Abstract
Background
Sexual health is an important area of study—particularly for minority youth and youth living in disadvantaged neighborhoods.
Objectives
The purpose of the research was to examine the sources of sexual health information associated with youth adopting sexual risk reduction behaviors.
Methods
Data collection took place in a small city in the Northeastern United States using cross-sectional behavioral surveys and modified venue-based sampling. Participants included 249 African-American and Latino/a youth aged 13–24. Participants reported their sources of information about contraception and human immunodeficiency virus (HIV)/sexually transmitted disease (STD), such as TV/movies, parents, social media; their intentions to have sex; and condom and contraception use during their last sexual activity. Social media use, past pregnancy experience, past sexual history, age, and gender were also measured. Standard tests of bivariate association (chi-squared and F-tests) were used to examine initial associations between sexual risk reduction behavior and exposure to sexual risk reduction information on social media. Logistic regression models were used to test multivariate relationships between information sources and sexual risk reduction behavior.
Results
Youth who were exposed to sexual health messages on social media were 2.69 times (p < .05) and 2.49 times (p < .08) more likely to have used contraception or a condom at last intercourse, respectively. Parents, schools, or traditional media as information sources were not significantly associated with contractive use or condom use at last intercourse.
Discussion
Youth sexual behavior is increasingly informed by social media messages. Health practitioners should utilize social media as an important health promotion tool.
Keywords: adolescent, African American, contraception, Latino, sexual behavior, social media, youth
Sexual health remains a high priority area for youth in the United States. Youth aged 13–24 accounted for 22% of all new human immunodeficiency virus (HIV) cases and half of all new sexually transmitted diseases (STD) in 2014 (Centers for Disease Control [CDC], 2014). Unintended teenage pregnancies also pose an additional public health concern, especially since early parenthood is associated with long-term, economic disadvantage (Huang, Costeines, Ayala, & Kaufman, 2014; Gibb, Fergusson, Horwood, & Boden, 2015). According to the 2015 CDC national Youth Risk Behavior Survey (n.d.), 20.0% of sexually active Latino/a youth and 15.9% of African-American youth did not use any method of contraception during their most recent sexual intercourse. It is therefore important for researchers and healthcare professionals to engage the broader social context of sexual communication that occurs, including online communications, to address these persistent, negative, sexual health outcomes and risks among minority youth (Widman, Choukas-Bradley, Helms, Golin, & Prinstein, 2014). An emerging field of study is currently addressing these issues—specifically examining the influence of digital neighborhoods or online communities (e.g., social media use) on sexual health and sexual risk reduction behaviors (Buhi, Klinkenberger, Hughes, Blunt, & Rietmeijer, 2013; Jones, Eathington, Baldwin, & Sipsma, 2014; Stevens, Dunaev, Malven, Bleakley, & Hull, 2016; Stevens, Gilliard-Matthews, Dunaev, Woods, & Brawner, 2016).
Social Media Use
The use of social media among teens has increased dramatically—from 55% in 2006 to 76% in 2015 (Lenhart, 2015)—changing how information is transmitted to and among youth. Regardless of race/ethnicity, education, or economic status, youth demonstrate rapid uptake of social media (Pew Research Center, 2017; Ralph, Berglas, Schwartz, & Brindis, 2011), with their underlying goal being to connect with peers via these new technologies (Boyd, 2014). With the low-cost and wide-reaching potential for information transmission, social media may be a unique medium for communicating sexual health information to high-risk populations.
Very few social media interventions are reported in the scientific literature; therefore, it is largely unknown to what extent, or to what effect, social media is being used for sexual health promotion. In a systematic review, Gold et al. (2011) found that the use of social networking sites to share sexual health information was not widespread. The information that existed was primarily based in the U.S. (70.8%) and consisted of sites used to establish the presence of an organization (62.9%), promote campaigns or interventions (28.7%), and connect individuals (5.6%; Gold et al., 2011). The authors also reported that approximately 29.6% of this information explicitly targeted youth (Gold et al., 2011). Studies also report nurses and other health professionals are utilizing social media to a greater extent for general health promotion (Farmer, Bruckner Holt, Cook, & Hearing, 2009). Some examples of these uses include creating health-related support communities, sharing health and disease information, and hosting online health communication interventions (Moorhead et al., 2013). Further research is needed; however, to assess the potential efficacy of these social media strategies and identify best practices specific to online sexual health promotion.
A potential barrier to reaching youth online with sexual health information is privacy (Divecha, Divney, Ickovics, & Kershaw, 2012; Ralph et al., 2011). Previous research has found that teens are wary of learning about and sharing sexual health information via online platforms and prefer to learn about sexual health topics from healthcare professionals, family members, and friends (Bleakley, Hennessy, Fishbein, & Jordan, 2009; Divecha et al., 2012; Jones & Biddlecom, 2011). However, as social media has evolved, sharing personal information (e.g., photos, videos, birthdates, real names) online has become increasingly normative (Boyd, 2014; Madden, Lenhart, Duggan, Cortesi, & Gasser, 2013). It is therefore important to understand how these evolving platforms, and the information being shared on them, impacts adolescent sexual attitudes and behaviors.
Media Exposure and Sexual Behavior
Adolescent exposure to sexual content in the media has been linked to early sexual initiation, risky sexual behavior (Bleakley, Hennessy, Fishbein, & Jordan, 2008; Bleakley et al., 2009; O’Hara, Gibbons, Gerrard, Li, & Sargent, 2012), and sexual victimization, including intimidation and rape (Ybarra, Strasburger, & Mitchell, 2014). Although sexual media exposure predicts the broadening of sexual engagement among youth, baseline sexual activity also predicts sexual media exposure, illustrating a recursive relationship (Bleakley et al., 2008). Merely focusing on how exposure affects behavior ignores the complex dynamic that requires scholars to treat exposure tendencies as behaviors themselves (Bleakley et al., 2008). This may be particularly true in the case of sexual health information exposure on the Internet, considering the information is more likely to be intentionally sought.
Compared to traditional forms of media (e.g., television, movies, and music), youth report much less sexual content being depicted on the websites they visit (Ybarra et al., 2014). Further, youth who report learning about sex from the Internet demonstrate increased self-efficacy (i.e., belief in one’s ability to have sex) and a belief that having sex will lead to positive outcomes. The same study also found that friends who serve as sources of information about sex have a similar influence on self-efficacy and expectancies, suggesting that online sources convey authority similar to that of peers (Bleakley et al., 2008). Additionally, research conducted after the surge in social media uptake suggests that youth who are more willing to share sexual health information using social media have greater self-efficacy beliefs for condom usage as well as knowledge of risk factors for HIV/STDs (Divecha et al., 2012). These findings demonstrate that adolescents use social media to find and distribute sexual risk-reduction information and highlight the need for further investigation into these practices.
Previous research on youths’ social media use has largely been conducted with college students, most of whom did not belong to a racial or ethnic minority group. Additionally, social media research on sexual health remains in its formative stages, with a majority of published work utilizing qualitative methods (Selkie, Benson, & Moreno, 2011). This study contributes to the literature through its use of survey methods to examine the relationship between social media use and sexual risk-reduction behaviors among African-American and Latino/a youth living in disadvantaged neighborhoods. This study sought to answer several research questions, specifically: What does social media use look like among African-American and Latino youth living in low-income neighborhoods? Where are youth exposed to sexual health messages specifically related to HIV, STDs, and pregnancy prevention? What sources of sexual health information are associated with higher future intentions to have sex? Where do youth who are practicing safer sex hear about birth control and condoms? This study is an initial step in assessing social media as an influential source of sexual risk reduction information.
Theoretical Framework
This study was informed by the Integrative Model of Behavior Change (IMBC), which combines theoretical constructs from social cognitive theory and the theories of Reasoned Action and Planned Behavior (Fishbein & Yzer, 2003). This framework was used to systemically examine social media as a correlate of sexual behavior (Fishbein & Yzer, 2003). According to this model, engagement in sexual risk reduction behaviors is a function of attitudes toward the behavior, normative perceptions about the behavior, perceived self-efficacy over the behavior, and resultant intentions to engage in the behavior. The model further articulates that although attitudes, norms, and efficacy should influence intentions to perform a behavior, the relationship between intentions and behavior is constrained by the extent to which environmental barriers and facilitators intervene. That is, intention should be a strong predictor of behavior, but only to the extent that an individual has the abilities and knowledge to perform the behavior and the environmental constraints are not excessive. The IMBC includes media exposure as a predictor of behavior. This study focuses on the pathways between media exposure to intention and behavior.
Purpose
This study examines the sources of sexual risk-reduction information among sexually active youth and which sources are associated with sexual risk-reduction behaviors. This study explicitly tests whether social media is an influential source of sexual risk-reduction information.
Methods
Setting
Participants in this study resided in the Northeast region of the U.S. in a small city with a population that was approximately 77,000 in 2011. City residents’ racial distributions were 48% African American, 47% Latino/a, and 5% White/other. The median household income in 2010 was approximately $27,000, with 36% of the population living below the federal poverty line. Relative to other neighborhoods in the state, this inner city had a relatively young demographic profile with 32% of the population younger than 18 years of age. The city also has multiple other risk factors including high childhood poverty rates (19%), high unemployment rates (11%), a large subset of single-parent households (37%), and low high school graduation rates (66%). Additionally, it is typically characterized as one of the most dangerous cities in the U.S. with 2,448 violent crimes for every 100,000 residents in 2010 (U.S. Census Bureau, 2010).
Procedures
The Institutional Review Board at Rutgers University approved this study and procedures. Data for this study are drawn from surveys with African-American and Latino/a youth living in a Northeast U.S. city and collected from June 2013–February 2014. This data is part of a larger mixed-methods study conducted to examine how youth negotiate risk-taking behavior within the context of high crime, high poverty neighborhoods. This study began with 60 qualitative interviews with youth, and findings based on those interviews have been published (Stevens, Gilliard-Matthews, Dunaev, Woods, & Brawner, 2016; Stevens, Gilliard-Matthews, Nilsen, Malven, & Dunaev, 2014; Gilliard-Matthews, Stevens, Nilsen, & Dunaev, 2015). The findings from those interviews also informed the development of the surveys used in this study.
Researchers visited eight community-based, nonprofit organizations to administer surveys onsite to participants at their convenience and based on their availability. Other surveys were administered on the investigators’ college campus for youth who were not being served by community-based, nonprofit organizations. Prior to survey administration, youth were given an identification number to correspond to their answers, and ensure privacy and confidentiality. Survey responses were collected using a computerized self-assisted interview (CASI) method via netbooks using Medialab software. Responses were recorded onsite and then uploaded to a secure server once data were collected. CASI methods increase reliability of self-report data and provide increased privacy, particularly when collecting sexual health data among adolescents (Turner et al., 1998). Researchers oriented participants to the process of completing the survey and assigned each individual a netbook to input his or her responses. The surveys took 45–60 minutes to complete. In addition to sociodemographic information, participants answered questions broadly involving neighborhood assessment, personal health, alcohol and drug use, family relationships, violence, digital life (i.e., most frequented social media sites and duration of time spent online), and goals and aspirations. While youth were encouraged to answer every question, they were also informed that they could refuse to answer any questions or withdraw from the study without penalty. No participants withdrew from the study.
Sample
To be included in the study, youth had to meet the following criteria: self-identify as African-American and/or Latino/a; aged 13–24; able to read and write in English; and reside in the targeted Northeast U.S. city. The study followed human subject protection procedures. Parental consent and youth assent forms were required for all participants younger than 18 years of age, while participants 18 years of age and older provided their own consent. Participants were compensated $25 in cash for their time.
Participants were recruited using a modified, venue-based, sampling technique. Research team members spent several months scouting and frequenting locations visited by youth throughout the city to identify and quantify potential locations. These community-based, nonprofit organizations included places like the Boys and Girls Clubs, after-school programs, and adolescent outreach initiatives. Relationships were established with these sites and fliers were distributed throughout specific neighborhood areas to reach the targeted population. The percentage of youth who viewed the recruitment flyers and opted to participate is not known, nor is the number of youth who wanted to participate but were unable to obtain parental consent known.
Measures
Social media use
Social media use was measured with the item: “About how often do you use social media?” Response categories were: several times a day; about once a day; three to five days a week; one to two days a week, every few weeks, less often, and I don’t use social media. This was recoded to the following five categories for clarity: 1 = more than once a day;2 = about once a day; 3 = several times a week; 4 = every few weeks; and 0 = I don’t use social media. Youth were also asked to identify their favorite social media site from a list of popular sites (e.g., Facebook, Instagram, Twitter, ooVoo, Kik); they could also list their favorite sites not included on the list.
Sources of sexual risk reduction information
Contraception information sources were measured with the question: “In the past 30 days, where have you heard about pregnancy prevention among young people?” HIV/STD information sources were measured similarly with the following item: “In the past 30 days, where have you heard about HIV or STDs?” For both items, participants could choose multiple responses from the following options: TV/movies, magazines, billboards/ posters, school, friends, music/music videos, parents/guardians, word of mouth/neighborhood gossip, social networking sites. Each response option was coded yes or no.
Previous sexual intercourse
Previous sexual intercourse was measured with a yes-or-no item: “Have you ever had sexual intercourse?” (CDC, n.d.)
Pregnancy experiences
Pregnancy history was measured with the item: “How many times have you been or gotten someone pregnant?” Response options included: 0 = never, 1 = one time, 2 = two or more times, or 0 = not sure. Never and not sure were collapsed into one category.
Sexual intentions
Sexual intentions were measured using the mean score of two items: “I will have sex in the next six months” and “I intend to have sex in the next six months.” Responses were measured using a Likert scale ranging from 1 = strongly disagree) to 5 = strongly agree. Cronbach’s alpha for these two items was 0.95.
Condom use
Condom use was measured with the yes or no item: “The last time you had sexual intercourse, did you or your partner use a condom?” (CDC, n.d.).
Contraception use
Contraception use was measured with the item: “The last time you had sexual intercourse, what one method did you or your partner use to prevent pregnancy? (select only one response)” The response options were: I have never had sexual intercourse; No method was used to prevent pregnancy; Birth control pills; Condoms; An IUD (such as Mirena or ParaGard) or implant (such as Implanon or Nexplanon); A shot (such as Depo-Provera); Patch (such as Ortho Evra) or birth control ring (such as NuvaRing); Withdrawal or some other method; or Not sure (CDC, n.d.). Contraception use was recoded into a binary variable where those who reported using either a hormonal form of birth control or a condom were coded as users. Respondents who answered that “no method” was used, they were not sure of the method, or that the withdraw method was used were coded as nonusers. Youth who were not sexually active were exempted from the condom use and contraception use items.
Neighborhood quality
Neighborhood quality was assessed using three items: “How safe from crime do you consider your neighborhood to be?” (response options ranged from 1 = not safe at all to 4 = extremely safe; “Overall, how would you rate your neighborhood as a place to live?” (response options ranged from 1 = poor) to 4 = excellent); and “How do you think your neighborhood compares to other neighborhoods in the area?” (response options ranged from 1 = much worse to 4 = much better). A composite score was created by averaging these three items, with higher scores indicating higher quality neighborhoods. Cronbach’s alpha for this scale was 0.75.
Demographics
Participants reported on their age, gender, and race/ethnicity.
Statistical Analyses
Stata v.13 (StataCorp LP, College Station, TX) was used to conduct statistical analyses. F-tests and t-tests were used to test bivariate associations. Logistic regression and multiple regression models were used for multivariate analyses. Regression diagnostics were conducted to ensure regression assumptions were met for the models. All models met the appropriate regression assumptions (e.g., normally distributed residuals, multicollinearity, etc.). All sexually active youth were included in the regression models. This approach leads to a more conservative estimate of effects from any of the sources as it includes null effects from youth who were not exposed to a particular source.
Results
Participant Characteristics
Participant characteristics are shown in Table 1. The majority of the sample was female (n = 152; 60.6%), with a mean age of 18.2 (SD = 3.2). As shown in Table 1, 70.3% (n = 175) of the sample had had sexual intercourse, and 43.4% (n = 109) had been pregnant or impregnated their sexual partner. In terms of sexual risk reduction behaviors, a large percentage of the sexually active youth (58.2%; n = 102) reported using a condom during their last sexual intercourse. Further, 69.1% (n = 121) of the sexually active participants in the sample used some form of contraception (including condoms) at their last sexual intercourse. There were some inconsistencies between the responses to the two questions. Specifically, 10 youth reported not using birth control, but reported condom use at last sex. Overall, condom and contraception use reported in the sample is consistent with Youth Risk Behavior Survey (YRBS) estimates, although this sample is older than the YRBS population (CDC, n.d.).
TABLE 1.
Participant Characteristics
| Characteristic | M | (SD) |
|---|---|---|
| Age | 18.2 | (3.2) |
| Neighborhood quality (score) | 2.3 | (0.7) |
| Sexual Intention Score | 3.1 | (1.4) |
|
|
||
| Gender | n | (%) |
|
|
||
| Female | 151 | (60.6) |
| Male | 98 | (39.4) |
| Ever had sex (yes) | 175 | (70.3) |
| Pregnancies | ||
| 0 | 140 | (56.6) |
| 1 | 63 | (25.1) |
| ≥2 | 46 | (18.3) |
| Contraception use (yes) | 121 | (48.6) |
| Condom use (yes) | 102 | (41.0) |
| Sources: contraception | ||
| TV/movies | 157 | (63.1) |
| Magazines | 97 | (39.0) |
| Billboards/posters | 55 | (22.1) |
| School | 139 | (55.8) |
| Friends | 104 | (41.8) |
| Music/music videos | 33 | (13.3) |
| Parents/guardians | 119 | (47.8) |
| Word of mouth/gossip | 67 | (26.9) |
| Social media | 117 | (47.0) |
| Sources: HIV/STD prevention | ||
| TV/movies | 158 | (63.5) |
| Magazines | 98 | (39.4) |
| Billboards/posters | 67 | (26.9) |
| School | 140 | (56.2) |
| Friends | 101 | (40.6) |
| Music/music videos | 47 | (18.9) |
| Parents/guardians | 116 | (46.6) |
| Word of mouth/gossip | 73 | (29.3) |
| Social media | 111 | (44.6) |
Note. N = 249. HIV = human immunodeficiency virus; STD = sexually transmitted diseases.
Participants varied greatly on the frequency of their social media usage, with 8.8% (n = 22) reporting not using social media at all; 5.6% (n = 14) every few weeks; 10.9% (n = 27) weekly; 17.3% (n = 43) daily; and 57.0% (n = 142) multiple times each day. Similar to most estimates of social media use by youth, social media use among this sample of youth is high (Lenhart, 2015). The most commonly used social media sites at the time of this study were Facebook (64.4%), Instagram (18.7%), and Twitter (5.5%). Participants also reported using other sites, including Vine and Snapchat (11%). There were no statistically significant differences in social media preferences or usage frequency by age or gender.
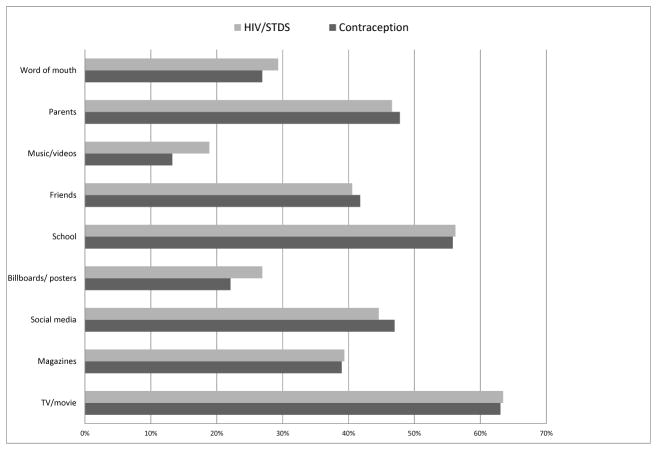
Sources of Sexual Risk-Reduction Information
As shown in Figure 1, there were similar exposure levels by source for contraception information and HIV/STD prevention information. The most common sources of sexual risk- reduction information reported were television and movies (63%; n = 157), school (56%; n = 140), and parents (47–48%; n = 117–120). Social media served as the fourth most commonly cited source of sexual risk reduction information, with slightly less than half of the sample reporting it as a source of recent sexual risk-reduction information (45–47%; n = 112–117). This finding is more notable considering 8.8% (n = 22) of the sample reported not using social media at all. Further, communication on social media could easily include information shared by friends or parents. There were also no significant differences between parents and social media as information sources. Although there appears to be differences in exposure to messaging on billboards/posters and music videos, independent sample t-tests reveal these differences are not statistically significant.
FIGURE 1.
Recent sources of contraception and HIV/STD information (N = 249).
Table 2 depicts sample characteristics and sources of sexual risk-reduction information stratified by participant sexual risk-reduction behavioral profile. Participants were separated into contraception users and nonusers during last sex and condom users and nonusers. Word of mouth and social media appear to serve as important sources of contraception information among those who reported using contraception at last sex. However, high percentages of nonusers also reported getting information from these sources. There were no statistically significant gender differences for any of the categories.
TABLE 2.
Contraceptive and Condom Use Among Sexually Active Youth by Characteristic
| Characteristic | Contraceptive usea (n = 175)
|
Condom usea (n = 172)
|
||||||
|---|---|---|---|---|---|---|---|---|
| Yes (n = 121)
|
No (n = 54)
|
Yes (n = 102)
|
No (n = 70)
|
|||||
| M | (SD) | M | (SD) | M | (SD) | M | (SD) | |
| Age | 19.4 | (2.8) | 19.6 | (2.5) | 19.1 | (2.6) | 19.9 | (2.8) |
| Neighborhood quality (score) | 2.3 | (0.7) | 1.9 | (0.7) | 2.3 | (0.7) | 2.0 | (0.7) |
| Sexual Intention Score | 3.6 | (1.2) | 3.6 | (1.2) | 3.6 | (1.2) | 3.6 | (1.1) |
|
|
|
|
|
|||||
| Gender | n | (%) | n | (%) | n | (%) | n | (%) |
|
|
|
|
|
|||||
| Female | 74 | (61.2) | 31 | (57.4) | 59 | (57.8) | 44 | (62.9) |
| Male | 47 | (38.8) | 23 | (42.6) | 43 | (42.2) | 26 | (37.1) |
| Ever had sex (yes) | 121 | (100.0) | 54 | (100.0) | 102 | (100.0) | 70 | (100.0) |
| Pregnancies | ||||||||
| 0 | 74 | (61.2) | 25 | (46.3) | 69 | (67.6) | 29 | (41.4) |
| 1 | 30 | (24.8) | 14 | (25.9) | 22 | (21.6) | 20 | (28.6) |
| ≥2 | 17 | (14.0) | 15 | (27.8) | 11 | (10.8) | 21 | (30.0) |
| Contraception use (yes) | 121 | (100.0) | 54 | (100.0) | 92 | (90.2) | 27 | (38.6) |
| Condom use (yes) | 94 | (77.3) | 10 | (18.9) | 102 | (100.0) | 70 | (100.0) |
| Sources: contraception | ||||||||
| TV/movies | 79 | (65.3) | 29 | (53.7) | 64 | (62.7) | 43 | (61.4) |
| Magazines | 54 | (44.6) | 19 | (35.2) | 42 | (41.2) | 29 | (41.4) |
| Billboards/posters | 33 | (27.3) | 11 | (20.4) | 26 | (25.5) | 17 | (24.3) |
| School | 64 | (52.9) | 23 | (42.6) | 53 | (52.0) | 32 | (45.7) |
| Friends | 51 | (42.1) | 17 | (31.5) | 42 | (41.2) | 25 | (35.7) |
| Music/music videos | 19 | (15.7) | 5 | (9.3) | 17 | (16.7) | 6 | (8.6) |
| Parents/guardians | 66 | (54.5) | 20 | (37.0) | 53 | (52.0) | 32 | (45.7) |
| Word of mouth/gossip | 41 | (33.9) | 7 | (13.0) | 35 | (34.3) | 12 | (17.1) |
| Social media | 65 | (53.7) | 15 | (27.8) | 55 | (53.9) | 24 | (34.3) |
| Sources: HIV/STD prevention | ||||||||
| TV/movies | 85 | (70.2) | 34 | (63.0) | 71 | (69.6) | 47 | (67.1) |
| Magazines | 59 | (48.8) | 21 | (38.9) | 50 | (49.0) | 29 | (41.4) |
| Billboards/posters | 40 | (33.1) | 15 | (27.8) | 33 | (32.4) | 21 | (30.0) |
| School | 66 | (54.5) | 27 | (50.0) | 55 | (53.9) | 36 | (51.4) |
| Friends | 59 | (48.8) | 19 | (35.2) | 47 | (46.1) | 29 | (41.4) |
| Music/music videos | 29 | (24.0) | 10 | (18.5) | 24 | (23.5) | 14 | (20.0) |
| Parents/guardians | 68 | (56.2) | 22 | (40.7) | 61 | (59.8) | 28 | (40.0) |
| Word of mouth/gossip | 42 | (34.7) | 16 | (29.6) | 34 | (33.3) | 23 | (32.9) |
| Social media | 65 | (53.7) | 24 | (44.4) | 56 | (54.9) | 32 | (45.7) |
Note. None of the associations between characteristics or information sources with contraceptive or condom use were significant (p < .05). HIV = human immunodeficiency virus; STD = sexually transmitted diseases.
Use at last sexual experience among sexually active respondents.
Intention to Have Sex
Displayed in Table 3, a simultaneous, multiple-regression model was used to assess the effects of health information sources, previous sexual intercourse, age, gender, and neighborhood quality on intentions to have sex. Results indicate that previous sexual intercourse is by far the best predictor of future intentions to have sex, as is standard in the literature. Gender and age were also significant predictors, with males and older adolescents reporting significantly higher intentions to have sex. No sources of pregnancy prevention information were significantly associated with youth intentions to have sex. The only information sources associated with sexual intentions were HIV/STD prevention information from school and magazines. Both magazines and school were significantly negatively associated with intentions to have sex.
TABLE 3.
Sexual Risk Reduction Information Sources and Intentions to Have Sex: Regression Model
| Predictor | b | (SE) | b* | p |
|---|---|---|---|---|
| Contraception source | ||||
| TV/movie | 0.20 | (0.14) | 0.09 | .15 |
| Magazines | −0.04 | (0.13) | −0.02 | .74 |
| Billboards/posters | 0.09 | (0.15) | 0.04 | .54 |
| School | 0.10 | (0.13) | 0.05 | .47 |
| Friends | 0.10 | (0.13) | 0.05 | .45 |
| Music/music videos | −0.15 | (0.20) | −0.05 | .47 |
| Parents/guardians | −0.06 | (0.13) | −0.03 | .64 |
| Word of mouth/gossip | 0.03 | (0.14) | 0.01 | .82 |
| Social media | −0.14 | (0.14) | −0.06 | .32 |
| HIV/STD prevention source | ||||
| TV/movie | −0.22 | (0.14) | −0.10 | .13 |
| Magazines | −0.33 | (0.15) | −0.15 | .03 |
| Billboards/posters | 0.07 | (0.17) | 0.03 | .70 |
| School | −0.23 | (0.13) | −0.11 | .04 |
| Friends | 0.15 | (0.14) | 0.07 | .30 |
| Music/music videos | 0.20 | (0.20) | 0.08 | .30 |
| Parents/guardians | 0.25 | (0.15) | 0.12 | .09 |
| Word of mouth/gossip | −0.01 | (0.15) | −.003 | .97 |
| Social media | 0.04 | (0.14) | 0.02 | .78 |
| Gendera | 0.49 | (0.11) | 0.23 | <.001 |
| Age | 0.09 | (0.02) | 0.28 | <.001 |
| Neighborhood quality | −0.12 | (0.08) | −0.08 | .15 |
| Ever had sexb | −0.94 | (0.15) | −0.41 | <.001 |
| Constant | 0.79 | (0.60) | .19 | |
Note. N = 249. Adjusted R2 = .45 (p < .001). HIV = human immunodeficiency virus. STD = sexually-transmitted disease.
Female = 1; male = 0.
No = 0; yes = 1.
Condom and Contraception Use
Table 4 displays the results from two logistic regression models testing the associations between sexual health information sources and condom and contraception use. Model 1 presents the predictors of contraception use (including condoms) and Model 2 presents the predictors of condom use alone. Model 2 includes information sources for both contraception and HIV/STDs as either type of prevention message could plausibly recommend increased condom use.
TABLE 4.
Contraceptive and Condom Use Among Sexually Active Youth: Logistic Regression Models
| Predictor | Contraception use(n = 175)
|
Condom use(n = 172)
|
||||
|---|---|---|---|---|---|---|
| OR | (SE) | p | OR | (SE) | p | |
| Pregnant oncea | 0.78 | (0.40) | .63 | 0.38 | (0.18) | .04 |
| Pregnant more than oncea | 0.35 | (0.20) | .06 | 0.19 | (0.11) | .005 |
| Contraception source | ||||||
| TV/movie | 0.74 | (0.35) | .52 | 0.59 | (0.32) | .34 |
| Magazines | 1.23 | (0.62) | .68 | 0.79 | (0.41) | .65 |
| Billboards/posters | 0.99 | (0.51) | .98 | 0.65 | (0.36) | .44 |
| School | 0.96 | (0.45) | .93 | 1.16 | (0.59) | .77 |
| Friends | 0.74 | (0.37) | .55 | 0.78 | (0.39) | .62 |
| Music/music videos | 0.49 | (0.37) | .34 | 2.84 | (2.34) | .20 |
| Parents/guardians | 1.95 | (0.88) | .14 | 0.67 | (0.32) | .40 |
| Word of mouth/gossip | 4.06 | (2.22) | .01 | 3.59 | (2.01) | .02 |
| Social media | 2.69 | (1.34) | .05 | 2.49 | (1.28) | .08 |
| HIV/STD prevention source | ||||||
| TV/movie | 0.88 | (0.50) | .83 | |||
| Magazines | 0.87 | (0.49) | .81 | |||
| Billboards/posters | 0.87 | (0.57) | .84 | |||
| School | 0.54 | (0.28) | .24 | |||
| Friends | 1.31 | (0.69) | .61 | |||
| Music/music videos | 0.86 | (0.67) | .84 | |||
| Parents/guardians | 4.06 | (2.23) | .01 | |||
| Word of mouth/gossip | 0.49 | (0.28) | .21 | |||
| Social media | 0.88 | (0.46) | .80 | |||
| Genderb | 1.19 | (0.51) | .69 | 1.33 | (0.57) | .50 |
| Age | 1.11 | (0.10) | .24 | 1.06 | (0.10) | .52 |
| Neighborhood quality | 2.85 | (0.99) | .002 | 1.78 | (0.51) | .04 |
| Constant | .003 | (.007) | .009 | 1.66 | (3.38) | .80 |
Note. Number of pregnancies was represented as three dummy variables with no previous pregnancies serving as the reference group.
The reference category was never pregnant.
Female = 1; male = 0.
Results indicate that youth who heard about contraception through word of mouth or neighborhood gossip were 4.06 times more likely to use contraception than those who did not. Further, youth who were exposed to contraception information on social media were 2.69 times more likely to report using contraception at last intercourse. Word of mouth or gossip and social media had the largest associations with contraception use, associations larger than parents, schools, or traditional media. Model 2 shows a similar relationship for recent condom use. Youth who were exposed to sexual risk reduction messages through neighborhood gossip or social media were 3.59 times and 2.49 times more likely to have used a condom at their last intercourse, respectively. Further, youth who reported parents as a source of information on HIV/STD prevention were 4.06 times more likely to have used a condom at last sex than those whose parents were not reported as a source. Other significant predictors of contraception and condom use were multiple, previous pregnancy experiences and neighborhood quality. The odds of condom and contraception use at last sex were much lower for those with previous multiple pregnancy experiences. Neighborhood quality was also positively associated with both contraception and condom use.
Discussion
Youth exposure to sexual content in the media has often used a risk or deficit perspective, focusing on the effects of sexual content in the media on age of sexual initiation (O’Hara et al., 2012), risky sexual behaviors (Bleakley et al., 2009; Brown et al., 2006), and sexual victimization (Ybarra et al., 2014). However, current research indicates that online sources may have a positive impact on youth sexual behavior. For example, youth who learn about sex via social media demonstrate increased self-efficacy to use of condoms, as well as greater knowledge of HIV/STD risk factors (Divecha et al., 2012). A growing body of research has broadened our understanding of the relationship between social media use and youth sexual behavior; however, these studies have been mostly qualitative (Stevens et al., 2014) and relied upon nonracial and ethnic minority youth (Selkie et al., 2011). Our study contributes to the empirical literature by examining how the Integrative Model of Behavior Change can be applied to better understand the relationship between social media use and sexual risk-reduction behaviors among African-American and Latino/a youth. This study presents a number of important results.
First, social media functions as an important source of contraception and HIV/STD prevention information. These findings mirror Jones and Biddlecom (2011), which indicated that nearly 50% of youth were exposed to contraception information online. However, the authors found that teens did not particularly view the Internet as a reliable or trustworthy source. Distrust stemmed from user-generated content and the belief that some content was being used to sell products (Jones & Biddlecom, 2011). Because social media is more akin to personal communication, it may be viewed as more reliable than the Internet at large. While this study did not delve into youth trust of sexual risk-reduction information, nor did it collect data on the type of information (e.g., sexually explicit material, advertisements) obtained from social media sources, exposure to information on social media was positively associated with practicing recent sexual risk reduction behaviors. Future research should explore this issue further.
Second, this study found that social media had an influence on sexual risk-reduction behaviors similar to that of word-of-mouth information/neighborhood gossip. Social media may be an amplification of word-of-mouth information and gossip that has migrated to an online platform. Because word-of-mouth information is not consistently accurate, nurses and health practitioners should look for ways to work within the social media space to ensure the spread of scientifically accurate sexual risk-reduction information. Health professionals can leverage the role of social media to develop innovative interventions or as an additional component of existing HIV/STD prevention interventions for youth. Coupling these preexisting modes of health information dissemination with the trusted role nurses often have as practitioners would create a dynamic and synergistic approach to reducing sexual risk.
Third, these findings suggest shifts in sources of sexual risk-reduction information. Specifically, youth in this study reported receiving sexual risk-reduction information in online spaces at levels similar to information received from friends and parents. To be sure, social media can include information received from parents and friends online, but it is not limited to those immediate relationships. Further, discussions concerning the influence of social media on adolescent attitudes and behaviors often liken it to a peer, or media “super peer.” This super peer establishes and amplifies norms in ways similar to regular peers (Strasburger et al 2002). As a super peer, social media also connects youth with a larger array of people and information outside of their immediate friendship networks. As social media sexual health interventions are being developed, deployed, and tested (Bull, Levine, Black, Schmiege, & Santelli, 2012; Ralph et al., 2011), health practitioners and nurse researchers can benefit from sharing best practices and effective strategies for capitalizing on these extended spaces of youth community.
Fourth, past sexual behavior, gender, age, and neighborhood quality all influence future intentions to have sex and sexual risk-reduction behaviors. The school setting remains important as youth with lower intentions to have sex report greater exposure to HIV/STD prevention messages in schools. The significant role of schools and school nurses as information sources for sexual decision making highlights the need for investment in and integration of science-based, sexual health information into the curricula of public, private, and charter schools in urban communities.
Previous experiences with pregnancy also matter. Past findings indicate that teenagers who have experienced previous pregnancies are more likely to report using contraception (Patel et al., 2016), particularly long-term hormonal contraception (Paukku, Quan, Darney, & Raine, 2003). However, in this sample, multiple past pregnancy experiences were associated with not using contraception. Thus, further investigation examining the relationship between previous pregnancies and contraception use in ethnic minority populations at high risk for unintended pregnancy is needed. For ethnic minority youth, a lack of access to contraceptive services is also a salient problem (Champion, Young, & Rew, 2016; Patel et al., 2016) which may moderate the effects of past pregnancy experiences and sexual risk reduction behaviors. Environmental constraints, as outlined in the IMBC, should therefore also be examined in future research.
Neighborhood quality among low-income communities was an important covariate of sexual risk-reduction behaviors. These results suggest that even interventions that focus on individual-level strategies to promote sexual health and risk reduction in marginalized communities should engage the structural determinants of health. Structures like policing and crime, business investment, economic opportunity, and political leadership impact neighborhood quality and, subsequently, sexual risk-reduction behaviors. Investment in low-income neighborhoods and communities as a route to improve sexual health outcomes among youth could be part of an effective prevention strategy.
Finally, consistent with findings from Ritchwood et al. (2016), it is clear from the data that knowledge about condoms remains an area of concern. A small portion of this sample did not consider condoms to be a form of birth control. This suggests that there continues to be a need—despite the increasing availability of sexual health information online—for clear communication about condoms as effective contraception as well as a HIV/STD protection. To quantify the prevalence of misinformation in this area, future research should explicitly assess sexual health knowledge.
Limitations
Despite its contributions to the field, this study has several limitations. First, because this is a cross-sectional study, only associations and not causes can be demonstrated. However, longitudinal studies of this nature have also struggled with temporal order in determining causality. Further, research suggests that rather than correlation, there is evidence for recursive relationships between media exposure and sexual behavior (Bleakley et al., 2008). Second, the measure used for sexual intercourse did not specify the behavioral meaning (e.g., vaginal, oral, anal), leaving each respondent to interpret the question individually. This approach is the standard practice used in the CDC’s national YRBS survey (2014). Third, this study did not gather information on the actual content and messages received from the different information sources. Future research should utilize more detailed measures of both sexual behaviors and types of sexual health information received. Fourth, although this study provides evidence for the significant influence of social media as a source of contraception information on sexual risk-reduction behaviors, it remains unclear what IMBC constructs mediate these effects. Future studies should examine the influence of social media as a source of sexual health information on normative beliefs, attitudes, and self-efficacy for sexual risk-reduction behaviors in order to explicate these processes.
Conclusion
The findings presented here contribute to the growing body of research on social media use and sexual risk-reduction behaviors and further expand the literature by assessing this relationship among African-American and Latino/a youth. The results highlight the important role of social media in shaping sexual risk-reduction behaviors among minority youth. The implications of these findings cannot be understated, as community health and school nurses can integrate social media strategies into future sexual health promotion strategies, screenings, and interventions for racial and ethnic minority youth. Nurse scientists must stay informed about the media usage behaviors of youth, considering the platforms by which youth communicate online are ever evolving. Indeed, nurses will need to be flexible and incorporate developing technologies into their health promotion programs. Importantly, there is a need to forge new partnerships between nurses and technologists, computer scientists, and target populations. Only then will nurse scientists be able to fully leverage the utility of these platforms to effectively and efficiently disseminate sexual health information to youth.
Footnotes
The authors have no conflicts of interest to report.
Contributor Information
Robin Stevens, School of Nursing, University of Pennsylvania, Philadelphia, PA.
Stacia Gilliard-Matthews, Department of Sociology, Anthropology, and Criminal Justice, Rutgers University, Camden, NJ.
Jamie Dunaev, Health Sciences Program, Rutgers University, Camden, NJ.
Abigail Todhunter-Reid, Department of Childhood Studies, Rutgers University, Camden, NJ.
Bridgette Brawner, School of Nursing, University of Pennsylvania, Philadelphia, PA.
Jennifer Stewart, School of Nursing, Department of Community Public Health, Johns Hopkins University, Baltimore, MD.
References
- Bleakley A, Hennessy M, Fishbein M, Jordan A. It works both ways: The relationship between exposure to sexual content in the media and adolescent sexual behavior. Media Psychology. 2008;11:443–461. doi: 10.1080/15213260802491986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bleakley A, Hennessy M, Fishbein M, Jordan A. How sources of sexual information relate to adolescents’ beliefs about sex. American Journal of Health Behavior. 2009;33:37–48. doi: 10.5993/AJHB.33.1.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyd D. It’s complicated: The social lives of networked teens. New Haven, CT: Yale University Press; 2014. [Google Scholar]
- Brown JD, L’Engle KL, Pardun CJ, Guo G, Kenneavy K, Jackson C. Sexy media matter: Exposure to sexual content in music, movies, television, and magazines predicts black and white adolescents’ sexual behavior. Pediatrics. 2006;117:1018–1027. doi: 10.1542/peds.2005-1406. [DOI] [PubMed] [Google Scholar]
- Buhi ER, Klinkenberger N, Hughes S, Blunt HD, Rietmeijer C. Teens’ use of digital technologies and preferences for receiving STD prevention and sexual health promotion messages: Implications for the next generation of intervention initiatives. Sexually Transmitted Diseases. 2013;40:52–54. doi: 10.1097/OLQ.0b013e318264914a. [DOI] [PubMed] [Google Scholar]
- Bull SS, Levine DK, Black SR, Schmiege SJ, Santelli J. Social media–Delivered sexual health intervention. American Journal of Preventive Medicine. 2012;43:467–474. doi: 10.1016/j.amepre.2012.07.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control (CDC) 2015 High school youth risk behavior survey data. n.d Retrieved from http://nccd.cdc.gov/youthonline/
- Centers for Disease Control and Prevention (CDC) HIV Surveillance Report, Vol.26: Diagnoses of HIV infection in the United States and dependent areas, 2014. 2014 Retrieved from https://www.cdc.gov/hiv/pdf/library/reports/surveillance/cdc-hiv-surveillance-report-2014-vol-26.pdf.
- Champion JD, Young C, Rew L. Substantiating the need for primary care-based sexual health promotion interventions for ethnic minority adolescent women experiencing health disparities. Journal of the American Association of Nurse Practitioners. 2016;28:487–492. doi: 10.1002/2327-6924.12346. [DOI] [PubMed] [Google Scholar]
- Divecha Z, Divney A, Ickovics J, Kershaw T. Tweeting about testing: Do low-income, parenting adolescents and young adults use new media technologies to communicate about sexual health? Perspectives on Sexual and Reproductive Health. 2012;44:176–183. doi: 10.1363/4417612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farmer AD, Bruckner Holt CE, Cook MJ, Hearing SD. Social networking sites: A novel portal for communication. Postgrad Medical Journal. 2009;85:455–459. doi: 10.1136/pgmj.2008.074674. [DOI] [PubMed] [Google Scholar]
- Fishbein M, Yzer MC. Using theory to design effective health behavior interventions. Communication Theory. 2003;13:164–183. doi: 10.1111/j.1468,-2885.2003.tb00287.x. [DOI] [Google Scholar]
- Gibb SJ, Fergusson DM, Horwood LJ, Boden JM. Early motherhood and long-term economic outcomes: Findings from a 30-year longitudinal study. Journal of Research on Adolescence. 2015;25:163–172. doi: 10.1111/jora.12122. [DOI] [Google Scholar]
- Gilliard-Matthews S, Stevens R, Nilsen M, Dunaev J. “You see it everywhere. It’s just natural.” Contextualizing the role of peers, family, and neighborhood in initial substance use. Deviant Behavior. 2015;36:492–509. doi: 10.1080/01639625.2014.944068. [DOI] [Google Scholar]
- Gold J, Pedrana AE, Sacks-Davis R, Hellard ME, Chang S, Howard S, … Stoove MA. A systematic examination of the use of online social networking sites for sexual health promotion. BMC Public Health. 2011;11:583. doi: 10.1186/1471-2458-11-583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang CY, Costeines J, Ayala C, Kaufman JS. Parenting stress, social support, and depression for ethnic minority adolescent mothers: Impact on child development. Journal of Child and Family Studies. 2014;23:255–262. doi: 10.1007/s10826-013-9807-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones RK, Biddlecom AE. Is the internet filling the sexual health information gap for teens? An exploratory study. Journal of Health Communication. 2011;16:112–123. doi: 10.1080/10810730.2010.535112. [DOI] [PubMed] [Google Scholar]
- Jones K, Eathington P, Baldwin K, Sipsma H. The impact of health education transmitted via social media or text messaging on adolescent and young adult risky sexual behavior: A systematic review of the literature. Sexually Transmitted Diseases. 2014;41:413–419. doi: 10.1097/OLQ.0000000000000146. [DOI] [PubMed] [Google Scholar]
- Lenhart A. Teens, social media & technology overview 2015. 2015 Retrieved from http://www.pewinternet.org/2015/04/09/teens-social-media-technology-2015/
- Madden M, Lenhart A, Duggan M, Cortesi S, Gasser U. Teens and technology 2013. Washington, DC: Pew Research Center; 2013. Retrieved from PIP_TeensandTechnology2013.pdf. [Google Scholar]
- Moorhead SA, Hazlett DE, Harrison L, Carroll JK, Irwin A, Hoving C. A new dimension of healthcare: Systematic review of the uses, benefits, and limitations of social media for health communication. Journal of Medical Internet Research. 2013;15(4):e85. doi: 10.2196/jmir.1933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Hara RE, Gibbons FX, Gerrard M, Li Z, Sargent JD. Greater exposure to sexual content in popular movies predicts earlier sexual debut and increased sexual risk taking. Psychological Science. 2012;23:984–993. doi: 10.1177/0956797611435529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel PR, Huynh MT, Alvarez CA, Jones D, Jennings K, Snyder RR. Postpartum teenagers’ views on providing contraception in school-based health clinics. Journal of Women’s Health. 2016;25:32–37. doi: 10.1089/jwh.2015.5285. [DOI] [PubMed] [Google Scholar]
- Paukku M, Quan J, Darney P, Raine T. Adolescents’ contraceptive use and pregnancy history: Is there a pattern? Obstetrics & Gynecology. 2003;101:534–538. doi: 10.1016/S0029-7844(02)02717-5. [DOI] [PubMed] [Google Scholar]
- Pew Research Center. Social Media Fact Sheet. 2017 Retrieved from www.pewinternet.org/fact-sheet/social-media/
- Ralph LJ, Berglas NF, Schwartz SC, Brindis CD. Finding teens in TheirSpace: Using social networking sites to connect youth to sexual health services. Sexuality Research and Social Policy. 2011;8:38–49. doi: 10.1007/s13178-011-0043-4. [DOI] [Google Scholar]
- Ritchwood TD, Dave G, Carthron DL, Isler MR, Blumenthal C, Wynn M, … Corbie-Smith G. Adolescents and parental caregivers as lay health advisers in a community-based risk reduction intervention for youth: Baseline data from Teach One, Reach One. AIDS Care. 2016;28:537–542. doi: 10.1080/09540121.2015.1112348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Selkie EM, Benson M, Moreno M. Adolescents’ views regarding uses of social networking websites and text messaging for adolescent sexual health education. American Journal of Health Education. 2011;42:205–212. doi: 10.1080/19325037.2011.10599189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stevens R, Gilliard-Matthews S, Nilsen M, Malven E, Dunaev J. Socioecological factors in sexual decision making among urban girls and young women. Journal of Obstetric, Gynecologic, & Neonatal Nursing. 2014;43:644–654. doi: 10.1111/1552-6909.12493. [DOI] [PubMed] [Google Scholar]
- Stevens R, Dunaev J, Malven E, Bleakley A, Hull A. Social media in the sexual lives of African American and Latino youth: Challenges and opportunities in the digital neighborhood. Media and Communication. 2016;4 doi: 10.17645/mac.v4i3.524. [DOI] [Google Scholar]
- Stevens R, Gilliard-Matthews S, Dunaev J, Woods MK, Brawner BM. The digital hood: Social media use among youth in disadvantaged neighborhoods. New Media & Society. 2016 doi: 10.1177/1461444815625941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strasburger VC, Wilson BJ, Jordan AB. Children, adolescents, and the media. Thousand Oaks, CA: Sage; 2009. [Google Scholar]
- Turner CF, Ku L, Rogers SM, Lindberg LD, Pleck JH, Sonenstein FL. Adolescent sexual behavior, drug use, and violence: Increased reporting with computer survey technology. Science. 1998;280:867–873. doi: 10.1126/science.280.5365.867. [DOI] [PubMed] [Google Scholar]
- U.S. Census Bureau. State and metropolitan area data book: 2010. 2010 Retrieved from www.census.gov/prod/2010pubs/10smadb/2010smadb.pdf.
- Widman L, Choukas-Bradley S, Helms SW, Golin CE, Prinstein MJ. Sexual communication between early adolescents and their dating partners, parents, and best friends. Journal of Sex Research. 2014;51:731–741. doi: 10.1080/00224499.2013.843148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ybarra ML, Strasburger VC, Mitchell KJ. Sexual media exposure, sexual behavior, and sexual violence victimization in adolescence. Clinical Pediatrics. 2014;53:1239–1247. doi: 10.1177/0009922814538700. [DOI] [PubMed] [Google Scholar]