Abstract
Sexual abuse is associated with a host of negative repercussions in adolescence. Yet, the possible mechanisms linking sexual abuse and negative outcomes are understudied. The purpose of this study was to investigate the relationships among self-blame, shame, coping strategies, posttraumatic stress disorder (PTSD), depressive symptoms, and suicidal ideation. The sample included 147 sexually abused adolescent girls between 14 and 18 years of age. A total of 66% of girls reached clinical score for PTSD and 53% reached clinical score for depressive symptoms. Close to half (46%) reported suicidal thoughts in the past three months. Shame was found to partially mediate the relationship between self-blame and PTSD. Shame and depressive symptoms were also found to partially mediate the relationship between self-blame and suicidal ideation. Results suggest that shame is a crucial target in interventions designed for sexually abused adolescent girls.
Keywords: Child sexual abuse, attributions, stigma, coping strategies, depression, self-blame
The consequences associated with child sexual abuse (CSA) have been studied for more than three decades now. The bulk of studies have shown more depressive symptoms, posttraumatic stress disorder (PTSD), and suicidal ideation (Hillberg, Hamilton-Giachritsis, & Dixon, 2011; Maniglio, 2009; Paolucci, Genuis, & Violato, 2001) among CSA victims than among the general population, especially during adolescence (Kendall-Tackett, Williams, & Finkelhor, 1993; Tyler, 2002). A recent review revealed a significant association between CSA and suicidal ideation or attempts in 49 out of 52 studies conducted with adolescents (Miller, Esposito-Smythers, Weismoore, & Renshaw, 2013). The risk for CSA increases substantially in late adolescence for girls with 36.8% of CSA occurring between their 15th and 17th birthday (Finkelhor, Shattuck, Turner, & Hamby, 2014).
According to Whiffen and MacIntosh (2005), now that the association between CSA and emotional distress has been documented, research should focus on identifying the underlying mechanisms involved in this link. In their review of the literature, shame, self-blame, and avoidance coping strategies were identified as crucial factors related to a heightened risk of emotional distress among victims of CSA. Yet, few studies have explored the impact of these factors on outcomes in sexually abused adolescents. The aim of the present study was to further investigate self-blame, shame, and coping strategies among sexually abused adolescent girls and their impact on PTSD, depression, and suicidal ideation by testing a mediational model.
Self-blame and shame
The Traumagenic Dynamic of Stigmatization model proposed by Finkelhor and Browne (1985) was the first to emphasize the role of shame and self-blame in the symptomatology of sexually abused youth. According to these authors, the negative connotations surrounding sexual abuse (taboo, shame, guilt, blaming the victim) are communicated to the victims by their environment, their aggressor, or society and are then integrated by the victims creating a stigma. Victims may feel they are to blame for the abuse and develop feelings of shame and guilt. They may also feel different from others, isolated, have low self-esteem, and engage in self-destructive behaviors, including suicide attempts.
Candice Feiring and her colleagues have highlighted the role of self-blame and shame as mediators of the relationship between sexual abuse characteristics and psychosocial adjustment (Feiring, Taska, & Lewis, 1996). Their longitudinal study of 160 CSA victims between eight and 15 years of age showed that shame and self-blame were not only strongly correlated with depressive and PTSD symptoms, even after controlling for age, gender, and CSA characteristics, but also mediated the relationship between the number of abusive events and depressive symptoms (Feiring, Taska, & Lewis, 1998). Self-blame was also found to predict depressive and PTSD symptoms in follow-up assessments conducted one and six years later (Feiring & Cleland, 2007; Feiring, Taska, & Chen, 2002). Shame was also related to PTSD symptoms after 6 years (Feiring & Taska, 2005). Furthermore, shame was found to mediate the relationship between self-blame and PTSD symptoms and self-blame predicted PTSD after controlling for age, gender, and CSA characteristics (Feiring et al., 2002). More recently, using a six-year longitudinal design, Simon, Feiring and Cleland (2014) showed that self-blame and shame shortly after the abuse and one year later significantly increased the likelihood of using avoidant coping strategies six years later.
Coping Strategies
Sarah Ullman and her colleagues conducted a series of studies on the psychological adjustment of women sexually abused during childhood or adulthood. Self-blame and maladaptive coping strategies were found to be related to more severe depression and PTSD symptoms (Ullman, Filipas, Townsend, & Starzynski, 2007; Ullman, Peter-Hagene, & Relyea, 2014) and to predict suicidal ideation (Ullman & Najdowski, 2009). Maladaptive coping strategies were also found to mediate the relationship between CSA severity and depressive and PTSD symptoms, but self-blame did not (Ullman et al., 2014).
The attribution theory of Weiner (1985) is consistent with the Traumagenic Dynamic of Stigmatization model and can be used to understand not only how internal self-blame can lead to shame (Feiring et al. 1996; Feiring, Taska, & Lewis, 2002; Lewis, 2016; Ullman et al. 2014), but also the relevance of coping strategies in CSA victims. It posits that the perception of failure, including internal or external attribution of failure, has a strong influence on an individual’s emotional experience (i.e., anger, guilt, hopelessness, shame). The affect experienced will then influence the individual’s behaviors. In accordance with this theory, we hypothesized that victims who perceive themselves as responsible for the abuse will be more likely to experience shame and rely on maladaptive coping which in turn will be linked to negative outcomes. The outcomes investigated are depression, PTSD and suicidal ideation. In contrast, we expect that victims who do not perceive themselves as responsible will not experience shame and will rely on more efficient coping that will be associated with fewer symptoms.
Relationships among self-blame, shame, and coping strategies in explaining CSA symptoms
The relationships between coping strategies, self-blame, and shame have rarely been studied during childhood and adolescence. Yet, during adulthood avoidance coping has been found to mediate the relationship between self-blame and psychological distress (Frazier, Mortensen, & Steward, 2005) and PTSD symptoms (Cantón-Cortés, Cantón, Justicia, & Cortés, 2011).
The complex relationships between self-blame, feelings of shame, coping strategies, and psychological adjustment are compatible with a cognitive behavioral model but they need to be further investigated among sexually abused adolescent girls. Moreover, although various studies have shown the impact of self-blame and shame on the symptomatology of CSA victims, more precisely on PTSD and depressive symptoms, we know little about their impact on suicidal ideation and attempts. According to a recent review, sexual abuse is the adverse life event most consistently and strongly associated with suicide among young people aged 10–25 years (Serafini et al., 2015). Suicide is the first worldwide cause of death among adolescent girls aged 15–19 years (Patton et al., 2009). A recent meta-analysis also indicates that between 20% and 22% of suicide and suicidal attempts among women can be imputed to CSA (Devries et al., 2014).
Depressive mood is a well-known risk factor for suicidal ideation and behaviors, along with PTSD (Beautrais, 2000; Devenish, Berk, & Lewis, 2016; Krysinska & Lester, 2010; Miller & Eckert, 2009). Recent studies also show that among sexually abused adolescents, not only do depressive and PTSD symptoms predict suicidal ideation (Brabant, Hébert, & Chagnon, 2014), but depressed mood also mediates the relationship between sexual abuse and suicidal ideation (Sigfusdottir, Asgeirsdottir, Gudjonsson, & Sigurdsson, 2013). Against this backdrop, the aim of the present study was to investigate the effect of self-blame, shame, and coping strategies on depressive symptoms, PTSD, and suicidal ideation among sexually abused adolescent girls. We first hypothesized that shame and coping strategies will mediate the relationships between self-blame and PTSD, depressive symptoms, and suicidal ideation. We also hypothesized that depressive and PTSD symptoms will mediate the relationship between self-blame and suicidal ideation.
METHOD
Participants and Procedure
A sample of 147 female teenagers aged between 14 and 18 years was recruited to participate in a larger study on the diversity of profiles among victims of CSA. Teenagers were recruited following disclosure of CSA in four intervention centers in the province of Quebec, Canada: the Clinique de l’adolescence of the Centre Hospitalier Universitaire (CHU) Sainte-Justine, Parent-Unis Repentigny (PURL), the Centre d’Intervention en Abus Sexuels pour la Famille (CIASF), and the Centre Jeunesse de la Mauricie et du Centre du Québec (CJMCQ). Written consent was obtained by a research assistant after explaining the purpose of the study. The questionnaires were then completed at the intervention center, or if participant preferred in another location (home, research center). A research assistant provided assistance if required. Participants received a $30 gift card and a list of relevant resources available. The study was approved by the Ethics Committee of the Centre Hospitalier Universitaire Sainte-Justine. Sociodemographic characteristics of the sample are presented in Table 1.
Table 1.
Sociodemographic Characteristics
| Characteristics | Participants (%) |
|---|---|
| Age | |
| 14 | 25.9 |
| 15 | 27.2 |
| 16 | 19.0 |
| 17 | 25.9 |
| 18 | 2.0 |
| Nationality | |
| Born in Canada from parents born in Canada | 65.2 |
| Born in Canada with one or two parents born outside Canada | 21.2 |
| Born outside of Canada | 13.6 |
| Parents’ nationality | |
| Canadian | 71.4 |
| Caribbean | 9.5 |
| Latin American | 8.2 |
| Other | 10.9 |
| Language at home | |
| French | 86.4 |
| English | 4.8 |
| Other | 8.8 |
| Family structure | |
| Intact family | 20.4 |
| Single-parent family | 46.3 |
| Recomposed or foster family | 33.3 |
Measures
Shame
The Abuse Specific Shame Questionnaire (ASSQ) (Feiring et al., 1998) was used to assess feelings of shame. The scale contains four items rated on a 3-point scale: not true, somewhat true, and very true. Sample items include: “What happened makes me feel dirty.” The internal consistency for this measure is adequate (α = .85) (Feiring et al., 2002) and .75 in the present sample.
Self-blame attributions
The Abuse Attribution Inventory (AAI) (Feiring et al., 2009) was used to assess abuse-specific self-blame with eight items rated on a 3-point scale : not true, somewhat true, and very true. Sample items include: “It happened to me because I am not a cautious person.” Internal consistency of the global score was found to be satisfactory in the original study (α = .75–.80; Feiring et al., 2009) as well as in the present study (α = .83).
Coping strategies
The brief version of the Ways of Coping Questionnaire (WCQ) (Folkman & Lazarus, 1988) was adapted to assess abuse-specific coping strategies. It contains 12 items rated on a 4-point scale: does not apply or not used, used somewhat, used quite a bit, and used a great deal. Three subscales are derived from the items: Social support seeking (α = .75), Problem solving (α = .78), and Avoidance coping (α = .69).
Posttraumatic stress disorder
The Children’s Impact of Traumatic Events Scale II (CITES II) (Wolfe, 2002) (French version by Hébert, 2006) was used to assess PTSD symptoms. The PTSD scale was designed to cover all symptoms identified in the Diagnostic and Statistical Manual of Mental Disorders Fourth Edition (American Psychiatric Association, 1994), and diagnostic status can be calculated for the PTSD symptom criteria (Wolfe, 2007). Three dimensions of PTSD are considered: Intrusive thoughts, Avoidance, and Hyperarousal and evaluated on a 3-point scale: none, some, or a lot. The global PTSD score (46 items) was used in the analyses (α = .95).
Depressive Symptoms
The Affective problems scale from the Youth Self Report (YSR) (Achenbach & Rescorla, 2001) was used to assess depressive symptoms. Clinical scores can be derived from the YSR (T scores > 70). Ferdinand (2008) and Nakamura, Ebesutani, Bernstein and Chorpita (2009) concluded that the affective problem scale from CBCL and YSR was a better measure of major depressive disorder than the anxiety/depressive scale. This scale originally contains 13 items, including the suicidal ideation item (question 91). In order to properly analyze the relationship between depressive symptoms and suicidal ideation, this item was analyzed separately. The revised scale contains 12 items with a Cronbach alpha of .80.
Suicidal ideation
One question (“I think about killing myself”) from the YSR was used to assess suicidal ideation in the past three months. The question is rated on a 3-point scale: not true, somewhat or sometimes true, and very true or often true. Participants who endorsed “not true” were attributed a score of 0 while other participants were given a score of 1.
Abuse characteristics
Characteristics of the abuse were assessed using the French version of the History of Victimization Form (HVF) (Wolfe, Gentile, & Bourdeau, 1987; Parent & Hébert, 1995) completed by the caseworker. The data collected include severity and duration of the abuse, relationship to abuser, age and sex of abuser, presence of violence, threat, drugs, number of reported CSA situations, time passed since last episode of CSA. The information regarding abuse characteristics is presented in Table 2.
Table 2.
Sexual Abuse Characteristics
| Characteristics | Participants (%) |
|---|---|
| Age at first abuse | |
| 13 or less | 27.8 |
| 14 | 19.8 |
| 15 | 14.3 |
| 16 | 15.1 |
| 17 | 23.0 |
| Severity of abuse | |
| Less severe | 2.6 |
| Severe | 2.9 |
| Very severe | 90.5 |
| Duration of abuse | |
| One episode | 63.0 |
| A few events | 10.2 |
| Chronic/Repetitive | 26.8 |
| Use of threat, drug, violence, or reward | |
| No threat, violence, drug, or reward | 28.6 |
| Verbal threat | 23.2 |
| Force or physical violence | 22.9 |
| Alcohol or drug | 27.9 |
| Gift or reward | 6.3 |
| Number of aggressors | |
| 1 | 82.9 |
| 2 | 8.9 |
| 3 | 8.2 |
| Sex of aggressor | |
| Men | 97.6 |
| Women | 1.6 |
| Men and Women | 0.8 |
| Age of aggressor | |
| Less than 15 years | 3.3 |
| 15–19 | 32.7 |
| 20–59 | 61.5 |
| 60 or more | 2.5 |
| Aggression intra or extra familial | |
| Intra familial | 27.2 |
| Extra familial | 72.8 |
| Aggressor living with victim at time of abuse | |
| Yes | 24.8 |
| No | 75.2 |
| Delay between last episode and evaluation | |
| 0 month | 5.7 |
| 1 month | 52.0 |
| 2–5 months | 16.3 |
| 6 months and more | 26.0 |
Sociodemographic variables
The sociodemographic questionnaire includes items on adolescents’ age, nationality, parents’ nationality, language, and family structure (see Table 1).
RESULTS
Preliminary analyses and correlations among variables
Analyses were performed with SPSS 22 software. The Skewness and Kurtosis tests revealed a normal distribution for every variable tested: between −0.13 and 3.84 for Skewness, between −0.38 and 3.00 for Kurtosis. Suicidal ideation, assessed with only one item on a 3-point scale, had the highest skewness. Skewness is under 3 for all other variables. Symptom scores were in the clinical range for a large percentage of girls: 53.10% for the Affective Problems Scale, 66.40% for PTSD, while 45.80% of them reported suicidal thoughts in the past 3 months. Correlations between self-blame, shame, avoidance, PTSD symptoms, depressive symptoms, and suicidal ideation were statistically significant (see Table 3). However, problem-solving and social support seeking were both eliminated from further analysis since they were not correlated with outcomes variables (Baron & Kenny, 1986).
Table 3.
Summary of Intercorrelations, Means and Standard Deviations for Scores of Self-Blame, Shame, Avoidance, PTSD Symptoms, Depressive Symptoms, and Suicidal Ideations
| Variables | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | M | SD |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. Self-blame | - | 5.38 | 4.00 | |||||||
| 2. Shame | .395*** | - | 4.04 | 2.46 | ||||||
| 3. Avoidance coping | .330*** | .527*** | - | 7.74 | 3.08 | |||||
| 4. Social support seeking | .118 | .034 | .134 | - | 6.38 | 3.21 | ||||
| 5. Problem solving | .127 | .185* | .301* | .460** | - | 6.48 | 3.43 | |||
| 6. PTSD symptoms | .385*** | .658*** | .520*** | −.059 | .092 | - | 51.30 | 18.93 | ||
| 7. Depressive symptoms | .378*** | .404*** | .301*** | −.158 | −.142 | .596*** | - | 10.80 | 5.13 | |
| 8. Suicidal ideation | .407*** | .398*** | .201* | −.109 | −.119 | .388*** | .605*** | - | 0.60 | 0.73 |
Note. The self-blame score is from the Abuse Attribution Inventory (AAI) (Feiring et al., 2009); the shame score from the Abuse Specific Shame Questionnaire (ASSQ) (Feiring et al., 1998); the coping strategies scores are from the Ways of Coping Questionnaire (WCQ) (Folkman & Lazarus, 1988); the PTSD symptom score from Children’s Impact of Traumatic Events Scale II (CITES II) (Wolfe, 2002); the depressive symptoms score from the Affective problems scale from the Youth Self Report (YSR) (Achenbach & Rescorla, 2001); and the suicidal ideations from the Youth Self Report (YSR) (Achenbach & Rescorla, 2001).
p < .05,
p < .01,
p < .001
Mediation and path analysis
Shame, self-blame, and avoidance were significantly correlated with depressive symptoms, PTSD, and suicidal ideation. However, avoidance coping only explained 0.36% of the variance of suicidal ideation when self-blame, shame, depressive symptoms, and PTSD were included into the model. Moreover, PTSD symptoms did not explain a significant percentage of the variance of suicidal ideation (1.08%) when self-blame, shame, and depressive symptoms were included into the model. Avoidance coping and PTSD were therefore rejected from the model explaining suicidal ideation.
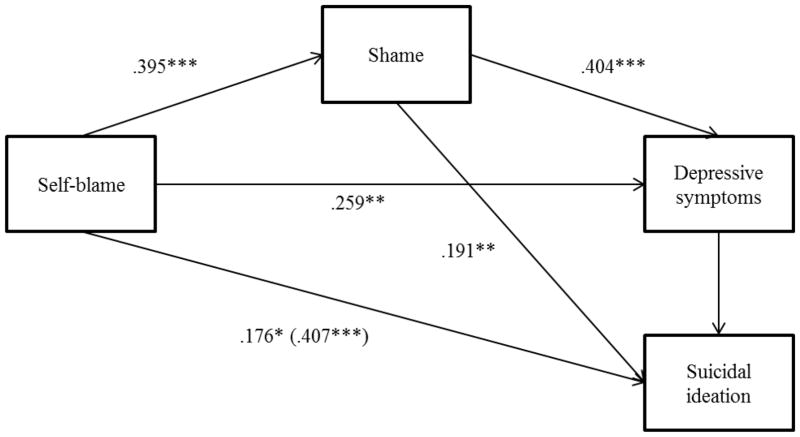
A path analysis was performed using linear regressions in accordance with Wonnacott and Wonnacott’s (1995) procedure to examine the effect of shame and depressive symptoms on the relation between self-blame and suicidal ideation. A total of 41.60% of the variance of suicidal ideation was explained by self-blame, shame, and depressive symptoms. Self-blame was a significant predictor of suicidal ideation (β = .41, SE = .01, p < .001) and shame (β = .40, SE = .05, p < .001). Shame was a significant predictor of depressive symptoms (β = .40, SE = .16, p < .001), and depressive symptoms a significant predictor of suicidal ideation (β = .60, SE = .01, p <.001). The standardized indirect effect was (.40) (.40) (.60) = .10. The Sobel test (Baron & Kenny, 1986) indicated that shame and depressive symptoms mediated (z = 2.06, p < .05) the relation between self-blame and suicidal ideation. The total effect of self-blame on suicidal ideation including shame and depressive symptoms as mediators was .18 + .15 + .07 + .10 = .50. Finally, results of the path analysis show a partial mediation of shame and depressive symptoms on the relationship between self-blame and suicidal ideation (see Figure 1) since the direct effect of self-blame on suicidal ideation was still significant after controlling for shame and depressive symptoms (β = .17, SE = .01, p < .05).
Figure 1.
Path Analysis of Suicidal Ideation through Self-blame, Shame, and Depressive Symptoms
* p < .05, ** p < .01, *** p < .001
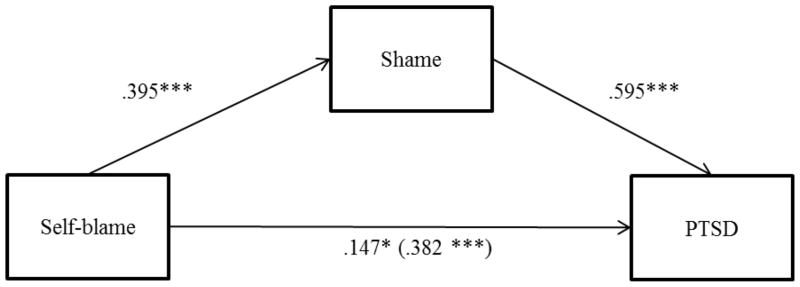
Because PTSD was rejected from the previous model, we further investigated the effect of shame and avoidance in its relationship to self-blame, and a path analysis was conducted with self-blame, shame, and avoidance as predictors of PTSD. Avoidance coping was excluded from the model because shame was found to completely mediate the relationship between self-blame and avoidance coping, and avoidance coping didn’t predict enough variance (3.88%) when self-blame and shame were included into the model. A mediation analysis was performed using Preacher and Hayes’ (2008) procedure to examine the effect of shame on the relationship between self-blame and PTSD symptoms. Data were transformed into Z scores to get standardized coefficients. A total of 45.20% of the variance of PTSD symptoms was explained by self-blame and shame. Self-blame was a significant predictor of PTSD symptoms (β = .38, SE = .08, p < .001) and a significant predictor of shame (β = .40, SE = .08, p < .001). Shame was a significant predictor of PTSD symptoms (β = .60, SE = .07, p < .001). The indirect effect was tested using a bootstrap estimation approach with 5,000 samples (Preacher & Hayes, 2004). Results of the mediation analysis confirmed that shame partially explained the relation between self-blame and PTSD symptoms (see Figure 2) (β = .24, SE = .05, 95% CI [.14, .35]). The direct effect of self-blame on PTSD symptoms was still significant after controlling for shame (β = .15, SE = .07, p < .05).
Figure 2.
Partial Mediation of the Relationship between Self-blame and PTSD through Shame
* p < .05, ** p < .01, *** p < .001
DISCUSSION
The aim of our study was to examine the effect of self-blame, shame, and coping strategies on depressive symptoms, PTSD, and suicidal ideation among adolescent girls who were identified as victims of CSA. Consistent with past studies, self-blame, shame, and avoidance coping were all significantly correlated with depressive and PTSD symptoms as well as with suicidal ideation.
We hypothesized that shame and coping strategies would mediate the relationships between self-blame and PTSD, depressive symptoms, and suicidal ideation. Consistent with previous research conducted with sexually abused children and adults, self-blame and shame were both found to be predictors of PTSD, depressive symptoms, and suicidal ideation (Feiring & Cleland, 2007; Feiring & Taska, 2005; Feiring et al., 2002; Ullman & Najdowski, 2009). Shame was found to partially mediate the relationship between self-blame and PTSD with self-blame and shame predicting as much as 45% of the variance of PTSD scores. Feiring et al. (2002) reported similar findings. Shame and depressive symptoms were also found to partially mediate the relationship between self-blame and suicidal ideation. Close to 42% of the variance of suicidal ideation was explained by self-blame, shame, and depressive symptoms. As expected, self-blame and shame were both important predictors of symptoms with shame partially mediating the effect of self-blame. These findings seem to confirm that internal attributions for a negative event lead to shame and shame leads to psychopathology (Lewis, 2016).
But why do sexually abused adolescent girls blame themselves? Although we may expect that attitudes towards victims of CSA have somewhat changed with increased awareness, according to the Traumagenic Dynamic of Stigmatization model (Finkelhor & Browne, 1985), negative reactions and lack of support from family and peers have a strong impact on the victims. Bedera and Nordmeyer (2015) also pointed out that rape prevention may be presented by some as an easy task: don’t walk alone at night, don’t trust strangers, trust your instincts, be aware of surroundings, and say “no.” As such, sexually abused girls who were told avoiding rape is easy may be likely to feel ashamed for not being able to avoid or escape the situation. Moreover, when making an internal attribution for a failure, girls have been found to make more global attributions than boys (Levine & Conway, 2010; Lewis, 2016). These results suggest that self-blame, shame, and myths about sexual abuse should be targeted in interventions with sexually abused adolescents.
Recently, Brabant, Hébert and Chagnon (2014) found that PTSD predicted suicidal ideation among sexually abused adolescent girls, even after controlling for depressive symptoms. In this study, PTSD did not predict suicidal ideation when self-blame, shame, and depressive symptoms were included into the model. Self-blame and shame seem to be better predictors of suicidal ideation than PTSD in our sample, but note that Brabant et al. (2014) used a 19-item measure of suicidal ideation and relied on a one year longitudinal design. A comprehensive measure and a longitudinal design may be necessary to assess the impact of PTSD on suicidal ideation.
Among coping strategies, only avoidance coping was correlated with symptom scores. This finding is consistent with those of previous studies (Bal, Van Oost, De Bourdeaudhuij, & Crombez, 2003; Cantón-Cortés & Cantón, 2010; Hébert, Tremblay, Parent, Daignault, & Piché, 2006). However, avoidance coping was rejected from both models when shame and self-blame were included. This is an interesting result considering that none of the previous studies had included shame, self-blame, and avoidance coping to examine their impact on symptom scores. These results suggest that shame and self-blame might be more important predictors of CSA symptoms than avoidance coping at least shortly after disclosure. Yet self-blame and shame could gradually increase the probability of using avoidant coping and in turn avoidant coping could increase symptoms. This possibility needs to be investigated using a longitudinal design.
Sexually abused adolescent girls are at high risk of suicidal ideation and attempts (Devries et al., 2014; Miller et al., 2013). In our sample, close to half of participants (46%) reported suicidal ideation in the past three months. Scores obtained on the depressive and PTSD symptom scales were also high. More than half of the girls reached clinical scores of depression (53%) and PTSD (66%). In comparison, the National Comorbidity Survey Replication Adolescent Supplement (NCS-A) reported a prevalence among adolescent girls (13–18) of 16% for major depressive disorder or dysthymia, 8% for PTSD, and 15% for suicidal ideation (Merikangas et al., 2010; Nock et al., 2013). While direct comparison is precluded given differences in the measures used and the severity of CSA experienced in the present sample, our results nevertheless suggest that the prevalence of these disorders is much higher in our sample. A significant proportion of sexually abused girls seem to show severe symptoms impairing their functioning and are clearly in need of services.
Certain limitations of this study need to be mentioned. Participants were assessed only once and, except for abuse characteristics, only self-report questionnaires were used. Our sample included adolescent girls who sought services and 91% of them had experienced severe abuse. They may not be representative of adolescents who have experienced other forms of sexual abuse. Another limitation is the measure of suicidal ideation that contains only one item. To further investigate the impact of self-blame, shame, and coping strategies on sexually abused adolescent girls, longitudinal studies, including a multiple-informant perspective, should be conducted. Following the Traumagenic Dynamic of Stigmatization model (Finkelhor & Browne, 1985), parents’ and peers’ reactions to disclosure and social support as well as their impact on self-blame, shame, and outcomes should also be examined.
In addition, other outcomes not considered in the present study need to be analyzed. Recently, Dyer et al. (2016) studied shame among adults with dissociative identity disorder and found that they presented a different profile of shame compared to a complex trauma sample. Feiring et al. (2009) also found that self-blame and shame predicted dissociation. Dissociative symptoms may be relevant in the understanding of shame, self-blame, avoidance, and symptoms among CSA victims. Likewise, more than avoidant coping, poor emotion regulation skills could also be a crucial factor as recent studies have shown among sexually abused children (Langevin, Cossette, & Hébert, 2016) and adults (Ullman et al., 2014).
Despite these limitations, this study provides unique data on the impact of self-blame, shame, and avoidance on PTSD, depressive symptoms, and suicidal ideation among sexually abused adolescent girls. Not only has this study showed the importance of assessing suicidal ideation in addition to PTSD and depression among sexually abused adolescent girls, but it also underscores that interventions targeting self-blame and shame should not be neglected. In fact, our data suggest that self-blame and shame should be prioritized in interventions with this population.
Acknowledgments
This research was conducted as part of the first author’s PhD thesis and was supported by a grant from the Canadian Institutes of Health Research (CIHR) awarded to Martine Hébert, PI (#103944). The first author was supported by a scholarship from the Sexual and Violence Team (ÉVISSA) and the Interdisciplinary Research Centre on Intimate Relationship Problems and Sexual Abuse (CRIPCAS).
Biographies
Stéphanie Alix, Department of Psychology, Université du Québec à Montréal; Louise Cossette, Department of Psychology, Université du Québec à Montréal; Martine Hébert, Department of Sexology, Université du Québec à Montréal; Mireille Cyr, Department of Psychology, Université de Montréal; Jean-Yves Frappier, Pediatric Department, Centre Hospitalier Universitaire Sainte-Justine, Université de Montréal.
Stéphanie Alix, BS, is a doctoral student in the Department of Psychology at the Université du Québec à Montréal. Her research interests concern the factors influencing the impact of sexual abuse in adolescent girls.
Louise Cossette, PhD, is professor in the Department of Psychology at Université du Québec à Montréal. Her research interests concern gender and emotional development.
Martine Hébert, PhD (psychology), is the Canada Research Chair in Interpersonal Traumas and Resilience. She is full professor in the Department of Sexology at Université du Québec à Montréal and director of the Research Team Équipe violence et santé (ÉVISSA: Research Team on Sexual Violence and Health).
Mireille Cyr, PhD, is full professor at Université de Montréal, Québec, and director of the Centre de recherche sur les problèmes conjugaux et les agressions sexuelles (CRIPCAS: Research Centre on Intimate Relationship Problems and Sexual Abuse).
Jean-Yves Frappier, MD., FRCPC, MSC, is professor and director at the Pediatric Department of the Université de Montréal and Centre hospitalier universitaire Ste-Justine in Montréal.
Footnotes
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation [Ethics Committee of the Centre Hospitalier Universitaire Sainte-Justine] and with the Helsinki Declaration of 1975, as revised in 2000. Informed consent was obtained from all participants for being included in the study.
References
- Achenbach TM, Rescorla LA. An Integrated System of Multi-informant Assessment. ASEBA, University of Vermont; 2001. Manual for the ASEBA School-Age Forms & Profiles. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: Author; 1994. [Google Scholar]
- Bal S, Van Oost P, De Bourdeaudhuij I, Crombez G. Avoidant coping as a mediator between self-reported sexual abuse and stress-related symptoms in adolescents. Child Abuse & Neglect. 2003;27(8):883–897. doi: 10.1016/s0145-2134(03)00137-6. https://doi.org/10.1016/S0145-2134(03)00137-6. [DOI] [PubMed] [Google Scholar]
- Baron RM, Kenny DA. The moderator–mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51(6):1173–1182. doi: 10.1037//0022-3514.51.6.1173. http://doi.org/10.1037/0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Beautrais AL. Risk factors for suicide and attempted suicide among young people. Australian and New Zealand Journal of Psychiatry. 2000;34(3):420–436. doi: 10.1080/j.1440-1614.2000.00691.x. https://doi.org/10.1080/j.1440-1614.2000.00691.x. [DOI] [PubMed] [Google Scholar]
- Bedera N, Nordmeyer K. « Never go out alone »: An analysis of college rape prevention tips. Sexuality & Culture: An Interdisciplinary Quarterly. 2015;19(3):533–542. https://doi.org/10.1007/s12119-015-9274-5. [Google Scholar]
- Brabant ME, Hébert M, Chagnon F. Predicting Suicidal Ideations in Sexually Abused Female Adolescents: A 12-Month Prospective Study. Journal of Child Sexual Abuse. 2014;23(4):387–397. doi: 10.1080/10538712.2014.896842. https://doi.org/10.1080/10538712.2014.896842. [DOI] [PubMed] [Google Scholar]
- Cantón-Cortés D, Cantón J. Coping with child sexual abuse among college students and post-traumatic stress disorder: The role of continuity of abuse and relationship with the perpetrator. Child Abuse & Neglect. 2010;34(7):496–506. doi: 10.1016/j.chiabu.2009.11.004. http://doi.org/10.1016/j.chiabu.2009.11.004. [DOI] [PubMed] [Google Scholar]
- Cantón-Cortés D, Cantón J, Justicia F, Cortés MR. A model of the effects of child sexual abuse on post-traumatic stress: the mediating role of attributions of blame and avoidance coping. Psicothema. 2011;23(1):66–73. [PubMed] [Google Scholar]
- Devenish B, Berk L, Lewis AJ. The treatment of suicidality in adolescents by psychosocial interventions for depression: A systematic literature review. Australian and New Zealand Journal of Psychiatry. 2016;50(8):726–740. doi: 10.1177/0004867415627374. https://doi.org/10.1177/0004867415627374. [DOI] [PubMed] [Google Scholar]
- Devries KM, Mak JYT, Child JC, Falder G, Bacchus LJ, Astbury J, Watts CH. Childhood Sexual Abuse and Suicidal Behavior: A Meta-analysis. Pediatrics. 2014;133(5):e1331–e1344. doi: 10.1542/peds.2013-2166. http://doi.org/10.1542/peds.2013-2166. [DOI] [PubMed] [Google Scholar]
- Dyer KFW, Dorahy MJ, Corry M, Black R, Matheson L, Coles H, … Middleton W. Comparing Shame in Clinical and Nonclinical Populations: Preliminary Findings. Psychological Trauma: Theory, Research, Practice, and Policy. 2016 doi: 10.1037/tra0000158. http://doi.org/10.1037/tra0000158. [DOI] [PubMed]
- Feiring C, Cleland C. Childhood sexual abuse and abuse-specific attributions of blame over 6 years following discovery. Child Abuse & Neglect. 2007;31(11–12):1169–1186. doi: 10.1016/j.chiabu.2007.03.020. http://doi.org/10.1016/j.chiabu.2007.03.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feiring C, Simon VA, Cleland CM. Childhood sexual abuse, stigmatization, internalizing symptoms, and the development of sexual difficulties and dating aggression. Journal of Consulting and Clinical Psychology. 2009;77(1):127–137. doi: 10.1037/a0013475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feiring C, Taska LS. The Persistence of Shame Following Sexual Abuse: A Longitudinal Look at Risk and Recovery. Child Maltreatment. 2005;10(4):337–349. doi: 10.1177/1077559505276686. http://doi.org/10.1177/1077559505276686. [DOI] [PubMed] [Google Scholar]
- Feiring C, Taska L, Chen K. Trying to Understand Why Horrible Things Happen: Attribution, Shame, and Symptom Development Following Sexual Abuse. Child Maltreatment. 2002;7(1):25–39. doi: 10.1177/1077559502007001003. http://doi.org/10.1177/1077559502007001003. [DOI] [PubMed] [Google Scholar]
- Feiring C, Taska L, Lewis M. Adjustment following sexual abuse discovery: The role of shame and attributional style. Developmental Psychology. 2002;38(1):79–92. doi: 10.1037//0012-1649.38.1.79. https://doi.org/10.1037/0012-1649.38.1.79. [DOI] [PubMed] [Google Scholar]
- Feiring C, Taska L, Lewis M. The Role of Shame and Attributional Style in Children’s and Adolescents’ Adaptation to Sexual Abuse. Child Maltreatment. 1998;3(2):129–142. doi: 10.1177/1077559598003002007. [DOI] [Google Scholar]
- Feiring C, Taska L, Lewis M. A process model for understanding adaptation to sexual abuse: The role of shame in defining stigmatization. Child Abuse & Neglect. 1996;20(8):767–782. doi: 10.1016/0145-2134(96)00064-6. http://doi.org/10.1016/0145-2134(96)00064-6. [DOI] [PubMed] [Google Scholar]
- Ferdinand RF. Validity of the CBCL/YSR DSM-IV scales Anxiety Problems and Affective Problems. Journal of Anxiety Disorders. 2008;22(1):126–134. doi: 10.1016/j.janxdis.2007.01.008. http://doi.org/10.1016/j.janxdis.2007.01.008. [DOI] [PubMed] [Google Scholar]
- Finkelhor D, Browne A. The traumatic impact of child sexual abuse: A conceptualization. American Journal of Orthopsychiatry. 1985;55(4):530–541. doi: 10.1111/j.1939-0025.1985.tb02703.x. http://doi.org/10.1111/j.1939-0025.1985.tb02703.x. [DOI] [PubMed] [Google Scholar]
- Finkelhor D, Shattuck A, Turner HA, Hamby SL. The Lifetime Prevalence of Child Sexual Abuse and Sexual Assault Assessed in Late Adolescence. Journal of Adolescent Health. 2014 doi: 10.1016/j.jadohealth.2013.12.026. http://doi.org/10.1016/j.jadohealth.2013.12.026. [DOI] [PubMed]
- Folkman S, Lazarus RS. Coping as a mediator of emotion. Journal of Personality and Social Psychology. 1988;54:466–475. [PubMed] [Google Scholar]
- Frazier PA, Mortensen H, Steward J. Coping Strategies as Mediators of the Relations Among Perceived Control and Distress in Sexual Assault Survivors. Journal of Counseling Psychology. 2005;52(3):267–278. https://doi.org/10.1037/0022-0167.52.3.267. [Google Scholar]
- Hébert M. Traduction française du Children’s Impact of Traumatic Events Scale II de V.V. Wolfe (CITES II; 2004) (Document inédit) Département de sexologie, Université du Québec à Montréal; Montréal: 2006. [Google Scholar]
- Hébert M, Tremblay C, Parent N, Daignault IV, Piché C. Correlates of Behavioral Outcomes in Sexually Abused Children. Journal of Family Violence. 2006;21(5):287–299. http://doi.org/10.1007/s10896-006-9026-2. [Google Scholar]
- Hillberg T, Hamilton-Giachritsis C, Dixon L. Review of Meta-Analyses on the Association Between Child Sexual Abuse and Adult Mental Health Difficulties: A Systematic Approach. Trauma, Violence, & Abuse. 2011;12(1):38–49. doi: 10.1177/1524838010386812. http://doi.org/10.1177/1524838010386812. [DOI] [PubMed] [Google Scholar]
- Kendall-Tackett KA, Williams LM, Finkelhor D. Impact of sexual abuse on children: A review and synthesis of recent empirical studies. Psychological Bulletin. 1993;113(1):164–180. doi: 10.1037/0033-2909.113.1.164. http://doi.org/10.1037/0033-2909.113.1.164. [DOI] [PubMed] [Google Scholar]
- Krysinska K, Lester D. Post-traumatic stress disorder and suicide risk: A systematic review. Archives of Suicide Research. 2010;14(1):1–23. doi: 10.1080/13811110903478997. [DOI] [PubMed] [Google Scholar]
- Langevin R, Cossette L, Hébert M. Emotion regulation in sexually abused preschoolers. Child Psychiatry & Human Development. 2016;47(1):1–12. doi: 10.1007/s10578-015-0538-y. https://doi.org/10.1007/s10578-015-0538-y. [DOI] [PubMed] [Google Scholar]
- Levine LE, Conway JM. Self-other awareness and peer relationships in toddlers: Gender comparisons. Infant and Child Development. 2010;19(5):455–464. [Google Scholar]
- Lewis M. Self-conscious emotions: Embarrassment, pride, shame, guilt, and hubris. In: Barrett LF, Lewis M, Haviland-Jones JM, editors. Handbook of emotions. 4. New York, NY, US: Guilford Press; 2016. pp. 792–814. [Google Scholar]
- Maniglio R. The impact of child sexual abuse on health: A systematic review of reviews. Clinical Psychology Review. 2009;29(7):647–657. doi: 10.1016/j.cpr.2009.08.003. http://doi.org/10.1016/j.cpr.2009.08.003. [DOI] [PubMed] [Google Scholar]
- Merikangas KR, He J, Burstein M, Swanson SA, Avenevoli S, Cui L, … Swendsen J. Lifetime Prevalence of Mental Disorders in US Adolescents: Results from the National Comorbidity Study-Adolescent Supplement (NCS-A) Journal of the American Academy of Child and Adolescent Psychiatry. 2010;49(10):980–989. doi: 10.1016/j.jaac.2010.05.017. https://doi.org/10.1016/j.jaac.2010.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller DN, Eckert TL. Youth Suicidal Behavior: An Introduction and Overview. Research Gate. 2009;38(2):153–167. [Google Scholar]
- Miller AB, Esposito-Smythers C, Weismoore JT, Renshaw KD. The relation between child maltreatment and adolescent suicidal behavior: a systematic review and critical examination of the literature. Clinical Child and Family Psychology Review. 2013;16(2):146–172. doi: 10.1007/s10567-013-0131-5. http://doi.org/10.1007/s10567-013-0131-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakamura BJ, Ebesutani C, Bernstein A, Chorpita BF. A psychometric analysis of the Child Behavior Checklist DSM-Oriented Scales. Journal of Psychopathology and Behavioral Assessment. 2009;31(3):178–189. doi: 10.1007/s10862-009-9174-9. http://doi.org/10.1007/s10862-008-9119-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nock MK, Green JG, Hwang I, McLaughlin KA, Sampson NA, Zaslavsky AM, Kessler RC. Prevalence, correlates, and treatment of lifetime suicidal behavior among adolescents: Results from the National Comorbidity Survey Replication Adolescent Supplement. JAMA Psychiatry. 2013;70(3):300–310. doi: 10.1001/2013.jamapsychiatry.55. https://doi.org/10.1001/2013.jamapsychiatry.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paolucci EO, Genuis ML, Violato C. A Meta-Analysis of the Published Research on the Effects of Child Sexual Abuse. The Journal of Psychology. 2001;135(1):17–36. doi: 10.1080/00223980109603677. http://doi.org/10.1080/00223980109603677. [DOI] [PubMed] [Google Scholar]
- Parent N, Hébert M. Questionnaire sur la victimisation de l’enfant. Ste-Foy: Département de mesure et évaluation, Université Laval; 1995. Adaptation française du “History of Victimization Form” by Wolfe, Gentile & Boudreau (1987) [Google Scholar]
- Patton GC, Coffey C, Sawyer SM, Viner RM, Haller DM, Bose K, … Mathers CD. Global patterns of mortality in young people: a systematic analysis of population health data. The Lancet. 2009;374(9693):881–892. doi: 10.1016/S0140-6736(09)60741-8. http://doi.org/10.1016/S0140-6736(09)60741-8. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behavior Research Methods, Instruments & Computers. 2004;36(4):717–731. doi: 10.3758/bf03206553. http://doi.org/10.3758/BF03206553. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior research methods. 2008;40(3):879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- Serafini G, Muzio C, Piccinini G, Flouri E, Ferrigno G, Pompili M, Girardi P, Amore M. Life adversities and suicidal behavior in young individuals: a systematic review. European Child & Adolescent Psychiatry. 2015;24(12):1423–1446. doi: 10.1007/s00787-015-0760-y. http://doi.org/10.1007/s00787-015-0760-y. [DOI] [PubMed] [Google Scholar]
- Sigfusdottir ID, Asgeirsdottir BB, Gudjonsson GH, Sigurdsson JF. Suicidal ideations and attempts among adolescents subjected to childhood sexual abuse and family conflict/violence: The mediating role of anger and depressed mood. Journal of Adolescence. 2013;36(6):1227–1236. doi: 10.1016/j.adolescence.2013.10.001. https://doi.org/10.1016/j.adolescence.2013.10.001. [DOI] [PubMed] [Google Scholar]
- Simon VA, Feiring C, Cleland CM. Early Stigmatization, PTSD, and Perceived Negative Reactions of Others Predict Subsequent Strategies for Processing Child Sexual Abuse. Psychology of Violence. 2014 doi: 10.1037/a0038264. http://doi.org/10.1037/a0038264. [DOI] [PMC free article] [PubMed]
- Tyler KA. Social and emotional outcomes of childhood sexual abuse: A review of recent research. Aggression and Violent Behavior. 2002;7(6):567–589. http://doi.org/10.1016/S1359-1789(01)00047-7. [Google Scholar]
- Ullman SE, Filipas HH, Townsend SM, Starzynski LL. Psychosocial correlates of PTSD symptom severity in sexual assault survivors. Journal of Traumatic Stress. 2007;20(5):821–831. doi: 10.1002/jts.20290. http://doi.org/10.1002/jts.20290. [DOI] [PubMed] [Google Scholar]
- Ullman SE, Najdowski CJ. Correlates of Serious Suicidal Ideation and Attempts in Female Adult Sexual Assault Survivors. Suicide and Life-Threatening Behavior. 2009;39(1):47–57. doi: 10.1521/suli.2009.39.1.47. http://doi.org/10.1521/suli.2009.39.1.47. [DOI] [PubMed] [Google Scholar]
- Ullman SE, Peter-Hagene LC, Relyea M. Coping, Emotion Regulation, and Self-Blame as Mediators of Sexual Abuse and Psychological Symptoms in Adult Sexual Assault. Journal of Child Sexual Abuse. 2014;23(1):74–93. doi: 10.1080/10538712.2014.864747. http://doi.org/10.1080/10538712.2014.864747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiner B. An attributional theory of achievement motivation and emotion. Psychological Review. 1985;92(4):548–573. http://doi.org/10.1037/0033-295X.92.4.548. [PubMed] [Google Scholar]
- Whiffen VE, MacIntosh HB. Mediators of the Link between Childhood Sexual Abuse and Emotional Distress A Critical Review. Trauma, Violence, & Abuse. 2005;6(1):24–39. doi: 10.1177/1524838004272543. http://doi.org/10.1177/1524838004272543. [DOI] [PubMed] [Google Scholar]
- Wolfe VV. Unpublished assessment instrument. London, ON: Child and Adolescent Centre, Lonon Health Sciences Centre; 2002. Children’s Impact of Traumatic Events Scale-II. [Google Scholar]
- Wolfe VV. Child sexual abuse. In: Mash EJ, Barkley RA, editors. Assessment of childhood disorders. 4. New York, NY: Guilford Press; 2007. pp. 685–748. [Google Scholar]
- Wolfe VV, Gentile C, Bourdeau P. History of Victimization Form. Ontario, Canada: Unpublished assessment instrument, London Health Science Centre, London; 1987. [Google Scholar]
- Wonnacott TH, Wonnacott RJ. Introductory Statistics for Business and Economics. 4. John Wiley & Sons; 1995. Statistique. Economica. Translation from Wonnacott, T.H., Wonnacott, R.J. (1990) [Google Scholar]