Abstract
The government of Myanmar, with support from international donors, plans to address household financial risks from ill health and expand coverage. But evidence to design policy is limited. WHS (World Health Survey) data for 6045 households were used to investigate the association of out-of-pocket (OOP) health spending, catastrophic expenditures, and household borrowing and asset sales associated with illness with key socioeconomic and demographic correlates in Myanmar. Households with elderly and young children and chronically ill individuals, poor households, and ethnic minorities face higher financial stress from illness. Rural households use less care, suggesting their lower OOP health spending may be at the cost of health. Poorer groups rely more on public sector health services than richer groups. Better targeting, increased budgetary allocations, and more effective use of resources via designing cost-effective benefits packages appear key to sustainably addressing financial risks from ill health in Myanmar.
Keywords: equity, financial risk protection, health financing, health systems, Myanmar
Myanmar is among the poorest countries in Southeast Asia; with a stagnant economy and significant regional inequalities, nearly 32% of its population lives below the poverty line.1,2 Myanmar also has poor population health outcomes: it has among the highest rates of maternal and child mortality in the Southeast Asian region, with particularly poor health indicators in border areas where minorities live.3 Noncommunicable diseases (NCDs) are also emerging as a serious health challenge.4
Poor health outcomes have economic consequences for households, particularly when subsidized public services are hard to access and insurance options are limited. These economic consequences can take the form of earnings losses and use of health care services can result in out-of-pocket (OOP) expenses, borrowing and sale of assets.5,6 National Health Accounts data show that OOP spending accounts for more than 80% of aggregate health spending in Myanmar, the highest in the region.7–9 In 2012–2013, the share of health sector allocations in the government budget increased 3-fold, largely on curative care, but even at this higher level budgeted amounts remain low at about 0.8% of GDP.10
Discussions on universal coverage in Myanmar are gaining steam among national and international policy makers, and international donors appear ready to increase their health sector support to Myanmar.11 Expanded insurance coverage can contribute to financial risk protection, a key policy objective in most national health systems. However, the paucity of good quality information on health sector outcomes, including financial outcomes for households and groups who face higher risks from illness, remains a major challenge in effective use of health resources in Myanmar.11
We analyzed household-level predictors of OOP health spending, health service utilization and measures of financing stress from the World Health Survey (WHS) to understand the nature of illness related financial risks that households in Myanmar face. The WHS was used because it collected nationally representative information on OOP health spending and its financing and key potential correlates such as socioeconomic status, demographic characteristics, location and morbidity.12 To our knowledge this is the first study of household financial risks from illness in Myanmar in recent years.
Background
We briefly review the demographic and epidemiological profile of Myanmar and its health system—which likely underpin the financial risks confronting households in Myanmar.
Demographic and Epidemiological Profile
According to the UN (United Nations), Myanmar’s population was 51.9 million in 2010, almost 3 times that in 1950. This population is still quite young, with 26.1% of the population aged less than 15 years and 7.7% comprising the elderly (60 years plus).13 WHS data suggest the average size of a household in Myanmar to be 4.8, with one-third of its members below the age of 18.12 Life expectancy at birth has also risen from 36.1 years in 1950 to 64.2 years in 2010, with the share of the elderly expected to rise to 22.3% of total population by 2050.13 The population disease profile is also changing: estimates from the Global Burden of Disease 2010 study show that the share of NCDs in disability-adjusted life years (DALYs) rose from 33.0% in 1990 to 48.9% in 2010.4 The share of maternal and child health conditions and infectious diseases in DALYs lost correspondingly fell over this period.4
Health Service Delivery
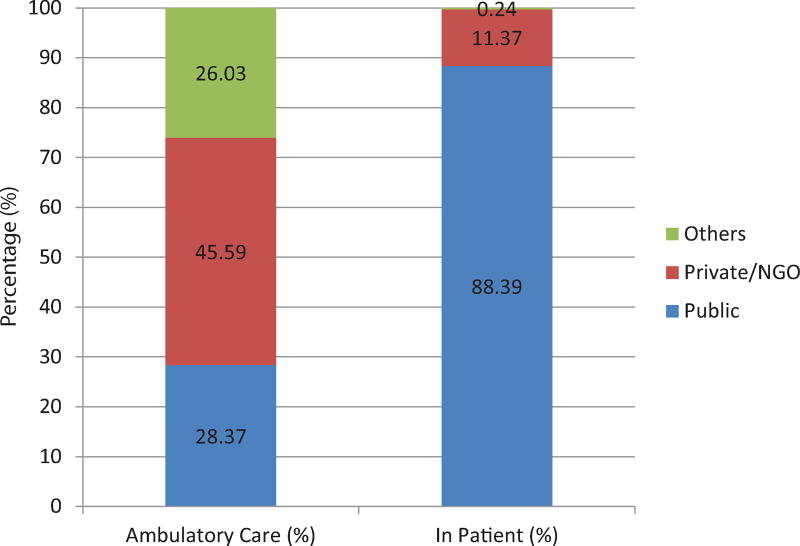
Both private and public health service providers are present in Myanmar with the former dominating ambulatory care and the latter dominating hospital services. The public sector accounts for about 90% of the 1090 hospitals currently operating in the country.3 Our estimates from analysis of raw WHS data for Myanmar show that 88% of the most recent hospital admissions were in the public sector.12 In contrast, the public sector share in the most recent ambulatory care visit was 28% (Figure 1).12 Provision of health services and budgets in Ministry of Health (MOH) facilities is highly centralized with little autonomy with regard to decision making at subnational levels. Private hospitals are concentrated in large cities and private for-profit ambulatory services (other than informal providers) are mostly located in urban areas.
Figure 1.
Ambulatory care visits and hospital admissions by provider type in Myanmar, 2003. Source: Authors’ (sample-weighted) estimates based on World Health Survey 2003.
Health Workforce
There are serious shortages in the health workforce of the country with only 17 doctors, 28 nurses and 23 midwives per 100 000 people in the public sector. The distribution of these personnel is also geographically unequal: Chin State has the highest density of 59 doctors and 160 nurses per 100 000 people, whereas Mon State had 6 doctors and 10 nurses per 100 000 people. The concentration of private practitioners in urban locations exacerbates these inequalities. Insufficient institutional capacity to absorb new health professional graduates adds to this with as many as 1500 doctors per year seeking employment outside the public health sector.3
Health Financing
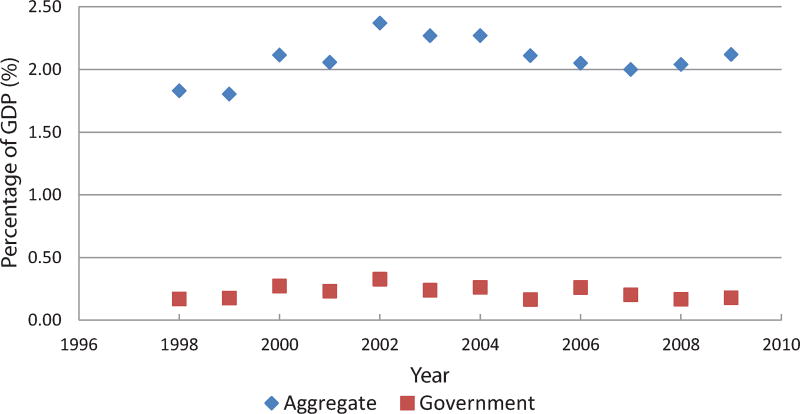
Health spending in Myanmar was 2.1% of GDP in 2009–2010, financed by a mix of government, households, social security, firms and external assistance.7 At US$12 per person, health care spending in Myanmar is among the lowest in the region and OOP health spending is 82.2% of total health spending.13 This contrasts with the share of the government which was merely 0.18% of GDP on health until 2012–2013, when it sharply increased to 0.80% of GDP. External aid accounts for about 9% of total health expenditures, a portion of which is also channeled through the government.7 Public and overall health spending as a share of GDP has remained essentially unchanged over the past decade (Figure 2).
Figure 2.
Aggregate and government health spending in Myanmar, 1998–2009. Source: Ministry of Heath reports on National Health Accounts (2007, 2009, and 2011).
In theory, services at public facilities are free to poor patients. But patients pay for items unavailable in public health facilities, particularly drugs and diagnostic services. National Health Accounts (NHA) for 2009–2010 in Myanmar show that 44.6% of all health spending was for drugs and consumables. Much of this spending on drugs and consumables was incurred by households, amounting to 53.7% of all OOP health spending. The NHA estimates are comparable to WHS estimates of the share of drugs of 47.8% of OOP health spending by households.7,12 In addition, NHA estimates of OOP spending on ambulatory care and diagnostics in 2009–2010 amounted to 32.4% of all household health expenses, comparable to WHS estimates of 33.8%.7,12
Methods
Data
The WHS survey, implemented in Myanmar during 2002–2003, covered 6045 households. The survey was implemented by the Ministry of Health, with a sampling frame that covered 90% of the population of Myanmar. The survey instrument collected information on household socioeconomic status, location and demographic characteristics, components of consumption spending, OOP health care expenditures and mechanisms (such as borrowing and asset sales) for financing health care. Sample households were selected based on a random, stratified sampling procedure, described in detail elsewhere.14
Methods
Our outcome measures included household (log) OOP spending and 2 measures of financial stress. The first measure of stress, “catastrophic health spending,” was defined as the ratio of a household’s OOP health expenditures to its “capacity to pay” exceeding 40%.8 Capacity was the difference between a household’s total expenditure and subsistence level spending based on national poverty line estimates.1,15 The second measure of stress was whether a household borrowed or sold assets in response to illness in the 12 months preceding the WHS.
We examined socioeconomic and demographic correlates of our 3 outcomes. The existing literature suggests that OOP health spending (and catastrophic spending) is correlated with the availability of health insurance, the incidence and severity of illness, demographic characteristics of households, incomes, and other indicators of socioeconomic position.16–18 The correlates used in this study are indicators of rural residence, household composition (size, presence of over-60-year-old members in the household, presence of a child younger than 5 years, female as household head), the highest level of education for an adult female family member (15 years and older), ethnicity (membership of the majority Bamar group), and economic status based on household rankings using a wealth index constructed using principal components methods.19 Two indicators of disease severity were also included (self-reported “bad or very bad” health by survey respondent and whether someone with chronic illness was a household member). An indicator for a pregnant woman was included given the likely impact on health care use. To account for antimalarial programs or people living in high malarial risk areas, we included an indicator for whether a household used an insecticide-treated bed net.
We estimated multivariate regression models to test the association between our outcomes and the explanatory variables described above. A major concern with any multivariate analysis is that estimated associations may capture effects of variables unaccounted for in the regression model such as interregional differences in costs of health care which can lead to varying OOP spending for local households, all else the same. This can bias our results. Thus, along with a baseline specification (specification 1), a fixed effects specification was estimated to account for such variations, using 108 additional indicator variables for the primary sampling units used in implementing the survey (specification 2). Using multiple specifications also helps to check how robust our results are.
A 2-part model was used to test the association between OOP spending and the explanatory variables.”20 The first part tests the association between an indicator variable for whether a household incurred any OOP spending and explanatory variables. The “second part” examines the correlates of (logarithm of) OOP health spending for the subset of households reporting any spending on health care. This is an effective statistical approach to handle large numbers of zeroes in OOP spending data, as in the Myanmar WHS. Moreover, the dependent variable of the first part (whether the household incurred any OOP spending) can be interpreted as an indicator of utilization/access, particularly given the high share of OOP spending on health care in Myanmar, and this enables additional insights.21 For example, if rural households have lower OOP than urban households, this might be due to lower rural average health care use and higher OOP when using health care, and not because rural households enjoy better financial risk protection than urban households.
We also assessed the relative share of public and private facilities in health care use at different levels of socioeconomic status (using the wealth quintile) based on the “last visit” or “hospital admission” reported by the respondent. For our statistical analyses, we used Stata, version 12.1.
Results
Summary statistics data in Table 1 underline that 75% of Myanmar’s population resides in rural areas, with one-fifth of the households being headed by women. Nearly one-third of the sample had an individual aged 60 years and over living in them, with a similar proportion reporting a child of less than 5 years. The majority Bamar community composed 72% of the sample. The share of respondents reporting “bad or very bad” health was 3%; and 4% of the households reported a member with “chronic” conditions. Nearly 41% of the households reported incurring catastrophic spending, and about 5% reported borrowing or selling assets to finance health care.
Table 1.
Descriptive Statistics for Sample Households From Myanmar WHS, 2003.
| Household Characteristics | Mean | SD |
|---|---|---|
| Out-of-pocket health expenditure (kyats) | 2632 | 7476 |
| Aggregate expenditure (kyats) | 42 098 | 32 190 |
| Catastrophic OOP expenditure (1 if yes, 0 otherwise) | 0.41 | 49.20 |
| Households reporting borrowing/asset sales (1 if yes, 0 otherwise) | 0.05 | 0.23 |
| Rural (1 if yes, 0 otherwise) | 0.75 | 0.43 |
| Household with elderly member (1 if yes, 0 otherwise) | 0.35 | 0.48 |
| Household with under-5 child (1 if yes, 0 otherwise) | 0.32 | 0.47 |
| Household with pregnant woman (1 if yes, 0 otherwise) | 0.03 | 0.18 |
| Household size | 4.80 | 2.03 |
| Female head of household (1 if yes, 0 otherwise) | 0.18 | 0.38 |
| Educational attainment of household head | ||
| Illiterate (1 if yes, 0 otherwise) | 0.46 | 0.50 |
| Primary and secondary (1 if yes, 0 otherwise) | 0.46 | 0.50 |
| High school and above (1 if yes, 0 otherwise) | 0.08 | 0.27 |
| Bamar (ethnic majority) (1 if yes, 0 otherwise) | 0.72 | 0.45 |
| “Bad/very bad” self-reported health (1 if yes, 0 otherwise) | 0.03 | 0.16 |
| Household member with chronic illness (1 if yes, 0 otherwise) | 0.04 | 0.20 |
| Use insecticide-treated bed-net (1 if yes, 0 otherwise) | 0.01 | 0.09 |
Authors’ (sample-weighted) estimates using WHS data for Myanmar. The total number of observations is 6045. Persons aged 60 years and over are defined as elderly. Catastrophic spending is defined as OOP exceeding 40% of a household’s capacity to pay (or the difference between household expenditure and the poverty line level of expenditure as per the national poverty line). Note that the means for indicator variables (taking values 0 or 1) in Table 1 can be translated into percentage terms by multiplying by 100.
Table 2 examines key correlates of catastrophic OOP spending and borrowing/sale of assets to finance health care. Catastrophic spending is positively correlated with a household having elderly members and children aged less than 5 years, larger sized households, female-headed households, households with respondents reporting poor self-reported health, and economically worse-off households. In specification 2, rural residence was negatively associated with catastrophic expenditure. Results for the multivariate analysis on the likelihood of asset sales or borrowing as the dependent variable are similar to those for catastrophic spending. Evidence on the relationship between ethnic status and economic outcomes was mixed, although in the expected direction, in that ethnic minorities were more likely to report financial stress, relative to the majority Bamar community.
Table 2.
Correlates of Catastrophic Spending in Myanmar: Logistic Regression Analyses, 2003.
| OOP Health Spending > 40% of Household Capacity to Pay |
Whether Household Borrowed Funds or Sold Assets to Finance Illness in preceding Year |
|||
|---|---|---|---|---|
|
|
|
|||
| Household Characteristic | (1) | (2) | (1) | (2) |
| Household location (rural = 1, 0 otherwise) | −0.01 (.96) | −2.30* (.01) | −0.06 (.89) | −0.92* (.01) |
| With individuals aged 60 and over (yes = 1, 0 otherwise) | 0.25* (.01) | 0.30* (.01) | 0.16 (.20) | 0.09 (.51) |
| With under-5 children (yes = 1, 0 otherwise) | 0.23* (.01) | 0.22* (.01) | 0.27† (.08) | 0.21 (.15) |
| Household size | 0.10* (.01) | 0.15* (.01) | 0.07* (.02) | 0.03 (.29) |
| Household ranking on asset index quintile 2 = 1, 0 otherwise | 0.03 (.80) | −0.12 (.26) | 0.03 (.90) | −0.07 (.76) |
| Household ranking on asset index quintile 3 = 1, 0 otherwise | 0.11 (.37) | 0.002 (.98) | −0.14 (.58) | −0.24 (.28) |
| Household ranking on asset index quintile 4 = 1, 0 otherwise | −0.16* (.27) | −0.37* (.01) | −0.18 (.55) | −0.28 (.29) |
| Household ranking on asset index quintile 5 (richest 20%) = 1, 0 otherwise | −0.38* (.02) | −0.71* (.01) | −0.92* (.04) | −0.94* (.02) |
| Sex of household head (female = 1, 0 otherwise) | 0.15 (.14) | 0.16† (.10) | 0.07 (.70) | 0.13 (.49) |
| Most educated female 15+ illiterate = 1, 0 otherwise | 0.08 (.53) | 0.13 (.28) | 0.30 (.28) | 0.05 (.85) |
| Most educated female 15+ primary and secondary=1, 0 otherwise | 0.12 (.14) | 0.14 (.17) | 0.41† (.08) | 0.08 (.72) |
| Ethnic Bamar (yes = 1, 0 otherwise) | 0.34† (.06) | −0.05 (.71) | 0.41 (.17) | −0.36† (.10) |
| SRH of respondent (bad/very bad = 1, 0 otherwise) | 1.00* (.01) | 0.85* (.01) | 1.36* (.01) | 1.00* (.01) |
| Member with chronic illness (yes = 1, 0 otherwise) | 0.62* (.01) | 0.51* (.01) | 0.60* (.01) | 0.73* (.03) |
| Uses insecticide-treated bed net (yes = 1, 0 otherwise) | 1.86* (.03) | 0.52 (.29) | 0.23 (.64) | −0.07 (.94) |
| With pregnant woman (yes = 1, 0 otherwise) | 0.31* (.05) | 0.19 (.27) | 0.46† (.09) | 0.39 (.21) |
| Total number of observations | 6045 | 6045 | 6045 | 6045 |
Authors’ estimates based on WHS data and sample-weighted (P values for a 2-tailed test are reported in parentheses below the coefficient estimates). S (1) uses Strata fixed effects and S (2) uses an additional 108 indicator variables for cluster fixed effects, for which coefficient estimates are not reported for reasons of space. Standard errors are adjusted for clustering at the primary sampling unit level.
Statistically significant at the 5% level.
Statistically significant at the 10% level.
Table 3 reports results from the estimation of the 2-part model.
Table 3.
Correlates of Out-of-Pocket Spending Due to Illness in Myanmar: 2-Part Model, 2003.
| Part I Whether OOP Expenditure > 0 |
Part II Log (OOP Expenditure) |
|||
|---|---|---|---|---|
|
|
|
|||
| Household Characteristic | (1) | (2) | (1) | (2) |
| Household location (rural = 1, 0 otherwise) | −0.27 (.29) | −2.44* (.01) | 0.14† (.10) | 0.24* (.01) |
| Individuals aged 60 and over (yes = 1, 0 otherwise) | 0.05 (.43) | 0.09 (.28) | 0.12* (.01) | 0.14* (.01) |
| With under-5 children (yes = 1, 0 otherwise) | 0.30* (.01) | 0.30* (.01) | 0.09* (.05) | 0.09* (.04) |
| Household size | 0.005 (.84) | 0.06* (.01) | −0.15* (.01) | −0.14* (.01) |
| Household ranking on asset index quintile 2 = 1, 0 otherwise | 0.13 (.31) | −0.12 (.29) | 0.003 (.97) | 0.01 (.88) |
| Household ranking on asset index quintile 3 = 1, 0 otherwise | 0.35* (.01) | 0.21† (.07) | 0.10 (.21) | 0.12† (.08) |
| Household ranking on asset index quintile 4 = 1, 0 otherwise | 0.36* (.02) | 0.14 (.28) | 0.21* (.01) | 0.21* (.01) |
| Household ranking on asset index quintile 5 = 1, 0 otherwise | 0.53* (.01) | 0.36* (.02) | 0.52* (.01) | 0.51* (.01) |
| Sex of household head (female = 1, 0 otherwise) | 0.08 (.49) | 0.05 (.67) | −0.07 (.22) | −0.05 (.34) |
| Most educated female 15+ illiterate = 1, 0 otherwise | −0.13 (.38) | −0.06 (.63) | −0.15† (.08) | −0.20* (.01) |
| Most educated female 15+ primary/secondary=1, 0 otherwise | 0.01 (.90) | 0.03 (.78) | −0.15* (.02) | −0.17* (.01) |
| Ethnic Bamar (yes = 1, 0 otherwise) | 0.52* (.01) | 0.12 (.39) | −0.18* (.02) | −0.26† (.08) |
| SRH of respondent (bad/very bad = 1, 0 otherwise) | 0.94* (.01) | 0.80* (.01) | 0.43* (.01) | 0.38* (.01) |
| Member with chronic illness (yes = 1, 0 otherwise) | 0.88* (.01) | 0.59* (.01) | 0.43* (.01) | 0.47* (.01) |
| Uses insecticide-treated bed net (yes = 1, 0 otherwise) | 1.63† (.10) | 0.06 (.93) | −0.15 (.53) | 0.10 (.79) |
| With pregnant woman (yes = 1, 0 otherwise) | 0.43* (.02) | 0.34† (.10) | 0.15† (.10) | 0.13 (.17) |
| Total number of observations | 6045 | 6045 | 3514 | 3514 |
Authors’ estimates based on WHS data and sample-weighted (P values for a 2-tailed test are reported in parentheses below the coefficient estimates). S (1) uses 8 strata fixed effects and S (2) uses 108 indicator variables for cluster fixed effects, for which coefficient estimates are not reported for reasons of space.
Statistically significant at the 5% level.
Statistically significant at the 10% level.
The first part of the model (columns 2 and 3 in Table 3) examines the association between whether a household incurred any OOP spending—a proxy for health care use—and explanatory variables. Health care use is positively correlated with a household having children aged less than 5 years, households where the respondent reported poor health, households where a person with chronic illness resides, household with pregnant women, and larger sized households. Moreover, wealthier households are more likely to use health care than their poorer counterparts.
Columns 4 and 5 in table 3 presents results from the “second part” of our 2-part model: an association of OOP spending and plausible correlates for the subset of households that report any spending on health care. The results suggest that households with elderly, households with young children, richer households, ethnic minorities and rural households spend more on average.
Table 4 presents data on the share of public sector ambulatory visits (or inpatient stays) by household wealth quintile. There is a gradient by household wealth in the percentage of visits (or stays) which are public: 93% of hospital admissions among the poorest 20% were in the public sector, compared to 80% among the richest 20%, similar to results from many other developing countries.22,23 At the same time, data on per capita hospital admissions in the past 5 years in Myanmar (column 4 of table 4) show that wealthier households use public hospitals more frequently than poorer households.
Table 4.
Public Sector Health Services Use by Quintile in Myanmar, 2003.
| Share of Public Sector (%) in | |||
|---|---|---|---|
|
|
|||
| Rankings by Asset Quintiles |
Most Recent Ambulatory Care Visit (Recall Period: 12 Months) |
Most Recent Hospital Stay (Recall Period: 5 Years) |
Public Hospital Use (per 100 Households) in Past 5 Years |
| Quintile 1 (poorest 20%) | 37.64 | 96.53 | 4.13 |
| Quintile 2 | 35.23 | 94.25 | 6.12 |
| Quintile 3 | 31.26 | 84.83 | 5.07 |
| Quintile 4 | 23.02 | 86.80 | 7.17 |
| Quintile 5 (richest 20%) | 16.96 | 83.41 | 8.85 |
Authors’ sample-weighted estimates using WHS data. Households are ranked by asset quintiles based on scores constructed using principal components methods.
Discussion and Conclusions
Existing literature has highlighted the economic burden that households and specific subgroups face from illness in developing countries.24 We confirm many of these findings and illustrate the major correlates of financial risks that households face from illness in the specific context of Myanmar: poorer households, households with elderly members, young children, members who are chronically ill or who report poor health, and minority ethnic communities face a greater risk of catastrophic health expenditures. While rural households are less likely to incur catastrophic expenses they also use less care. This saves on OOP expenditures, but could adversely affect their health and earnings opportunities. Richer households use more health care and conditional on use, spend more on health care, but face lower financial stress. Although the poor seek health care less frequently than the rich, when they do, they are more likely to rely on the public sector than the rich; similar findings in other settings have been reported elsewhere.23 Unfortunately, the rich use more of all health services, public and private, so public health subsidies in Myanmar are likely to be unequally distributed across socioeconomic groups.
Our findings shed light on the need to better target health sector resources in Myanmar, including for curative care, to specific population groups, including households with young children, households living in rural areas and households with chronically ill members. However, Myanmar’s public sector share of aggregate health spending is low relative to other countries in the region and will adversely impact physical access and quality of health services for needy groups.25 Limited budgets likely result in fewer personnel, shortages of drugs and other equipment and overall quality of care in public sector facilities. In WHS data, nearly 15.5% of rural respondents rated their outpatient care experience in the public sector as being moderate to very bad (compared to 5.3% for urban respondents).12 Shortages of drugs and other equipment in public sector facilities are reflected in high levels of OOP spending for drugs and diagnostics in National Health Accounts data.7 The mountainous terrain and the predominantly rural location of Myanmar’s population is an additional constraint in physically accessing health services with almost one-fifth of WHS respondents finding travel time as being moderate to very bad.12
Budgetary constraints in Myanmar government will limit its ability to replicate the large increases in health sector allocations introduced by China and India in recent years.26 Serious economic challenges remain alongside the social challenges of a society with ethnic strife just emerging from a long period of military rule. Although the government has increased its health allocations in the current budgetary cycle, its continuation is questionable without sustained assistance from international donors.27 However, the government could still promote efficient spending of public funds on health through priority-setting processes, say by providing well defined benefit packages that are cost-effective in addition to targeting key groups. One example of targeted support is a recent Global Alliance on Vaccines Initiative (GAVI) effort to provide funding for infrastructure development and a pool to cover expenses for poor households requiring inpatient treatment.28 Resource effectiveness could also be enhanced via targeting key gaps in personnel, drugs, and consumables to help use available resources better and implementing prevention and primary care programs. These could include promoting maternal health, child vaccination, and prevention actions for NCDs and major infectious diseases in Myanmar. Investment in program evaluation is needed to ensure funds are used effectively and efficiently, as the government and donors introduce additional funds and money into the system.
Our analysis has obvious weaknesses. The 2003 WHS data are a decade old and the aggregate health spending in 2003 was slightly higher as a proportion of GDP than in later years (Figure 1). This may influence our findings. The indicators of financial stress used in this article do not adequately capture other possible implications of ill health, such as loss of work effort and earnings, especially when households forgo care due to lack of finances or physical access. Including these considerations would present a bleaker picture of the impact of illness in Myanmar.24
These limitations withstanding, Myanmar’s domestic policy and economic environment has changed little since 2003. Official data suggest rapid income growth but are considered unreliable by experts.2 Raw data from 2 rounds of the Integrated Household Living Conditions Survey (IHLCS) in 2004–2005 and 2009–2010 are not readily accessible, but published reports from these data show that OOP health spending has remained unchanged as a proportion of total household spending over the 2 survey rounds at 5%.1 This is comparable to 6% in WHS data.12 IHLCS surveys also show that absolute levels of real OOP health spending have also changed little over the 2 survey rounds. While newer data are obviously needed, the findings based on WHS data may not change, even with more recent survey data.
Acknowledgments
The authors wish to acknowledge the constructive comments of 2 anonymous reviewers that have greatly improved this article.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: SH acknowledges support from the Australian Leadership Awards of the Australian government. KA acknowledges support from the Australian Postgraduate Award of the Australian government. AM was supported by an establishment grant from Monash University.
Footnotes
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- 1.Ministry of National Planning and Economic Development, editor. Ministry of National Planning and Economic Development. Integrated Household Living Conditions Survey in Myanmar: Poverty Profile. Nay Pyi Taw, Myanmar: Government of Myanmar; 2012. [Google Scholar]
- 2.Myint U. Myanmar’s GDP growth and investment: lessons from a historical perspective. In: Skidmore M, Wilson T, editors. Dictatorship, Disorder and Decline in Myanmar. Canberra: Australian National University; 2008. p. 229. [Google Scholar]
- 3.Ministry of Health. Myanmar Health Statistics. Nay Pyi Taw, Myanmar: Department of Health Planning; 2010. [Google Scholar]
- 4.Institute for Health Metrics and Evaluation. Global Burden of Disease Study 2010 Online Database. Seattle, WA: [Accessed August 12, 2014]. Available at: http://www.healthdata.org/sites/default/files/files/country_profiles/GBD/ihme_gbd_country_report_myanmar.pdf. [Google Scholar]
- 5.Bloom D, Canning D. The health and wealth of nations. Science. 2000;287:1207–1209. doi: 10.1126/science.287.5456.1207. [DOI] [PubMed] [Google Scholar]
- 6.Gertler P, Gruber J. Insuring consumption against illness. Amer Econ Rev. 2002;92(1):51–70. doi: 10.1257/000282802760015603. [DOI] [PubMed] [Google Scholar]
- 7.Ministry of Health. National Health Accounts, Myanmar (2009–2010) Nay Pyi Taw, Myanmar: Government of Myanmar; 2012. [Google Scholar]
- 8.van Doorslaer E, O’Donnell O, Rannan-Eliya R, et al. Paying out-of-pocket for health care in Asia: catastrophic and poverty impact. [Accessed January 15, 2014];EQUITAP Working Paper no. 2. 2005 Available at: http://econpapers.repec.org/paper/esswpaper/id_3a823.htm.
- 9.Sein TT, Myint P, Tin N, Win H, Aye SS, Sein T. The Republic of the Union of Myanmar: health system review. Health Syst Transition. 2014;4(3) [Google Scholar]
- 10.Grundy J. Road to Recovery: Charting a Course to Universal Health Coverage in Myanmar. Melbourne, Australia: University of Melbourne; 2013. [Google Scholar]
- 11.Risso-Gill I, McKee M, Coker R, Piot P, Legido-Quigley H. Health system strengthening in Myanmar during political reforms: perspectives from international agencies. Heal Pol Plan. 2013;29:1–9. doi: 10.1093/heapol/czt037. [DOI] [PubMed] [Google Scholar]
- 12.World Health Organization (WHO) World Health Survey: Report of Myanmar. Geneva, Switzerland: WHO; 2003. [Google Scholar]
- 13.United Nations (UN) UN Population Statistics (POPIN) Online Database. [Accessed August 12, 2014]; Available at: http://esa.un.org/unpd/wpp/index.htm.
- 14.WHO (World Health Organization) World Health Survey Sampling Guidelines for Participating Countries. Geneva, Switzerland: WHO; 2003. [Google Scholar]
- 15.Xu K, Evans D, Kawabata K, Zeramdini R, Klavus J, Murray C. Household catastrophic health expenditure: a multi-country analysis. Lancet. 2003;362:111–117. doi: 10.1016/S0140-6736(03)13861-5. [DOI] [PubMed] [Google Scholar]
- 16.Spaan E, Mathijssen J, Tromp N, McBain F, Have A, Baltussen R. The impact of health insurance in Africa and Asia: a systematic review. Bull WHO. 2012;90(9):685–692. doi: 10.2471/BLT.12.102301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Li Y, Xu L, Legge D, et al. Factors affecting catastrophic health expenditure and impoverishment from medical expenses in China: policy implications of universal health insurance. Bull WHO. 2012;90(9):664. doi: 10.2471/BLT.12.102178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Valtorta N, Hanratty B. Socioeconomic variation in the financial consequences of ill health for older people with chronic diseases: a systematic review. Maturitas. 2013;74(4):313–333. doi: 10.1016/j.maturitas.2013.01.015. [DOI] [PubMed] [Google Scholar]
- 19.Vu L, Tran B, Le A. The use of total assets as a proxy for socioeconomic status in northern Vietnam. Asia Pac J Public Health. 2011;23(6):996–1004. doi: 10.1177/1010539510361638. [DOI] [PubMed] [Google Scholar]
- 20.Yip W, Berman P. Targeted health insurance in a low income country and its impact on access and equity in access: Egypt’s school health insurance. Health Econ. 2001;10(3):207–220. doi: 10.1002/hec.589. [DOI] [PubMed] [Google Scholar]
- 21.Jung J, Liu J. Does Health Insurance Decrease Health Expenditure Risk in Developing Countries? The Case of China Unpublished. Towson, MD: Towson University, Department of Economics; 2012. [Google Scholar]
- 22.Mahal A, Yazbeck A, Peters D, Ramana G. The Poor and Health Service Use in India. Washington, DC: World Bank, Health Nutrition and Population Working Paper; 2001. [Google Scholar]
- 23.Peters D, Garg A, Bloom G, Walker D, Brieger W, Rahman M. Poverty and access to health care in developing countries. Ann New York Acad Sci. 2008;1136:161–171. doi: 10.1196/annals.1425.011. [DOI] [PubMed] [Google Scholar]
- 24.Alam K, Mahal A. Economic impacts of health shocks on households in low and middle income countries: a review of the literature. Global Health. 2014;10:21. doi: 10.1186/1744-8603-10-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kwon S. Health care financing in Asia: key issues and challenges. Asia Pac J Public Health. 2011;23(5):651–661. doi: 10.1177/1010539511422940. 2011. [DOI] [PubMed] [Google Scholar]
- 26.Yip W, Mahal A. The health care systems of China and India: performance and future challenges. Health Aff. 2008;27(4):921–932. doi: 10.1377/hlthaff.27.4.921. [DOI] [PubMed] [Google Scholar]
- 27.Government of Myanmar. DPO 2012 Presentation Folder; Conference on Development of Policy Options with Special Reference to Education and Health in Myanmar; Nay Pyi Taw, Myanmar. 2012. [Google Scholar]
- 28.Tin N, Lwin S, Kyaing N, Htay T, Grundy J, Skold M. An approach to health system strengthening in the Union of Myanmar. Health Pol. 2010;95:95–102. doi: 10.1016/j.healthpol.2009.11.013. [DOI] [PubMed] [Google Scholar]