Abstract
Background:
Barosinusitis, or sinus barotrauma, may arise from changes in ambient pressure that are not compensated by force equalization mechanisms within the paranasal sinuses. Barosinusitis is most commonly seen with barometric changes during flight or diving. Understanding and better classifying the pathophysiology, clinical presentation, and management of barosinusitis are essential to improve patient care.
Objectives:
To perform a comprehensive review of the available literature regarding sinus barotrauma.
Methods:
A comprehensive literature search that used the terms “barosinusitis,” “sinus barotrauma,” and “aerosinusitis” was conducted, and all identified titles were reviewed for relevance to the upper airway and paranasal sinuses. All case reports, series, and review articles that were identified from this search were included. Selected cases of sinus barotrauma from our institution were included to illustrate classic signs and symptoms.
Results:
Fifty-one articles were identified as specifically relevant to, or referencing, barosinusitis and were incorporated into this review. The majority of articles focused on barosinusitis in the context of a single specific etiology rather than independent of etiology. From analysis of all the publications combined with clinical experience, we proposed that barosinusitis seemed to fall within three distinct subtypes: (1) acute, isolated barosinusitis; (2) recurrent acute barosinusitis; and (3) chronic barosinusitis. We introduced this terminology and suggested independent treatment recommendations for each subtype.
Conclusion:
Barosinusitis is a common but potentially overlooked condition that is primed by shifts in the ambient pressure within the paranasal sinuses. The pathophysiology of barosinusitis has disparate causes, which likely contribute to its misdiagnosis and underdiagnosis. Available literature compelled our proposed modifications to existing classification schemes, which may allow for improved awareness and management strategies for barosinusitis.
Keywords: Barosinusitis, sinus barotrauma, diving, aerosinusitis, hyperbaric oxygen therapy, vacuum sinusitis, recurrent sinusitis, sinus pressure, sinus headache, flight sinusitis
INTRODUCTION AND HISTORY OF BAROSINUSITIS
Barosinusitis, or sinus barotrauma, is a condition that describes the varying degrees of sinonasal injury and/or inflammation that result when the aerated spaces of the nose and sinuses are exposed to an uncompensated change in ambient pressure. This entity was first documented in World War II aviation literature,1,2 with its pathophysiology first described by Campbell3 in 1942. In 1965, Flottes4 reported the first case of diving-related barosinusitis, which occurred in a deep sea diver who was using a self-contained underwater breathing apparatus. Over the past 50 years, additional causes of sinus barotrauma have also been documented and include the use of gaseous general anesthetic agents,5 hyperbaric oxygen therapy,6 Chinook wind exposure,7 prolonged high altitude exposure,8 automobile travel,9 submarine decompression,10 nasal blowing,11 and vigorous Valsalva maneuver12 (Table 1).
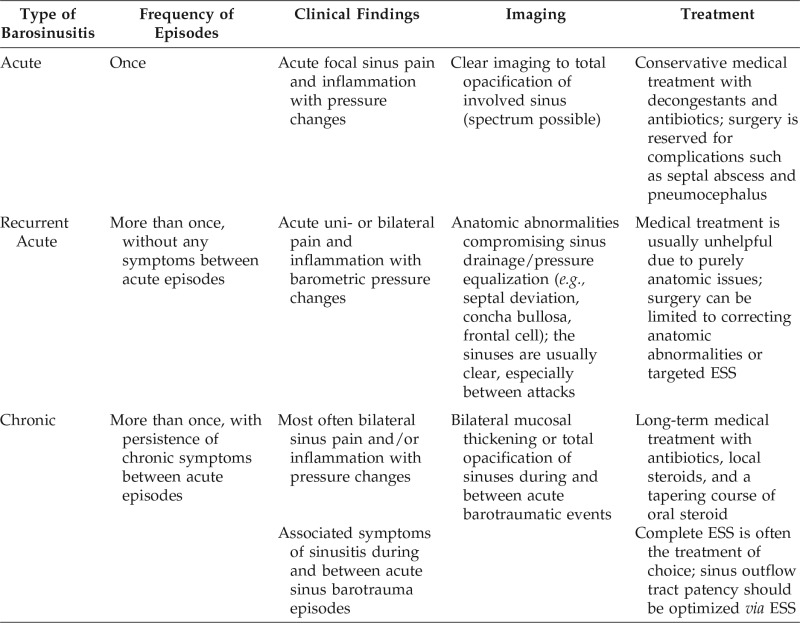
Table 1.
The spectrum of etiologies that contributes to barosinusitis, with the highest levels of evidence available in the literature*
Based on Ref. 51.
Due to the increasing frequency of air travel and recreational and/or commercial deep-sea diving, more patients may seek otolaryngology evaluation with symptoms related to barosinusitis. However, many otolaryngologists remain unfamiliar with this clinical entity due to the lack of differentiating features from other forms of sinusitis as well as the relative paucity of publications in the otolaryngology literature regarding this topic. This review offered a current comprehensive assessment of the published literature on barosinusitis and focused on factors to assist in the diagnosis, prevention, and timely treatment of this condition. In addition, we presented two cases of recurrent acute barosinusitis, a condition not previously well documented in the literature, and proposed a new classification system for sinus barotrauma.
PREVALENCE AND INCIDENCE OF SINUS BAROTRAUMA
The exact prevalence and incidence of barosinusitis remains unknown but is thought to vary with underlying etiology. Estimates of prevalence range from 34% in divers,13 to 19.5–25% in pilots.14,15 Concurrent sinonasal inflammation (e.g., allergic rhinitis) further increases the prevalence of barosinusitis in pilots, with rates reported as high as 55% in commercial pilots and 34% in high-performance fighter pilots.15 Although the incidence of barosinusitis in divers has been reported up to 26%,16 this value is unknown in pilots due to a dearth of reliable studies in this patient cohort. The incidence and prevalence from rare causes are equally difficult to assess; however, prevalence of sinus barotrauma in patients who undergo hyperbaric oxygen exposure is reported to be around 3%.17
PATHOPHYSIOLOGY AND REPORTED CAUSES OF BAROSINUSITIS
Boyle's Law, which states that, at a given temperature, the volume of a gas varies inversely with pressure, is highly applicable to understanding the pathogenesis of barosinusitis. The paranasal sinuses are labyrinthine air-filled spaces bounded by thick, fixed bony outer walls, and by thin, pliable, internal walls. Under normal circumstances, barometric air pressure within the sinus cavities equilibrates with the pressure in the surrounding nasal passages through the openings into the sinuses, known as the sinus ostia. Communication between the central nasal cavity and more laterally located sinuses allows changes in pressure to be compensated by small changes in the volume of gas within the sinuses. In patients with barosinusitis, the ostia may be anatomically smaller (due to minor fluctuations in the wall positions around the ostia) or become narrowed or obstructed due to local inflammation, edema, or trauma, which compromise the ability of the ostia to compensate and facilitate air exchange.18–20 The uncompensated changes in intrasinus pressure can result in the mucosal injuries observed in barosinusitis. The numerous downstream mechanistic pathways are further discussed by etiology.
Flying and Diving
As previously noted, secondary shifts in barometric pressure due to altitude changes during flight and diving are the most common causes of barosinusitis. During ascent in an aircraft or ascent after deep dives, the ambient pressure decreases with the decrease in gravity, which results in intrasinus gaseous expansion against the rigid sinus outer walls, and the intrasinus pressure increases. In a normal sinus, this change is typically compensated by pressure equilibration between the sinus ostia and the nasal cavity, akin to a pressure-release valve (Fig. 1). However, in an inflamed or partially obstructed sinus, increased air expansion and elevated intrasinus pressure without this compensated pressure release is called “reverse squeeze.” This phenomenon, most commonly seen in resurfacing divers, produces an outward, “expansile” compression injury of the sinus mucosa against the bony sinus outer walls (Fig. 2).19,20
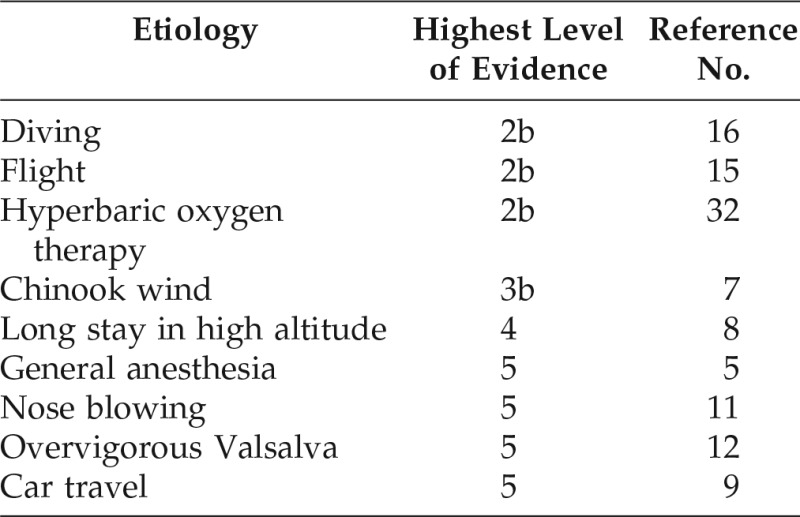
Figure 1.
Illustrations depicting sinus pressure equalization in common contexts. (A) Normal sinus equalization in a healthy, unobstructed frontal sinus at sea level. (B) Normal sinus equalization during flight. The ambient pressure decreases with the decrease in gravity, which results in intrasinus gaseous expansion against the rigid sinus outer walls and intrasinus pressure increases; in a normal sinus, this change is typically compensated by pressure equilibration between the sinus ostia and nasal cavity (outward flow). (C) Normal sinus equalization during diving. The ambient pressure increases due to the effects of gravity and/or water mass; this results in a decrease in gaseous volume within the sinuses and creates intrasinus decompression. In a normal sinus, this change is typically compensated by pressure equilibration between the sinus ostia and the nasal cavity (inward flow).
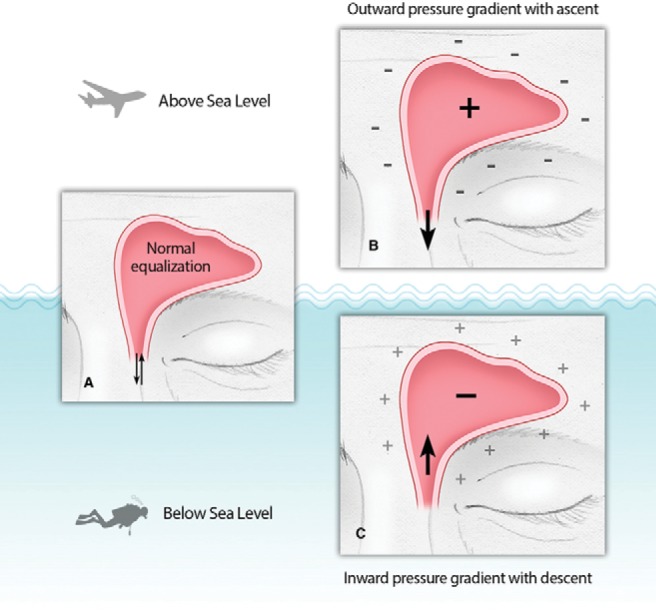
Figure 2.
Illustrations that depict scenarios of sinus barotrauma. (A) Reverse squeeze or compression injury in an inflamed or partially obstructed sinus. Increased air expansion and elevated intrasinus pressure during ascent, without compensated pressure release, produces an outward, “expansile” compression injury of the sinus mucosa against the bony sinus outer walls; this results in mucosal edema and rupture. (B) A squeeze or decompression injury in an inflamed or partially obstructed sinus. Decrease in gaseous volume within the sinuses during descent creates intrasinus decompression without inward pressure equalization; this results in “pulling” forces within the sinus cavity that can cause mucosal edema, avulsion of the mucosal surface from the bone, and hematoma formation, depending on the degree and rapidity of the pressure shifts. (C) Type 3 frontal cell that compromises sinus outflow; a reverse squeeze or compression injury may occur in both the frontal sinus and obstructing type 3 cell, producing severe, but focal, symptoms.
By contrast, during descent, ambient air and water pressures increase due to the effects of gravity and/or water mass. According to Boyle's Law, this results in a decrease in gaseous volume within the nasal cavity and sinuses themselves, and this, therefore, creates a decompression or squeeze effect. The corresponding injuries that may result from uncompensated centripetal, “pulling” forces can range from mild mucosal edema, to complete avulsion of the mucosal surface from the bone, to hematoma formation, depending on the degree and rapidity of the pressure shifts (Fig. 2). Aviation and diving studies indicate that decompression barosinusitis events associated with descent and increased gravity are twice as common as sinus barotrauma that is related to ascent, compression, and reverse squeeze phenomena.16,21
The differences between the physical properties of water and air explains why barosinusitis is reported to be more common in divers than in pilots. Water is noncompressible, and pressure increases linearly at a rate of 1 atmosphere every 10 m. Air, by contrast, is compressible and amorphous, which thereby requires much greater changes in altitude to cause similar changes in pressure.22 The pressure change that occurs during a rapid 5 m underwater dive is equivalent to that seen during a 5500 m descent above sea level; the latter will also occur more gradually.22 In the former scenario, the sinuses have less time to equilibrate to rapid alterations in ambient pressure, which may more readily result in barosinusitis.
Anesthesia
Barosinusitis due to general anesthesia has been described in one case report.5 Two major pathophysiologic mechanisms have been proposed in this setting. First, the use of inhaled nitrous oxide (N2O) has been implicated due to its high blood-to-gas partition coefficient, which is 30 times higher than that of nitrogen (N2). As a result, when an inspired volatile gas mixture is switched from ambient air that contains ∼75–78% N2 to an anesthetic mixture that contains 70% N2O, the N2O will permeate into all gas-filled spaces, such as the paranasal sinuses, ∼30 times faster than N2 can exit. As a result, the intranasal–intrasinus volume or pressure within the bone-encased sinus cavities may rapidly increase.23 When N2O is terminated at the end of an anesthetic procedure, rapid reversal of this process may also ensue to form a marked subatmospheric pressure change within the sinuses, which results in “squeeze” or descent-related phenomenon within an affected sinus or airway. Second, it has been postulated that certain ventilator settings themselves may contribute to sinus barotrauma. Patients with allergic inflammation or chronic sinusitis with a reduced capacity to balance and/or equilibrate pressure between the nose and the sinuses may be predisposed to otherwise harmless peaks in inspiratory pressures during volatile inhalational anesthetic administration.5
Hyperbaric Oxygen Therapy
Hyperbaric medicine, also known as hyperbaric oxygen therapy (HBOT), is the medical use of oxygen at a level higher than atmospheric pressure. The use of HBOT chambers have been well described in various conditions, including carbon monoxide poisoning, necrotizing soft-tissue infections, osteoradionecrosis, decompression sickness, and arterial gas embolism.6 Typically, this treatment is well tolerated by patients due to the slow, graduated elevation of ambient pressures within the HBOT chamber. However, in patients with narrowed or obstructed nasal passages or sinus ostia, HBOT treatment can contribute to squeeze or decompression types of sinus barotrauma injury.
Chinook Wind
A Chinook wind, also known as a “snow eater,” is a weather phenomenon characterized by the rapid flow of warm, high-pressured winds in mountainous regions. It has been described in the Pacific Northwest, New Zealand, southern Europe, and Argentina. The warm wind is theorized to result in an increased concentration of positive ions with rapid ambient pressure changes that can produce barosinusitis. Rudmik et al.7 indicated that several anatomic variants may predispose individuals to Chinook-wind–related barosinusitis. These include the presence of concha bullosa, sphenoethmoidal cells, and large maxillary sinus volumes, which all serve to increase the relative volume of the sinonasal cavity. This, in turn, may increase the intensity of squeeze and reverse-squeeze phenomena during atmospheric pressure changes.
CLINICAL PRESENTATIONS AND A PROPOSED CLASSIFICATION SYSTEM FOR BAROSINUSITIS
To our knowledge, no formal classification system for barosinusitis exists. Therefore, based on our review of the available literature of sinus barotrauma, we developed a proposed classification system for this disease entity: (1) acute barosinusitis, (2) recurrent acute barosinusitis, and (3) chronic barosinusitis (Table 2). The primary distinction between these terms is the frequency of episodes for a given patient with barosinusitis and symptomatology between acute episodes.
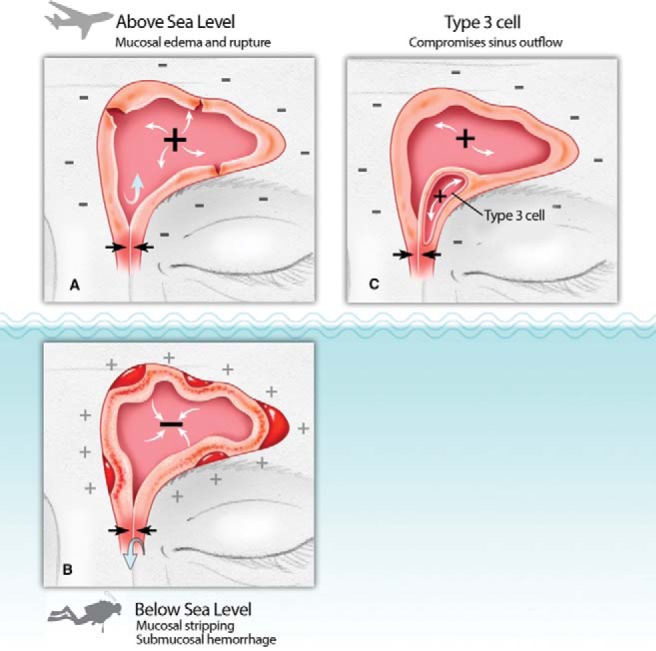
Table 2.
Proposed new classification of barosinusitis
ESS = Endoscopic sinus surgery.
Acute Barosinusitis
We defined acute barosinusitis, the most common form, as an isolated episode of sinus-related pain and inflammation that lasts a few hours to days after exposure to an identifiable cause of change in ambient air pressure. Although acute barosinusitis can occur in the absence of preexisting sinus pathology, reports24–26 indicate that it manifests much more frequently in the setting of preexisting acute sinonasal inflammation. Several series report the presence of a coexisting upper respiratory tract infection (URTI) in 50–73% of cases, whereas other series also document a high incidence of concurrent allergic rhinitis.24–26 From the literature, acute barosinusitis involves a single sinus, with the frontal sinus most commonly affected (68–100% in different series),6,24 followed by maxillary9,27 and sphenoid sinuses.28–30 This is most likely explained by the narrow dimensions of the frontal ostium and recess, and also the thin-walled frontoethmoid type III/IV air cells that commonly partially obstruct the frontal sinus outflow tract (Fig. 2).
Sudden onset of pain is the most frequently reported symptom of acute barosinusitis, and this is often well localized to the affected sinus. In isolated acute sphenoid barosinusitis, discomfort has been reported to be periorbital or temporo-occipital.28,29 Although pain is typically reported as sharp in nature, a dull headache-type pain has also been described. It is possible that this common presentation may indeed represent an “airplane headache,” a phenomenon recently described in the neurologic literature, in which patients experience a frontal and/or medial supraorbital headache that lasts <30 minutes during flight, without clinical or radiologic abnormality.31 Epistaxis is the second most commonly reported symptom and typically occurs in reverse-squeeze barosinusitis associated with ascent.
Disparate series have shown variable rates of epistaxis that range from 33 to 66%.24,32 Patients frequently describe the feeling of a “cracking” or “popping” sensation from the sinus region, which is thought to be a consequence of mucosal stripping and submucosal hematoma formation in the affected sinus (Fig. 2). Rare presentations of acute barosinusitis include excessive lacrimation, purulent nasal discharge,33 anesthesia over the V2 branch of the trigeminal nerve,34 and dental pain. Although highly uncommon, patients have initially presented with symptoms directly related to complications from an acute episode, such as meningitis,35,36 septal abscess,28 pneumocephalus,12,37 orbital floor fracture,11 and even blindness.38
In 1972, Weissman26 attempted to further classify acute barosinusitis based on the duration of symptoms and plain film radiographic findings. He defined class 1 acute barosinusitis as lasting <24 hours, with normal sinus radiographs. Class 2 and class 3 both showed sinus opacification on plain radiographs; however, class 2 attacks last <24 hours and class 3 attacks persist for >1 day. Although plain films are no longer indicated for the routine evaluation of sinus disease, the duration can be a helpful way to categorize these symptoms.
Recurrent Acute Barosinusitis
When acute attacks of barosinusitis present frequently, we propose that the term “recurrent acute barosinusitis” be applied. Between attacks, these patients remain completely asymptomatic, with no clinical or radiologic evidence of disease. Only one other article in the literature mentioned this term and indicated that patients may have a higher incidence of underlying sinonasal inflammation and anatomic variants, e.g., septal deviation.36 Treating physicians must be aware of this structural possibility in their workup and management of this subset of patients. It should be mentioned that recurrent acute barosinusitis is distinct from recurrent sinus barotrauma, which we would now classify as chronic barosinusitis. We present two cases of recurrent acute barosinusitis in the section Radiology Associated with Barosinusitis.
Chronic Barosinusitis
Chronic barosinusitis, the most severe form of barosinusitis, is also the most poorly described in the literature. It is often confused with chronic rhinosinusitis secondary to underlying sinonasal inflammation due to the long-standing duration and nature of symptoms. A detailed history with specific attention to occupational or recreational causes of barotrauma is essential for the proper diagnosis of this condition. Recent studies18,39,40 of recreational and professional divers indicate that repeated barotrauma may actually cause this condition; however, caution must be used when evaluating these studies to avoid equating correlation with causation. The rate of mucosal thickening, as demonstrated on magnetic resonance imaging (MRI) in recreational divers, was double the rate seen in controls, with 41.8% of divers having radiologic changes within the sinuses.39
Another study of professional divers showed a directly proportional relationship between the prevalence of chronic rhinosinusitis and the number of dives performed.40 In contrast to acute barosinusitis, chronic barosinusitis often presents bilaterally and involves numerous sinuses in parallel. Recurrent severe pain during ambient pressure changes prevents patients with chronic barosinusitis from flying or diving. Up to 72% of these patients show other symptoms of chronic rhinosinusitis as well.18 At present, there is not enough evidence to conclude whether a preexisting chronic sinusitis causes recurrent barotrauma symptoms or vice versa in this subgroup of patients.
RADIOLOGY ASSOCIATED WITH BAROSINUSITIS
Acute sinus barotrauma can present with a wide range of imaging findings. In many cases, there may be no radiologic abnormalities evident; whereas, in other cases, computed tomography (CT) imaging may demonstrate partial to complete opacification of one or more of the paranasal sinuses.26 On MRI, acute sinus barotrauma may be seen as an area of hyperintensity on both T1 and T2 without contrast enhancement. These imaging characteristics are hypothesized to be related to submucosal hemorrhage that occurs during the squeeze or revere squeeze injury to the sinonasal mucosa and are similar to signal changes seen with mucoceles and cholesterol granulomas that should be considered in the differential diagnosis. Typically, a thorough history, along with activity associated with changes in ambient pressure, are the discriminating factors in establishing the diagnosis of barosinusitis.41
Recurrent acute barosinusitis and even, at times, early presentations of recurrent sinus barotrauma may demonstrate similar imaging characteristics that coincide with the episode. It is important that careful evaluation of imaging is performed to allow identification of correctable anatomic abnormalities or variants that may predispose an individual to repeated attacks. In cases of recurrent sinus barotrauma, one may see signs of chronic mucosal changes between episodes as well.
The CT of a patient who had nasal congestion and experienced several episodes of bilateral maxillary and ethmoid pain during commercial air travel is presented in Fig. 3. Most pain occurred during ascent (reverse squeeze) and was associated with bilateral V2 trigeminal nerve numbness and tingling. Bilateral concha bullosa with the ostiomeatal complex narrowing was present, without evidence of mucosal thickening or sinusitis on imaging. He underwent surgery to both improve his nasal airway (septoplasty and submucosal turbinate reductions) and sinus patency (concha bullosa resection, bilateral maxillary antrostomies, total ethmoidectomies). Symptoms of barosinusitis completely resolved after sinus surgery, with the absence of symptoms confirmed even after five flights after surgery.
Figure 3.

Sinus computed tomography, coronal view of a frequent airline traveler with recurrent episodes of bilateral maxillary and ethmoid pain during ascent (reverse squeeze), associated with bilateral V2 trigeminal nerve anesthesia versus tingling sensation. Bilateral concha bullosa were noted to compress the ostiomeatal complexes (OMC) and narrow the bilateral maxillary infundibulae, in addition to mild septal deviation–broad septal width and profound inferior turbinate hypertrophy. Treatment for this presentation of recurrent acute barosinusitis is noted in the accompanying text.
The sinus CT of an F-16 fighter pilot, grounded due to acute episodes of facial pain and “whistling sounds” that originated from “somewhere between my eyes” on high-speed descent (squeeze-type injury) is presented in Fig. 4. He also noted chronic nasal congestion. Significant septal deviation and small left concha bullosa that compromised the left ostiomeatal complex was present on imaging, with right inferior turbinate hypertrophy, but the sinuses were clear overall. This scenario of recurrent acute barosinusitis was treated with septoplasty and submucosal inferior turbinate reductions to improve the nasal airways as well as bilateral maxillary antrostomies and anterior ethmoidectomies to improve sinus patency. At 4 weeks after surgery to the present, 3 years after surgery, this patient has been on active duty as a fighter pilot and confirmed the absence of symptoms reminiscent of nasal obstruction or barosinusitis.
Figure 4.

Sinus computed tomography (CT), coronal view from an F-16 fighter pilot who was temporarily grounded for workup of recurrent acute episodes of maxillary facial pain and “whistling sounds” that originated from “areas between the eyes“ on rapid descent (squeeze) from a high altitude. Significant septal deviation narrowing the left greater than right nasal airway and maxillary sinus infundibulum is evident on CT imaging, as is compensatory right inferior turbinate hypertrophy. Treatment for this presentation of recurrent acute barosinusitis is noted in the accompanying text.
Finally, the radiologic changes associated with chronic barosinusitis are similar to those seen in chronic rhinosinusitis and range from mucosal thickening and patchy opacification to complete opacification of all paranasal sinuses.
MANAGEMENT OPTIONS FOR BAROSINUSITIS
Medical
Different medical treatments have been proposed for the management of acute barosinusitis and range from observation to the use of antibiotics, decongestants, and oral steroids.29,42 Isolated acute symptomatic episodes can be successfully managed with decongestants and analgesics immediately after an episode, albeit direct evidence for this is sparse and limited to expert opinion. The roles of antibiotics and of steroids remain unclear and might be reserved for symptoms that persist for >24 hours.25 We suggest that, if patients present with a single episode of acute barosinusitis, then current guidelines regarding acute sinusitis from any other etiology could be used to decide on treatment and that imaging be avoided in the absence of suspected complications. In patients with suspected recurrent acute barosinusitis, a lower threshold for CT imaging may be used to evaluate for structural sinus anomalies that predispose to these episodes.
In the setting of chronic barosinusitis, a trial of maximal medical therapy, similar to that used in patients with chronic sinusitis, should be attempted before considering surgery. There is no standardized medical treatment for chronic barosinusitis in patients exposed to repetitive barotrauma. In the literature on diving, one proposed regimen described a 6-week course of saline solution rinses and fluticasone topical steroid spray plus a 5-day course of 100 mg prednisone.40,43 A 1-month course of antibiotics has also been suggested for active-duty pilots.19 For pilots, complete resolution of symptoms after medical therapy may warrant an altitude chamber and/or pressure test. Recurrent symptoms should prompt CT or MRI imaging, and sinus surgery may be required. Although a recent study indicated that 49% of divers with chronic rhinosinusitis responded well to medical therapy and could return to diving duties,43 there is no consensus among researchers regarding success rates for medical therapy of chronic barosinusitis.
Surgery
Surgical management of barosinusitis is best considered in the context of its classification. The primary indication for surgery for an episode of isolated, acute barosinusitis is the management of complications such as septal abscess,28 orbital sequelae, or pneumocephalus.44 However, if the history indicates recurrent acute barosinusitis, then a search for correctable and possibly predisposing anatomic variants should be undertaken by using both imaging and endoscopy. Surgery should be tailored to the individual and may range from septoplasty and/or concha bullosa reduction alone to uncinectomy and targeted sinus surgery in the case of isolated sinus disease to complete bilateral endonasal surgery for correction of anatomic causes of barosinusitis.
The role of surgery in patients with chronic barosinusitis for whom appropriate medical therapy failed is evident, with a reported long-term success rate for endoscopic surgery of almost 92–95%.18,45 Given the possibility of further exposure to sudden ambient pressure changes, most researchers agree that a maximal sinus ostial opening should be attempted to prevent restenosis and recrudescence of symptoms. A complete sinus surgery to all paranasal sinuses, maxillary antrostomy, sphenoethmoidectomy, and wide frontal recess clearance (Draf IIA at minimum), with or without septal and turbinate surgery, is the recommended set of procedures in these patients.20 Some researchers reserve the modified Lothrop procedure (Draf III) as a rescue procedure for recurrent restenosis with barotrauma of the frontal recess.46
There is sparse literature regarding the use of balloon catheter dilation (BCD) in the prophylactic or directed treatment of barosinusitis, and its utility remains unclear. Given multiple years of combined experience with this procedure, the senior authors (Z.M.P. and J.V.N.) hypothesize that BCD might provide the most benefit in cases of sinus barotrauma related primarily to sinus ostial narrowing and/or stenosis (Fig. 2A and B). Balloon dilation of the frontal sinus ostium, e.g., may prevent occlusion of the sinus outflow tract tissues that rapidly crescendos into barotrauma. Alternatively, if frontoethmoid air cells are instead largely contributing to the ostial constriction of the affected sinus (Fig. 2C), BCD might be counterproductive. Balloon dilation may render improved patency to the affected sinus ostium but simultaneously compress the dimensions (and lumen) of the intervening air cell, which would now be expected to be more affected by squeeze–reverse squeeze pressures. Although one recent case report showed unsuccessful results with the use of BCD in recurrent frontal barosinusitis,47 increased numbers of reports and patient series naturally would be beneficial to further corroborate these hypotheses.
PREVENTION OF BAROSINUSITIS
Acute barosinusitis is often associated with recent URTI, therefore, avoiding significant altitude changes during episodes of acute viral inflammation is the first and most important step that should be emphasized to patients who are affected. It is recommended that patients with a recent or ongoing URTI or with severe allergic rhinitis avoid activities that increase the risk of sinus barotrauma. If ambient pressure change is unavoidable, then administration of oral decongestants before the anticipated event and temporal administration of local or topical decongestants at times of anticipated shifts in pressure can often prevent barotrauma.48 Studies in the field of otic barotrauma49–50 indicated that 120 mg of pseudoephedrine taken 30 minutes before exposure to a barotraumatic event may have decreased the incidence of otic trauma in up to 52% of patients with a history of barotitis. Conversely, the relative risk reduction of only 10% is reported in patients who use only local decongestants (oxymetazoline) before a barotraumatic event exposure.49,50
CONCLUSION
Barosinusitis, or sinus barotrauma, is a well-understood disease process from a pathophysiologic standpoint but one that is poorly appreciated in the physician community. In this comprehensive review, we illuminate aspects of the history, major reported causes, treatment paradigms, and preventative strategies associated with sinus barotrauma. Moreover, we introduce a new classification system for patients with barosinusitis - acute, recurrent acute, and chronic barosinusitis - which may simplify understanding and diagnosis of this fascinating clinical entity, and trigger earlier consideration of treatment options for patients who are afflicted.
Footnotes
No external funding sources reported
A.J. Psaltis is a consultant with Medtronic, Aerin Medical Technologies, 480 Biomedical, ENT technologies and on the speakers bureau with Smith & Nephew; Z.M. Patel is a consultant with Medtronic and Intersect ENT; J.V. Nayak is a consultant with Olympus America, Lannett, and Medtronic, and a former consultant with Acclarent/J&J. The remaining authors have no conflicts of interest pertaining to this article
REFERENCES
- 1. Hermann A. “Laceration of the Mucous Membrane and Hematoma of the Nasal Sinuses in Aviators.” Ztschr. f. Hals-, Nasen-u. Ohrenh. 47:103–112, 1940. [Google Scholar]
- 2. Surgeon General. Book chapter in: German aviation medicine in World War II. United States Air Force (USAF), US Govt Printing Office, Washington DC: 990–992, 1948. [Google Scholar]
- 3. Campbell PA. Aerosinusitis. Arch Oto 35:107–114, 1942. [Google Scholar]
- 4. Flottes L. Barotrauma of the ear and sinuses caused by underwater immersion [in Spanish]. Acta Otorinolaryngol Iber Am 16:453–483, 1965. [PubMed] [Google Scholar]
- 5. Salvinelli F, Rinaldi V, D'Ascanio L. Paranasal sinus barotrauma in general anesthesia: Special attention. J Clin Anesth 17:323, 2005. [DOI] [PubMed] [Google Scholar]
- 6. Ambiru S, Furuyama N, Aono M, et al. Analysis of risk factors associated with complications of hyperbaric oxygen therapy. J Crit Care 23:295–300, 2008. [DOI] [PubMed] [Google Scholar]
- 7. Rudmik L, Muzychuk A, Oddone Paolucci E, Mechor B. Chinook wind barosinusitis: An anatomic evaluation. Am J Rhinol Allergy 23:e14–e16, 2009. [DOI] [PubMed] [Google Scholar]
- 8. Prasad BK. ENT morbidity at high altitude. J Laryngol Otol 125:188–192, 2011. [DOI] [PubMed] [Google Scholar]
- 9. Tosun F, Durmaz A, Kıvrakdal C, et al. Severe maxillary sinus barotrauma associated with car travel. Int J Pediatr Otorhinolaryngol Extra 2:151–153, 2007. [Google Scholar]
- 10. Slisković Z. Cases of barotrauma of paranasal sinuses in diving, submarine and flying services [in Serbian]. Vojnosanit Pregl 25:567–569, 1968. [PubMed] [Google Scholar]
- 11. García de Marcos JA, del Castillo-Pardo de Vera JL, Calderon-Polanco J. Orbital floor fracture and emphysema after nose blowing. Oral Maxillofac Surg 12:163–165, 2008. [DOI] [PubMed] [Google Scholar]
- 12. Babl FE, Arnett AM, Barnett E, et al. Atraumatic pneumocephalus: A case report and review of the literature. Pediatr Emerg Care 15:106–109, 1999. [PubMed] [Google Scholar]
- 13. Taylor DM, O'Toole KS, Ryan CM. Experienced scuba divers in Australia and the United States suffer considerable injury and morbidity. Wilderness Environ Med 14:83–88, 2003. [DOI] [PubMed] [Google Scholar]
- 14. Rosenkvist L, Klokker M, Katholm M. Upper respiratory infections and barotraumas in commercial pilots: A retrospective survey. Aviat Space Environ Med 79:960–963, 2008. [DOI] [PubMed] [Google Scholar]
- 15. Ulanovski D, Barenboim E, Raveh E, et al. Sinusitis in pilots of different aircraft types: Is allergic rhinitis a predisposing factor? Am J Rhinol 22:122–124, 2008. [DOI] [PubMed] [Google Scholar]
- 16. Uzun C. Paranasal sinus barotrauma in sports self-contained underwater breathing apparatus divers. J Laryngol Otol 123:80–84, 2009. [DOI] [PubMed] [Google Scholar]
- 17. Fitzpatrick DT, Franck BA, Mason KT, Shannon SG. Risk factors for symptomatic otic and sinus barotrauma in a multiplace hyperbaric chamber. Undersea Hyperb Med 26:243–247, 1999. [PubMed] [Google Scholar]
- 18. O'Reilly BJ, Lupa H, Mcrae A. The application of endoscopic sinus surgery to the treatment of recurrent sinus barotrauma. Clin Otolaryngol Allied Sci 21:528–532, 1996. [DOI] [PubMed] [Google Scholar]
- 19. Weitzel EK, McMains KC, Rajapaksa S, et al. Aerosinusitis: Pathophysiology, prophylaxis, and management in passengers and aircrew. Aviat Space Environ Med 79:50–53, 2008. [DOI] [PubMed] [Google Scholar]
- 20. Weitzel EK, McMains KC, Wormald PJ. Comprehensive surgical management of the aerosinusitis patient. Curr Opin Otolaryngol Head Neck Surg 17:11–17, 2009. [DOI] [PubMed] [Google Scholar]
- 21. McGibbon JE. Nasal sinus pain caused by flying (The syndrome of sinus barotrauma): an analysis of 145 cases. J Laryngol Otol 59:405–427, 1944. [Google Scholar]
- 22. Becker GD, Parell GJ. Barotrauma of the ears and sinuses after scuba diving. Eur Arch Otorhinolaryngol 258:159–163, 2001. [DOI] [PubMed] [Google Scholar]
- 23. Morgan GE, Mikhail MS, Murray MJ. Clinical Anesthesiology, 4th ed New York: Lange Medical Books/McGraw Hill, 2006. [Google Scholar]
- 24. Fagan P, McKenzie B, Edmonds C. Sinus barotrauma in divers. Ann Otol Rhinol Laryngol 85(pt. 1):61–64, 1976. [DOI] [PubMed] [Google Scholar]
- 25. Edmonds C. Sinus barotrauma: a bigger picture. J South Pac Underwater Med Soc J 24:13–19, 1994. [Google Scholar]
- 26. Weissman B, Green RS, Roberts PT. Frontal sinus barotrauma. Laryngoscope 82:2160–2168, 1972. [DOI] [PubMed] [Google Scholar]
- 27. Butler FK, Bove AA. Infraorbital hypesthesia after maxillary sinus barotrauma. Undersea Hyperb Med 26:257–259, 1999. [PubMed] [Google Scholar]
- 28. Jeong JH, Kim K, Cho SH, Kim KR. Sphenoid sinus barotrauma after scuba diving. Am J Otolaryngol 33:477–480, 2012. [DOI] [PubMed] [Google Scholar]
- 29. Bourolias C, Gkotsis A. Sphenoid sinus barotrauma after free diving. Am J Otolaryngol 32:159–161, 2011. [DOI] [PubMed] [Google Scholar]
- 30. Larsen AS, Buchwald C, Vesterhauge S. Sinus barotrauma—Late diagnosis and treatment with computer-aided endoscopic surgery. Aviat Space Environ Med 74:180–183, 2003. [PubMed] [Google Scholar]
- 31. Atkinson V, Lee L. An unusual case of an airplane headache. Headache 44:438–439, 2004. [DOI] [PubMed] [Google Scholar]
- 32. Plafki C, Peters P, Almeling M, et al. Complications and side effects of hyperbaric oxygen therapy. Aviat Space Environ Med 71:119–124, 2000. [PubMed] [Google Scholar]
- 33. Yoshida Y. Aerosinusitis an experience of treatment of two cases. [in Japanese] Japan J Occup Med Traumatol 51:71–84, 2003. [Google Scholar]
- 34. Garges LM. Maxillary sinus barotrauma—Case report and review. Aviat Space Environ Med 56:796–802, 1985. [PubMed] [Google Scholar]
- 35. Javan R, Duszak R, Jr, Eisenberg AD, Eggers FM. Spontaneous pneumocephalus after commercial air travel complicated by meningitis. Aviat Space Environ Med 82:1153–1156, 2011. [DOI] [PubMed] [Google Scholar]
- 36. Parell GJ, Becker GD. Neurological consequences of scuba diving with chronic sinusitis. Laryngoscope 110:1358–1360, 2000. [DOI] [PubMed] [Google Scholar]
- 37. Mahabir RC, Szymczak A, Sutherland GR. Intracerebral pneumatocele presenting after air travel. J Neurosurg 101:340–342, 2004. [DOI] [PubMed] [Google Scholar]
- 38. Bellini MJ. Blindness in a diver following sinus barotrauma. J Laryngol Otol 101:386–389, 1987. [Google Scholar]
- 39. Sonmez G, Uzun G, Mutluoglu M, et al. Paranasal sinus mucosal hypertrophy in experienced divers. Aviat Space Environ Med 82:992–994, 2011. [DOI] [PubMed] [Google Scholar]
- 40. Klingmann C, Praetorius M, Baumann I, Plinkert PK. Otorhinolaryngologic disorders and diving accidents: An analysis of 306 divers. Eur Arch Otorhinolaryngol 264:1243–1251, 2007. [DOI] [PubMed] [Google Scholar]
- 41. Segev Y, Landsberg R, Fliss DM. MR imaging appearance of frontal sinus barotrauma. AJNR Am J Neuroradiol 24:346–347, 2003. [PMC free article] [PubMed] [Google Scholar]
- 42. Smith JP, Furry DE. Aeromedical considerations in the management of paranasal sinus barotrauma. Aerosp Med 43:1031–1033, 1972. [PubMed] [Google Scholar]
- 43. Skevas T, Baumann I, Bruckner T, et al. Medical and surgical treatment in divers with chronic rhinosinusitis and paranasal sinus barotrauma. Eur Arch Otorhinolaryngol 269:853–860, 2012. [DOI] [PubMed] [Google Scholar]
- 44. Murugesan C, Powell M, Khayal HB. Sinus barotrauma leading to extradural muco-pneumocephalus. Br J Neurosurg 24:80–81, 2010. [DOI] [PubMed] [Google Scholar]
- 45. Parsons DS, Chambers DW, Boyd EM. Long-term follow-up of aviators after functional endoscopic sinus surgery for sinus barotrauma. Aviat Space Environ Med 68:1029–1034, 1997. [PubMed] [Google Scholar]
- 46. Weitzel EK, Flottmann JT, McMains KC. Endoscopic frontal sinus drillout for recurrent barotrauma: A procedure to save a pilot's career. Aviat Space Environ Med 80:660–662, 2009. [DOI] [PubMed] [Google Scholar]
- 47. Andrews JN, Weitzel EK, Eller R, McMains CK. Unsuccessful frontal balloon sinuplasty for recurrent sinus barotrauma. Aviat Space Environ Med 81:514–516, 2010. [DOI] [PubMed] [Google Scholar]
- 48. Stewart TW., Jr Common otolaryngologic problems of flying. Am Fam Physician 19:113–119, 1979. [PubMed] [Google Scholar]
- 49. Jones JS, Sheffield W, White LJ, Bloom MA. A double-blind comparison between oral pseudoephedrine and topical oxymetazoline in the prevention of barotrauma during air travel. Am J Emerg Med 16:262–264, 1998. [DOI] [PubMed] [Google Scholar]
- 50. Csortan E, Jones J, Haan M, Brown M. Efficacy of pseudoephedrine for the prevention of barotrauma during air travel. Ann Emerg Med 23:1324–1327, 1994. [DOI] [PubMed] [Google Scholar]
- 51. Guyatt G, Gutterman D, Baumann M, et al. Grading strength of recommendations and quality of evidence in clinical guidelines: Report from an american college of chest physicians task force. Chest 129:174–181, 2006. [DOI] [PubMed] [Google Scholar]