Abstract
The aim of this study was to evaluate the clinical efficacy of external fixation, delayed open reduction, and internal fixation in treating tibial plateau fracture with dislocation.
Clinical data of 34 patients diagnosed with tibial plateau fracture complicated with dislocation between January 2009 and May 2015 were retrospectively analyzed. Fifteen patients in group A underwent early calcaneus traction combined with open reduction and internal fixation and 19 in group B received early external fixation combined with delayed open reduction and internal fixation. Operation time, postoperative complication, bone healing time, knee joint range of motion, initial weight-bearing time, Rasmussen tibial plateau score, and knee function score (HSS) were statistically compared between 2 groups.
The mean follow-up time was 18.6 months (range: 5–24 months). The mean operation time in group A was 96 minutes, significantly longer than 71 minutes in group B (P < .05). In group A, 5 cases had postoperative complications and 1 in group B (P < .05). The mean bone healing time in group A was 6.9 months (range: 5–9 months) and 6.0 months (range: 5–8 months) in group B (P > .05). In group A, initial weight-bearing time in group A was (14.0 ± 3.6) weeks, significantly differing from (12.9 ± 2.8) weeks in group B (P < 0.05). In group A, the mean knee joint range of motion was 122° (range: 95°–150°) and 135° (range: 100°–160°) in group B (P > 0.05). Rasmussen tibial plateau score in group A was slightly lower than that in group B (P > .05). The excellent rate of knee joint function in group A was 80% and 84.21% in group B (P > .05).
External fixation combined with delayed open reduction and internal fixation is a safer and more efficacious therapy of tibial plateau fracture complicated with dislocation compared with early calcaneus traction and open reduction and internal fixation.
Keywords: delayed treatment, external fixation, fracture dislocation, tibial plateau
1. Introduction
Tibial plateau fracture contains a wide range of types and severities of injury. Multiple classifications of tibial plateau fractures have been developed to assess injury severity, treatment plan, and predict clinical prognosis. Currently, Schatzker classification system [1] is the most widely accepted and composed of 6 condylar fracture types classified by fracture pattern and fragment anatomy. Type I facture refers to lateral plateau fracture without depression. Type II is lateral plateau fracture and involves vertical split of the lateral condyle combined with depression of the adjacent load-bearing part of the condyle. Type III is defined as compression fracture of the lateral or central tibial plateau in which the articular surface of the tibial plateau is depressed and driven into the lateral tibial mataphysis by axial forces. Type IV refers to medial tibial plateau fracture with a split or depression. Type V is bicondylar fracture of the medial and lateral tibial plateau and type VI is defined as transverse subcondylar fracture with dissociation of the metaphysis from the diaphysis. It is challenging to properly treat tibial plateau fracture with dislocation. If not properly treated, severe postoperative complications, skin necrosis, wound infection, bone exposure, anchylosis, knee joint pain, traumatic osteoarthritis, and knee joint instability are likely to occur.[2,3]
At present, it is widely accepted that protection of soft tissues and prevention of soft tissue complications play a pivotal role in the treatment of complicated tibial plateau fracture.[4] Currently, calcaneus skeletal traction and knee joint external fixation are commonly adopted to treat tibial plateau fracture with dislocation. Calcaneus skeletal traction is simple to operate, whereas it probably induces the incidence of pressure ulcer and the effect of reduction is difficult to evaluate. External fixation of the knee joint complies with the principle of injury control and staged treatment. However, the effect of external fixation upon delayed internal fixation and clinical prognosis has been rarely studied.
In this investigation, clinical data of 34 patients with tibial plateau fracture with dislocation admitted to Qingpu Branch of Zhongshan Hospital affiliated to Fudan University between January 2009 and May 2015 were retrospectively analyzed. Among them, 15 cases underwent early calcaneus traction (group A) and 19 received early external fixation (group B). Clinical efficacy and surgical safety were statistically evaluated between 2 surgical techniques.
2. Materials and methods
2.1. Baseline data
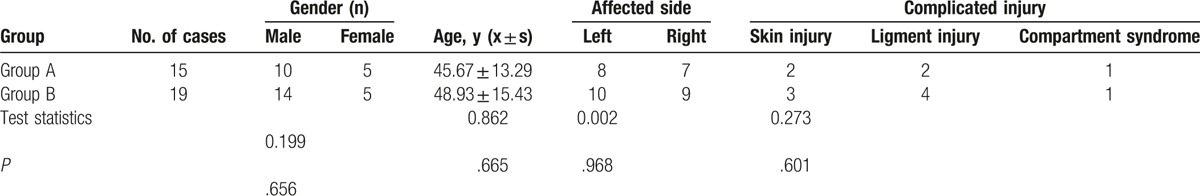
Among 34 patients, 24 were male and 10 female, aged 31 to 65 years with an average age of 47.6 years. Twenty-five cases were injured by traffic accident, 5 by falling, and 4 by heavy crush. Five patients were accompanied by skin open injury or soft tissue denudation injury, 6 with collateral and cruciate ligament injury, and 2 with acute compartment syndrome. In group A, there were 15 patients, 10 male and 5 female, aged 31 to 59 years with an average age of 45.7 years, 2 accompanied by skin open injury or denudation wound, 2 with ligament injury, and 1 with compartment syndrome. In group B, there were 19 patients, 14 male and 5 female, aged 33 to 65 years with a mean age of 48.9 years, 3 complicated with skin open injury or denudation wound, 4 with ligament injury, and 1 with compartment syndrome. Baseline data including age, gender, and concurrent injury did not significantly differ between the 2 groups (all P > .05), as illustrated in Table 1. All patients were not complicated with other chronic systemic diseases. The severity and type of tibial plateau fracture did not significantly differ among different individuals. This study was approved by the local ethnics committee of our institution. Written informed consents were obtained from all participants.
Table 1.
Comparison of preoperative baseline data between 2 groups.
2.2. Inclusion and exclusion criteria
Inclusion criteria included patients with tibial plateau fracture with dislocation admitted to Qingpu Branch of Zhongshan Hospital affiliated to Fudan University between January 2009 and May 2015; temporary external fixation or calcaneus traction was performed before internal fixation; follow-up duration ≥5 months. Exclusion criteria included those with severe osteoporosis or pathological fracture; those with multiple fracture or old fracture; and those complicated with relatively severe splanchnopathy and cannot tolerate the surgery.
2.3. Preoperative examination
Preoperative examinations were performed to exclude the surgical contraindications. Imaging examinations included anteriolateral X-ray of knee joint (Fig. 1A, B), computed tomography (CT) plain scan (Fig. 2A, B) and 3-dimensional reconstruction (Fig. 1C, D), blood vessel ultrasound, or digital subtraction angiography to evaluate the vascular status of the affected limbs and magnetic resonance imaging (MRI) examination to assess the severity of ligament injury in the knee joint. Before surgery, all patients were subjected to the test of weight-bearing time, knee joint range of motion, and Rasmussen tibial plateau score, and no significant difference was observed between groups A and B.
Figure 1.
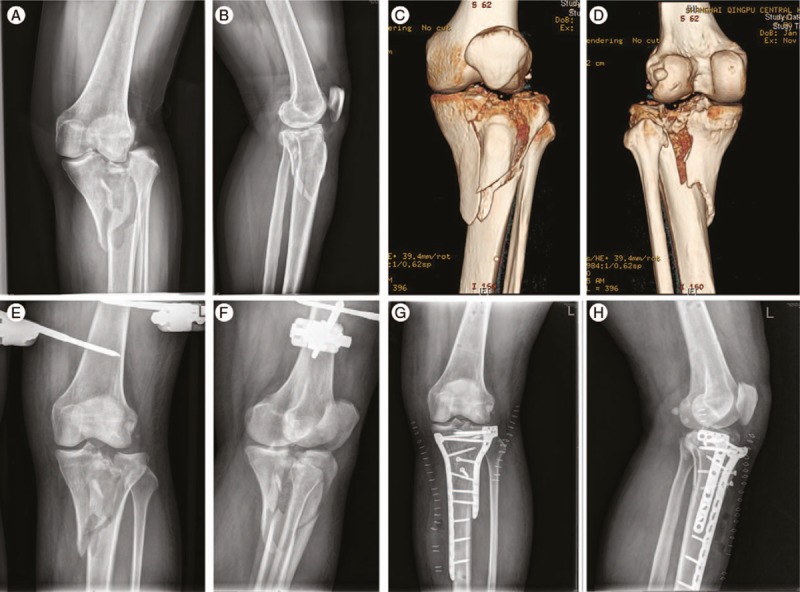
Case 1 undergoing external fixation and delayed open reduction and internal fixation. Preoperative X-ray imaging (A, B), 3D reconstruction imaging (C, D), postoperative CT scan (E–H).
Figure 2.
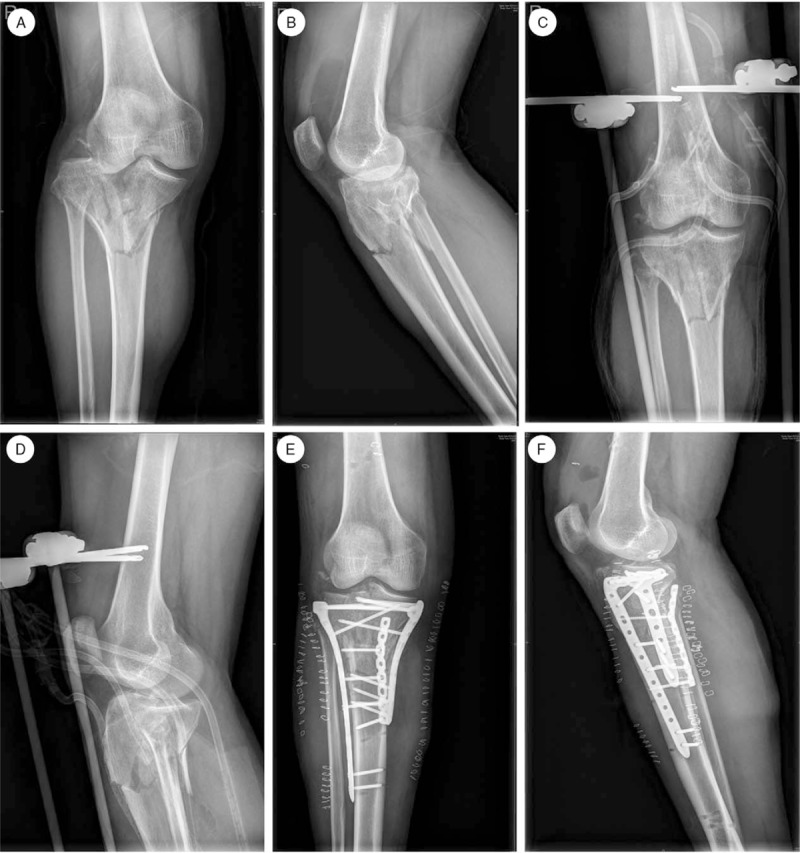
Case 2 undergoing external fixation and delayed open reduction and internal fixation. Preoperative X-ray (A, B), postoperative X-ray imaging (C–F).
2.4. Clinical treatment
2.4.1. Calcaneus traction in combination with delayed open reduction and internal fixation
Initially, wound debridement and suturing was performed in the emergency department. The compartment syndrome was treated with fascial opening and decompression and skeletal traction was conducted with 6 hours with a traction load of approximately half of the body weight. The lower extremity was elevated approximately 20 cm after surgery. The patient's conditions and physical signs were carefully evaluated before internal fixation to exclude the possibility of surgical contraindications. The surgery date was determined according to the severity of affected limb swelling. All participants underwent the operation within 7 to 14 days after the injury. Lateral or medial or combined incision was created to expose the bone fracture. The side with less displacement was reduced and temporarily fixed by using Kirschner wires. After reduction, the subchondral bone was subject to temporary fixation suing 1.5 mm Kirschner wires.[5] Allogeneic bone implantation was performed during the process of reduction. After reduction, dissection steel plate was utilized for fracture fixation. Posterior fracture was supported and fixed by placement of reconstructed steel plate as necessary. Meniscus injury should be repaired throughout the surgery to retain the meniscus as possible. The avulsion fracture of insertional cruciate ligament was fixed using steel wire.
2.5. Staged surgical treatment
2.5.1. Transjoint external fixation (stage I)
All patients completed the surgery within 6 hours after injury. Patient's condition and vital signs were assessed and preoperative examinations were conducted to exclude the possibility of surgical contraindications. During stage I surgery, open wound was subject to debridement and suturing and fascial opening and decompression was performed to treat compartment syndrome. Two pieces of Schanz screws with a diameter of approximately 6 mm were inserted into the distal femur and middle lower segment of the tibia. Trans-knee joint external fixation was delivered. Traction reduction was adjusted according to axial alignment of lower limbs. The fixation position of the external fixation pole was determined based upon the eversion angle and length of the contralateral lower limbs. Reduction clamp was applied for those failed to receive traction reduction. Favorable traction was maintained for those with difficulty in condyles of tibia reduction.
2.5.2. Open reduction and internal fixation (stage II)
Internal fixation was performed within 7 to 14 days following stage I external fixation. Stent extraction combined with open reduction and internal fixation was conducted after disappearance of skin swelling, blister decrustation, and wound surface healing. The surgical incision and surgical procedures were similar to those of group A, as illustrated in the Figs. 1 and 2.
2.6. Postoperative management and function evaluation
Postoperative routine nursing, drainage tube management, elevation of the affected limb, and anti-infection and pain-relieving therapies were delivered. All patients were required to cooperate with muscular contraction training, and passive and active movement of knee joint. Patients were prohibited from full load within postoperative 3 months. X-ray of the knee joint was performed on the day and every month within 3 months after drainage tube removal. Appropriate weight-load exercise was gradually delivered according to the callus growth status until full-load activity. At postoperative follow-up of 5 to 24 months, knee joint grading was qualitatively evaluated according to the Rasmussen tibial plateau score[6] and HSS knee joint function evaluation criteria.[7]
2.7. Statistical analysis
SPSS 19.0 statistical software was used for data analysis (SPSS Inc., Chicago, IL). Measurement data, such as operation time, bone healing time, knee joint range of motion, and time of postoperative loading, were expressed as mean ± standard deviation and statistically analyzed using analysis of variance (ANOVA) test. Postoperative complications, including postoperative wound infection, knee joint angle and knee joint deformity, Rasmussen and HSS scores, were statistically compared using Chi-square test between the 2 groups. A P value of less than .05 was considered as statistical significance.
3. Results
3.1. Postoperative follow-up
All participants between 2 groups were surgically treated by the same surgeon and advised to take early function exercises. Postoperative follow-up endured for 18.6 months on average, ranging from 5 to 24 months. In group A, the mean operation time was recorded as 96 minutes significantly longer than 71 minutes in group B.
3.2. Postoperative complications
In group A, 3 patients presented with surface incisional wound infection and 2 cases had 15° to 20° of angulation deformity. No symptoms of deep infection, compartment syndrome, osteomyelitis, or alternative postoperative complications were documented. The incidence of postoperative complication in group A was 33.33%, significantly higher than 5.26% in group B (P < .05). In group B, merely 1 patient developed surface incisional wound infection. All patients in 2 groups obtained bone healing.
3.3. Postoperative recovery
In group A, the mean bone healing time was calculated as 6.9 months (range: 5–9 months), which did not significantly differ from 6.0 months, ranging from 5 to 8 months, in group B (P > .05). During the period of follow-up, the time of initial loading in group A was (14.0 ± 3.6) weeks, significantly longer than (12.9 ± 2.8) weeks in group B (P < .05). In group A, the group knee joint range of motion was 122° (range: 95°–150°), which did not considerably differ from 135° (range: 100°–160°) in group B (P > .05). Rasmussen tibial plateau score in group A was slightly lower than that in group B with no statistical significance (P > .05). The excellent rate of knee joint function in group A was 80% and 84.21% in group B with no statistical significance between the 2 groups (P > .05) and others achieved fair outcomes, as summarized in Table 2.
Table 2.
Comparison of clinical parameters between 2 groups.

4. Discussion
Tibial plateau fracture with dislocation is constantly caused by high energy injury. It is likely to be complicated with severe peripheral soft tissue injury and knee joint instability, even accompanied by multiple regional fracture and multiorgan damages. If improperly treated, the incidence of soft tissue necrosis and infection reaches as high as 50% to 80%.[8] Consequently, it is a challenging task for orthopedists to treat tibial plateau fracture with dislocation. The main goals of tibial plateau fracture treatment are to obtain smooth articular surface, normal axial alignment, stable painless joint, and favorable knee joint range of motion.[9] Several therapeutic options are currently available, such as external fixation, early open reduction and internal fixation, limited open reduction and internal fixation, and combined application of external and internal fixation and ring-shaped external fixation. However, the optimal treatment of tibial plateau fracture remains elusive. At present, more and more attention has been paid not only to the healing of tibial plateau fracture but also to the protection of surrounding soft tissues.[10] The prevention of soft tissue injury is involved with both the stage I and II surgical procedures.
Rotondo et al[11] first applied staged therapeutic strategy to treat high energy fracture and considered that early temporary external fixation could avoid aggravating the joint trauma and peripheral soft tissue injury. Until the mitigation of systemic symptoms and topical soft tissue damage, open reduction and internal fixation was subsequently delivered. The application of these sequential procedures can reduce the incidence of soft tissue necrosis and infection, and enhance the success rate of surgery.
In this investigation, staged therapeutic strategy was applied to treat patients with tibial plateau fracture with dislocation in group B. Initially, transjoint external fixation was performed during stage I surgery, which effectively restored the limb length, provoked moderate tension of joint capsule, ligament, and articular peripheral soft tissues, and generated traction and compression reduction upon multiple fracture fragments. Through maneuver compression or forcep reduction and correction of displaced fracture, the joint rotation deformity was corrected, the articular surface became smooth, and the bone, cartilage, and soft tissue injury was alleviated. For patients undergoing calcaneus traction, the fractures bones were not treated early, which probably induced the occurrence of hematoma, soft tissue adhesion, and joint capsule and adjacent ligament contraction, etc. Hence, compared with those patients, the advantages of the modified technique are that it is simple and convenient to operate, which can decrease the incidence of 2-stage operation reduction or violent reduction, shorten operation time, reduce the occurrence of intraoperative soft tissue traction, and avert the incidence of soft tissue irritation. The position of transjoint external fixation lays the foundation for stage II internal fixation and self-repairing of peripheral soft tissue injury, and reduces the surgical risk of stage II internal fixation.[12] The combined surgery is able to decrease the postoperative complications of stage II internal fixation. Although calcaneus traction and transjoint external fixation may limit the functional training of knee joint, external fixation procedures can guarantee the success of stage II surgery, reduce the incidence of postoperative complication, and assist the patients to take functional training as early as possible. Meantime, the knee joint range of motion and excellent rate of Rasmussen and HSS scores in patients undergoing external fixation are higher than their counterparts receiving calcaneus traction.
Transjoint external fixation is likely to limit the functional training of knee joint and provoke the incidence of peripheral soft tissue fibrosis, amyotrophy, myodynamia, synarthrophysis, and screw infection.[13] Consequently, it is not recommended to place the transjoint external fixation stent for a long period. In this investigation, the external fixation stent was retained in all patients from group B who did not exceed 2 weeks. At present, most scholars consider that it is an efficacious option to perform internal fixation after the disappearance of swelling, skin fold and infectious symptoms in the affected limbs when the external fixation device is retained.[12,14] In our experience, if no apparent infection symptoms occur, the soft tissue injury can self-repair within 2 weeks. Previous studies[15,16] have demonstrated that satisfactory clinical efficacy can be obtained if internal fixation is performed at 14 days after external fixation device placement. No severe soft tissue necrosis and infection are noted. All patients achieve excellent postoperative recovery. Nevertheless, the time of external fixation stent placement should be properly prolonged for those with severe soft tissue injury or those with poor recovery.
In this study, combined application of external fixation and open reduction and internal fixation is an efficacious and safe surgical technique in the management of tibial plateau fracture with dislocation, which can decrease the incidence of postoperative complications of stage II internal fixation. It can yield higher clinical efficacy than traction combined with open reduction and internal fixation. However, due to the insufficient sampling size in this investigation, no statistical significance was obtained when comparing multiple parameters between 2 groups. Moreover, logistic regression analysis was not performed to analyze the risk factors of clinical prognosis of patients with tibial plateau fracture with dislocation.
Footnotes
Abbreviations: CT = computed tomography, HSS = knee function score.
The authors declare that they have no conflict of interest.
References
- [1].Markhardt K, Gross JM, Monu JU. Schatkzker classification of tibial plateau fractures: use of CT and MR Imaging improves assessment. Radiographics 2009;29:585–97. [DOI] [PubMed] [Google Scholar]
- [2].Borrelli J. Management of soft tissue injuries associated with tibial plateau fractures. J Knee Surg 2014;27:5–10. [DOI] [PubMed] [Google Scholar]
- [3].McNamara IR, Smith TO, Shepherd KL, et al. Surgical fixation methods for tibial plateau fractures. Cochrane Database Syst Rev 2015;9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Egol KA, Tejwani NC, Capla EL, et al. Staged management of high-energy proximal tibia fractures (OTA types 41): the results of a prospective, standardized protocol. J Orthop Trauma 2005;19:448–55. [DOI] [PubMed] [Google Scholar]
- [5].Yoon YC, Oh JK, Oh CW, et al. Inside out rafting K-wire technique for tibial plateau fractures. Arch Orthop Tramua Surg 2012;132:233–7. [DOI] [PubMed] [Google Scholar]
- [6].Rasmussen PS. Tibial condylar fractures. Impairment of knee joint stability as an indication for surgical treatment. J Bone Joint Surg Am 1973;55:1331–50. [PubMed] [Google Scholar]
- [7].Insall JN, Ranawat CS, Aglietti P, et al. A comparison of four models of total knee-replacement prostheses. J Bone Joint Surg Am 1976;58:754. [PubMed] [Google Scholar]
- [8].Spagnolo R, Pace F. Management of the schatzker VI fractures with lateral locked screw plating. Musculoskelet Surg 2012;96:75–80. [DOI] [PubMed] [Google Scholar]
- [9].Wang D, Xiang JP, Chen XH, et al. A meta-analysis for postoperative complications in tibial plafond fracture: open reduction and internal fixation versus limited internal fixation combined with external fixator. J Foot and Ankle Surg 2015;54:646–51. [DOI] [PubMed] [Google Scholar]
- [10].Scalea TM, Boswell SA, Scott JD, et al. External fixation as a bridge to intramedullary nailing for patients with multiple injuries and with femur fractures: damage control orthopedics. J Trauma 2000;48:613–23. [DOI] [PubMed] [Google Scholar]
- [11].Rotondo MF, Schwab CW, McGonigal MD, et al. Damage control: an approach for improved survival in exsanguinating penetrating abdominal injury. Acute Care Surg 1993;35:375–83. [PubMed] [Google Scholar]
- [12].Perumal VM, Mauffrey C, Roberts CS. External Fixators in the Treatment of Tibial Plateau Fractures. External fixation in Orthopedic Traumatology. 2012;London: Springer, 121–129. [Google Scholar]
- [13].Lowenberg DW, Githens M, Boone C. Principles of tibial fracture management with circular external fixation. Orthop Clin North Am 2014;45:191–206. [DOI] [PubMed] [Google Scholar]
- [14].Maru N, Mandaliya D, Parmar R. Two stage reconstruction protocol in management of hing-energy proximal tibia fractures (schatzker,type IV-VI). J Evol Med Dental Sci 2012;4:639. [Google Scholar]
- [15].Mahadeva D, Costa ML, Graffey A. Open reduction and internal fixation versus hybrid fixation for bicondylar/severe tibial plateau fractures: a systemic review of the literature. Arch Orthop Trauma Surg 2008;128:1169–75. [DOI] [PubMed] [Google Scholar]
- [16].Stark E, Stucken C, Trainer G, et al. Compartment syndrome in Schatzker type VI plateau fractures and medial condylar fracture-dislocations treated with temporary external fixation. J Orthop Trauma 2009;23:502–6. [DOI] [PubMed] [Google Scholar]


