Abstract
Background
Low-and-Middle-Income-Countries (LMICs) account for 75% of global suicides. While primary care populations in high-income countries (HIC) typically have higher prevalence of suicidal behavior relative to general populations, few studies have explored suicidal behavior among general medical outpatients in LMICs. This study addresses the research gap by characterizing potential risk factors for suicidal ideation in a large general medical outpatient setting in rural Kenya.
Methods
A cross-sectional study of adult general medical outpatients attending a rural sub-county hospital in Kaloleni, Kenya. Primary outcomes included major depressive disorder (MDD), posttraumatic stress disorder (PTSD) and suicidal behavior measured by the Mini International Neuropsychiatric Interview (MINI 5.0). We use binary logistic regression to model suicidality, mental disorders, intimate partner violence, and lifetime abuse.
Results
394 outpatients completed the assessment. The prevalence of SI over the past month was 20%. 18% of those with suicidal ideation over the past month also attempted suicide in the past month. Participants who met criteria for MDD (suicidality item removed) were 19 times [CI: 4.56, 79.05] more likely to report suicidal ideation compared to those without MDD (adjusted odds ratio 12.15 [CI: 2.66, 55.49]).
Limitations
This was a cross sectional study design with convenience sampling and hence vulnerable to selection and recall bias.
Conclusion
The prevalence of SI and its strong association with actual suicide attempt in this population, make an urgent public health case for intervention. These data identify MDD as a highly significant correlate of SI.
Keywords: Suicide, Suicidal ideation, Depression, Posttraumatic stress disorder (PTSD), Global mental health, Sub-Saharan Africa
1. Introduction
Globally, suicide is the fifteenth leading cause of death and claims 800,000 lives each year. 75% of all suicides occur in low-and middle-income countries (LMICs), and the majority are young adults (World Health Organization, 2014). Suicide is a focus of the World Health Organization (WHO), with a goal of 10% reduction by 2020 (World Health Organization, 2014).
Across diverse populations, the risk of suicide is significantly higher among individuals with poor physical and/or mental health, compared with their healthier counterparts (Scott et al., 2010; Whittier et al., 2016). Perhaps reflecting this fact is the higher prevalence of suicidal behavior, defined as suicide ideation, plan and/or attempt, among primary care patient populations relative to general populations (Ani et al., 2008; Berghöfer et al., 2014). Studies of populations in sub-Saharan Africa also find that the prevalence of suicidal behavior is higher among primary care patients compared with general populations (Fekadu et al., 2016). Nearly half of all suicide completers have contact with their primary care provider within one month of committing suicide and 75% have contact in the year prior (Luoma, Martin, and Pearson, 2002)—presenting an enormous opportunity for prevention.
In both HICs and sub-Saharan Africa, suicidal ideation is now understood to be a key step in the progression to suicide attempt and hence a target for early intervention to prevent suicide (Fekadu et al., 2016; Joe et al., 2008; Klonsky et al., 2016). While the rate of transition from suicidal ideation to suicide attempt is thought to be relatively low in HICs (e.g., 7.4% over 2 years), (Have et al., 2009) among sub-Saharan African patients, the transition from suicidal ideation to suicide attempt is higher: 30–50% of patients with suicidal ideation attempt suicide in the subsequent year (Fekadu et al., 2016; Joe et al., 2008).
Despite the fact that LMICs account for the vast majority of global suicides, and the strong association between suicidal ideation and suicide attempt in sub-Saharan Africa, few studies have focused on risk factors for suicidal ideation. There have been several studies of urban sub-Saharan African populations that characterize the demographic, mental and physical health parameters of suicidal behavior, symptoms or risk in general outpatient settings (Aillon et al., 2013; Fekadu et al., 2016; Whittier et al., 2016), but these studies do not center on suicidal ideation, its predictors or address the large rural populations that make up the majority of those affected by mental disorders in many LMICs. This study aims to address this critical research gap by characterizing potential risk factors for suicidal ideation in a large primary care setting in rural Kenya.
The Kaloleni Sub-County of Kenya (population 298,287) is a rural coastal region near Mombasa with some of the poorest health indicators in Kenya. Kaloleni has high rates of exposure to traumatic experiences, including high levels of intimate partner violence (39.4%), alcohol abuse (17.6%), deaths related to HIV infection (6% prevalence) and extreme poverty (Kenya Inter Agency Rapid Assessment ((KIRA), 2014), 2014; Kenya National Bureau of Statistics, 2005). The poverty rate in Kaloleni is at 70.8% compared with a national rate of 45.9%; and the county ranks 39 out of 47 counties in wealth (Kenya, 2013). Kaloleni is the focus of the Integrated Primary Health Care (IPHC) Programme. Launched in 2011, the IPHC is a public-private collaboration between Aga Khan University East Africa (AKU-EA), the Kenyan Ministry of Health and the University of California San Francisco (UCSF). IPHC's objective is to improve access to quality medical care in Kaloleni, including mental health care for common mental disorders and it is for this reason that we harnessed its resources.
Public Sector Healthcare Delivery in Kenya (Table 1)
Table 1.
Organization of health service delivery around a four tiered health system in Kenya.
| Care Tier | Care Type | Core Services Provided | Facility Type | Provider Type |
|---|---|---|---|---|
| 1 | Community care | Facilitate community diagnosis, management & referral. | Household and community based outreach care. | Community health workers. |
| 2 | Primary Care: Dispensaries, clinics and health centers. | Basic outpatient diagnostic, medical, surgical & rehabilitative services. | 1–2 exam rooms, | Nurses and clinical officers |
| 3 | Secondary Care Referral: Primary and secondary care hospitals. | Comprehensive in patient diagnostic, medical, surgical and rehabilitative care, including reproductive health services | 50 exam rooms and varying number of inpatient beds, 24 h access | Nurses, clinical officers and physicians |
| 4 | Tertiary Care Referral: National referral hospitals and specialized hospitals. | Highly specialized health care | Typically 200 exam rooms and 500 inpatient beds, 24 h access | Nurses, clinical officers and physicians |
Note: Clinical officers (Cos) provide a great deal of healthcare in Kenya. They receive approximately 3 years of clinical training – more than nurses and less than physicians and they function between nurses and doctors with regards to the complexity of the cases that they manage.
Kenya's health service delivery is organized around a 4 tiered health system. These include: community, primary care, county referral and national referral services. The central government is responsible for health care provision in the national referral hospitals. The other 3 tiers fall under the county governments (Ministry of Health, 2012; Kenya Healthcare Federation, 2016). Dispensaries (tier 2) are the most numerous type of healthcare facility and are designed to be the first point of contact for patients. They are stafied by nurses and provide preventative health-care and treatment for simple conditions, such as cold, flu and uncomplicated malaria. Conditions that cannot be treated at dispensaries are referred to health centers (tier 2), which are stafied by clinical officers (approximately 2 years of clinical training) or nurses. Health centers serve populations of about 80,000 people and provide more comprehensive outpatient primary care than dispensaries, but continue to focus primarily on preventative care. Conditions that cannot be treated at health centers are referred to the county referral hospitals (tier 3), the staff for which typically includes physicians. As opposed to the preventative focus of tiers 1 and 2 county referral hospitals can address complicated medical conditions and provide more extensive surgical services. County referral hospitals are the first level at which inpatient beds are available and have a varying bed capacity. The final healthcare referral point is tier 4, which includes national tertiary referral hospitals, staffed by physicians and providing a wide range of highly specialized inpatient and outpatient services, including psychiatric care.
While Kenya's referral protocols guide patients to higher healthcare tiers as needed, many individuals elect to go to their nearest health facility, regardless of its tier. For example, 90% of the patients seen at Mariakani sub-county hospital (tier 3) in Kaloleni are local residents who self-refer for healthcare, rather than being referred by tier 1 or 2 facilities (Hospital, 2015). Given that sub-county hospitals are widely dispersed across Kenya and provide access to physicians and specialty care, they are the ideal setting in which to develop mental health care services. We assessed mental health care needs study of out-patients served by the general medical outpatient clinics of Mariakani Hospital. We included measures of suicide, depression, trauma exposure, post-traumatic-stress disorder (PTSD), substance abuse and perceived physical health.
2. Methods
2.1. Study Site
Mariakani Sub-county hospital serves a catchment of over 300,000 people with a bed capacity of 68. No formal mental health care services are currently provided. The medical staff includes 7 doctors, 40 nurses and 11 clinical officers. The number of outpatients seen per day in the general medical outpatient clinic ranges from 80 to 150 per day.
As mentioned above, the vast majority of the of the clinic's patients (90%) are local self-referrals who have not seen any other provider for their chief complaint (Hospital, 2015). Like other sub-county hospital general medical outpatient clinics in Kenya, Mariakani outpatient clinic provides urgent and emergency healthcare. Emergencies and urgent cases are handled in the general outpatient clinic. Many of the patients attending Marikani general medical outpatient clinic present with acute healthcare needs including severe respiratory tract infections, malaria and serious injuries. Also unlike high income country counterparts, only a very small group of patients present for scheduled appointments for preventative or follow-up care.
2.2. Target population
Outpatients from the general medical care outpatient clinic aged 18 years and above at the Mariakani Sub-county hospital.
2.3. Participants
Participants were 18 years of age or older, seeking care at the Mariakani Sub-county Hospital, able to give informed consent and available for duration of interview. Exclusion criteria were self-reported need for urgent/emergent medical or mental health inpatient care (e.g., acute psychosis). Of note, suicidality was not an exclusion criteria.
2.4. Procedures
We recruited participants using a convenience sample of eligible participants seeking care at the Outpatient Department (OPD) of Mariakani Sub-county Hospital. The research team approached patients in the waiting area and informed them that KEMRI was conducting health research within the facility. The research team inquired if they had some time to spare and whether they would be interested in hearing more details related to the study following their consultation. They were reassured that their choice to participate would in no way affect their ability to receive healthcare services. Following their clinic appointment, the research team invited patients who had expressed interest to meet in a private room where they undertook consenting before enrollment. Prospective participants were informed that the study was a mental health needs assessment to identify the burden of common mental illnesses in the Mariakani Hospital general outpatient clinics. They were further informed that screening and enrollment, if eligible, would take approximately 20 min and completion of measures would take an additional 60 min.
2.5. Sample size
We calculated the study sample size using epidemiological data from other regions of Kenya, where the prevalence of mood disorder was estimated at 39%. (Aillon et al., 2013). The sample size for this study was based on the maximum value obtained (the prevalence affective disorder for a similar setting). Using this formula, we required a sample of 366 eligible participants to obtain a 95% confidence interval and an alpha of 5%.
2.6. Study design
A cross-sectional survey conducted between April 2015 and September 2015 in a rural sub-county hospital setting.
2.6.1. Data collection Instruments
The study Principal Investigator (LO) designed a questionnaire which we used to collect socio-demographic information related to age, gender, level of education and religion. We used an additional structured questionnaire (Socio-Economic Survey–SEARCH instrument) which we adapted from the instrument used in the Sustainable East Africa Research on Community Health (SEARCH) study in the same region (Thirumurthy, n.d.) and contained 27 items spanning both formal (e.g., wages, self-employed business) and informal (e.g., farming) income and time spent earning the income.
We used the MINI international Neuropsychiatric Interview version 5.0 (Sheehan et al., 1998) sections to assess mood disorders, generalized anxiety disorders, PTSD, alcohol and substance use and suicidality. The following questions were part of the suicidality questionnaire (yes/ no): (1) “In the past month did you think about suicide?”;(2) “In the past month did you have a plan for suicide?”; (3) “In the past month did you attempt suicide?”; and (4) “In your lifetime, did you ever attempt suicide?”. We coded “Yes” responses: to (1) as suicidal ideation over the past month; to (2) as suicide plan in the past month; to (3) as a suicide attempt in the past month; and to (4) as a lifetime suicide attempt.
The Trauma History Questionnaire (THQ) (Hooper et al., 1993) used was a 24-item self-report measure to examine experiences with potentially traumatic events such as crime, general disaster, and sexual and physical assault using a yes/no format. For each event endorsed, respondents were asked to provide the frequency of the event as well as their age at the time of the event.
We used the Conflict Tactic Scale (CTS) (Straus, 1979) to measure psychological and physical attacks on a partner in a marital, cohabiting, or dating relationship; and also use of negotiation as an assessment of IPV. Only participants reporting on a dating, cohabiting or marital relationship were assessed using this instrument. For this study, we modified the CTS to refer to the prior week, only, rather than the prior year. In data analysis, we summed CTS items 4–19 to create a composite score a verbal and physical abuse in the context of an intimate partner relationship.
The WHOQOL-BREF (Skevington et al., n.d.) assesses individuals' perceptions of their position in life in the context of the culture and value systems in which they live and in relation to their goals, expectations, standards and concerns. WHO developed it collaboratively in some 15 cultural settings over several years and has now been field tested in 37 field centers. It is a 26-question assessment that currently exists indirectly comparable forms in 29 language versions. WHOQOL-BREF subscales include an overall quality of life index, as well as sub-scales for physical, social, environmental and psychological health.
2.7. Data collection
Three trained research assistants collected the data. A five member team, including the PI and the co-investigators provided them with a five-day training course on consenting, administering the study tools and ethical considerations.
2.8. Data analysis
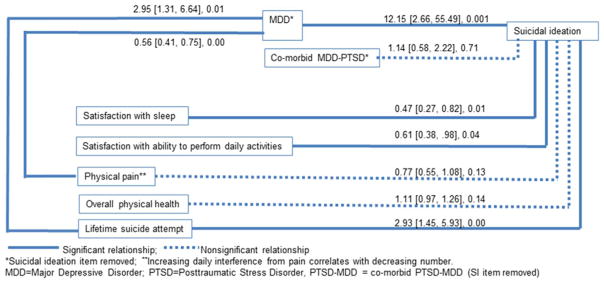
Experienced data entry clerks entered the data into a Microsoft Access database. The data were extracted from excel and analyzed using STATA (version 12.1). We analyzed sample characteristics for those with and without suicidal ideation in the past month. We used binary logistic regression to identify directionality and significance of the relationships between past month suicidal ideation for demographic, mental health, lifetime suicide attempt, intimate partner violence, other abuse and quality of life variables. We characterized common mental disorders. Given the established gender differences in mood and anxiety disorders, we conducted sub-group analysis by gender, also using binary logistic regression to assess the direction and strength of relationships with gender (Seedat et al., 2009). Using binary logistic regression, we modelled past month suicidal ideation to determine its relationship with demographic, mental health, lifetime suicide attempt, intimate partner violence, other abuse and quality of life variables, with sub-group analyses by gender. Lastly, we constructed figures of hypothetical relationships between variables that were significantly associated with suicidal ideation for women and men, then superimposed the adjusted odds ratios derived from multivariate logistic regression on a path diagram. An additional step included regression of variables that had a significant relationship with MDD. To preserve clarity of the diagram, we included only the variables with a significant relationship to MDD.
2.9. Ethics
We obtained approval to carry out the study from the UCSF Committee on Human Research, Scientific and Ethics Review Committee at the Kenya Medical Research Institute (KEMRI) and the Health Research Ethics Committee at AKU-EA. We also obtained written permission to carry out the research from county health and research committee in Kilifi County and the medical superintendent of Mariakani Sub-county Hospital. Participants signed written informed consent after detailed explanation of the study purpose. All consents and study documents were in both English and Kiswahili translations. We asked recruited participants to pick the language they preferred for the interview.
3. Results
We recruited 5 days a week for a period of 2 months (July-September 2015). 880 prospective participants were approached for the study, and of these 394 (45%) agreed to participate following consenting. 486 eligible participants (about 8% of all attendees in the 2 month period) refused to participate citing the following: time pressure (n = 299, 62%); fear of research (n = 82, 17%); no mental illness (n = 66, 14%), other concerns (urgent medical condition and suspicion of study, (n = 34, 7%)). Males refusals were slightly more at 52%
Table 2 presents sample characteristics for the 77 (20%) participants who experienced suicidal ideation in the past month and the 317 participants who did not. The majority of participants in both groups were under the age of 40 years, female, married, had completed primary education and were Christian with no individual monthly income (versus household income). Higher proportions that reported suicidal ideation over the past month were widowed and had little formal education compared their counterparts.
Table 2.
Sample Characteristics by Suicidal Ideation (SI) in the past month (n = 394).
| No SI (317) | SI (77) | Total (394) | ||
|---|---|---|---|---|
| Group | Characteristics | n (%) | n (%) | n (%) |
| Age in years | ||||
| 18–25 | 77 (24) | 22 (29) | 99 (25) | |
| 26–39 | 95 (30) | 21 (27) | 116 (29) | |
| 40–59 | 102 (32) | 19 (25) | 121 (31) | |
| ≥ 60 | 42 (13) | 15 (19) | 57 (14) | |
| Gender | ||||
| Female | 162 (51) | 48 (62) | 210 (53) | |
| Male | 155 (49) | 29 (38) | 184 (47) | |
| Marital Status | ||||
| Married/Cohabiting | 178 (56) | 33 (43) | 211 (54) | |
| Divorced/Separated | 19 (6) | 9 (12) | 28 (7) | |
| Single | 82 (26) | 14 (18) | 96 (24) | |
| Widowed*** | 38 (12) | 21 (27) | 59 (15) | |
| Highest level of education | ||||
| No formal | 75 (24) | 28 (36) | 103 (26) | |
| education* | ||||
| Primary (10 years) | 140 (44) | 33 (43) | 173 (44) | |
| Secondary (14 years) | 77 (24) | 12 (16) | 89 (23) | |
| Tertiary(> 14 years) | 25 (8) | 4 (5) | 29 (7) | |
| Religion | ||||
| Christianity | 175 (55) | 40 (52) | 215 (55) | |
| Islam | 119 (38) | 29 (38) | 148 (37) | |
| Traditional Religion | 20 (6) | 8 (10) | 28 (7) | |
| Others | 3 (1) | 0 (0) | 3 (1) | |
| Occupation | ||||
| Note: some | Not Employed | 121 (38) | 23 (30) | 144 (32) |
| participants | outside the home | |||
| work in | Salaried/Waged | 115 (36) | 32 (42) | 147 (33) |
| multiple | Farm Work | 56 (18) | 18 (23) | 74 (17) |
| occupations. | Self Employed | 70 (22) | 12 (16) | 82 (18) |
| Monthly income (individual) | ||||
| Not Indicated/Not | 149 (47) | 37 (48) | 186 (47) | |
| Employed | ||||
| USD. 1–50 | 33 (10) | 17 (22) | 50 (13) | |
| USD. 50.01–100 | 48 (15) | 10 (13) | 58 (15) | |
| USD. 100.01–250 | 52 (16) | 8 (10) | 60 (15) | |
| USD. 250.01–400 | 12 (4) | 3 (4) | 15 (4) | |
| USD 400.01 and | 21 (7) | 2 (3) | 23 (6) | |
| above | ||||
Significantly greater among those with SI in the past month:
p < .05;
p < .01;
p < .001.
Mental disorders were common: approximately 19% of participants met criteria for major depressive disorder (MDD); 30–50% met criteria for posttraumatic stress disorder (PTSD) and 20–30% met criteria for both. Prevalence of PTSD and MDD-PTSD comorbidity were both significantly higher among women than men. Alcohol dependence (8% women, 33% men) was much higher among men. Intimate partner violence (IPV) over the past week, both experience of abuse and perpetration of abuse, were high: 34% of women reported experiencing IPV in the past week and 37% reported perpetration, while 41% of men reported experiencing IPV and 38% reported perpetration. Lifetime physical abuse and sexual abuse were higher among women (20% and 23%, respectively), compared with men (16% and 18%, respectively), though not significantly different (Table 3).
Table 3.
Common Mental Disorders, Trauma Exposures and Suicidality by gender (Female = 211, Male = 185, Total = 394).
| Group | Disorder/Event | Female n (%) | Male n (%) | Overall n (%) | |
|---|---|---|---|---|---|
| Suicidality | |||||
| Past month | Suicidal ideation | 48 (23%) | 29 (16%) | 77 (20%) | |
| Plan for suicide | 23 (11%) | 15 (8%) | 38 (10%) | ||
| Suicide attempt | 8 (4%) | 6 (3%) | 14 (4%) | ||
| Suicide attempt without ideation or plan | 0 | 0 | 0 | ||
| Lifetime | Suicide Attempt | 40 (19%) | 27 (15%) | 67 (17%) | |
| Common mental disorders | |||||
| MDD (no PTSD) | 33 (16%) | 41 (22%) | 74 (19%) | ||
| PTSD (no MDD)** | 29 (27%) | 21 (19%) | 50 (13%) | ||
| MDD-PTSD (co-morbid)* | 52 (33%) | 34 (23%) | 86 (22%) | ||
| Alcohol dependence*** | 16 (8%) | 60 (33%) | 76 (19%) | ||
| Intimate partner violence in the past week | |||||
| Experienced | 56 (34%) | 54 (41%) | 110 (28%) | ||
| Perpetrated | 60 (37%) | 51 (38%) | 111 (28%) | ||
| Lifetime abuse | |||||
| Physical abuse | 42 (20%) | 29 (16%) | 71 (18%) | ||
| Sexual abuse | 48 (23%) | 34 (18%) | 82 (21%) | ||
Significantly greater for females versus males:
p < .05;
p <.01;
p<.001;
MDD = Major Depressive Disorder; PTSD = Posttraumatic Stress Disorder.
Across genders, 18% of those with suicidal ideation over the past month also attempted suicide in the past month (17% of women and 21% of men).
3.1. Risk factors for suicidal ideation over the past month
In logistic regression, those with MDD (suicidality item removed) were approximately 19 times more likely to report suicidal ideation over the past month, compared to their counterparts without MDD (Table 4). Of note, there was a large confidence interval for MDD odds ratios, reflective of the small number of people who had suicidal ideation over the past month and did not meet criteria for current MDD (1 female and 1 male). However, the lower margin of the OR confidence interval was nearly 5, still higher than the OR of any other variable.
Table 4.
Bivariate logistic regression of Suicidal Ideation (SI) over the past month (n = 394).
| Variable | Female OR (95% CI) | p value | Male OR (95% CI) | p value | Overall OR (95% CI) | p value | |
|---|---|---|---|---|---|---|---|
| Demographics | |||||||
| Age | 1.00 [0.99, 1.02] | 0.75 | 1.02 [0.99, 1.04] | 0.16 | 1.01 [0.99, 1.02] | 0.25 | |
| Educationa | 0.57 [0.30, 1.11] | 0.10 | 0.60 [0.23, 1.57] | 0.30 | 0.54 [.32, .92] | 0.02 | |
| Marital Status | |||||||
| Cohabiting | 0.67 [0.08, 5.86] | 0.72 | See footnoteb | 0.40 [0.05, 3.20] | 0.39 | ||
| Divorced/Separated | 1.77 [0.57, 5.45] | 0.32 | 2.60 [0.74, 9.08] | 0.14 | 2.08 [0.90, 4.79] | 0.09 | |
| Married | 0.63 [0.33, 1.20] | 0.16 | 0.56 [0.25, 1.28] | 0.17 | 0.63 [0.38, 1.04] | 0.07 | |
| Single | 0.45 [0.17, 1.24] | 0.12 | 0.97 [0.41, 2.29] | 0.95 | 0.64 [0.34, 1.20] | 0.16 | |
| Widowed | 3.02 [1.42, 6.55] | 0.00 | 2.12 [0.76, 5.93] | 0.15 | 2.75 [1.50, 5.04] | 0.00 | |
| Employment & Income | |||||||
| Employmentc | 1.25 [0.80, 1.95] | 0.34 | 0.91 [0.50, 1.66] | 0.76 | 1.10 [0.77, 1.57] | 0.61 | |
| Incomec | 1.00 [1.00, 1.00] | 0.72 | 1.00 [1.00, 1.00] | 0.06 | 1.00 [1.00, 1.00] | 0.09 | |
| Mental Disorders and Suicide Attempts | |||||||
| MDD (SI removed), no PTSD | 24.26 [3.25,181.25] | 0.00 | 13.79 [1.82,104.56] | 0.01 | 18.99 [4.56, 79.05] | 0.00 | |
| PTSD, no MDD | 1.93 [0.91, 4.09] | 0.09 | 2.13 [0.87, 5.23] | 0.10 | 2.13 [1.20, 3.77] | 0.01 | |
| PTSD-MDD (SI removed) comorbidity | 3.58 [1.69, 7.58] | 0.00 | 3.08 [1.24, 7.65] | 0.02 | 3.51 [1.97, 6.23] | 0.00 | |
| Alcohol dependence over the past year | 0.76 [0.21, 2.79] | 0.68 | 0.81 [0.33, 1.96] | 0.64 | 0.67 [0.33, 1.34] | 0.25 | |
| Suicide attempt over the past month | See footnoted | See footnoted | See footnoted | ||||
| History of suicide attempt (lifetime) | 3.79 [1.81, 7.92] | 0.00 | 5.31 [2.13, 13.21] | 0.00 | 4.42 [2.49, 7.83] | 0.00 | |
| Intimate Partner Violence (IPV) | |||||||
| Experienced IPV over the past week | 3.15 [1.40, 7.11] | 0.01 | 1.01 [0.36, 2.85] | 0.98 | 1.97 [1.05, 3.69] | 0.04 | |
| Perpetrated IPV in the past week | 2.29 [1.02, 5.10] | 0.04 | 1.49 [0.52, 4.15] | 0.45 | 1.92 [1.02, 3.60] | 0.04 | |
| Lifetime abuse | |||||||
| Physical abuse | 1.30 [0.59, 2.84] | 0.51 | 1.92 [0.73, 5.04] | 0.18 | 1.55 [0.85, 2.84] | 0.16 | |
| Sexual abuse | 1.40 [0.67, 2.93] | 0.38 | 1.51 [0.59, 3.89] | 0.40 | 1.47 [0.82, 2.63] | 0.19 | |
| Quality of Life | |||||||
| Overall | 0.79 [0.67, 0.93] | 0.01 | 0.85 [0.70, 1.02] | 0.08 | 0.81 [0.72, 0.92] | 0.00 | |
| Psychological health | 0.83 [0.72, 0.95] | 0.01 | 0.92 [0.80, 1.06] | 0.24 | 0.87 [0.79, 0.96] | 0.01 | |
| Social relationships | 0.93[0.86, 1.01] | 0.10 | 0.88[0.78, 0.99] | 0.04 | 0.92 [0.86, 0.98] | 0.01 | |
| Environmente | 0.95 [0.87, 1.04] | 0.29 | 0.92 [0.82, 1.03] | 0.15 | 0.94 [0.88, 1.01] | 0.08 | |
| Physical health (overall) | 0.91 [0.85, 0.99] | 0.02 | 0.89 [0.81, 0.97] | 0.01 | 0.90 [0.85, 0.95] | 0.00 | |
| Painf | 0.80 [0.64, 0.99] | 0.04 | 0.61 [0.45, 0.81] | 0.00 | 0.72 [0.60, 0.86] | 0.00 | |
| Satisfaction with performance of daily activities | 0.60 [0.38, 0.94] | 0.03 | 0.61 [0.45, 0.81] | 0.00 | 0.59 [0.42, 0.82] | 0.00 | |
| Sleep | 0.65 [0.42, 0.99] | 0.04 | 0.45 [0.25, 0.79] | 0.01 | 0.55 [0.39, 0/77] | 0.00 | |
| Need for medical treatment to perform daily activities | 0.83 [0.65, 1.06] | 0.14 | 0.67 [0.50, 0.90] | 0.01 | 0.76 [0.63, 0.92] | 0.00 | |
Bold print indicates p < .05.
Education: 0 (none); 1 (primary); 2 (secondary); 3 (tertiary).
No men who were cohabitating had suicidality over the past month.
Salaried work, farming, self-employed business.
All of those who had a suicide attempt in the last month also had suicidal ideation in the last month.
Financial resources, freedom, safety, security, accessibility and quality of health and social care, home environment, opportunities, recreation, transport and physical environment (pollution, noise, traffic, climate).
Increasing daily interference from pain correlates with decreasing number. MDD = Major Depressive Disorder; PTSD = Posttraumatic Stress Disorder, PTSD-MDD = co-morbid PTSD-MDD (SI item removed).
Participants who reported a history of suicide attempt were more than 4 times as likely to report suicidal ideation over the past month, compared to those without a history of attempt. Participants who met criteria for both MDD and PTSD (suicidality item removed) were three times more likely to report suicidal ideation compared to those without MDD-PTSD comorbidity. Decreased quality of life related physical health and multiple sub-domains were associated with higher likelihood of reporting suicidal ideation for both men and women. For women, widowhood, experiencing or perpetrating IPV, quality of psychological health and overall quality of life were also significantly related to suicidal ideation. For men, quality of social relationships and ability to perform daily activities without medical treatment were associated with suicidal ideation.
Participants who met criteria for major depressive disorder (suicidality item removed) were 19 times more likely to report suicidal ideation compared to those without MDD (Table 1).
Participants with suicidal ideation over the past month were more than four times as likely to report lifetime suicidal attempt compared to those without recent suicidal ideation (Table 1).
We identified those variables that were significantly associated with suicidal ideation in separate analyses of men and women (MDD, PTSD-MDD, lifetime suicide attempt, and quality of life measures relating to: overall physical health, pain, performance of daily activities and sleep) and constructed a multi-variate regression (see data analysis for details). Results are presented in diagram format with adjusted odds ratios (Fig. 1). Given the cross-sectional nature of these data, and studies showing bi-directional relationships between model variables (e.g., depression and pain(K M Scott et al., 2007; Walker et al., 2014)), we intentionally constructed the diagram without directional arrows.
Fig. 1.
Adjusted ODDS Ratios [95% CI], p value (n = 310).
3.2. Suicidal ideation in the past month: adjusted odds ratios
In an adjusted model, suicidal ideation was significantly associated with MDD (suicidal ideation item removed) with an odds ratio of 12.15 (p = 0.001), meaning that those with MDD were 12 times as likely as those without MDD to report suicidal ideation over the past month, after adjusting for all other variables in the model (Fig. 1). Satisfaction with sleep and ability to perform daily activities were both inversely associated with suicidal ideation –as satisfaction declined, risk of suicidal ideation increased (p = 0.01 and 0.04, respectively). Lifetime history of suicidal ideation was associated with report of suicidal ideation over the past month—those with a history of suicide attempt were nearly 3 times as likely as those without a history to report suicidal ideation (p = 0.003). We assessed the relationship between MDD and other variables in the model and found that lifetime suicidal attempt and physical pain were indirectly related to suicidal ideation via MDD (non-significant associations with MDD excluded for figure clarity).
4. Discussion
4.1. Response rate
This study's response rate was 45%, meaning that approximately half of the participants who provided consent and met eligibility criteria agreed to participate in the study. This response rate is consistent with the rates observed in face-to-face surveys of waiting room attendees in HICs (Beckwith et al., 2016; Michael et al., 2013; Slater and Kiran, 2016). The majority of those who refused to participate cited time constraints, which is unlikely to bias the study results. It is notable that some declined participation because they denied having a mental illness (14%). It is possible that if healthy individuals opted out of the study, the study participants would over-represent mental disorders in this general medical outpatient population. On the other hand, in this region of eastern Africa, the term mental disorder is most often equated with a severe psychosis or intellectual disability, requiring lifelong institutionalization and bringing great burden to the family. Refusal to participate in the study may also represent cultural stigma and/or fear regarding mental disorders.
4.2. Prevalence suicidal ideation, mental disorders and gender correlates
Participants in this study had a high prevalence of suicidal ideation (20%) in the past month. Studies of general medical populations in and around Nairobi, Kenya, which found prevalence of suicidal ideation at 10–12% (Ndetei et al., 2010; Aillon et al., 2014). Discrepancies between our findings and those from Kenya's capital, Nairobi, may reflect the relatively higher rates of trauma reported in this rural Kenyan population, ranging from poverty, to the loss of family members (poor healthcare access) and higher rates of domestic violence. This study also found a high prevalence of lifetime suicide attempt among general medical outpatient clinic attendees: 19% (female) 15% (male), a figure that is nearly 9 times higher than general populations in Kenya (Jenkins et al., 2015; Nock et al., 2008).
We also found a high prevalence of depression and PTSD. Approximately 1/3 of study participants met criteria for MDD or PTSD and near 1/4 met criteria for both. Consistent with other studies on gender and mental disorders, our study found higher rates of mood and anxiety disorder among women compared to men and higher rates of alcohol dependence among men compared to women (Seedat et al., 2009; Wilsnack et al., 2009).
4.3. Bivariate and adjusted models of suicidal ideation
We found that participants with MDD (suicidality item removed) were 19 times more likely to report suicidal ideation in the past month compared to those without MDD. MDD remained a significant predictor of suicidal ideation in the adjusted model across both females and males, increasing the likelihood of suicidal ideation by more than 12. Given that many evidence-based treatments for MDD can now be delivered by non-specialists in LMICs (Bass et al., 2013; Bolton et al., 2003; Chibanda et al., 2016; Meffert et al., 2016; van Gínneken et al., 2013), this finding has significant clinical import and may be a key strategy for reducing suicidal ideation and associated attempts.
Consistent with prior research, in binary analyses, we found that lower education, widowhood,(Luoma and Pearson, 2002; Smith et al., 1988; Lloyd-Sherlock et al., 2015; Sasson and Umberson, 2014) MDD, PTSD and co-morbid MDD-PTSD, IPV and quality of life measures (including physical pain) were significantly associated with suicidal ideation (Fishbain et al., 2014; Han et al., 2015; LeBouthillier et al., 2015; Oquendo et al., 2005; Scocco et al., 2008). Also consistent with recent work in Africa, we did not find an association between suicidal ideation and employment or income (Lund et al., 2010). Unlike prior studies, we did not find suicidal ideation to be associated with alcohol dependence for men.
We found evidence that suicidal ideation in the study population was more associated with past month suicide attempt than in other settings, making identification of suicidal ideation both high yield and urgent for clinicians (18% of those with suicidal ideation attempted suicide in the past month). Suicidal ideation in the past month was associated with an approximately 4-fold increase of lifetime suicide attempt (Fig. 1). While the association between suicidal ideation and past suicide attempt is well-established, the magnitude of the correlation found in our study is substantial. Given the high prevalence of suicidal ideation in this population and the relationship between suicidal ideation and suicide attempt, we estimate that 36% of those with suicidal ideation over the past month have attempted to harm themselves in their lifetime—a figure of both statistical and clinical significance.
Major depressive disorder is a major risk factor for suicidal ideation (adjusted OR = 12).
Suicidal ideation is major risk factor for suicide attempt (36% attempt suicide) in rural Kenyan.
4.4. Suicidal ideation, sleep and satisfaction with ability to perform daily activities
In our adjusted model, we found significant links between decreased sleep quality and suicidal ideation. This finding supports and builds on emerging studies showing a link between sleep quality and suicidality, including those from sub-Saharan Africa (Chu et al., 2017; Gelaye et al., 2015, 2016). As posited by studies investigating the relationship between poor sleep and suicidality, insomnia is thought to exacerbate a thwarted sense of belonging because the affected individual is awake while others are sleeping and may be less motivated to make social connections during the daytime (Chu et al., 2017).
We also found independent associations between suicidal ideation and satisfaction with ability to perform daily activities. According to the interpersonal theory of suicide, limited ability to give back to others and perceived burdensomeness is a risk factor for suicide. Capability to commit suicide is thought to be facilitated by exposure to painful and disinhibiting experiences, such as prior suicide attempt. In our adjusted model, the independent link between prior suicide attempt and suicidal ideation fit well with the interpersonal theory of suicide.
4.5. Suicidal ideation and suicide attempt among general medical outpatients
The relationship between suicidal ideation and suicide attempt is supported by the interpersonal theory of suicide (Van Orden et al., 2008) which posits that the combination of “thwarted [social] belongingness and perceived [social] burdensomeness” with “painful and provocative experiences and acquired capability for suicide” foster suicidal ideation and its transition to suicide attempt. Kenya is known for the high value that it places on social connections with respect to living arrangements, recreation, religion and financial support of community members (Behrman et al., 2002) It is possible that individuals living in a community which prioritizes social belonging would be particularly sensitive to factors which threatened it (such as medical conditions), perhaps explaining high rates of suicidal ideation in this general medical clinic population.
5. Limitations
This was a cross sectional study design with convenience sampling and hence vulnerable to selection and recall bias. As discussed above, some individuals who refused to participate claimed that they had no mental disorder (14% of refusals). Therefore, it is possible that the study results reflect some degree inflated prevalence of suicidal ideation and mental disorders relative to the true prevalence among general medical outpatients in this setting. However, mental health literacy is low in this region and mental disorders are often understood as severely disabling psychoses or intellectual disabilities, rather than suicidal ideation, depression and PTSD. The latter would suggest that individuals who opted out of the study did not bias results with respect to suicidality, affective and anxiety prevalence. Lastly, Mariakani Sub County Hospital being a tier 3 secondary referral hospital, serves both a mix of referrals from other healthcare facilities, walk in patients from the local area and emergency/urgent cases. Hence, our study population may not be an exclusively “normal" primary care population in keeping with EuroAmerican norms. However, this mix of patients is quite typical for Kenyan Sub-County hospitals and the results of this study are likely to be nationally applicable.
6. Conclusions
This study highlights suicidal ideation and presence of major depressive disorders as potential risk factors for suicidal attempts in a general medical outpatient care setting. Future studies would benefit from in-depth qualitative work to understand the experience and expressions of suicidal ideation and depression in this setting. This study also adds urgency to the effort to close the mental health treatment gap in LMICs, particularly as it pertains to depression and associated risk of suicide attempt in East Africa. Task-shifting strategies which deploy non-specialists to deliver evidence-based depression treatments have strong efficacy and emerging effectiveness data in the region, and these treatment efforts should advance to implementation research and scale up (Bass et al., 2006, 2011, 2013; Bolton et al., 2007; Onu et al., 2016; Verdeli et al., 2008).
Acknowledgments
Role of funding source
This work was supported by UCSF-GloCal Health Research Fellowship through a Fogarty Grant. The funders played no role in the writing process and did not influence the decision to publish. This project was supported by NIH Research Training Grant # R25 TW009343 funded by the Fogarty International Center and the National Institute of Mental Health, as well as the University of California Global Health Institute (UCGHI). The content is solely the responsibility of the authors and does not necessarily represent the oficial views of the NIH or UCGHI.
This work harnessed resources of the Integrated Primary Health Care (IPHC) program. Our thanks goes to the study participants, the Kilifi County and Mariakani Sub County Hospital administration for the study facilitation. Many thanks to Mr. Felix Agoi for coordinating the study.
Footnotes
- Linnet Ongeri – contributed to the design, acquisition and interpretation of data, as well as manuscript drafting.
- Charles McCulloch-contributed to the analysis, interpretation of data as well as manuscript drafting.
- Thomas Neylan-contributed to the design and interpretation of data, as well as manuscript drafting.
- Elizabeth Bukusi-contributed to the design, acquisition and interpretation of data, as well as manuscript drafting.
- Sarah Macfarlane-contributed to the design, interpretation of data as well as manuscript drafting.
- Caleb Othieno-contributed to the design and manuscript drafting. 7. Anthony Ngugi-contributed to the design, acquisition and interpretation of data, as well as manuscript drafting.8. Susan Meffert-contributed to the design, acquisition, analysis and interpretation of data as well as manuscript drafting.
They all give consent to the publication of this manuscript.
Conflict of interest statement
No conflict of Interest to declare.
References
- Aillon J-L, Ndetei DM, Khasakhala L, Ngari WN, Achola HO, Akinyi S, Ribero S. Prevalence, types and comorbidity of mental disorders in a Kenyan primary health centre. Soc Psychiatry Psychiatr Epidemiol. 2013 doi: 10.1007/s00127-013-0755-2. http://dx.doi.org/10.1007/s00127-013-0755-2. [DOI] [PubMed]
- Aillon JL, Ndetei DM, Khasakhala L, Ngari WN, Achola HO, Akinyi S, Ribero S. Prevalence, types and comorbidity of mental disorders in a Kenyan primary health centre. Soc Psychiatry Psychiatr Epidemiol. 2014;49(8):1257–1268. doi: 10.1007/s00127-013-0755-2. http://dx.doi.org/10.1007/s00127-013-0755-2. [DOI] [PubMed] [Google Scholar]
- Ani C, Bazargan M, Hindman D, Bell D, Farooq MA, Akhanjee L, Rodriguez M. Depression symptomatology and diagnosis: discordance between patients and physicians in primary care settings. BMC Fam Pract. 2008;9:1. doi: 10.1186/1471-2296-9-1. http://dx.doi.org/10.1186/1471-2296-9-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bass J, Neugebauer R, Clougherty KF, Verdeli H, Wickramaratne P, Ndogoni L, Bolton P. Group interpersonal psychotherapy for depression in rural Uganda: 6-month outcomes: randomised controlled trial. Br J Psychiatry: J Ment Sci. 2006;188:567–573. doi: 10.1192/bjp.188.6.567. http://dx.doi.org/10.1192/bjp.188.6.567. [DOI] [PubMed] [Google Scholar]
- Bass J, Poudyal B, Tol W, Murray L, Nadison M, Bolton P. A controlled trial of problem-solving counseling for war-affected adults in Aceh, Indonesia. Social Psychiatry Psychiatr Epidemiol. 2011 doi: 10.1007/s00127-011-0339-y. http://dx.doi.org/10.1007/s00127-011-0339-y. [DOI] [PubMed]
- Bass JK, Annan J, McIvor Murray S, Kaysen D, Grifiths S, Cetinoglu T, Bolton PA. Controlled trial of psychotherapy for Congolese survivors of sexual violence. New Engl J Med. 2013;368(23):2182–2191. doi: 10.1056/NEJMoa1211853. http://dx.doi.org/10.1056/NEJMoa1211853. [DOI] [PubMed] [Google Scholar]
- Beckwith N, Jean-Baptiste ML, Katz A. Waiting room education in a community health system: provider perceptions and suggestions. J Community Health. 2016;41(6):1196–1203. doi: 10.1007/s10900-016-0201-y. http://dx.doi.org/10.1007/s10900-016-0201-y. [DOI] [PubMed] [Google Scholar]
- Behrman JR, Kohler HP, Watkins SC. Social networks and changes in contraceptive use over time: evidence from a longitudinal study in rural Kenya. Demography. 2002;39(4):713–738. doi: 10.1353/dem.2002.0033. (Retrieved from). < http://www.ncbi.nlm.nih.gov/pubmed/12471851>. [DOI] [PubMed] [Google Scholar]
- Berghöfer A, Roll S, Bauer M, Willich SN, Pfennig A. Screening for depression and high utilization of health care resources among patients in primary care. Community Ment Health J. 2014;50(7):753–758. doi: 10.1007/s10597-014-9700-4. http://dx.doi.org/10.1007/s10597-014-9700-4. [DOI] [PubMed] [Google Scholar]
- Bolton P, Bass J, Neugebauer R, Verdeli H, Clougherty KF, Wickramaratne P, Weissman M. Group interpersonal psychotherapy for depression in rural Uganda: a randomized controlled trial. JAMA. 2003;289(23):3117–3124. doi: 10.1001/jama.289.23.3117. http://dx.doi.org/10.1001/jama.289.23.3117. [DOI] [PubMed] [Google Scholar]
- Bolton P, Bass J, Betancourt T, Speelman L, Onyango G, Clougherty KF, Verdeli H. Interventions for depression symptoms among adolescent survivors of war and displacement in northern Uganda: a randomized controlled trial. JAMA: J Am Med Assoc. 2007;298(5):519–527. doi: 10.1001/jama.298.5.519. http://dx.doi.org/10.1001/jama.298.5.519. [DOI] [PubMed] [Google Scholar]
- Chibanda D, Weiss HA, Verhey R, Simms V, Munjoma R, Rusakaniko S, Araya R. Effect of a Primary care-based psychological intervention on symptoms of common mental disorders in zimbabwe: a randomized clinical trial. JAMA. 2016;316(24):2618–2626. doi: 10.1001/jama.2016.19102. http://dx.doi.org/10.1001/jama.2016.19102. [DOI] [PubMed] [Google Scholar]
- Chu C, Hom MA, Rogers ML, Stanley IH, Ringer-Moberg FB, Podlogar MC, Joiner TE. Insomnia and suicide-related behaviors: a multi-study investigation of thwarted belongingness as a distinct explanatory factor. J Affect Disord. 2017;208:153–162. doi: 10.1016/j.jad.2016.08.065. http://dx.doi.org/10.1016/j.jad.2016.08.065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fekadu A, Medhin G, Selamu M, Shiferaw T, Hailemariam M, Rathod SD, Hanlon C. Non-fatal suicidal behaviour in rural Ethiopia: a cross-sectional facility- and population-based study. BMC Psychiatry. 2016;16:75. doi: 10.1186/s12888-016-0784-y. http://dx.doi.org/10.1186/s12888-016-0784-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fishbain DA, Lewis JE, Gao J. The pain suicidality association: a narrative review. Pain Med. 2014;15(11):1835–1849. doi: 10.1111/pme.12463. http://dx.doi.org/10.1111/pme.12463. [DOI] [PubMed] [Google Scholar]
- Gelaye B, Barrios YV, Zhong QY, Rondon MB, Borba CPC, Sánchez SE, Williams MA. Association of poor subjective sleep quality with suicidal ideation among pregnant Peruvian women. General Hosp Psychiatry. 2015;37(5):441–447. doi: 10.1016/j.genhosppsych.2015.04.014. http://dx.doi.org/10.1016/j.genhosppsych.2015.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gelaye B, Okeiga J, Ayantoye I, Berhane HY, Berhane Y, Williams MA. Association of suicidal ideation with poor sleep quality among Ethiopian adults. Sleep Breath = Schlaf Atm. 2016;20(4):1319–1326. doi: 10.1007/s11325-016-1418-9. http://dx.doi.org/10.1007/s11325-016-1418-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han B, Compton WM, Gfroerer J, McKeon R. Prevalence and correlates of past 12-month suicide attempt among adults with past-year suicidal ideation in the United States. J Clin Psychiatry. 2015;76(3):295–302. doi: 10.4088/JCP.14m09287. http://dx.doi.org/10.4088/JCP.14m09287. [DOI] [PubMed] [Google Scholar]
- Have M, de Graaf R, van Dorsselaer S, Verdurmen J, van’t Land H, Vollebergh W, Beekman A. Incidence and course of suicidal ideation and suicide attempts in the general population. Can J Psychiatry Rev Can De Psychiatr. 2009;54(12):824–833. doi: 10.1177/070674370905401205. [DOI] [PubMed] [Google Scholar]
- Hooper LM, Stockton P, Krupnick JL, Green BL. Development, use, and psychometric properties of the trauma history questionnaire because early research often focused on specific populations with their own specific trauma measures (e.g., Vietnam War veterans) 1993 < https://doi.org/10.1080/15325024.2011.572035>.
- Hospital, M.S.C. Kaloleni District Health Information System. 2015. [Google Scholar]
- Jenkins R, Othieno C, Omollo R, Ongeri L, Sifuna P, Ongecha M, Ogutu B. Tedium vitae, death wishes, suicidal ideation and attempts in Kenya-prevalence and risk factors. BMC Public Health. 2015;15:759. doi: 10.1186/s12889-015-2089-3. http://dx.doi.org/10.1186/s12889-015-2089-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joe S, Stein DJ, Seedat S, Herman A, Williams DR. Non-fatal suicidal behavior among South Africans. Soc Psychiatry Psychiatr Epidemiol. 2008;43(6):454–461. doi: 10.1007/s00127-008-0348-7. http://dx.doi.org/10.1007/s00127-008-0348-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kenya KCG. Kilifi County First County Integrated Development Plan 2013–2017. 2013 Retrieved from < https://cog.go.ke/images/stories/CIDPs/KIlifi.pdf>.
- Kenya Healthcare Federation. Kenya Healthcare Sector Report. 2016 Retrieved from < https://www.rvo.nl/sites/default/files/2016/10/2016_Kenyan_Healthcare_Sector_Report_Compleet.pdf>.
- Kenya Inter Agency Rapid Assessment (KIRA) Kilifi Secondary Data Review as at February 2014. 2014 Retrieved from < https://www.humanitarianresponse.info/system/files/documents/files/KilifiSecondaryDataReview_20141112.pdf>.
- Kenya National Bureau of Statistics. Basic Report on Well-Being in Kenya. 2005 Retrieved from < https://www.file:///C:/Users/Linnet/Downloads/ReportonwellbeinginKenya.pdf>.
- Klonsky ED, May AM, Saffer BY. Suicide, Suicide Attempts, and Suicidal Ideation. Annu Rev Clin Psychol. 2016;12:307–330. doi: 10.1146/annurev-clinpsy-021815-093204. http://dx.doi.org/10.1146/annurev-clinpsy-021815-093204. [DOI] [PubMed] [Google Scholar]
- LeBouthillier DM, McMillan KA, Thibodeau MA, Asmundson GJG. Types and number of traumas associated with suicidal ideation and suicide attempts in PTSD: findings From a U.S. nationally representative sample. J Trauma Stress. 2015;28(3):183–190. doi: 10.1002/jts.22010. http://dx.doi.org/10.1002/jts.22010. [DOI] [PubMed] [Google Scholar]
- Lloyd-Sherlock P, Corso B, Minicuci N. Widowhood, socio-economic status, health and wellbeing in low and middle-income countries. J Dev Stud. 2015;51(10):1374–1388. doi: 10.1080/00220388.2015.1066497. http://dx.doi.org/10.1080/00220388.2015.1066497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lund C, Breen A, Flisher AJ, Kakuma R, Corrigall J, Joska JA, Patel V. Poverty and common mental disorders in low and middle income countries: a systematic review. Social Sci Med (1982) 2010;71(3):517–528. doi: 10.1016/j.socscimed.2010.04.027. http://dx.doi.org/10.1016/j.socscimed.2010.04.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luoma JB, Pearson JL. Suicide and marital status in the United States, 1991–1996: is widowhood a risk factor? Am J Public Health. 2002;92(9):1518–1522. doi: 10.2105/ajph.92.9.1518. (Retrieved from). < http://www.ncbi.nlm.nih.gov/pubmed/12197986>. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luoma JB, Martin CE, Pearson JL. Contact with mental health and primary care providers before suicide: a review of the evidence. Am J Psychiatry. 2002;159(6):909–916. doi: 10.1176/appi.ajp.159.6.909. http://dx.doi.org/10.1176/appi.ajp.159.6.909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meffert SM, Neylan TC, Chambers DA, Verdeli H. Novel implementation research designs for scaling up global mental health care: overcoming translational challenges to address the world's leading cause of disability. Int J Ment Health Syst. 2016;10:19. doi: 10.1186/s13033-016-0049-7. http://dx.doi.org/10.1186/s13033-016-0049-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michael M, Schaffer SD, Egan PL, Little BB, Pritchard PS. Improving wait times and patient satisfaction in primary care. J Healthc Qual. 2013;35(2):50–60. doi: 10.1111/jhq.12004. http://dx.doi.org/10.1111/jhq.12004. [DOI] [PubMed] [Google Scholar]
- Ministry of Health. Kenya Health Policy 2014–2030: Towards attaining th e highest standards of health. 2012 Retrieved from < https://www.healthresearchweb.org/files/KenyaHealthpolicyfinalversion.pdf>.
- Ndetei DM, Khasakhala LI, Mutiso V, Mbwayo AW. Suicidality and depression among adult patients admitted in general medical facilities in Kenya. Ann General Psychiatry. 2010;9(1):7. doi: 10.1186/1744-859X-9-7. http://dx.doi.org/10.1186/1744-859X-9-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nock MK, Borges G, Bromet EJ, Alonso J, Angermeyer M, Beautrais A, Williams D. Cross-national prevalence and risk factors for suicidal ideation, plans and attempts. Br J Psychiatry: J Ment Sci. 2008;192(2):98–105. doi: 10.1192/bjp.bp.107.040113. http://dx.doi.org/10.1192/bjp.bp.107.040113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Onu C, Ongeri L, Bukusi E, Cohen CR, Neylan TC, Oyaro P, Meffert SM. Interpersonal psychotherapy for depression and posttraumatic stress disorder among HIV-positive women in Kisumu, Kenya: study protocol for a randomized controlled trial. Trials. 2016;17(1):64. doi: 10.1186/s13063-016-1187-6. http://dx.doi.org/10.1186/s13063-016-1187-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oquendo M, Brent DA, Birmaher B, Greenhill L, Kolko D, Stanley B, Mann JJ. Posttraumatic stress disorder comorbid with major depression: factors mediating the association with suicidal behavior. Am J Psychiatry. 2005;162(3):560–566. doi: 10.1176/appi.ajp.162.3.560. http://dx.doi.org/10.1176/appi.ajp.162.3.560. [DOI] [PubMed] [Google Scholar]
- Sasson I, Umberson DJ. Widowhood and depression: new light on Gender differences, selection, and psychological adjustment. J Gerontol Ser B: Psychol Sci Social Sci. 2014;69B(1):135–145. doi: 10.1093/geronb/gbt058. http://dx.doi.org/10.1093/geronb/gbt058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scocco P, de Girolamo G, Vilagut G, Alonso J. Prevalence of suicide ideation, plans, and attempts and related risk factors in Italy: results from the European Study on the Epidemiology of Mental Disorders–World Mental Health study. Compr Psychiatry. 2008;49(1):13–21. doi: 10.1016/j.comppsych.2007.08.004. http://dx.doi.org/10.1016/j.comppsych.2007.08.004. [DOI] [PubMed] [Google Scholar]
- Scott KM, Bruffaerts R, Tsang A, Ormel J, Alonso J, Angermeyer MC, Von Korff M. Depression-anxiety relationships with chronic physical conditions: results from the World Mental Health Surveys. J Affect Disord. 2007;103(1–3):113–120. doi: 10.1016/j.jad.2007.01.015. http://dx.doi.org/10.1016/j.jad.2007.01.015. [DOI] [PubMed] [Google Scholar]
- Scott KM, Hwang I, Chiu WT, Kessler RC, Sampson NA, Angermeyer M, Nock MK. Chronic physical conditions and their association with first onset of suicidal behavior in the world mental health surveys. Psychosom Med. 2010;72(7):712–719. doi: 10.1097/PSY.0b013e3181e3333d. http://dx.doi.org/10.1097/PSY.0b013e3181e3333d. [DOI] [PubMed] [Google Scholar]
- Seedat S, Scott KM, Angermeyer MC, Berglund P, Bromet EJ, Brugha TS, Kessler RC. Cross-national associations between gender and mental disorders in the World Health Organization World Mental Health Surveys. Arch General Psychiatry. 2009;66(7):785–795. doi: 10.1001/archgenpsychiatry.2009.36. http://dx.doi.org/10.1001/archgenpsychiatry.2009.36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, Dunbar GC. The Mini-International neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59(Suppl 2) (22-33-57. Retrieved from). < http://www.ncbi.nlm.nih.gov/pubmed/9881538>. [PubMed] [Google Scholar]
- Skevington SM, Lotfy M, O’connell KA. The World Health Organization’s WHOQOL-BREF Quality of Life Assessment: Psychometric Properties and Results of the International Field Trial a Report from the WHOQOL Group. n.d doi: 10.1023/B:QURE.0000018486.91360.00. [DOI] [PubMed] [Google Scholar]
- Slater M, Kiran T. Measuring the patient experience in primary care. Can Fam Physician. 2016;62(12):e740–e748. [PMC free article] [PubMed] [Google Scholar]
- Smith JC, Mercy JA, Conn JM. Marital status and the risk of suicide. Am J Public Health. 1988;78(1):78–80. doi: 10.2105/ajph.78.1.78. (Retrieved from). < http://www.ncbi.nlm.nih.gov/pubmed/3337311>. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Straus MA. Measuring Intrafamily Conflict and Violence: the Conflict Tactics (CT) scales. J Marriage Fam. 1979;41(1):75–88. (Retrieved from). < https://eric.ed.gov/?id=EJ195884>. [Google Scholar]
- Thirumurthy H. SocioEconomic Survey from teh UCSF Sustainable East Africa Resarch on Community Health (SEARCH) Study: Modified for use in Kaloleni Primary Care Clinics n.d [Google Scholar]
- van Ginneken N, Tharyan P, Lewin S, Rao GN, Meera S, Pian J, Patel V. Non-specialist health worker interventions for the care of mental, neurological and substance-abuse disorders in low- and middle-income countries. Cochrane Database Syst Rev. 2013;11:CD009149. doi: 10.1002/14651858.CD009149.pub2. http://dx.doi.org/10.1002/14651858.CD009149.pub2. [DOI] [PubMed] [Google Scholar]
- Van Orden KA, Witte TK, Gordon KH, Bender TW, Joiner TE. Suicidal desire and the capability for suicide: tests of the interpersonal-psychological theory of suicidal behavior among adults. J Consult Clin Psychol. 2008;76(1):72–83. doi: 10.1037/0022-006X.76.1.72. http://dx.doi.org/10.1037/0022-006X.76.1.72. [DOI] [PubMed] [Google Scholar]
- Verdeli H, Clougherty K, Onyango G, Lewandowski E, Speelman L, Betancourt TS, Bolton P. Group Interpersonal Psychotherapy for depressed youth in IDP camps in Northern Uganda: adaptation and training. Child Adolesc Psychiatr Clin North Am. 2008;17(3):605–624. doi: 10.1016/j.chc.2008.03.002. http://dx.doi.org/10.1016/j.chc.2008.03.002. [DOI] [PubMed] [Google Scholar]
- Walker AK, Kavelaars A, Heijnen CJ, Dantzer R. Neuroinflammation and comorbidity of pain and depression. Pharmacol Rev. 2014;66(1):80–101. doi: 10.1124/pr.113.008144. http://dx.doi.org/10.1124/pr.113.008144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whittier AB, Gelaye B, Deyessa N, Bahretibeb Y, Kelkile TS, Berhane Y, Williams MA. Major depressive disorder and suicidal behavior among urban dwelling Ethiopian adult outpatients at a general hospital. J Affect Disord. 2016;197:58–65. doi: 10.1016/j.jad.2016.02.052. http://dx.doi.org/10.1016/j.jad.2016.02.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilsnack RW, Wilsnack SC, Kristjanson AF, Vogeltanz-Holm ND, Gmel G. Gender and Alcohol consumption: patterns from the multinational Genacis Project. Addiction. 2009;104(9):1487–1500. doi: 10.1111/j.1360-0443.2009.02696.x. http://dx.doi.org/10.1111/j.1360-0443.2009.02696.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. WHO | Preventing Suicide: A Global Imperative. WHO Press; Geneva: 2014. [Google Scholar]