Supplemental Digital Content is available in the text
Keywords: Blinder–Oaxaca decomposition, diabetes, hospital readmission, variation
Abstract
Little is known about hospital readmission for patients with diabetes in China. We aimed to assess the temporal pattern, risk factors, and variations of all-cause readmission among hospitalized patients with diabetes in Tianjin, China, from 2008 to 2013.
The Tianjin Basic Medical Insurance Register System database was used to identify discharged patients with diabetes from 2008 to 2013. The influential factors and trends of rehospitalization were analyzed for 30-, 60- and 90-day predicted readmission rates. The Blinder–Oaxaca decomposition was used to explain the readmission variations between 2008 and 2013.
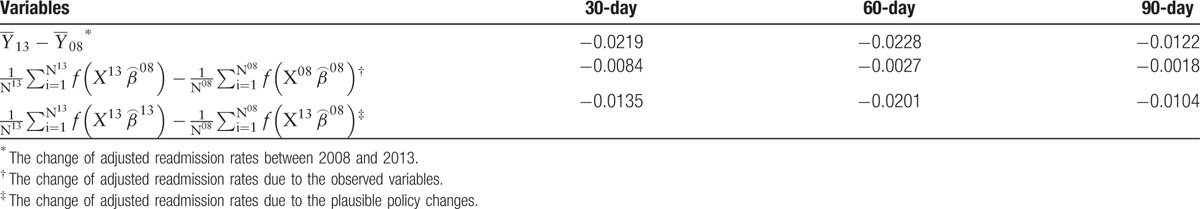
The long stay-time at the index hospitalization is a shared risk factor for readmission at 30, 60, and 90 days each year. The 90-day predicted readmission rates were the highest for each year (all P < .001). The adjusted readmission rates generally decreased by year (all P < .001), except for at the 90-day interval, which decreased in 2010 and slightly increased in 2013 (from 7.47% in 2012 to 7.65% in 2013). If the patients had been readmitted to the hospital in 2013 and the only changes that had occurred since 2008 were observable characteristics, then the readmission rates would have decreased by 0.84%, 0.27%, and 0.18% at 30, 60, and 90 days, respectively. The potential policy changes decreased the readmission rates at 1.35%, 2.01%, and 1.04% for the 3 intervals, respectively.
Identifying targeted factors for the decrease in readmission rates may help to control readmission, particularly for long-interval patients.
1. Introduction
The prevalence of diabetes varies from 8.3% to 12.7% in China,[1] and given the large population, this prevalence makes China carry the burden of having the largest diabetic population among the developing nations. Patients with diabetes are more likely to be repeatedly admitted to hospitals than patients who are diabetes free.[2] These rehospitalizations are responsible for the dramatically increased medical costs of diabetes treatment,[3] as they place substantial physical and psychological stresses on patients and reflect suboptimal patient outcomes.[4,5]
Diabetes-related readmissions were primarily driven by the severity of illness, the presence or absence of coexisting conditions of a patient,[4,6] hospital-level factors, the status of medical insurance usage,[7] the prevalence of hospitalization,[8] and the interventions that were carried out by hospitals before or shortly after discharge.[9] Given these characteristics, a majority of readmissions are preventable and can reflect the effectiveness of health care within a certain region. Therefore, understanding the nature of readmission of Chinese patients with diabetes is essential for controlling readmission, which would be a breakthrough in improving health care quality and reducing health care costs at the same time, especially during an age of reform of the health care system.[10] However, few population-based studies on readmission among diabetes patients have been carried out, specifically in the Chinese setting.
The city of Tianjin is located in the eastern coastal area of China, where the prevalence of diabetes is the highest. Tianjin is the third-largest city in China, and its political status is equal to that of the provinces. On the basis of the political priority and strong economic background, Tianjin is a pioneer in responding to the reform in health care. Therefore, the opportunity for evaluating the profile of readmission for patients with diabetes is unique. Understanding the prevalence and influential factors of readmission and its variations under the reform can help improve the quality of health care. In this study, we first uncovered the profile of readmission patients from 2008 to 2013. Second, the predicted readmissions rates at 30-, 60-, and 90-day intervals after the index hospitalization and its influential factors were compared across the years. Then, we used the Blinder–Oaxaca decomposition method to quantitatively assess the source of variation of readmission (2008 vs 2013). We aimed to provide insights into the profile and variation of readmission and shed light on the areas in which interventions can lead to better medical services and lower costs.
2. Materials and methods
2.1. Data and studied population
We retrospectively used the Tianjin Basic Medical Insurance Register System (TBMIRS) database to identify all records of basic medical insurance (BMI) beneficiaries [International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10) codes for diabetes, E10-E14] who were discharged alive with diabetes from hospitals in Tianjin, China, between January 1, 2008, and December 30, 2013. Since 2008, the coverage rate of BMI was higher than 90%; thus, TBMIRS can identify almost all residents in Tianjin.[11] This database included administrative health care records, and we were able to identify each patient's exclusive personal code, age, gender, clinical diagnoses, and information on the characteristics of hospitals in which the patient had been admitted. We used a randomized stratified sampling method, selecting 50% of these records as a sample, according to the admission years. We excluded patients who were transferred on the day of discharge to other hospitals or patients who were discharged on the same day of admission. We also excluded patients discharged from hospitals located outside of Tianjin due to the hospitals’ unavailable information. The final sample consisted of 73,144 patients from 2008 to 2013. The study design and procedures were approved by the Tianjin Labor and Social Security Bureau Institutional Review Board. All patients’ records and information were anonymized and de-identified before analysis.
2.2. Outcome variables
We defined patients with multiple hospitalization records within a certain year as the readmission patients, and patients with only the index hospital admission within the year were defined as the readmission-free patients. The readmission ratios were calculated by the number of patients in the sample who were discharged with the primary diagnosis of diabetes in each year from a hospital and readmitted to any hospital in Tianjin divided by the total number of patients in the sample who were discharged alive with diabetes in the same year. We counted no more than one readmission for each discharge.
We calculated each patient's likelihood of readmission within 3 periods, 0 to 30 days, 31 to 60 days, and 61 to 90 days after discharge, on the basis of the patients’ characteristics, including age, gender, and the presence or absence of common coexisting conditions, including diabetes complications, hypertension, and congestive heart failure (CHF). Other considerations were the type of diabetes, family history of diabetes, history of diabetes screening within 1 year before diagnosis (which was identified as diabetes screening history), previous usage of diabetes-related medical services (which was defined as the usage of diabetes-related medical services in pharmacies and outpatient services within 1 year before the index hospitalization), medical insurance usage, length of stay at the index hospitalization, and the level of hospitals. Among these variables, the age and the length of stay at the index hospitalization were the continuous variables. The level of hospitals was a 3-level categorical variable (primary, secondary and tertiary hospital; the primary hospital served as the reference category). Other variables were categorical with 2 levels, female and negative results (e.g., CHF-free, family history free of diabetes) served as the reference categories. We used these likelihoods to calculate the predicted median probabilities of readmission for patients hospitalized at each readmission interval in each year. The impact factors of readmission were identified, and the differences between years and between time intervals were compared.
Next, we focused on the differences in 30-, 60-, and 90-day readmission rates between 2008 and 2013. We used the estimated coefficients of the adjusted readmission rate models for 2 years to perform Blinder–Oaxaca decomposition.[12] The Blinder–Oaxaca decomposition method, which was developed by Blinder and Oaxaca and generalized by Juhn, is a popular descriptive tool in labor economics and became a standard technique for decomposing gaps in outcomes between different groups. This method permits the decomposition of the readmission difference between 2008 and 2013 into (I) a part that is explained by observed variables and (II) a part attributable to differences in the estimated coefficients. We denoted the estimated probability of patients with readmission in 2008 and 2013 as  08 and
08 and  13, respectively. We followed the extensions of the Blinder–Oaxaca method for the nonlinear setting, and the change in 30-, 60-, and 90-day hospital readmission rates between the 2 years can be decomposed as
13, respectively. We followed the extensions of the Blinder–Oaxaca method for the nonlinear setting, and the change in 30-, 60-, and 90-day hospital readmission rates between the 2 years can be decomposed as
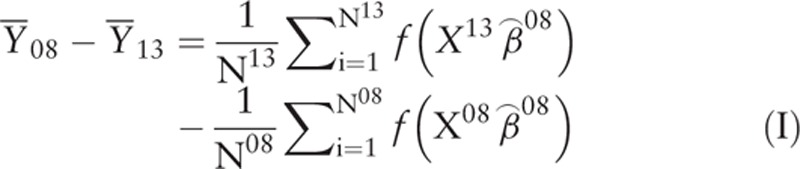 |
 |
where  were the vectors of coefficient estimates from the logistic model of the readmissions, estimated using data from year
were the vectors of coefficient estimates from the logistic model of the readmissions, estimated using data from year  were the vectors of explanatory variables for the hospital readmission of subject m in year i, and Ni were the sample sizes in year i.
were the vectors of explanatory variables for the hospital readmission of subject m in year i, and Ni were the sample sizes in year i.
The part (I) represented the change of hospital readmission rates between 2 years if the only changes that occurred were the observed variables (which we used to construct the baseline models). Several studies have focused on the explanatory variables of the first part and explained the second part (II) as troublesome or unobserved factors, such as certain policies or strategies.[13] Hereby, we also paid attention to the second part, as it would be interpreted as the results of the health system reform, which might have effects on hospital readmission rates in 2013 but not in 2008.
2.3. Statistical analysis
We first used χ2 tests and Wilcoxon tests to compare the characteristics of patients and hospitals between the patients with or without readmission. The comparisons of readmission rates between different time intervals and between years were performed by Kruskal–Wallis tests.
We built the patient-level multivariable models using a logistic model, adjusting for patients’ characteristics, hospital-level factors, and patients’ clinical characteristics. These variables included patients’ age, gender, type of diabetes, length of stay of the index admission, family history of diabetes, diabetes screening history, the reimbursement ratio of health care costs for each subjects, the total inpatient cost at the index hospitalization, the presence or absence of diabetes-related complications (including diabetic ketoacidosis, nonketotic hyperosmolar coma, diabetic cardiomyopathy, diabetic nephropathy, diabetic neuropathy, diabetic retinopathy, diabetic myonecrosis, and diabetic foot), hypertension, and CHF. A stepwise approach was used to select the best fitting model for each year and each time interval. All patients in a particular hospital were assigned that hospital's values for hospital-level variables. The accuracy of all built models was comparable to the existing models (see Table S1 in Appendix, Supplemental Digital Content, which illustrates the predicted accuracy of baseline model).
The costs in Chinese Yuan (CHY) were converted to United States Dollars (USD) using the exchange rate as of 2008 (USD$1 = CHY¥6.9444).
All reported P values are 2-sided, and P < .05 was considered statistically significant. All analyses were conducted with R Software 3.3.1 Version for Windows.
3. Results
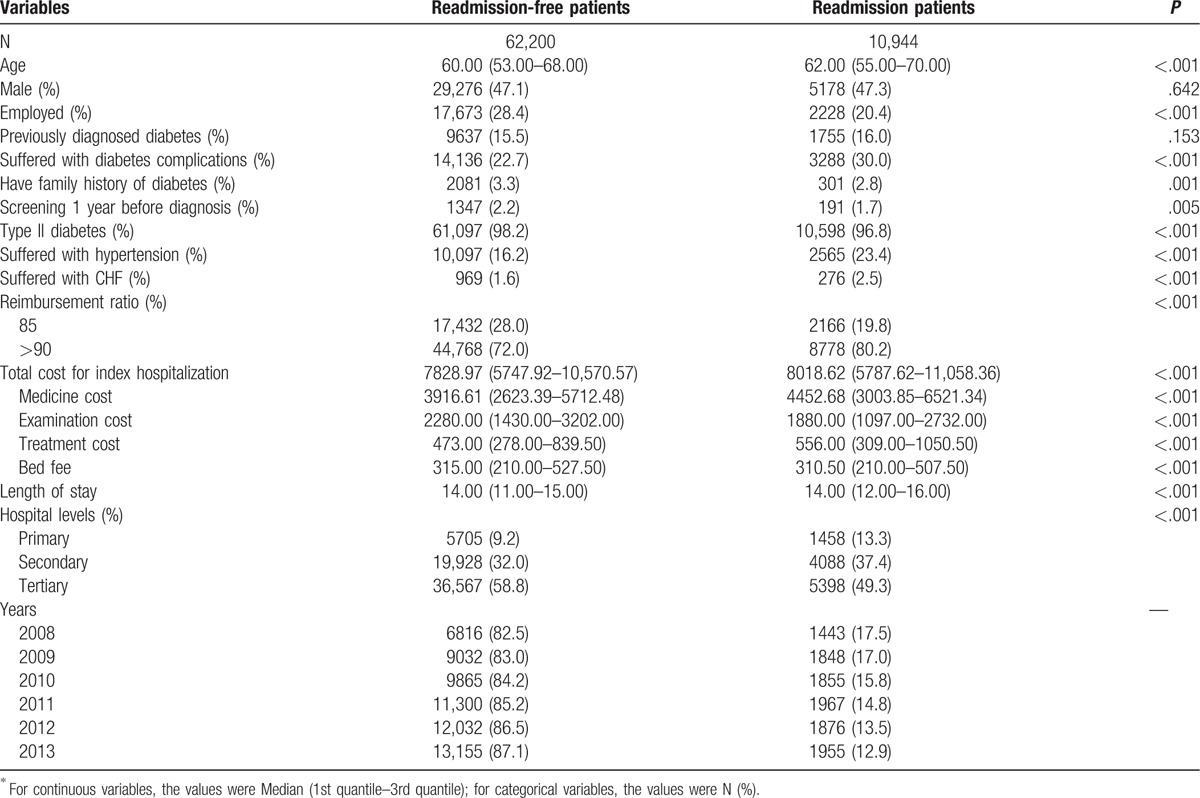
In our final sample, 73,144 patients with diabetes were admitted to hospitals from 2008 to 2013. In regard to the time-interval of readmission, compared with readmission-free patients, more readmitted patients were admitted to the primary and secondary hospitals (13.3% and 37.4%, respectively), were older (62.0 ± 15.0 years old), had higher total costs for the index hospitalization [CHY¥8018.62 (5787.62–11,058.36), USD$1154.69 (833.42–1592.41)], had higher prescribed medicine costs [CHY¥4452.68 (3003.85–6521.34), USD$641.19 (432.56–939.08)], and had higher treatment costs [CHY¥556.00 (309.00–1050.50), USD$80.06 (44.50–151.27)]. In addition, more readmitted patients suffered from diabetes complications (30.0%), hypertension (23.4%), and CHF (2.5%) and had higher out-of-pocket payment rates (85% with reimbursement rate higher than 90%). The readmission ratios gradually decreased by year: 17.5% in 2008, 17.0% in 2009, 15.8% in 2010, 14.8% in 2011, 13.5% in 2012, and 12.9% in 2013 (Table 1). The ratios of readmission at 90-day intervals were the highest compared with those at 30- and 60-day intervals (90-day readmission ratios from 2008 to 2013 were 9.2%, 9.2%, 9.2%, 9.1%, 8.3%, and 8.4%, respectively, all P < .001) (see Table S2 in Appendix, Supplemental Digital Content, which illustrates the readmission ratios at different time intervals).
Table 1.
Discharge characteristics by readmission status∗.
Several key characteristics for 30-, 60-, and 90-day rehospitalizations in each year are shown in Fig. 1 and Table S3–S5 in Appendix (Supplemental Digital Content, which illustrates the characteristics of patients and hospitals of discharge for 30-, 60-, and 90-day readmission). Generally, older patients, patients with diabetic complications, and patients who had a longer stay-time at the index hospitalization were more likely to be readmitted within 30 days after discharge from hospitals [Fig. 1A, the dark blue solid circles indicated the odds ratios (ORs) that were significantly higher than 1 in each year, P values for length of stay and suffering with complications were <.001 from 2008 to 2013, except for suffering with complications in 2008 and 2009, for which P values were .012 and .021, respectively], but patients with type 2 diabetes were more likely to be readmission-free in each year (Fig. 1A, the orange solid circles indicated the ORs that were significantly lower than 1 in each year, all P < .001 except for those in 2011 and 2012, for which P values were .004 and .014, respectively). Patients had a longer stay-time at the index hospitalization (ORs were significantly higher than 1 except for that in 2011), and those admitted to the tertiary hospitals were more likely readmitted within 31 to 60 days after discharge (ORs were significantly lower than 1, P values were .003, .001, <.001, <.001, .043, and .044 for 2008–2013, respectively) (Fig. 1B). Generally, a longer stay-time at the index hospitalization (ORs were significantly higher than 1 except for that in 2008), suffering from hypertension (ORs were significantly higher than 1 except for that in 2011), and advanced age (ORs were significantly higher than 1) had significant risk effects for readmission in each year within 61 to 90 days after discharge, and patients admitted to high-level hospitals at the index hospitalization were less likely to readmitted to the hospital (ORs were significantly lower than 1 for secondary hospitals except for those in 2008 and 2010 and were significantly lower than 1 for tertiary hospitals, P < .001) (Fig. 1C). We also found that a family history of diabetes, history of diabetes screening within 1 year before diagnosis, and a previous usage of diabetes-related medical services had no significant effects on hospital readmission (Fig. 1, the gray solid circles indicated ORs that were insignificant).
Figure 1.
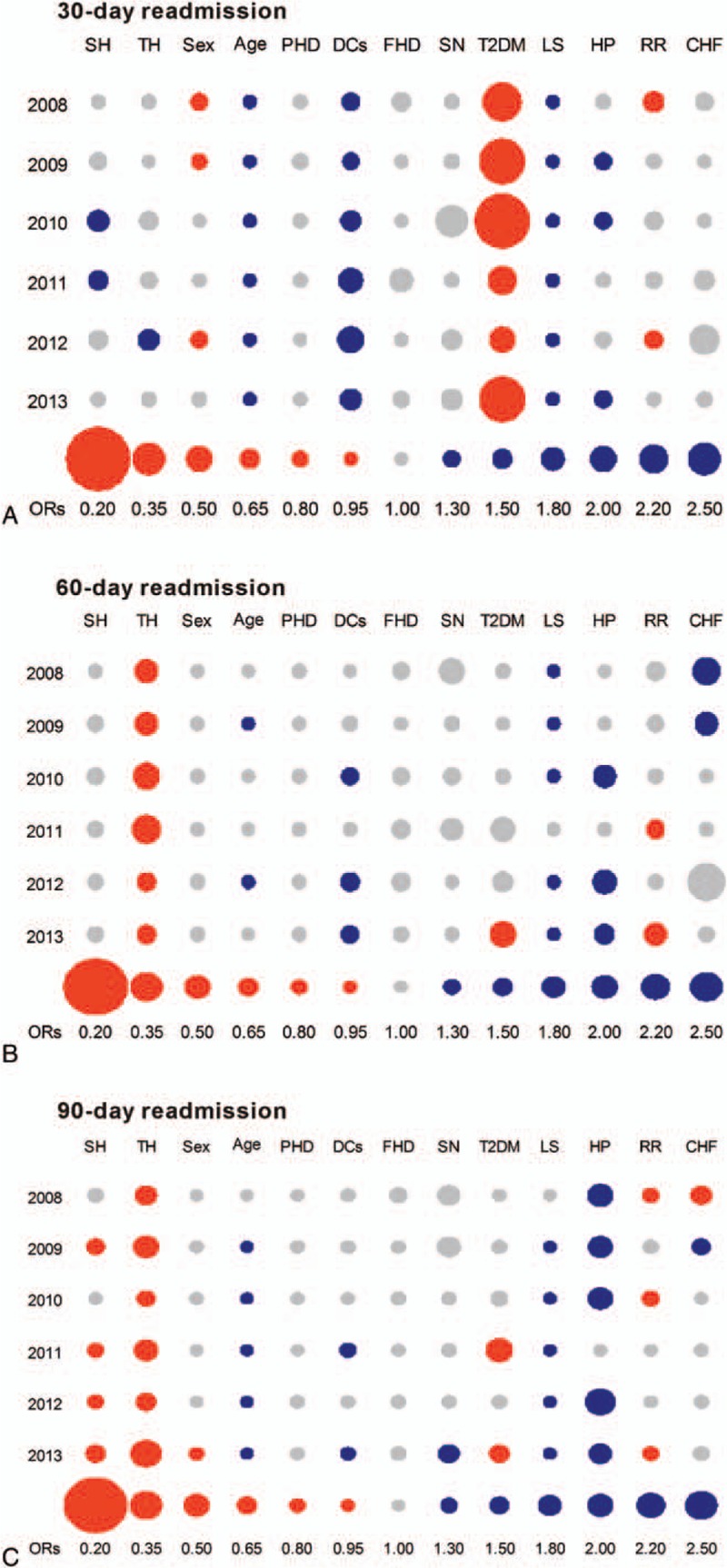
The effect factors for 30-, 60-, and 90-day readmission rates in each year. (A) shows the effect factors for 30-day readmission rates from 2008 to 2013. (B) shows the effect factors for 60-day readmission rates for 2008 to 2013. (C) shows the effect factors for 90-day readmission rates from 2008 to 2013. The dark blue solid circles indicate the ORs that were significantly higher than 1 in each year (P < .05), the orange solid circles indicate the ORs that were significantly lower than 1 in each year (P < .05), and the gray solid circles indicate the ORs that were insignificant (P > .05). CHF = congestive heart failure, DCs = diabetes complications, FHD = family history of diabetes, HP = hypertension, LS = length of stay, PHD = previous diagnosed diabetes, RR = reimbursement ratio, SH = secondary hospitals, SN = screening history of diabetes, T2DM = type 2 diabetes, TH = tertiary hospitals.
The predicted readmission rates generally decreased by year (Table 2, all P < .001), except for at the 90-day interval, which decreased in 2010 and slightly increased in 2013 (from 7.47% in 2012 to 7.65% in 2013) (Fig. 2, Table 2). The 90-day predicted readmission rates were the highest in each year, followed by the 30-day and 60-day readmission rates (Fig. 2, Table 2). Table 3 summarizes the results of the nonlinear Blinder–Oaxaca decomposition of the change in 30-, 60-, and 90-day hospital readmission rates between 2008 and 2013 based on the estimated coefficients. The predicted 30-, 60-, and 90-day readmission rates decreased by 2.19%, 2.28%, and 1.22%, respectively. We estimated that if the patients had been readmitted to the hospital, assuming their characteristics remained the same and that the only changes occurring in that year were those observable characteristics, then the readmission rates would decrease by 0.84%, 0.27%, and 0.18% for 30-, 60-, and 90-day intervals, respectively. Instead, the other unobserved changes and potential policy changes between the 2 years decreased the hospital readmission rates at a relatively larger level: 1.35%, 2.01%, and 1.04% for 30-, 60-, and 90-day intervals, respectively.
Table 2.
Predicted readmission rates at each time interval in 2008–2013.
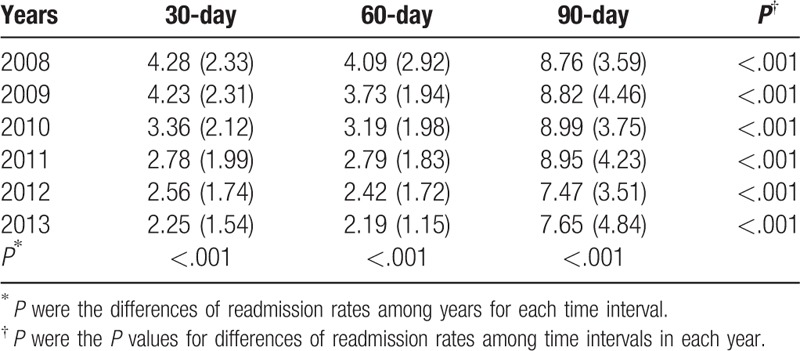
Figure 2.
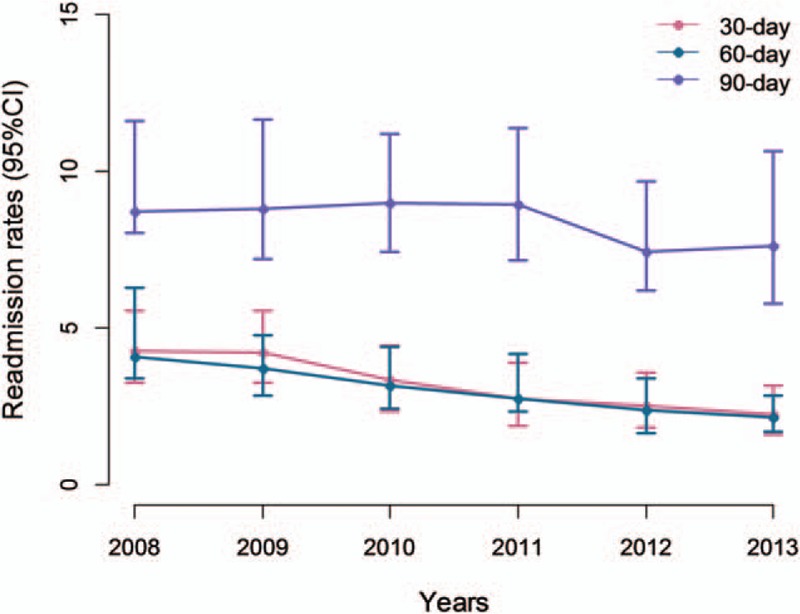
The variation of readmission rates between 2008 and 2013. The solid dots indicate the predicted readmission rates and the bars indicate 95% confidence interval at 30, 60, and 90-day intervals in each year. CI = confidence interval.
Table 3.
Nonlinear decomposition of changes in adjusted readmission rates in 2008–2013.
4. Discussion
Our previous study suggested that the increase in health care costs might be partly driven by the repeated use of hospital resources.[14] Therefore, controlling hospital readmission rates may have helped to balance the quality of health care services and the corresponding costs. However, hospital readmission rates have not yet been monitored officially. This lack of monitoring generally occurs because it is rare for quantitative studies to pay attention to readmission rates in Chinese cities, and the potential factors impacting readmission have rarely been recorded, such as the quality of health care services, the equity of the allocation of the health care sources, the patients’ discharge orientations, and the profiles of uninsured citizens.
Previous studies have reviewed hospital readmission rates focusing on the diseases that would easily involve acute exacerbation, such as acute myocardial infarction, heart failure, and pneumonia, and according to the best of our knowledge, this is the first study that unveils China's diabetes readmissions and its long-term variations using a large administrative dataset. We found that the prevalence of diabetes-readmission ratios had decreased from 17.5% in 2008 to 12.9% in 2013, which was higher than the ratios in developing countries but much lower than those in developed countries.[15–17] This decrease may be attributed to health care improvements in China targeting diabetes and/or the increased population with diabetes covered by the BMI, which would increase the pool of the studied population. Therefore, we estimated the readmission rates to confirm the decreases.
The 30-day readmission rate has generally been used as an indicator to assess the quality of health services by the governmental bodies of Canada, Australia, the United Kingdom, and New Zealand.[18–21] The primary reason is the large number of patients readmitted within this interval. In the current study, we found that the readmission rates were highest for 90-day readmissions, and the underlying reasons for readmission might also be different at different time intervals between 2 hospitalizations. We found that the primary drivers of 30-day readmission rates were associated with age and the characteristics of diabetes itself, but comorbidities and hospital characteristics, such as hospital level, may drive the longer interval of hospital admission. The hospital levels present a dividing line that distinguishes hospital quality levels in China, as the primary hospitals would only provide primary health care services to a specific local community, the secondary hospitals would provide primary health care services to more than one local community as teaching and research hospitals, and the tertiary hospitals would provide highly professionalized health care services without regional boundary limitations, as well as have the ability to train advanced professionals and conduct scientific research independently. These roles indicate that 90-day readmission rates, instead of 30-day readmission rates, could play roles in the evaluation of health care quality in China. Further studies, such as a study that evaluates the association between the quality of hospital performance and readmissions, are needed to confirm this assumption.
We found that 90-day readmission rates were considerably higher than the 30- and 60-day readmission rates after discharge. Unlike the 30- and 60-day readmission rates, which gradually decreased over the years, 2 peaks for the 90-day hospital readmission rates were found in 2010 and 2013, and the decrease of 90-day hospital readmission rates was only 1.22%, much lower than that of 30- and 60-day rates (2.19% and 2.28%, respectively). The current study included variables that explained 38.4%, 11.8%, and 14.8% of the decrease of 30-, 60-, and 90-day readmission rates, respectively. This finding suggests that targeting individual-level characteristics and diabetes care in the face of powerful population-level determinants would be expected to have a relatively large impact on the prevalence and distribution of 30-day readmission rates, but hospital level and other comorbid diseases are not enough to explain the change in readmission rate at longer intervals. Other plausible policy environments might also play a role, such as the change in hospital quality care under the health care system reform. Investigating these factors, specifically the change of readmission rates, is an important avenue for future research for examining evidence-based interventions.
China's central government reformed its health care system to establish a primary health care system providing universal health care services since 2009; therefore, we expected to see a decrease in the repeated use of hospital resources. However, in contrast to the primary medical facilities, admission to high-level hospitals prevents readmission as long-term readmission. This finding suggests that the primary health care system did not play a gatekeeping role to provide qualified services for patients with diabetes in Tianjin.
Previous studies have suggested that individuals covered by insurance are more likely to receive high-quality health care services,[22] which paradoxically results in either readmitting in hospitals or reducing the use of hospital resources.[23,24] Although the index hospitalization cost and reimbursement ratios were not included to the final model, our results still showed that readmitted patients had higher medical costs at the index hospitalization, and the majority of them had to pay less out-of-pocket costs for services. This finding indicates that instead of reducing the possibility of hospital readmission, possession of health insurance may motivate patients to repeatedly use medical services, and future studies need to assess causality and whether putting efforts into reducing reimbursements would result in fewer hospital readmissions and subsequent cost savings.
The current study has several limitations. The data we used were limited to administrative data, which might exclude undiagnosed diabetes patients at the index hospitalization and therefore bias the results.[25] Although our data on coexisting conditions were accurate and complete, they were limited to information contained in claims, with more detailed information on disease conditions, a mix of cases might have had a greater effect. As we lacked data on the transition of care and outpatient care, we could not assess whether our findings were due to inadequacies in these areas; thus, to guide further developments, updated monitoring might be needed in these areas.
5. Conclusion
The majority of the patients were readmitted at 61 to 90 days after the index hospitalization. Diabetes is related to short interval readmissions, but hospital-related factors and comorbid conditions may drive long-term readmissions. Using long-term readmissions instead of short interval readmissions to evaluate health care quality may be more appropriate in the Chinese setting. The 30- and 60-day readmission rates gradually decreased by years, a tendency that was not found for the 90-day readmission rates. The current study included variables that can explain a relatively large part of the decrease of the 30-day readmission rates only, thus, identifying more targeted factors for the decreases may help in controlling hospital readmission, particularly for the long-interval readmissions.
Acknowledgment
The authors were grateful to the Medical Insurance Association of Tianjin, China, for their valuable comments.
Supplementary Material
Footnotes
Abbreviations: BMI = basic medical insurance, CHF = congestive heart failure, CHY = Chinese Yuan, ICD-10 = International Classification of Diseases, Tenth Revision, Clinical Modification, TBMIRS = Tianjin Basic Medical Insurance Register System, USD = United States Dollar.
XL and YG contribute equally to this work.
Funding/support: This study was supported by grants from the National Natural Science Foundations of China [Grant number 71373175] and 2017 Ministry of Education Humanities and Social Science Planning.
The authors report no conflicts of interest.
Supplemental Digital Content is available for this article.
References
- [1].Zhou M, Astell-Burt T, Bi Y, et al. Geographical variation in diabetes prevalence and detection in China: multilevel spatial analysis of 98,058 adults. Diabetes Care 2015;38:72–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Morganstein DL, Tan S, Gore M, et al. Prevalence of diabetes in patients admitted to a cancer hospital. Br J Diabetes Vasc Dis 2012;12:178–80. [Google Scholar]
- [3].Zuckerman RB, Sheingold SH, Orav EJ, et al. Readmissions, observation, and the hospital readmissions reduction program. N Engl J Med 2016;374:1543–51. [DOI] [PubMed] [Google Scholar]
- [4].Epstein AM, Jha AK, Orav EJ. The relationship between hospital admission rates and rehospitalizations. N Engl J Med 2011;365:2287–95. [DOI] [PubMed] [Google Scholar]
- [5].Bayati M, Braverman M, Gillam M, et al. Data-driven decisions for reducing readmissions for heart failure: general methodology and case study. PLoS One 2014;9:e109264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Edmondson D, Green P, Ye S, et al. Psychological stress and 30-day all-cause hospital readmission in acute coronary syndrome patients: an observational cohort study. PLoS One 2014;9:e91477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Valenzuela JM, Seid M, Waitzfelder B, et al. Prevalence of and disparities in barriers to care experienced by youth with type 1 diabetes. J Pediatr 2014;164:1369–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Rumball-Smith J, Hider P. The validity of readmission rate as a marker of the quality of hospital care, and a recommendation for its definition. N Z Med J 2009;122:63–70. [PubMed] [Google Scholar]
- [9].Joynt KE, Jha AK. Thirty-day readmissions: truth and consequences. N Engl J Med 2012;366:1366–9. [DOI] [PubMed] [Google Scholar]
- [10].Chin DL, Bang H, Manickam RN, et al. Rethinking thirty-day hospital readmissions: shorter intervals might be better indicators of quality of care. Health Aff (Millwood) 2016;35:1867–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Yip WC, Hsiao WC, Chen W, et al. Early appraisal of China's huge and complex health-care reforms. Lancet 2012;379:833–42. [DOI] [PubMed] [Google Scholar]
- [12].Bauer TK, Sinning M. An extension of the Blinder–Oaxaca decomposition to nonlinear models. AStA Adv Stat Anal 2008;92:197–206. [Google Scholar]
- [13].Palangkaraya A, Yong J, Webster E, et al. The income distributive implications of recent private health insurance policy reforms in Australia. Eur J Health Econ 2009;10:135–48. [DOI] [PubMed] [Google Scholar]
- [14].Liu XQ, Yu WH, Fan LL. The characteristics of readmission in Tianjin China and its influencing factors. Tianjin Medical Insurance Seminar 2013;13:188–91. [Google Scholar]
- [15].Robbins JM, Webb DA. Diagnosing diabetes and preventing rehospitalizations: the urban diabetes study. Med Care 2006;44:292–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med 2009;360:1418–28. [DOI] [PubMed] [Google Scholar]
- [17].Joynt KE, Orav EJ, Jha AK. Thirty-day readmission rates for Medicare beneficiaries by race and site of care. JAMA 2011;305:675–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Statistics Canada. Health Indicators. Canada: Canadian Institute for Health Information; 2004. [Google Scholar]
- [19].National Health Ministers’ Benchmarking Working Group. First National Report on Health Sector Performance Indicator: Public Hospital: the State of Play. Canberra: Australian institute of Health and Welfare; 1996. [Google Scholar]
- [20].Dobrzanska L. Readmissions-an evaluation of reasons for unplanned readmissions of older people: a United Kingdom and international studies literature review. Qual Ageing Older Adults 2004;5:20–8. [Google Scholar]
- [21].New Zealand Health Technology Assessment. Acute Medical Admissions: a Critical Appraisal of the Literature. Christchurch: Christchurch School of Medicine; 1998. [Google Scholar]
- [22].Halterman JS, Montes G, Shone LP, et al. The impact of health insurance gaps on access to care among children with asthma in the United States. Ambul Pediatr 2008;8:43–9. [DOI] [PubMed] [Google Scholar]
- [23].Coffey RM, Misra A, Barrett M, et al. Congestive heart failure: who is likely to be readmitted? Med Care Res Rev 2012;69:602–16. [DOI] [PubMed] [Google Scholar]
- [24].Lasser KE, Hanchate AD, McCormick D, et al. The effect of Massachusetts health reform on 30 day hospital readmissions: retrospective analysis of hospital episode statistics. BMJ 2014;348:g2329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Zhang N, Yang X, Zhu X, et al. Type 2 diabetes mellitus unawareness, prevalence, trends and risk factors: National Health and Nutrition Examination Survey (NHANES) 1999–2010. J Int Med Res 2017;45:594–609. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


