Abstract
Rationale:
Trans-sacral epiduroscopic laser decompression (SELD) is reported to have strong positive short-term effects in controlling lower back pain (LBP) or radicular leg pain following herniated lumbar disc (HLD). However, little is known about the possible complications following SELD.
Patient concerns:
A 36-year-old man received SELD with YAG laser for controlling LBP and radicular pain due to HLD on L5-S1. However, after SELD, voiding and defecation difficulties and sensory deficits on the S3-5 dermatome were presented.
Diagnoses:
An areflexic neurogenic bladder was demonstrated by a urodynamic study four days after onset of sacral nerve root injury symptoms. In the electromyogram study, latency of electrically induced bulbocavernosus reflex (BCR) was delayed on both sides at four days after symptom onset. Based on the patient's symptoms and the results of the clinical evaluation, we diagnosed the patient as having an injury in the sacral nerve roots.
Interventions:
The patient was observed without any specific medication.
Outcomes:
Three months after symptom onset, the patient's voiding and defecation difficulties were nearly completely recovered.
Lessons:
In this study, we described a patient who showed neurogenic bladder and bowel and sensory deficits in the S3 to S5 dermatome due to sacral nerve root injury after SELD. During SELD, clinicians should be mindful of the possibility of injury to sacral nerve roots.
Keywords: bulbocavernosus reflex, herniated lumbar disc, sacral nerve root injury, trans-sacral epiduroscopic laser decompression, urodynamic study
1. Introduction
Trans-sacral epiduroscopic laser decompression (SELD) is a less invasive surgical alternative to traditional open surgery for herniated lumbar disc (HLD). In SELD, interventionists insert a steerable catheter into the epidural space via sacral hiatus, and then the epiduroscope and laser device are advanced through the inserted catheter. Under the direct guidance of epiduroscopy, using the laser device, decompression of the ruptured HLD and adhesiolysis in the epidural space are performed.[1–3] In previous studies, the positive effect of SELD was demonstrated in patients with lower back pain (LBP) and radicular leg pain following HLD.[1–3] However, the safety of SELD has not yet been fully confirmed.
Here, the authors present the first reported case of iatrogenic sacral root injury that occurred during a SELD procedure.
2. Case presentation
A 36-year-old man underwent SELD with a neodymium-yttrium-aluminum-garnet (Nd:YAG) laser in a local medical center due to LBP and right buttock pain (numeric rating scale: 6) lasting for 1 month. For the procedure, 1000 Joules of a 1414 nm Nd:YAG laser were delivered to the herniated disc. The LBP and right buttock pain were due to right central disc extrusion at L5–S1, which was observed in lumbar spine magnetic resonance imaging performed 1 month after pain onset (Fig. 1A). He had a history of lumbar surgery (discectomy and internal fixation on L4–5) due to HLD on L4–5, 10 years ago. Three days after SELD, he visited the Rehabilitation Department of a University Hospital for voiding, and defecation difficulties initiated on the day of the SELD procedure, although his pain was significantly reduced (numeric rating scale: 1). Self-voiding urine was measured at 100 mL, and residual urine was approximately 400 mL. On the physical examination, perianal and deep anal light touch and pinprick sensations (S4–5 dermatome) were reduced on both sides, and voluntary anal contraction was decreased. In addition, decrease of light touch and pinprick sensations on the S3 dermatome was noted. Contrary, manually examined bulbocavernosus reflex (BCR) and anal wink were preserved. No motor weakness or sensory deficit was observed in either leg. In the follow-up magnetic resonance imaging performed 1 day after SELD, no newly developed lesions, such as hematoma, infection, and aggravated HLD, were observed (Fig. 1B). The patient provided informed signed consent for participation in the study.
Figure 1.
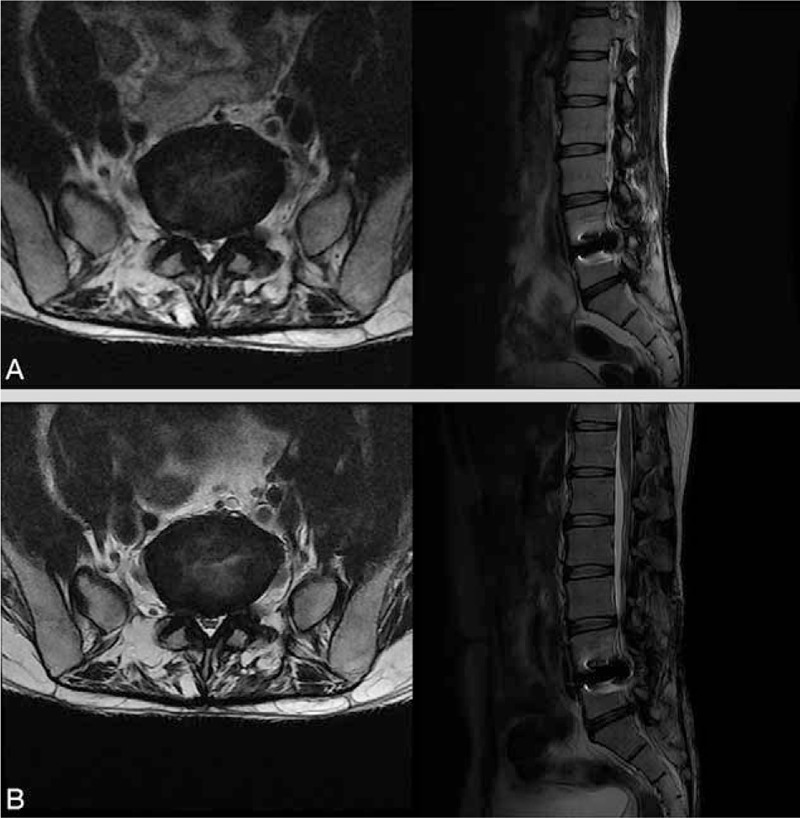
(A) Axial (left) and sagittal (right) T2-weighted lumbar spine MRI 1 month after the onset of lower back and right buttock pain showed right central disc extrusion at L5–S1. The artifact observed in the L4–5 level is due to the metal implant used in the operation for herniated lumbar disc 10 years ago. (B) In the follow-up MRI performed 1 day after SELD, no newly developed lesions, such as hematoma, infection, and aggravated HLD, were observed. HLD = herniated lumbar disc, MRI = magnetic resonance imaging, SELD = trans-sacral epiduroscopic laser decompression.
The urodynamic study (UDS) was performed 4 days after onset of voiding and defecation difficulties. In the UDS, the bladder was filled with normal saline at 20 mL/min filling rate. Vesical, abdominal, and detrusor pressures were monitored simultaneously during the filling phase. Bladder filling was terminated when 500 mL of saline were infused. Voiding desire was felt at the point the bladder was filled with 417 mL of saline, but self-voiding was not possible. During the UDS, no voluntary or involuntary detrusor contractions were found. Therefore, the patient was diagnosed with areflexic neurogenic bladder. In addition, we assessed the electrically induced BCR using electromyography 4 days after onset of voiding and defecation difficulties, and found delayed BCR latency in both the right and left sides (cut-off value: 45.0 ms[4]; right: 58.2 ms, left: 61.3 ms). Electromyography in both bulbocavernosus muscles showed reduced interference patterns but no active denervation potentials. Based on the patient's symptoms and the results of the clinical evaluation, we diagnosed the patient as having an injury in the sacral nerve roots.
Three weeks after onset of voiding and defecation difficulties, BCR latency was checked to be 50.0 and 52.2 ms in the right and left sides, respectively. Moreover, positive sharp wave (1+) was observed in both bulbocavernosus muscles, together with reduced interference patterns. Three months after symptom onset, the patient's voiding and defecation difficulties were nearly completely recovered. However, in the physical examination, sensory disturbance in the S3 to S5 dermatomes still remained.
3. Discussion
We reported a patient who had injury in the sacral nerve roots during SELD. Our patient presented with symptoms of sacral nerve root injury, including voiding and defecation difficulties and sensory deficits involving the S3 to S5 dermatomes. In our patient, delayed latency was observed in the electrically induced BCR, which demonstrates that the integrity of the sacral 2 to 4 nerve roots had deteriorated.[5] In addition, using UDS, the voiding difficulty in the patient was demonstrated to be an areflexic neurogenic bladder, one of the typical complications of sacral nerve root lesion. In addition, considering the fact that development of muscle membrane instability following neural injury occurs within 1 to 3 weeks and accompanied denervation potentials are manifested at least 1 week later after neural injury,[6] our findings that positive sharp wave, one of denervation potentials, was present in the 3-week EMG, but not in 4-day EMG indicated that the lesion in the sacral nerve roots was not a pre-existing condition, but a newly developed one.
For the SELD procedure, in our patient, the Nd:YAG laser was used. The Nd:YAG laser has a vaporizing effect, which is capable of destroying the herniated disc.[3,7] Although the Nd:YAG laser is considered to rarely cause significant thermal injury to the tissue structures during intraspinal procedures,[7] some studies have reported the occurrence of thermal injury to human tissues after the use of the Nd:YAG laser.[8,9] Likewise, we suggest that the sacral root lesion, in our patient, could be ascribed to thermal microinjury by the Nd:YAG laser. Another possibility might be that the sacral nerve roots may have been mechanically injured by the steerable catheter in the epidural space. Besides sacral nerve root injury, after epiduroscopic laser decompression, transient pain flare-up, infection, epidural hematoma, or incidental dural puncture can be occurred as complications.[2,10]
In this study, we reported a patient who had sacral root injury and presented with voiding and defecation difficulties and sensory deficits in the S3 to S5 dermatome after SELD. This is first study to report neural injury following SELD with Nd:YAG laser. Clinicians should be mindful of the possibility of this complication when performing SELD.
Footnotes
Abbreviations: BCR = bulbocavernosus reflex, HLD = herniated lumbar disc, LBP = lower back pain, Nd:YAG = neodymium-yttrium-aluminum-garnet, NRS = numeric rating scale, SELD = trans-sacral epiduroscopic laser decompression, UDS = urodynamic study.
The authors have no conflicts of interest to disclose.
References
- [1].Kim JD, Jang JH, Jung GH. Epiduroscopic laser disc and neural decompression. J Neurosurg Rev 2012;1:14–9. [Google Scholar]
- [2].Lee SH, Lee SH, Lim KT. Trans-sacral epiduroscopic laser decompression for symptomatic lumbar disc herniation: a preliminary case series. Photomed Laser Surg 2016;34:121–9. [DOI] [PubMed] [Google Scholar]
- [3].Zhao XL, Fu ZJ, Xu YG, et al. Treatment of lumbar intervertebral disc herniation using C-arm fluoroscopy guided target percutaneous laser disc decompression. Photomed Laser Surg 2012;30:92–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].lee DG, Kwak SG, Chang MC. Prediction of the outcome of bladder dysfunction based on electrically induced reflex findings in patients with cauda equina syndrome: a retrospective study. Medicine (Baltimore) 2017;96:e7014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Niu X, Wang X, Ni P, et al. Bulbocavernosus reflex and pudendal nerve somatosensory evoked potential are valuable for the diagnosis of cauda equina syndrome in male patients. Int J Clin Exp Med 2015;8:1162–7. [PMC free article] [PubMed] [Google Scholar]
- [6].Dumitru D, Amato A, Zwarts M. Electrodiagnostic Medicine. 2nd ed2002;Philadelphia: Lippincott Williams & Wilkins, 275. [Google Scholar]
- [7].Moon BJ, Lee HY, Kim KN, et al. Experimental evaluation of percutaneous lumbar laser disc decompression using a 1414 nm Nd:YAG laser. Pain Physician 2015;18:E1091–9. [PubMed] [Google Scholar]
- [8].Hunter JG, Dixon JA. Lasers in cardiovascular surgery-current status. West J Med 1985;142:506–10. [PMC free article] [PubMed] [Google Scholar]
- [9].Reszko AE, Magro CM, Diktaban T, et al. Histological comparison of 1064 nm Nd:YAG and 1320 nm Nd:YAG laser lipolysis using an ex vivo model. J Drugs Dermatol 2009;8:377–82. [PubMed] [Google Scholar]
- [10].Knight MT, Jago I, Norris C, et al. Transforaminal endoscopic lumbar decompression & foraminoplasty: a 10 year prospective survivability outcome study of the treatment of foraminal stenosis and failed back surgery. Int J Spine Surg 2014;8. [DOI] [PMC free article] [PubMed] [Google Scholar]


