Abstract
The long non-coding RNA (lncRNA) urothelial carcinoma associated 1 (UCA1) is an oncogenic lncRNA in bladder cancer, and its upregulation is associated with enhanced cell invasion. However, the underlying mechanism remains to be elucidated. The present study demonstrated that UCA1 was positively associated with cell invasion ability and promoted epithelial-mesenchymal transition (EMT) of bladder cancer cells by inducing high mobility group box 1 (HMGB1). Furthermore, bioinformatics and luciferase reporter assays demonstrated binding sites of the tumor suppressive miR-143 within UCA1 and the 3′untranslated region of HMGB1. UCA1 negatively regulated miR-143 expression in a dose-dependent manner in bladder cancer cells. In addition, UCA1 and HMGB1 were upregulated and miR-143 was downregulated in bladder cancer specimens. Overall, the data suggested that UCA1 may promote the invasion and EMT of bladder cancer cells by regulating the miR-143/HMGB1 pathway, which exhibits an important regulatory role in the pathology of bladder cancer.
Keywords: bladder cancer, epithelial-mesenchymal transition, high mobility group box 1, miR-143, urothelial carcinoma associated 1
Introduction
Bladder cancer is one of the most frequent malignancies in the world. Despite the significant advances in the development of diagnostic and therapeutic methods in recent years, patients with invasive bladder cancer still have a poor 5-year survival rate of less than 60% (1,2). Epithelial-mesenchymal transition (EMT), which is characterized by loss of cell adhesion and gain of migratory and invasive capability, is an important mechanism for metastatic potential and the initial stage of cancer metastasis, including bladder cancer (3,4).
Long non-coding RNAs (lncRNAs) are a class of noncoding regulatory RNA molecules that are longer than 200 nucleotides. Previous studies have focused on the regulatory roles of lncRNAs in several biological processes, such as chromosome inactivation, genomic imprinting and development (5–7). Recently, increasing reports have revealed that lncRNAs are frequently dysregulated in various human cancers, including bladder cancer (8,9). Of note, many dysregulated lncRNAs are involved in EMT and metastasis in human cancer. For example, high expression of the lncRNA PVT1 promotes invasion by inducing EMT in esophageal cancer (10), and increased lncRNA PANDAR expression indicates a poor prognosis for colorectal cancer and promotes metastasis by the EMT pathway (11). LncRNAs can also function as a competing endogenous RNA to sponge microRNAs (12–14). For example, the lncRNA H19 promotes EMT by functioning as a miRNA sponge to miR-138 and miR-200a in colorectal cancer (15). Therefore, by interacting with specific miRNAs, lncRNAs can play an important role in cancer development and progression.
UCA1 was first identified as an oncogenic lncRNA in bladder cancer (16). UCA1 is highly expressed in diverse cancer types, such as breast cancer (17), pancreatic cancer (18), gastric cancer (19), and colorectal cancer (20,21), suggesting that high expression of UCA1 might serve as a molecular marker for predicting metastasis and prognosis in these cancers (22). Several studies also demonstrated that upregulation of UCA1 is associated with EMT in breast cancer (23) and bladder cancer (24), but the underlying mechanism remains largely unknown.
HMGB1, a member of the high mobility group box (HMG-box) subfamily, is involved in many cancers (25,26). HMGB1 also functions as an inducer of EMT in human cancer cells (27–31). HMGB1 expression was much higher in bladder cancer cells than normal urethra epithelial cells and was associated with cell invasion (32,33). However, the mechanism of HMGB1 in bladder cancer is largely unknown.
MicroRNAs (miRNAs) play important roles during tumorigenesis, and dysregulated miRNAs are also involved in EMT in human cancer. In the past decades, the involvement of miRNAs in human bladder cancer has been widely studied. We previously reported that miR-143 acts as a tumor suppressor in human bladder cancer (34).
In the present study, UCA1 and HMGB1 were upregulated and miR-143 was downregulated in bladder cancer specimens. Bioinformatics found that binding sites of the tumor suppressive miR-143 within UCA1 and the 3′UTR of HMGB1. And taken the functional examinations together, we hypothesis that UCA1 may promote the invasion and EMT of bladder cancer cells by regulating the miR-143/HMGB1 pathway.
Materials and methods
Tissue specimens
A total of 81 bladder tissue specimens, including 52 tumor tissues and 29 adjacent noncancerous tissues (at least 2.5 cm away from the tumor), were obtained from our hospital. All tissues were collected from bladder cancer at the time of radical cystectomy, snap-frozen in liquid nitrogen and stored at −70°C until use. All patients gave informed consent prior to collection of specimens according to institutional guidelines. The study was approved by the Institute Research Ethics Committee at Peking University Shenzhen Hospital.
Cell culture
The human bladder cancer cell lines (T24, 5637, J82, RT4 and HT1376) were purchased from China Academia Sinica Cell Repository (Shanghai, China) and cultured in DMEM (Invitrogen, Carlsbad, CA, USA) or RPMI 1640 (Gibco; Thermo Fisher Scientific, Inc., Waltham, MA, USA) supplemented with 10% fetal calf serum at 37°C in a 5% CO2 incubator.
RNA isolation and qRT-PCR
Total RNA was extracted by TRIzol reagent (Invitrogen) and reverse transcribed using the Primer Script RT Reagent kit (Takara Bio, Tokyo, Japan). UCA1 and miR-381 expression levels were determined using the SYBR-Green qRT-PCR assay (BioRad, Berkeley, CA, USA) and mirVana qRT-PCR miRNA Detection kit (Ambion, Austin, TX, USA), respectively. GAPDH and U6 snRNA were used as endogenous controls for UCA1 and miR-143 relative expression, respectively. Primers used are as follows: UCA1-F, 5′-CTCTCCATTGGGTTCACCATTC-3′, UCA1-R, 5′-GCGGCAGGTCTTAAGAGATGAG-3′; HMGB1-F, 5′-ATCCCAATGCACCCAAGAGGCCT-3′, HMGB1-R, 5′-TTCGCAACATCACCAATGGACAGG-3′; β-actin-F, 5′-AGGGGCCGGACTCGTCATACT-3′, β-actin-R, 5′-GGCGGCACCACCATGTACCCT-3′; miR-143-F, 5′-CCTGGCCTGAGATGAAGCAC-3′, miR-143-R, 5′-CAGTGCTGGGTCCGAGTGA-3′; and U6-F, 5′-CTCGCTTCGGCAGCACA-3′, U6-R, 5′-AACGCTTCACGAATTTGCGT-3′. The relative levels were measured in triplicate using the 2−∆∆Cq method (35).
Luciferase reporter assay
Fragments of the 3′UTR of HMGB1 and UCA1 containing miR-143 binding sites were amplified and cloned into the psiCHECK-2 reporter vector (Promega, Shanghai, China). The mutated versions of the 3′UTR of HMGB1 and UCA1 (with substitutions of four bases in the miR-143 seed binding sites) were generated using the QuikChange™ Site-Directed Mutagenesis kit (Stratagene, La Jolla, CA, USA). T24 cells were co-transfected with the reporter vector (0.5 µg) and miR-143 mimics or scrambled mimics (50 nM) using Lipofectamine 2000 (Invitrogen). After 48 h, the Dual Luciferase Reporter assay system (Promega, Fitchburg, WI, USA) was used to examine luciferase activity. MiR-143, scramble mimics and miR-143 inhibitor mimics were purchased from RiboBio (Guangzhou, China).
Vector construction and siRNA
To construct the UCA1 expression vector, we amplified UCA1 cDNA with flanking sequences (forward primer, 5′-ATGCACCTTGTGACTCCCTCCTCT-3′; reverse primer, 5′-CACCTCATCAGACTGCCTTTGG-3′) and cloned it into the pcDNA3.1 vector in BamHI/XhoI sites (Invitrogen). We used the following siRNAs for knockdown experiments: si-UCA1, 5′-GAGCCGAUCAGACAAACAAUU-3′ (S), 5′-UUGUUUGUCUGAUCGGCUCUU-3′ (AS); si-HMGB1, 5′-CCCGUUAUGAAAGAGAAAUUU-3′ (S), 5′-AUUUCUCUUUCAUAAUGGGUU-3′ (AS); si-NC (control), 5′-UUCGUCUGUACUCCACAUATT-3′ (S), 5′-GAUGUCUUCUACAGUCCGATT-3′ (AS). We used Lipofectamine 2000 Reagent (Invitrogen) for cell transfection.
Cell invasion assays
Cell invasion was assessed by Transwell assays with matrigel (BD Bioscience, San Diego, CA, USA). Briefly, 5×104 cells in 200 µl of serum-free media were added into the upper chamber and 500 µl media with 10% fetal bovine serum were added to the bottom chamber. After 24 h, the cells that invaded through the membrane were fixed with 3% formaldehyde, stained with 0.5% crystal violet, and imaged under an inverted microscope (Olympus, Tokyo, Japan).
Western blot analysis
Total cellular extracts were prepared using lysis buffer (Sigma-Aldrich, St. Louis, MO, USA). Approximately 50 ug of total protein was separated by 10% SDS-PAGE and transferred to a PVDF membrane. Membranes were incubated with anti-E-cadherin (1:500), anti-N-cadherin (1:1,000) and anti-Vimentin (1:500) antibody (Santa Cruz Biotechnology, Santa Cruz, CA, USA) followed by the HRP-conjugated secondary antibody (Santa Cruz Biotechnology). Signals were visualized using the ECL detection system (SuperSignal West Femto, Pierce, USA).
Statistical analysis
Statistical analyses were carried out using the SPSS 19.0 software (IBM SPSS, Armonk, NY, USA). Student's t-test was used to analyze experimental significance. Spearman's correlation analysis was used to analyze the correlation between miR-143 and UCA1 and HMGB1 expression.
Results
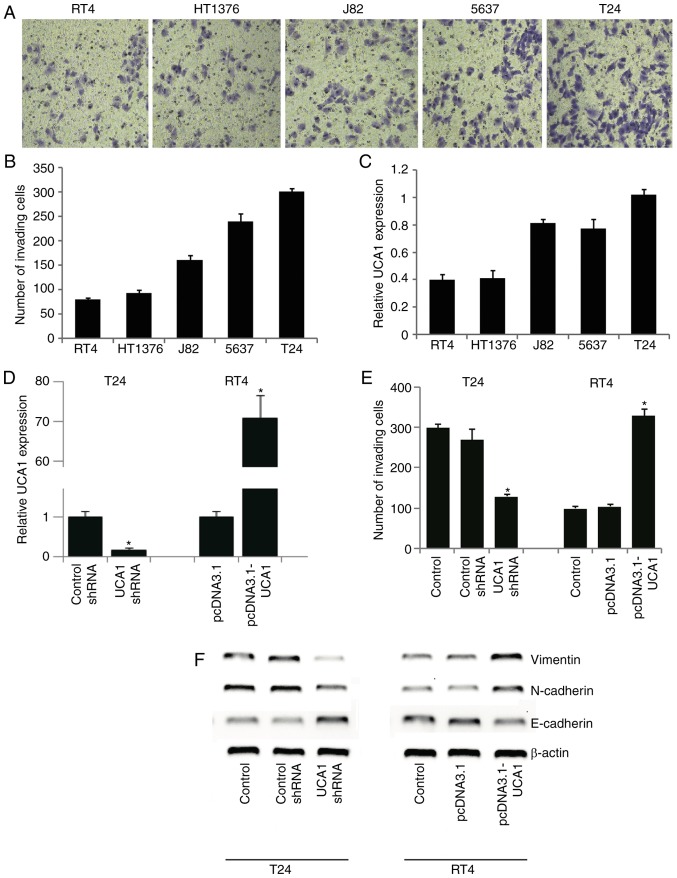
UCA1 modulated the invasion and EMT of bladder cancer cells
Previous studies revealed that UCA1 expression is associated with enhanced invasion ability of bladder cancer cells (24,36,37). We first investigated the relationship between the expression of UCA1 and the invasion ability of five bladder cancer cell lines. Comparison of Transwell assay results and qRT-PCR analysis of UCA1 expression showed that UCA1 expression was positively correlated with cell invasion ability (Fig. 1A-C). T24 cells showed stronger invasion capability and higher UCA1 expression levels, while RT4 cells showed relatively weaker invasion capability and lower UCA1 expression levels among the five tested bladder cancer cell lines. Knockdown of endogenous UCA1 in T24 cells by siRNA significantly (P<0.05) reduced the number of invading cells, while UCA1 overexpression in RT4 cells increased the number of invading cells significantly (P<0.05) (Fig. 1D and E), suggesting that UCA1 is closely involved in the invasion ability of bladder cancer cells.
Figure 1.
UCA1 modulated the invasion and EMT of bladder cancer cell lines. (A and B) Invasion capability of five bladder cancer cell lines was evaluated by Transwell assays. Crystal violet staining is shown in (A) and quantification of cells is shown in (B). (C) UCA1 mRNA expression levels in bladder cancer cell lines were evaluated by qRT-PCR. (D) T24 cells were transfected with UCA1 siRNA or control siRNA, and RT4 cells were transfected with UCA1-expressing pcDNA3.1 (pcDNA3.1-UCA1) or empty pcDNA3.1 vector (pcDNA3.1). Knockdown of UCA1 in T24 cells and overexpression of UCA1 in RT4 cells were validated by qRT-PCR. (E) Transwell assays in T24 and RT4 cells with UCA1 knockdown or overexpression. *P<0.05 vs. the control. (F) Western blot analysis of EMT markers E-cadherin, N-cadherin and Vimentin in response to UCA1 knockdown or overexpression. UCA1, urothelial carcinoma associated 1; EMT, epithelial-mesenchymal transition.
EMT is an important mechanism of enhanced invasion of bladder cancer cells. Therefore, we further investigated whether UCA1 modulated EMT in bladder cancer cells. The epithelial marker E-cadherin and mesenchymal markers N-cadherin and vimentin were examined by western blot analysis (Fig. 1F). UCA1 knockdown in T24 cells led to increased E-cadherin and decreased N-cadherin and vimentin, while UCA1 overexpression in RT4 cells inhibited E-cadherin and enhanced N-cadherin and Vimentin protein expression. Together these results suggest that UCA1 may modulate invasion and EMT of bladder cancer cells.
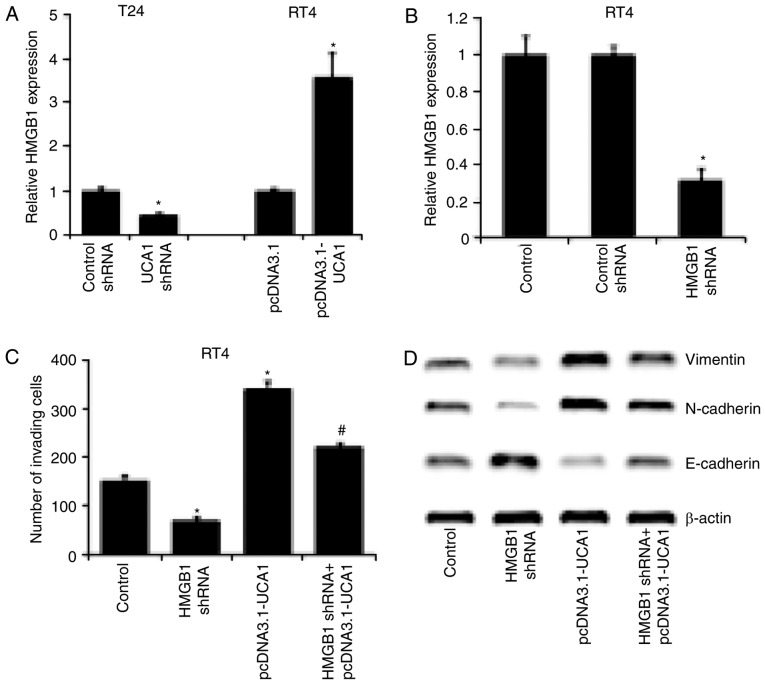
UCA1 promoted the invasion and EMT of bladder cancer cells by regulating HMGB1
To investigate the potential mechanism by which UCA1 regulates EMT in bladder cancer cells, we examined the effect of UCA1 on the expression of HMGB1, which is reported to be associated with the invasion ability of many types of human cancers including bladder cancer (24). qRT-PCR showed that HMGB1 mRNA expression was significantly (P<0.05) reduced by knockdown of UCA1 in T24 cells and increased by overexpression of UCA1 in RT4 cells (Fig. 2A). In addition, Transwell assays revealed that knockdown of HMGB1 by specific siRNA significantly inhibited the invasion of RT4 cells (Fig. 2B and C), similar to the effects of UCA1 knockdown. Of note, we found that knockdown of HMGB1 and overexpression of UCA1 significantly attenuated the effect of UCA1 on invasion and EMT of T24 cells (Fig. 2C and D). These results illustrated that UCA1 promoted the invasion and EMT of bladder cancer cells at least in part by regulating HMGB1.
Figure 2.
UCA1 promoted the invasion and EMT of bladder cancer cells by regulating HMGB1. (A) qRT-PCR analysis of HMGB1 mRNA expression in UCA1 knockdown and overexpressing T24 and RT4 cells, respectively. (B) Confirmation of HMGB1 knockdown using siRNA in RT4 cells by qRT-PCR. (C) Transwell assays in RT4 cells with HMGB1 knockdown (HMGB1 siRNA), UCA1 overexpression (pcDNA3.1-UCA1) or HMGB1 knockdown combined with UCA1 overexpression (HMGB1 shRNA+pcDNA3.1-UCA1). (D) Western blot analysis of EMT related markers E-cadherin, N-cadherin and Vimentin expression in RT4 cells with HMGB1 knockdown (HMGB1 siRNA), UCA1 overexpression (pcDNA3.1-UCA1) or HMGB1 knockdown combined with UCA1 overexpression (HMGB1 shRNA+pcDNA3.1-UCA1). *P<0.05 vs. the control, #P<0.05 vs. pcDNA3.1-UCA1. UCA1, urothelial carcinoma associated 1; EMT, epithelial-mesenchymal transition; HMGB1, high mobility group box 1.
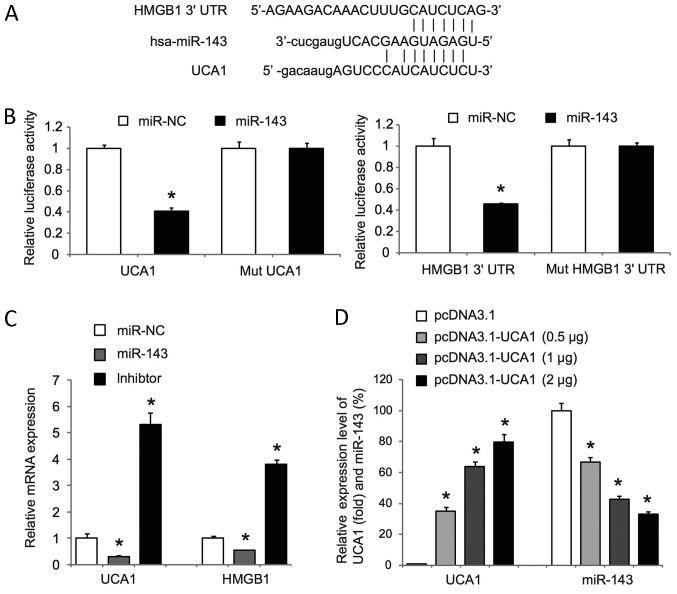
UCA1 induced HMGB1 expression through directly interacting with miR-143
Bioinformatics revealed putative binding sites for the tumor suppressive miR-143 within UCA1 and the 3′UTR of HMGB1 (Fig. 3A). Luciferase reporter assay, which was a standard way to prove the direct interaction between microRNAs and target genes (38), was used to determine whether miR-143 targets UCA1 and the 3′UTR of HMGB1. We cloned the full-length UCA1 and a fragment of the HMGB1 3′UTR containing miR-143 binding sites into luciferase reporter plasmids (psiCheck-2) and co-transfected the reporter plasmids with miR-143 mimics or scrambled mimics (miR-NC) into T24 cells. Luciferase assays showed that miR-143 mimics significantly reduced the activity of psiCheck-2-UCA1 and psiCheck-2-HMGB1 (Fig. 3B). Of note, mutations of the miR-143 binding sites in psiCheck-2-UCA1 and psiCheck-2-HMGB1 significantly abolished the effects on luciferase activity mediated by miR-143 mimics (Fig. 3B). In addition, miR-143 mimics significantly decreased UCA1 and HMGB1 expression, whereas miR-143 inhibitor mimics significantly increased UCA1 and HMGB1 expression in T24 cells (Fig. 3C). These data revealed that miR-143 could directly target and inhibit UCA1 and HMGB1 in T24 cells. We also observed that UCA1 overexpression in RT4 cells significantly repressed miR-143 expression in a dose-dependent manner (Fig. 3D). Taken together, our data suggest that UCA1 may act as a competing endogenous RNA of miR-143 and inhibit miR-143 to upregulate HMGB1 in bladder cancer cells.
Figure 3.
UCA1 induced HMGB1 expression through directly interacting with miR-143. (A) The putative binding sites of miR-143 in UCA1 and the 3′UTR of HMGB1. (B) Luciferase assays in T24 cells co-transfected with wild-type UCA1 (left) or HMGB1 3′UTR (right) luciferase vectors or mutant reporter vectors together with either miR-143 mimics (miR-143) or scrambled mimics (miR-NC). (C) qRT-PCR was used to detect the expression levels of UCA1 and HMGB1 mRNA in T24 cells transfected with scrambled mimics, miR-143 mimics or miR-143 inhibitor mimics. (D) qRT-PCR was performed to examine UCA1 and miR-143 mRNA expression levels in T24 cells transfected with pcDNA3.1 or pcDNA3.1-UCA1 expression plasmid at the indicated concentrations. *P<0.05. UCA1, urothelial carcinoma associated 1; EMT, epithelial-mesenchymal transition; HMGB1, high mobility group box 1.
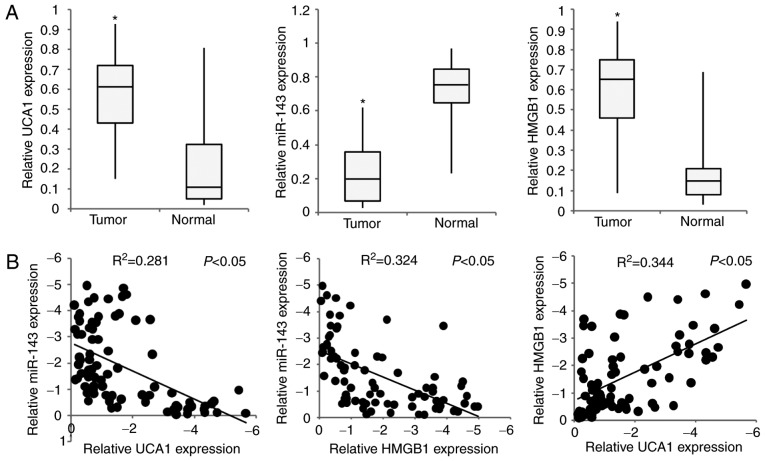
UCA1 and HMGB1 were upregulated and miR-143 was downregulated in bladder tumors
To examine the clinical significance of UCA1, HMGB1 and miR-143 in human bladder cancer development, qRT-PCR was performed to evaluate the expression levels of UCA1, miR-143 and HMGB1 mRNAs in a cohort of 81 bladder tissue specimens including 52 tumor tissues and 29 adjacent noncancerous tissues. As shown in Fig. 4A, UCA1 and HMGB1 were significantly upregulated while miR-143 was significantly downregulated in tumors compared with adjacent noncancerous tissues. In addition, correlation analysis revealed that UCA1 and HMGB1 expression levels had a positive correlation, but were both inversely correlated with miR-143 expression (Fig. 4B). Taken together, our observations suggest that dysregulation of the UCA1/miR-143/HMGB1 axis may be associated with the development and progression of bladder cancer.
Figure 4.
Expression levels of miR-143, UCA1 and HMGB1 in bladder cancer tissues. (A) Relative expression of miR-143, UCA1 and HMGB1 in 52 bladder tumor tissues (tumor) and 29 adjacent noncancerous tissues (normal). (B) Spearman's correlation analysis was carried out between miR-143, UCA1 and HMGB1 expression in 81 samples (52 bladder tumor tissues and 29 adjacent noncancerous tissues). *P<0.05. UCA1, urothelial carcinoma associated 1; EMT, epithelial-mesenchymal transition; HMGB1, high mobility group box 1.
Discussion
Increasing reports have revealed that dysregulated expression of lncRNAs is closely involved in the pathological development of a wide variety of human cancers including bladder cancer (8,9). UCA1 is a sensitive and specific oncogenic lncRNA in bladder cancer (16). Consistent with previous observations that high UCA1 expression was involved in cell invasion in many cancers as well as bladder cancer (24,36,37), our results clearly showed that cells with stronger invasion capability had higher UCA1 expression levels in bladder cancer cell lines in vitro. EMT is a well-characterized process that facilitates invasion and metastatic dissemination of human cancers (3,4). Therefore, we further investigated whether UCA1 could modulate EMT of bladder cancer cells. Gain and loss of function analysis showed that UCA1 knockdown increased E-cadherin and decreased N-cadherin and vimentin, while UCA1 overexpression led to the opposite results. These data suggest that UCA1 may modulate cell invasion by promoting EMT in bladder cancer cells.
The HMGB family could be divided into 3 subgroups, which are HMGB1, HMGB2 and HMGB3 (39). HMGB1 is widely distributed in the lymphoid tissue, brain, liver, lung, heart, spleen, kidney tissues, and exists in most organizations in the nucleus (40); The HMGB2/3 distribution is limited. HMGB2 is mainly distributed in the testicular and lymphoid tissues (41,42), while HMGB3 is found mainly in embryos (43). This is why we chose HMGB1 as our candidate.
To investigate the potential mechanism by which UCA1 regulates EMT in bladder cancer cells, we examined the effect of UCA1 on the expression of HMGB1. We found that HMGB1 mRNA expression was significantly reduced by knockdown of UCA1 in T24 cells and increased by overexpression of UCA1 in RT4 cells, suggesting that UCA1 can positively regulate HMGB1 mRNA expression. Cellular function assays further revealed that knockdown of HMGB1 significantly inhibited the invasion of RT4 cells and attenuated the effect of UCA1 on invasion and EMT of T24 cells. These results revealed that UCA1 promoted the invasion and EMT of bladder cancer cells, at least in part by inducing HMGB1. And in order to look into the biological function of HMGB1 in bladder cancer, we might pursue another research on how the protein level of HMGB1 affected by UCA1.
LncRNAs interact with miRNAs to function as miRNA sponges or inhibitors and also modulate the repression of miRNA targets. Increasing reports have revealed that UCA1 functions as an oncogenic lncRNA by interacting with and inhibiting tumor suppressive miRNAs such as miR-507 (44), miR-145 (24), miR-16 (45) and miR-216b (46). Based on bioinformatics and luciferase reporter assays, we confirmed binding sites of the tumor suppressive miR-143 within UCA1 and the 3′UTR of HMGB1. In addition, we observed that UCA1 overexpression significantly repressed miR-143 expression in a dose-dependent manner in RT4 cells. Our observation was closely consistent with a recently published report demonstrating that UCA1 promoted bladder cancer cell migration and invasion by the hsa-mir145-ZEB1/2-FSCN1 pathway (24). Similar to miR-143, miR-145 was also reported to be a tumor suppressive gene and a negative regulator of EMT (47–49). Thus, UCA1 might function as an oncogene by sponging EMT-related miRNAs.
miR-143 was already known to act as a tumor suppressor in multiple cancers, including bladder cancer (34). According to the literature found in Pubmed, miR-143 was found to suppress EMT and cell invasion in multiple cancers, including spinal glioblastoma (50), esophageal squamous cell carcinoma (51), and breast cancer (52). Our research showed that UCA1 may act as a competing endogenous RNA of miR-143 and inhibit miR-143 to upregulate HMGB1, result in promoting the invasion and EMT of bladder cancer cells. Taken together, we believe that miR-143 might also affect EMT in bladder cancer. Further studies were needed to look into the function of miR-143 on EMT and invasion in bladder cancer.
Expression analysis on clinical bladder cancer specimens also revealed that UCA1 and HMGB1 expression levels were positively correlated but were both inversely correlated with miR-143 expression. Taken together, our data suggest that UCA1 may act as a miRNA sponge to miR-143 and inhibit miR-143 to upregulate HMGB1 in bladder cancer cells. The limitation in this research was that this study only included in vitro models. Our future studies will pursue these findings in an in vivo model.
In conclusion, our study provided evidence that UCA1 promotes the invasion and EMT of bladder cancer by regulating the miR-143/HMGB1 pathway, which may play an important regulatory role in the pathology of bladder cancer.
Acknowledgements
The authors would like to thank the Guangdong and Shenzhen Key Laboratory of Male Reproductive Medicine and Genetics, Institute of Urology, Peking University Shenzhen Hospital. The present study was supported by Shenzhen Health and Family Planning System Scientific Research Project (grant no. 201401033, for Junhua Luo), the Science and Technology Development Fund Project of Shenzhen (grant no JCYJ20150403091443304, for Shangqi Yang), the fund of ‘San-ming’ Project of Medicine in Shenzhen and the fund of the Guangdong Key Medical Subject.
References
- 1.Dancik GM, Theodorescu D. Pharmacogenomics in bladder cancer. Urol Oncol. 2014;32:16–22. doi: 10.1016/j.urolonc.2013.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ploussard G, Shariat SF, Dragomir A, Kluth LA, Xylinas E, Masson-Lecomte A, Rieken M, Rink M, Matsumoto K, Kikuchi E, et al. Conditional survival after radical cystectomy for bladder cancer: Evidence for a patient changing risk profile over time. Eur Urol. 2014;66:361–370. doi: 10.1016/j.eururo.2013.09.050. [DOI] [PubMed] [Google Scholar]
- 3.Gonzalez DM, Medici D. Signaling mechanisms of the epithelial-mesenchymal transition. Sci Signal. 2014;7:re8. doi: 10.1126/scisignal.2005189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yun SJ, Kim WJ. Role of the epithelial-mesenchymal transition in bladder cancer: From prognosis to therapeutic target. Korean J Urol. 2013;54:645–650. doi: 10.4111/kju.2013.54.10.645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Autuoro JM, Pirnie SP, Carmichael GG. Long noncoding RNAs in imprinting and X chromosome inactivation. Biomolecules. 2014;4:76–100. doi: 10.3390/biom4010076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Caley DP, Pink RC, Trujillano D, Carter DR. Long noncoding RNAs, chromatin, and development. Scientific World Journal. 2010;10:90–102. doi: 10.1100/tsw.2010.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nagano T, Fraser P. No-nonsense functions for long noncoding RNAs. Cell. 2011;145:178–181. doi: 10.1016/j.cell.2011.03.014. [DOI] [PubMed] [Google Scholar]
- 8.Yin DD, Liu ZJ, Zhang E, Kong R, Zhang ZH, Guo RH. Decreased expression of long noncoding RNA MEG3 affects cell proliferation and predicts a poor prognosis in patients with colorectal cancer. Tumour Biol. 2015;36:4851–4859. doi: 10.1007/s13277-015-3139-2. [DOI] [PubMed] [Google Scholar]
- 9.Zhang Q, Su M, Lu G, Wang J. The complexity of bladder cancer: Long noncoding RNAs are on the stage. Mol Cancer. 2013;12:101. doi: 10.1186/1476-4598-12-101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zheng X, Hu H, Li S. High expression of lncRNA PVT1 promotes invasion by inducing epithelial-to-mesenchymal transition in esophageal cancer. Oncol Lett. 2016;12:2357–2362. doi: 10.3892/ol.2016.5026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lu M, Liu Z, Li B, Wang G, Li D, Zhu Y. The high expression of long non-coding RNA PANDAR indicates a poor prognosis for colorectal cancer and promotes metastasis by EMT pathway. J Cancer Res Clin Oncol. 2017;143:71–81. doi: 10.1007/s00432-016-2252-y. [DOI] [PubMed] [Google Scholar]
- 12.Cesana M, Cacchiarelli D, Legnini I, Santini T, Sthandier O, Chinappi M, Tramontano A, Bozzoni I. A long noncoding RNA controls muscle differentiation by functioning as a competing endogenous RNA. Cell. 2011;147:358–369. doi: 10.1016/j.cell.2011.09.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dey BK, Pfeifer K, Dutta A. The H19 long noncoding RNA gives rise to microRNAs miR-675-3p and miR-675-5p to promote skeletal muscle differentiation and regeneration. Genes Dev. 2014;28:491–501. doi: 10.1101/gad.234419.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kallen AN, Zhou XB, Xu J, Qiao C, Ma J, Yan L, Lu L, Liu C, Yi JS, Zhang H, et al. The imprinted H19 lncRNA antagonizes let-7 microRNAs. Mol Cell. 2013;52:101–112. doi: 10.1016/j.molcel.2013.08.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Liang WC, Fu WM, Wong CW, Wang Y, Wang WM, Hu GX, Zhang L, Xiao LJ, Wan DC, Zhang JF, Waye MM. The lncRNA H19 promotes epithelial to mesenchymal transition by functioning as miRNA sponges in colorectal cancer. Oncotarget. 2015;6:22513–22525. doi: 10.18632/oncotarget.4154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wang XS, Zhang Z, Wang HC, Cai JL, Xu QW, Li MQ, Chen YC, Qian XP, Lu TJ, Yu LZ, et al. Rapid identification of UCA1 as a very sensitive and specific unique marker for human bladder carcinoma. Clin Cancer Res. 2006;12:4851–4858. doi: 10.1158/1078-0432.CCR-06-0134. [DOI] [PubMed] [Google Scholar]
- 17.Huang J, Zhou N, Watabe K, Lu Z, Wu F, Xu M, Mo YY. Long non-coding RNA UCA1 promotes breast tumor growth by suppression of p27 (Kip1) Cell Death Dis. 2014;5:e1008. doi: 10.1038/cddis.2013.541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chen P, Wan D, Zheng D, Zheng Q, Wu F, Zhi Q. Long non-coding RNA UCA1 promotes the tumorigenesis in pancreatic cancer. Biomed Pharmacother. 2016;83:1220–1226. doi: 10.1016/j.biopha.2016.08.041. [DOI] [PubMed] [Google Scholar]
- 19.Zheng Q, Wu F, Dai WY, Zheng DC, Zheng C, Ye H, Zhou B, Chen JJ, Chen P. Aberrant expression of UCA1 in gastric cancer and its clinical significance. Clin Transl Oncol. 2015;17:640–646. doi: 10.1007/s12094-015-1290-2. [DOI] [PubMed] [Google Scholar]
- 20.Ni B, Yu X, Guo X, Fan X, Yang Z, Wu P, Yuan Z, Deng Y, Wang J, Chen D, Wang L. Increased urothelial cancer associated 1 is associated with tumor proliferation and metastasis and predicts poor prognosis in colorectal cancer. Int J Oncol. 2015;47:1329–1338. doi: 10.3892/ijo.2015.3109. [DOI] [PubMed] [Google Scholar]
- 21.Wang HM, Lu JH, Chen WY, Gu AQ. Upregulated lncRNA-UCA1 contributes to progression of lung cancer and is closely related to clinical diagnosis as a predictive biomarker in plasma. Int J Clin Exp Med. 2015;8:11824–11830. [PMC free article] [PubMed] [Google Scholar]
- 22.He A, Hu R, Chen Z, Liao X, Li J, Wang D, Lv Z, Liu Y, Wang F, Mei H. Role of long noncoding RNA UCA1 as a common molecular marker for lymph node metastasis and prognosis in various cancers: A meta-analysis. Oncotarget. 2017;8:1937–1943. doi: 10.18632/oncotarget.12463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Xiao C, Wu CH, Hu HZ. LncRNA UCA1 promotes epithelial-mesenchymal transition (EMT) of breast cancer cells via enhancing Wnt/beta-catenin signaling pathway. Eur Rev Med Pharmacol Sci. 2016;20:2819–2824. [PubMed] [Google Scholar]
- 24.Xue M, Pang H, Li X, Li H, Pan J, Chen W. Long non-coding RNA urothelial cancer-associated 1 promotes bladder cancer cell migration and invasion by way of the hsa-miR-145-ZEB1/2-FSCN1 pathway. Cancer Sci. 2016;107:18–27. doi: 10.1111/cas.12844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wang W, Jiang H, Zhu H, Zhang H, Gong J, Zhang L, Ding Q. Overexpression of high mobility group box 1 and 2 is associated with the progression and angiogenesis of human bladder carcinoma. Oncol Lett. 2013;5:884–888. doi: 10.3892/ol.2012.1091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yang GL, Zhang LH, Bo JJ, Huo XJ, Chen HG, Cao M, Liu DM, Huang YR. Huang, Increased expression of HMGB1 is associated with poor prognosis in human bladder cancer. J Surg Oncol. 2012;106:57–61. doi: 10.1002/jso.23040. [DOI] [PubMed] [Google Scholar]
- 27.Chang BP, Wang DS, Xing JW, Yang SH, Chu Q, Yu SY. miR-200c inhibits metastasis of breast cancer cells by targeting HMGB1. J Huazhong Univ Sci Technolog Med Sci. 2014;34:201–206. doi: 10.1007/s11596-014-1259-3. [DOI] [PubMed] [Google Scholar]
- 28.Chen YC, Statt S, Wu R, Chang HT, Liao JW, Wang CN, Shyu WC, Lee CC. High mobility group box 1-induced epithelial mesenchymal transition in human airway epithelial cells. Sci Rep. 2016;6:18815. doi: 10.1038/srep18815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cheng M, Liu H, Zhang D, Liu Y, Wang C, Liu F, Chen J. HMGB1 enhances the AGE-induced expression of CTGF and TGF-β via RAGE-dependent signaling in renal tubular epithelial cells. Am J Nephrol. 2015;41:257–266. doi: 10.1159/000381464. [DOI] [PubMed] [Google Scholar]
- 30.Lynch J, Nolan S, Slattery C, Feighery R, Ryan MP, McMorrow T. High-mobility group box protein 1: A novel mediator of inflammatory-induced renal epithelial-mesenchymal transition. Am J Nephrol. 2010;32:590–602. doi: 10.1159/000320485. [DOI] [PubMed] [Google Scholar]
- 31.Zhu L, Li X, Chen Y, Fang J, Ge Z. High-mobility group box 1: A novel inducer of the epithelial-mesenchymal transition in colorectal carcinoma. Cancer Lett. 2015;357:527–534. doi: 10.1016/j.canlet.2014.12.012. [DOI] [PubMed] [Google Scholar]
- 32.Huang Z, Zhong Z, Zhang L, Wang X, Xu R, Zhu L, Wang Z, Hu S, Zhao X. Down-regulation of HMGB1 expression by shRNA constructs inhibits the bioactivity of urothelial carcinoma cell lines via the NF-κB pathway. Sci Rep. 2015;5:12807. doi: 10.1038/srep12807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Liao H, Xiao Y, Hu Y, Xiao Y, Yin Z, Liu L. Suppression of cellular proliferation and invasion by HMGB1 knockdown in bladder urothelial carcinoma cells. Oncol Res. 2014;22:235–245. doi: 10.3727/096504015X14267282610858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lin T, Dong W, Huang J, Pan Q, Fan X, Zhang C, Huang L. MicroRNA-143 as a tumor suppressor for bladder cancer. J Urol. 2009;181:1372–1380. doi: 10.1016/j.juro.2008.10.149. [DOI] [PubMed] [Google Scholar]
- 35.Livak KJ, Schmittgen TD. Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) method. Methods. 2001;25:402–408. doi: 10.1006/meth.2001.1262. [DOI] [PubMed] [Google Scholar]
- 36.Wang F, Li X, Xie X, Zhao L, Chen W. UCA1, a non-protein-coding RNA up-regulated in bladder carcinoma and embryo, influencing cell growth and promoting invasion. FEBS Lett. 2008;582:1919–1927. doi: 10.1016/j.febslet.2008.05.012. [DOI] [PubMed] [Google Scholar]
- 37.Xue M, Li X, Li Z, Chen W. Urothelial carcinoma associated 1 is a hypoxia-inducible factor-1α-targeted long noncoding RNA that enhances hypoxic bladder cancer cell proliferation, migration, and invasion. Tumour Biol. 2014;35:6901–6912. doi: 10.1007/s13277-014-1925-x. [DOI] [PubMed] [Google Scholar]
- 38.Vella MC, Reinert K, Slack FJ. Architecture of a validated microRNA: Target interaction. Chem Biol. 2004;11:1619–1623. doi: 10.1016/j.chembiol.2004.09.010. [DOI] [PubMed] [Google Scholar]
- 39.Yanai H, Ban T, Wang Z, Choi MK, Kawamura T, Negishi H, Nakasato M, Lu Y, Hangai S, Koshiba R, et al. HMGB proteins function as universal sentinels for nucleic-acid-mediated innate immune responses. Nature. 2009;462:99–103. doi: 10.1038/nature08512. [DOI] [PubMed] [Google Scholar]
- 40.Bonaldi T, Talamo F, Scaffidi P, Ferrera D, Porto A, Bachi A, Rubartelli A, Agresti A, Bianchi ME. Monocytic cells hyperacetylate chromatin protein HMGB1 to redirect it towards secretion. EMBO J. 2003;22:5551–5560. doi: 10.1093/emboj/cdg516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mosevitsky MI, Novitskaya VA, Iogannsen MG, Zabezhinsky MA. Tissue specificity of nucleo-cytoplasmic distribution of HMG1 and HMG2 proteins and their probable functions. Eur J Biochem. 1989;185:303–310. doi: 10.1111/j.1432-1033.1989.tb15116.x. [DOI] [PubMed] [Google Scholar]
- 42.Bucci LR, Brock WA, Meistrich ML. Heterogeneity of high-mobility-group protein 2. Enrichment of a rapidly migrating form in testis. Biochem J. 1985;229:233–240. doi: 10.1042/bj2290233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Moleri S, Cappellano G, Gaudenzi G, Cermenati S, Cotelli F, Horner DS, Beltrame M. The HMGB protein gene family in zebrafish: Evolution and embryonic expression patterns. Gene Expr Patterns. 2011;11:3–11. doi: 10.1016/j.gep.2010.08.006. [DOI] [PubMed] [Google Scholar]
- 44.Wei Y, Sun Q, Zhao L, Wu J, Chen X, Wang Y, Zang W, Zhao G. LncRNA UCA1-miR-507-FOXM1 axis is involved in cell proliferation, invasion and G0/G1 cell cycle arrest in melanoma. Med Oncol. 2016;33:88. doi: 10.1007/s12032-016-0804-2. [DOI] [PubMed] [Google Scholar]
- 45.Li HJ, Li X, Pang H, Pan JJ, Xie XJ, Chen W. Long non-coding RNA UCA1 promotes glutamine metabolism by targeting miR-16 in human bladder cancer. Jpn J Clin Oncol. 2015;45:1055–1063. doi: 10.1093/jjco/hyv132. [DOI] [PubMed] [Google Scholar]
- 46.Wang F, Ying HQ, He BS, Pan YQ, Deng QW, Sun HL, Chen J, Liu X, Wang SK. Upregulated lncRNA-UCA1 contributes to progression of hepatocellular carcinoma through inhibition of miR-216b and activation of FGFR1/ERK signaling pathway. Oncotarget. 2015;6:7899–7917. doi: 10.18632/oncotarget.3219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Chiou GY, Cherng JY, Hsu HS, Wang ML, Tsai CM, Lu KH, Chien Y, Hung SC, Chen YW, Wong CI, et al. Cationic polyurethanes-short branch PEI-mediated delivery of Mir145 inhibited epithelial-mesenchymal transdifferentiation and cancer stem-like properties and in lung adenocarcinoma. J Control Release. 2012;159:240–250. doi: 10.1016/j.jconrel.2012.01.014. [DOI] [PubMed] [Google Scholar]
- 48.Ling DJ, Chen ZS, Zhang YD, Liao QD, Feng JX, Zhang XY, Shi TS. MicroRNA-145 inhibits lung cancer cell metastasis. Mol Med Rep. 2015;11:3108–3114. doi: 10.3892/mmr.2014.3036. [DOI] [PubMed] [Google Scholar]
- 49.Ren D, Wang M, Guo W, Zhao X, Tu X, Huang S, Zou X, Peng X. Wild-type p53 suppresses the epithelial-mesenchymal transition and stemness in PC-3 prostate cancer cells by modulating miR-145. Int J Oncol. 2013;42:1473–1481. doi: 10.3892/ijo.2013.1825. [DOI] [PubMed] [Google Scholar]
- 50.Yan Y, Wu J, Wu M, Xia Y, Tang W, Liao Z. MiR-143 suppresses the epithelial-mesenchymal transition of spinal glioblastoma through down-regulation of ERK5. Oncotarget. 2016 doi: 10.18632/oncotarget.12977. (Epub ahead of print) [DOI] [Google Scholar]
- 51.Liu J, Mao Y, Zhang D, Hao S, Zhang Z, Li Z, Li B. RETRACTED: MiR-143 inhibits tumor cell proliferation and invasion by targeting STAT3 in esophageal squamous cell carcinoma. Cancer Lett. 2016;373:97–108. doi: 10.1016/j.canlet.2016.01.023. [DOI] [PubMed] [Google Scholar]
- 52.Zhai L, Ma C, Li W, Yang S, Liu Z. miR-143 suppresses epithelial-mesenchymal transition and inhibits tumor growth of breast cancer through down-regulation of ERK5. Mol Carcinog. 2016;55:1990–2000. doi: 10.1002/mc.22445. [DOI] [PubMed] [Google Scholar]