. Conversely, HYP-ANLG mean scores were higher than HYP-C scores with respect to the experience of body change and image perception.
TABLE 7.
One way ANOVA of post-EMG experiential outcomes
| Outcome Variable | Condition | Mean | Std Dev | P value |
|---|---|---|---|---|
| HYP-TOT (n=18) | ||||
| No Hypnosis (n=8) | ||||
|
| ||||
| Body Changes | HYP-TOT | 41 | 30 | 0.688 |
| EDU | 31 | 29 | ||
|
| ||||
| Image perception | HYP-TOT | 32 | 28 | 0.668 |
| EDU | 27 | 21 | ||
|
| ||||
| Vividness of Images | HYP-TOT | 31 | 14 | 0.640 |
| EDU | 16 | 14 | ||
|
| ||||
| Relaxation | HYP-TOT | 55 | 30 | 0.773 |
| EDU | 37 | 29 | ||
|
| ||||
| Peace and Calm | HYP-TOT | 58 | 31 | 0.225 |
| EDU | 41 | 35 | ||
|
| ||||
| Focus | HYP-TOT | 53 | 31 | 0.117 |
| EDU | 32 | 35 | ||
DISCUSSION
Amongst adults undergoing electrodiagnostic evaluation for cervical or lumbosacral radiculopathy, a single recorded hypnotic induction compared with an educational audio recording showed some potential beneficial effects in terms of reducing patient report of worst pain during the needle portion of the examination. In addition, those in the hypnotic group showed a trend to report lower average pain and anxiety than did those randomized to an informational session.
There may be several reasons why a significant effect was not observed for other measures (average pain or anxiety) or why significant differences were not observed between the HYP-C and HYP-ANLG groups. First the sample sizes in each group were quite small. Second, while it is desirable to develop a minimal effect control condition in order to draw conclusions pertaining to the specific effect of hypnotic analgesia, there is the possibility that the hypnotic control may itself had measurable efficacy in reducing pain. As such, the differences in outcomes observed between two hypnotic interventions that differ only subtly may underestimate the overall effect of hypnosis in general.18 It is also possible that the effects noted were in part due to relaxation rather than hypnosis.
In addition, our study design employed only a single “dose” of hypnosis administered via an audio program on CD with headphones. Thus we purposefully had neither the direct involvement of the study psychologist [therapist] nor the opportunity for patient practice. Our audio approach is less common than direct therapist interaction, but is certainly not unprecedented. As previously described, Gillet and Coe used an audio version of Barber’s RIA with clear benefit to subjects undergoing various dental procedures.14 Additionally, Lang and colleagues in their study evaluating the efficacy of self-hypnotic relaxation during interventional radiological procedures found that hypnosis administered by mid-level care providers (as opposed to physicians or psychologists) relative to standard control resulted in less use of pain medication, less maximal pain, and improved physiologic stability during interventional radiologic procedures.6
A further example of using audio techniques in the context of hypnotic analgesia is provided by Harmon et al, who employed an audio technique for hypnosis with 60 women undergoing childbirth, and reported improved obstetric outcomes using hypnotic analgesia and skill mastery combined with childbirth education compared to a control condition. Specifically, Harmon and colleagues observed that audio-taped hypnotic induction relative to breathing and relaxation exercises [control] resulted in lower labor pain, shorter stage 1 labor, less pain medication use, children with higher Apgar scores at birth and five minutes, and a higher % of spontaneous deliveries.9 Although the women in Harmon’s study had more than one opportunity to practice the hypnosis [dose response], both conditions were audio-taped [just as in our study all three conditions were audio-recorded]. This suggests that therapist expectancy was decreased and we were therefore afforded the opportunity to see the real efficacy of the hypnosis.
In our study, we found that some patients with lower absorbtion scores benefited from hypnosis. Although this is of some theoretical interest, it is unfortunate that we not able to use a measure of hypnotizability, which would have been superior for the design of the study. Absorption has a low to moderate correlation with hypnotizability. There are several theories that address hypnotizability and effects of hypnotic analgesia. The trait theory of hypnosis espouses the view that hypnotizability [suggestibility] is related to the efficacy of observed hypnotic analgesia outcomes and that there is a great deal of variability and hence efficacy from one person to the next.19 Beyond the trait theory, there exist numerous theories regarding the mechanism(s) by which hypnotic analgesia works. Some of these include the social-cognitive model espoused by Chaves, which suggests that hypnotic induction leads to changes in cognition that in turn alter the affective states associated with pain.20 Other models beyond the scope of this discussion include the so-called neo-dissociative and dissociated control models.5 Thus, while the majority of studies indicate that hypnotizability is a factor in pain relief (cite Patterson and Jensen) the current study was consistent with some theoretical approaches that do not see this variable to be critical.
As mentioned above, the variable we measured was absorption rather than hypnotizability. We originally considered scales that while highly validated are also quite time consuming to perform, such as the Stanford Scale, 15 We ultimately settled upon the 34 item summated dichotomous version of the Tellegan Absorption Scale as a measure of hypnotizability16 which has been validated by Glisky and colleagues.21 In the Tellegan Absorption scale, a mean population score is thought to be 20 [S.D +/−6]. Individuals with absorption scores greater than twenty were predicted to be more amenable to hypnotic suggestion [highly hypnotizable], than those with scores less than 20 [low hypnotizable]. Lang, Gillet & Coe, and Barber, have reported that hypnotizability does not necessarily correlate with benefit of hypnosis; however, the majority of the literature supports a positive relationship.5
In our study, even those subjects with low absorption reported lower worst pain with hypnosis. While not a statistically significant difference, the effect size was essentially a 24% reduction in worst pain [Figure 2] and a 5% reduction in average pain [Table 6] amongst those individuals undergoing hypnotic induction.
Another limitation of our study is that subject blinding may have been inadequate. As such, it may have been difficult to control for expectancy.18 In our particular case however, direct interaction with a therapist was removed and as such presumably expectancy. Subjects undergoing the informational session likely knew they were not receiving a hypnotic intervention. It is also possible that sophisticated subjects may have been able to detect the analgesic suggestion in the hypnotic analgesia group. However, given that subjects were in the midst of the induction at the time the analgesic suggestion was made, identifying it as such seems unlikely [albeit not impossible]. Moreover, since the global experiential outcomes are similar in the HYP-C and HYP-ANLG groups, it is likely that the hypnosis conditions are equally credible and as such that adequate subject blinding was achieved.
That we noted a larger effect with worst pain compared to average pain and or anxiety supports the work of Lang et al who reported that during interventional radiologic procedures, compared to controls, test subjects used less analgesia [PCA] and reported less maximal but not average pain.6
With our limited sample we found only a small difference between the combined hypnosis group versus the no hypnosis group with a mean time to complete the EMG 31 minutes in the hypnosis group and 35 minutes in the standard care group [approximately 4 minutes less time to complete the EMG in the hypnosis group compared with control, p=0.453].
As noted previously, Gillet & Coe reported decreased time to complete dental procedures amongst those patients successfully utilizing Barber’s RIA, although they did not report the amount of time saved.14 In a follow up study by in 2000 Lang reported that amongst adults undergoing percutaneous vascular procedures, hypnosis provided pronounced effects on pain and anxiety reduction, improved hemodynamic stability and shorter procedure times. With respect to time, the mean hypnosis group procedure time was 61 vs 78 minutes in the standard group, p=0.0016.23 Whether that decrease in time required to complete their study completion translated into cost-effectiveness was addressed in a followup study by Lang and colleagues published in Radiology that concluded that adjunct hypnosis with sedation vs sedation alone reduced cost during interventional radiologic procedures, such that it cost $638 for standard sedation and $300 for sedation w/hypnosis (savings of $338/case).
We believe the use of an audio recording prior to an EMG is practical as it simply requires asking the patient to come about 30 minutes earlier to the appointment. Given the efficacy and practicality as well as the low risk of adverse effects, we believe that further study is warranted and that wider clinical use will likely be indicated.
Footnotes
Disclosures: This study was supported in part by grant R01 GM42725-09A1 from the National Institutes of Health.
References
- 1.Gans BM, Kraft GH. Pain perception in clinical electromyography. Arch Phys Med Rehabil. 1977;58:13–16. [PubMed] [Google Scholar]
- 2.Wee AS, et al. Pain perception to nerve conduction and needle electromyographic procedures. J Miss State Med Ass. 2004;45:327–30. [PubMed] [Google Scholar]
- 3.La Joie WI. Analgesia in Electromyography. Arch Phys Med Rehabil. 1963;44:42–44. [PubMed] [Google Scholar]
- 4.Spence WR, Guyton JD. Control of pain during electromyography. Arch Phys Med Rehabil. 1966;47:771–5. [PubMed] [Google Scholar]
- 5.Patterson DR, Jensen MP. Hypnosis and clinical pain. Psychol Bull. 2003;129:495–521. doi: 10.1037/0033-2909.129.4.495. [DOI] [PubMed] [Google Scholar]
- 6.Lang EV, et al. Self-hypnotic relaxation during interventional radiological procedures: Effects on pain perception and intravenous drug use. Int J Clin Exp Hyp. 1996;44:106–19. doi: 10.1080/00207149608416074. [DOI] [PubMed] [Google Scholar]
- 7.Katz ER, Kellerman J, Ellenberg L. Hyponsis in the Reduction of Acute Pain and Distress in Children with Cancer. J Pediatr Psychol. 1987;12:379–94. doi: 10.1093/jpepsy/12.3.379. [DOI] [PubMed] [Google Scholar]
- 8.Patterson DR, et al. Hypnosis for the treatment of burn pain. J Consult Clin Psych. 1992;60:713–17. doi: 10.1037//0022-006x.60.5.713. [DOI] [PubMed] [Google Scholar]
- 9.Harmon TM, Hynan MT, Tyre TE. Improved obstetric outcomes using hypnotic analgesia and skill mastery combined with childbirth education. J Consult Clin Psych. 1990;58:525–30. doi: 10.1037//0022-006x.58.5.525. [DOI] [PubMed] [Google Scholar]
- 10.Elkins GR, White J, Patel P. Hypnosis to manage anxiety and pain associated with colonoscopy for colorectal cancer screening: Case Studies and Possible Benefits. International Journal of Clinical and Experimental Hypnosis. 2006;54(4):416–431. doi: 10.1080/00207140600856780. [DOI] [PubMed] [Google Scholar]
- 11.Montgomery GH, Weltz CR, Seltz M, Bovbjerg DH. Brief presurgery hypnosis reduces distress and pain in excisional breast biopsy patients. International Journal of Clinical and Experimental Hypnosis. 2002;50(1):17–32. doi: 10.1080/00207140208410088. [DOI] [PubMed] [Google Scholar]
- 12.Montgomery GH, Weltz CR, Seltz M, Bovbjerg DH. Brief pre-surgery hypnosis reduces distress and pain in excisional breast biopsy patients. International Journal of Clinical and Experimental Hypnosis. 2002;50:17–32. doi: 10.1080/00207140208410088. [DOI] [PubMed] [Google Scholar]
- 13.Barber J. Rapid induction analgesia: A clinical report. Am J Clin Hypn. 1977;19:138–47. doi: 10.1080/00029157.1977.10403860. [DOI] [PubMed] [Google Scholar]
- 14.Gillett PL, Coe WC. The effects of rapid induction analgesia (RIA), hypnotic susceptibility and the severity of discomfort on reducing dental pain. Am J Clin Hypn. 1984;24:81–90. doi: 10.1080/00029157.1984.10402861. [DOI] [PubMed] [Google Scholar]
- 15.Morgan AH, Hilgard JR. The Stanford Hypnotic Clinical Scale for adults. Am J Clin Hypn. 1978–1979;21:134–147. doi: 10.1080/00029157.1978.10403968. [DOI] [PubMed] [Google Scholar]
- 16.Tellegen A, Atkinson G. Openness to absorbing and self-altering experiences (“Absorption”), a trait related to hypnotic susceptibility. J Abnorm Psychol. 1974;83:268–77. doi: 10.1037/h0036681. [DOI] [PubMed] [Google Scholar]
- 17.Montgomery GH, DuHamel KD, Redd WH. A meta-analysis of hypnotically induced analgesia. Int J Clin Exp Hyp. 2000;48:138–53. doi: 10.1080/00207140008410045. [DOI] [PubMed] [Google Scholar]
- 18.Jensen MP, Patterson DR. Control conditions in hypnotic analgesia clinical trials: Challenges and recommendations. Int J Clin Exp Hyp. 2005;53:130–39. doi: 10.1080/00207140590927536. [DOI] [PubMed] [Google Scholar]
- 19.Hilgard ER, Margan AH. Heart rate and blood pressure in the study of laboratory pain in man under normal conditions and as influenced by hypnosis. Acta Neurobiol Exp. 1975;35:741–59. [PubMed] [Google Scholar]
- 20.Chaves CF. Recent advances in the application of hypnosis to pain management. Am J Clin Hypn. 1994;37:117–29. doi: 10.1080/00029157.1994.10403124. [DOI] [PubMed] [Google Scholar]
- 21.Glisky ML, et al. Absorption, openness to experience, and hypnotizability. J Pers Soc Psychol. 1991;60:263–72. doi: 10.1037//0022-3514.60.2.263. [DOI] [PubMed] [Google Scholar]
- 22.Butler LD, et al. Hypnosis reduces distress and duration of an invasive medical procedure for children. Pediatrics. 2005;115:77–85. doi: 10.1542/peds.2004-0818. [DOI] [PubMed] [Google Scholar]
- 23.Lang EV, et al. Adjunctive non-pharmacological analgesia for invasive medical procedures:a randomized trial. Lancet. 2000;355:1486–90. doi: 10.1016/S0140-6736(00)02162-0. [DOI] [PubMed] [Google Scholar]