Abstract
Objective. To evaluate the design, implementation, and outcomes of a three-week pharmacy bridging course (PBC) covering five math and science areas for first-year doctor of pharmacy students in fall 2015.
Methods. Each topic was taught as a separate module. All five modules used pre- and post-module assessments to measure student knowledge and confidence. Course grades for subsequent first-year courses (PY1) were collected to examine relationships between PBC and PY1 courses.
Results. Scores on the post-knowledge assessments increased for all five subject areas compared to scores on pre-PBC knowledge assessments. Student confidence also increased pre-/post- in applied mathematics, biostatistics, and organic chemistry. Students agreed that PBC enhanced their level of academic preparation and increased their motivation to continue in the program. PBC performance was strongly correlated with first-year grade point average.
Conclusion. A bridging course is both feasible and effective for helping students prepare for and transition into a doctor of pharmacy degree program.
Keywords: short course, flipped classroom, biostatistics, physiology, chemistry
INTRODUCTION
Bridging courses are short intensive courses commonly designed to increase knowledge, boost confidence, facilitate academic and social transitions, and enhance student preparation for more advanced impending coursework. A growing body of research points to the benefits of providing a short course to bridge the academic gap and help students transition between two educational environments or programs.1-4 In undergraduate education, these courses tend to focus on helping incoming students transition into the college environment and coursework.1,4 In contrast, professions education typically use these types of courses to help students transition from a degree program into the workplace or postgraduate training (eg, a fourth-year capstone to assess clinical readiness).2,3 This approach may be particularly relevant for pharmacy education, where students enroll in doctoral programs with a broad array of skills, experiences, and expectations. Exploring the use of a bridging course for students transitioning into a doctor of pharmacy (PharmD) program is an important step toward helping students prepare for the demands of a professional curriculum. In fall 2015, a three-week pharmacy bridging course (PBC) comprised of five modules spanning foundational math and science areas was developed and implemented for first-year doctor of pharmacy students at the UNC Eshelman School of Pharmacy. This brief describes the design, implementation, and outcomes of the PBC.
METHODS
The PBC was a 3.5-credit hour course comprised of five modules: applied mathematics, biochemistry, biostatistics, organic chemistry, and physiology. There were 153 students enrolled, with 128 on the Chapel Hill campus and 25 connected synchronously from the Asheville campus. PBC was the first course offered in the school’s transformed curriculum.14 All first-year incoming students were required to take the course in a span of three weeks in August without concurrent courses. Once students completed PBC, they had to take the following classes immediately: Pathophysiology of Human Disease, Molecular Foundations of Drug Action, Evidence-Based Practice, Pharmacy Calculations and Medical Terminology, Immunization Training, and On Becoming a Pharmacist.
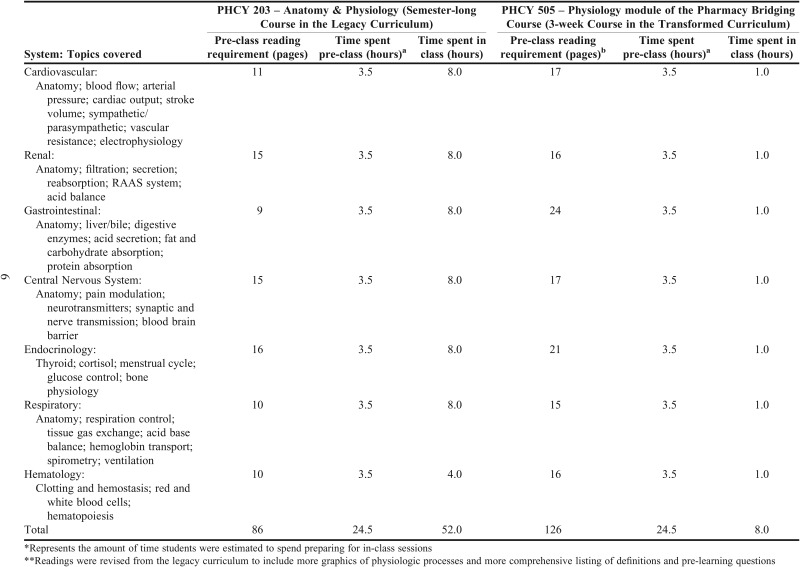
PBC included prerequisite content often retaught in the legacy curriculum as part of the foundational coursework (all topics except for biochemistry were required prerequisites for admission in 2015; biochemistry became a prerequisite in 2016). Within the legacy curriculum, for example, physiology was included as a 4 credit-hour course (60 contact hours) designed to address student deficiencies prior to pharmacotherapy coursework. Aspects of organic chemistry were retaught in three separate courses in the legacy curriculum (ie, pharmaceutics, medicinal chemistry, and pharmacodynamics) while applied math was reviewed in courses such as pharmacodynamics and pharmaceutical calculations. By creating the PBC, it is estimated that the time spent on these core topics decreased from 150+ hours spread across several courses in the legacy curriculum to approximately 35 hours of PBC at the onset of the transformed curriculum (Appendix).
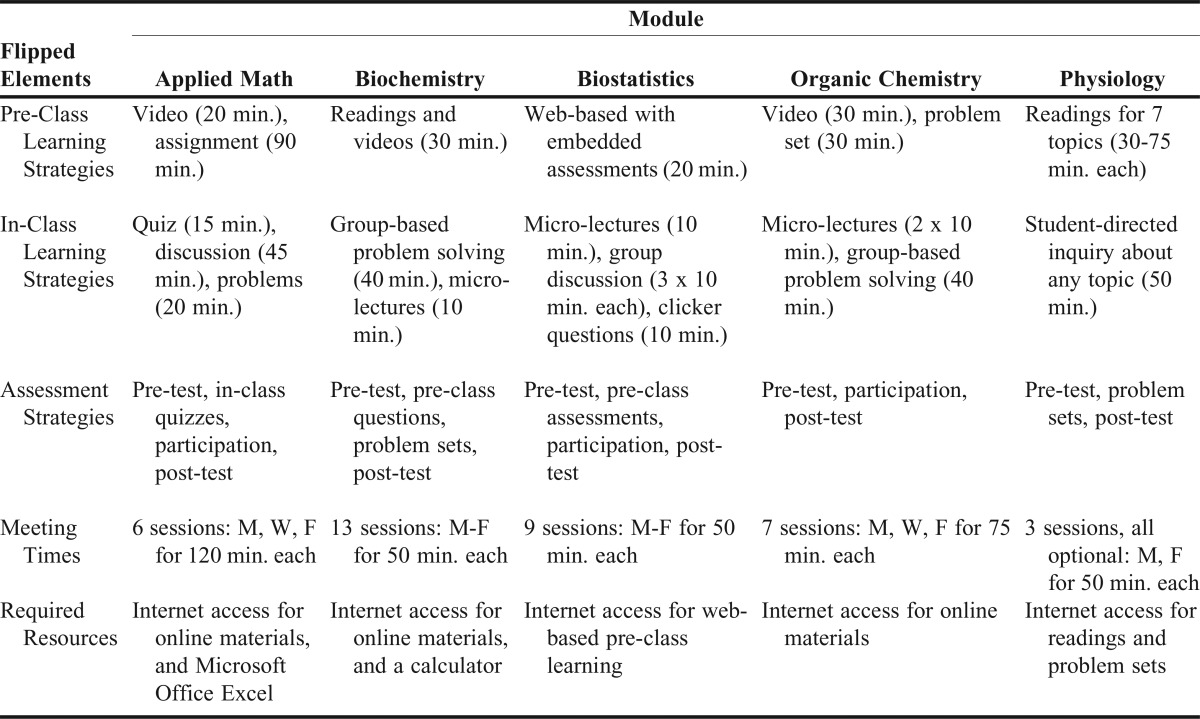
PBC was designed to help students learn key facts critical for the field of pharmacy, level the playing field for a diverse group of students, and introduce students to the instructional methods used in the transformed curriculum. Module directors were afforded the autonomy to design their respective module using any modalities, strategies, or technologies that aligned with the core principles of PBC, the flipped classroom,6-14 and the time constraints of the course. Students were required to earn 55 points (out of 100) in each module to pass. Physiology included an additional passing requirement for each topic area. The strategies and time commitments used for module development reflected the diversity and creativity of flipped implementation used by module directors (Table 1). The course director welcomed the students on the first day of PBC, provided an overview of the course, facilitated the implementation of all data collection instruments, and encouraged students to provide feedback about PBC throughout the course.
Table 1.
Operationalization of the Flipped Classroom for the Five Modules of the Pharmacy Bridging Course, Including Learning Strategies, Meeting Times, and Estimated Time Commitments
All modules used a required pre-test and post-test to assess student knowledge. On the day prior to the first module class session, students completed a pre-test that covered basic knowledge for all five modules. Each module pre-test was written by the module director and included only multiple choice questions, with the exception of some calculation problems in applied math. At the start of the first class session for each module, a survey was also administered to students to collect information about their confidence in knowledge of the topic (from 0 not at all confident to 100 completely confident). Confidence was also measured at the end of each module, along with a post-test written by the module director to reflect the same concepts, format, and difficulty as the pre-test. The number of questions on the post-test ranged from 20 items (biochemistry) to 97 items (physiology). All instruments were reviewed by the course director and module directors. A course evaluation was administered at the end of the course. The pre-test and post-test were required. The survey and course evaluation were voluntary and no incentives were provided. All instruments were administered using SofTest (Examsoft, Dallas, TX) except for applied math, which was paper and pen.
Course grades for all subsequent first-year courses (PY1) were also collected, along with admissions data for each student. Course grades were measured on a scale of 1(F) to 4(A) and averaged for an end of PY1 grade point average (GPA). All statistical analyses were conducted in SPSS, v23 (IBM, Armonk, NY). Paired t-test was used for all pre-post analyses. Pearson correlation was used to examine the relationship between PBC performance and end of PY1 GPA. Continuous data are represented by mean (standard deviation) and categorical data are represented by (median, range). A p<.05 was considered significant. This study was determined to be exempt from full review by the UNC Institutional Review Board.
RESULTS
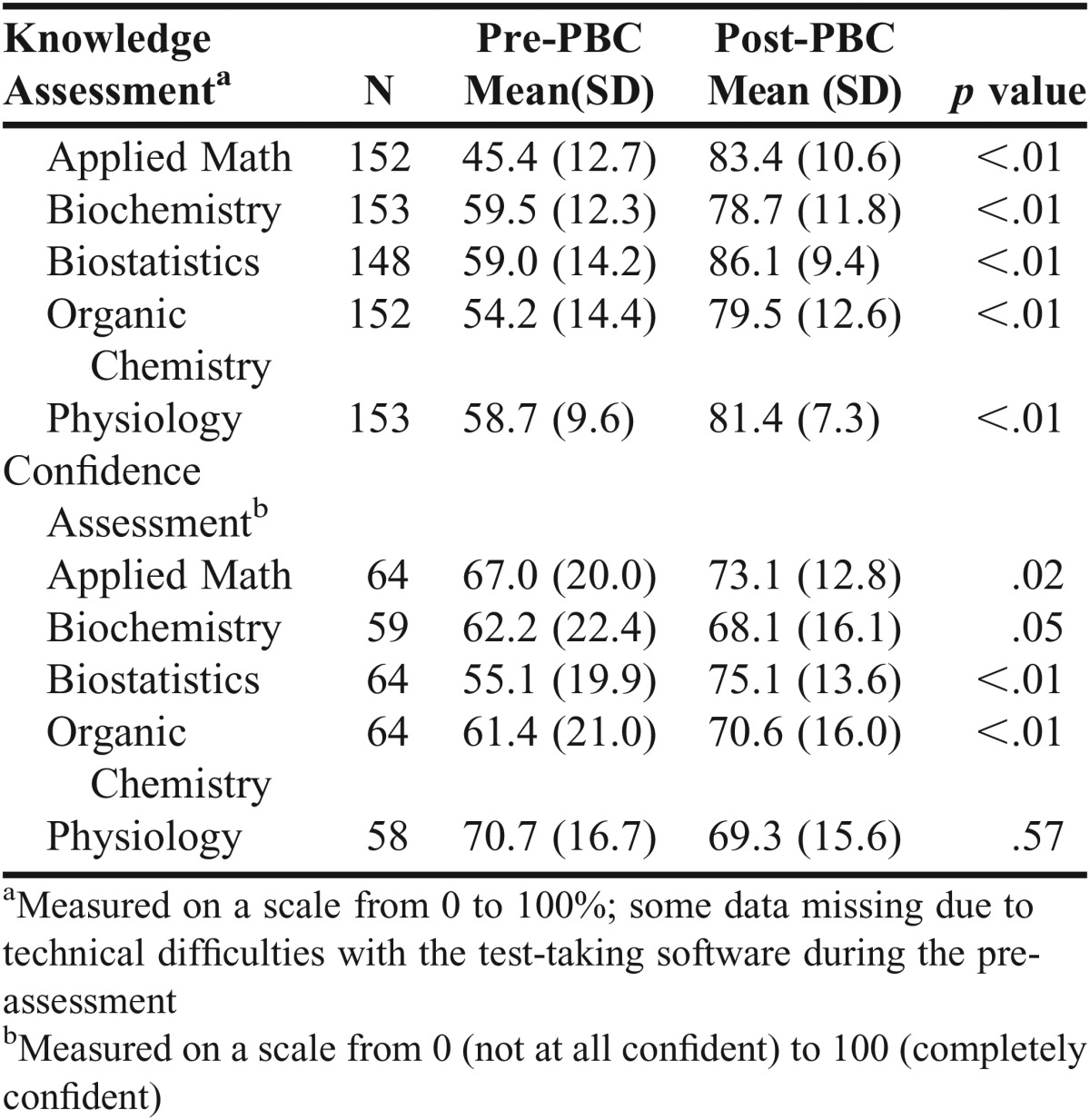
Most students in PBC were female (68%), white/Caucasian (62%), and have a bachelor’s degree prior to enrollment (78%). Average PCAT and undergraduate GPA were 87.58 (10.6) and 3.48 (.3) respectively. In PBC, 138 students (90.2%) scored ≤ 55% on one or more module pre-test, with 12 students failing all five pre-tests. There was a significant increase in scores from pre-test to post-test for all five subject areas (p<.01) (Table 2). Notably, students scoring 1 SD below the mean in applied math on the pre-test (n = 25) improved from 28.5(2.7) to 77.6(11.9) (p<.01) on the post-test; biochemistry (n=27) improved from 40.4(6.3) to 70.0(14.6) (p<.01); biostatistics (n=23) improved from 34.8(5.3) to 86.2(10.5) (p<.01); organic chemistry (n=14) improved from 30.0(4.3) to 68.6(10.9) (p<.01); and physiology (n=30) improved from 45.5(3.2) to 76.1(8.7) (p<.01).
Table 2.
Performance and Perception Scores for Each Subject Area (N=153)
Eight students did not achieve a passing score for biochemistry, three for organic chemistry, and two for applied math. In the physiology module, all students passed the module but 18 students failed an additional passing requirement for a topic area. Two students failed to achieve a passing score for more than one module. Students who did not pass were asked to work with the module director to create an individual learning plan consisting of self-directed study with online resources, meetings with remediation assistants, and input from the module instructors.
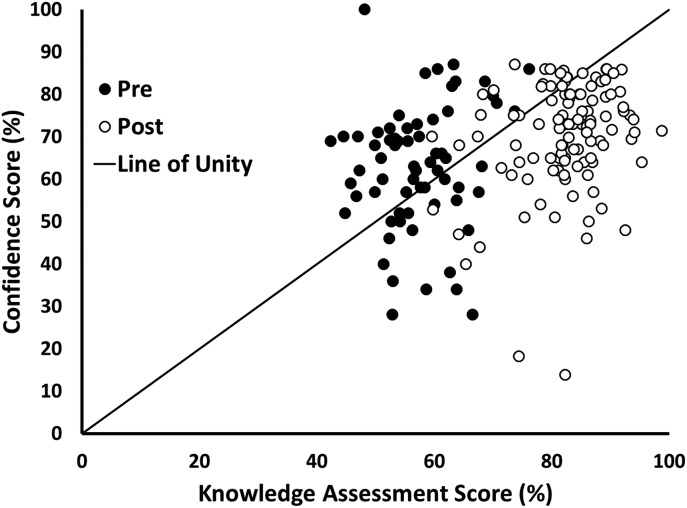
Confidence significantly increased in three topic areas: applied math (p=.02); biostatistics (p<.01); and organic chemistry (p<.01) (response rates 38% to 42%). In an analysis of confidence and test scores (Figure 1), students were generally overconfident on the pre-tests (ie, average pre-module confidence scores > average pre-test scores) and underconfident on the post-tests (ie, average post-module confidence scores < average post-test scores). More than 100 students completed the course evaluation (response rate 68.6%). On a five-point scale from 1 (poor) to 5 (excellent), PBC received an overall rating of very good (median=4, range 1-5), with 62% indicating the value of what they learned during PBC as very good or excellent. Eighty-six percent of students agreed or strongly agreed that the course enhanced their level of academic preparation (median=4, range 2-5), 84.8% agreed or strongly agreed that they needed the modules of the PBC, and 67.6% agreed or strongly agreed that PBC increased their motivation to continue in the PharmD program (median=4, range 1-5).
Figure 1.
Scatter Plot of Average Confidence Scores and Knowledge Test Scores, Pre- and Post-2015 PBC (n=58).
PBC overall performance (ie, average performance across all five modules) was very strongly correlated with PY1 GPA (rp=.8, p<.001) and moderately correlated with PCAT (rp=.5, p<.001) and undergraduate GPA (rp=.4, p<.001). The relationship of each module to each course in the PY1 year is beyond the scope of this brief.
DISCUSSION
Bridging courses provide schools with an opportunity to facilitate student transition into a curriculum while affording students the opportunity to further prepare for their impending studies.2,3 This study suggests that a bridging course for newly enrolled PharmD students improved confidence and increased knowledge for five key subject areas critical for success in pharmacy school, particularly for those who performed poorly on the pre-test. In addition, performance in this course was strongly related to performance in subsequent courses, which suggests that the PBC may have utility for identifying students early on that may benefit from additional academic support later in the curriculum. The findings of this study complement research that demonstrate positive outcomes associated with formally facilitating the academic transition into a new program or environment.15,16 Shreiber and colleagues, for example, described a multidisciplinary “boot camp” that created a network of peers and mentors, established a common language, and improved student proficiency in relevant techniques for undergraduates.17 Wayne and colleagues found that a 16-hour “boot camp” for students entering medical residency boosted a variety of clinical skills.3
Although this study was not designed specifically to evaluate the impact of using a flipped classroom design, there are several aspects of this design element worth noting. By asking module directors to use a flipped course design, the school was able to adhere to its guiding principles of active student engagement14 while empowering faculty to choose from a wide range of options for designing the module. The five module directors in this course employed various strategies for delivering content to students prior to class and engaging students in active learning during class, illustrating the flexibility and functionality of the flipped classroom for the enabling math and sciences.
While this course was seen as largely successful in its first iteration, optimizing the effectiveness of any course requires adaptation and adjustments. Based on our experiences and student feedback, changes to subsequent course offerings include: a redesigned applied math module as a self-paced online course; a new pharmacy toolkit module that introduces students to foundational pharmacy practice terminology and concepts; a new evidence-based learning module designed to help students articulate their PharmD learning goals, post-PharmD professional goals, and preferred learning approaches; more in-class time for the physiology module; and a higher passing criteria to ensure a minimal level of competency balanced with desirable difficulty.
In our experience, a bridging course is critical for students entering a PharmD program. However, further research is needed to understand how this course impacts student performance and behavior in subsequent coursework. For example, which elements of PBC (eg, course content, student small group collaborations, faculty interactions) help students transition into the PharmD program? Which content areas are most relevant for success later in the program? Low response rates for the confidence and difficulty data currently limit our ability to fully understand the relationship of these constructs with other aspects of the course and future research should examine these aspects more closely. In addition, this study was a pre-post design for a single cohort at a single institution, which limits our ability to generalize the findings. Future research should also examine longer term outcomes associated with the course.
CONCLUSION
Students demonstrated measureable increases in performance and perceptions across five key subject areas. This study is a first step toward understanding how a bridging course can help students transition into a doctor of pharmacy degree program. The design principles and tenets used to implement the course could be useful for other institutions.
ACKNOWLEDGMENTS
The authors would like to acknowledge the course director, Scott Singleton, along with all of the course module directors and instructors that helped design and implement all aspects of the Pharmacy Bridging Course.
Appendix. Time Spent on Physiology Content from a Semester-long Course (Legacy Curriculum) to the Three-week PBC (Transformed Curriculum)
Footnotes
Figure 1. The line of unity represents the point at which confidence matches performance on the test. Dots above the line of unity reflect overconfidence and dots below the line of unity reflect underconfidence.
REFERENCES
- 1.Gordon S, Nicholas J. Students’ conceptions of mathematics bridging courses. J Further Higher Educ. 2013;37(1):109–125. [Google Scholar]
- 2.Teo AR, Harleman E, O’Sullivan PS, Maa J. The key role of a transition course in preparing medical students for internship. Acad Med. 2011;86(7):860–865. doi: 10.1097/ACM.0b013e31821d6ae2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wayne DB, Cohen ER, Singer BD, et al. Progress toward improving medical school graduates’ skills via a “boot camp” curriculum. Simul Healthcare. 2014;9(1):33–39. doi: 10.1097/SIH.0000000000000001. [DOI] [PubMed] [Google Scholar]
- 4.Youl D, Read J, George A, Masters A, Schmid S, King M. Bridging the gap – student understanding and the chemistry bridging course. Poster presentation, UniServe Science Blended Learning Symposium Proceedings. 2005:191–194. [Google Scholar]
- 5.Khanova J, Roth MT, Rodgers JE, McLaughlin JE. Student experiences across multiple flipped classrooms in a single curriculum. Med Educ. 2015;49:1038–1048. doi: 10.1111/medu.12807. [DOI] [PubMed] [Google Scholar]
- 6.McLaughlin JE, Roth MT, Glatt DM, et al. The flipped classroom: a course design to foster learning and engagement in health professions education. Acad Med. 2014;89(2):236–243. doi: 10.1097/ACM.0000000000000086. [DOI] [PubMed] [Google Scholar]
- 7.O’Flaherty J, Phillips C. The use of flipped classrooms in higher education: a scoping review. Internet High Educ. 2015;25:85–95. [Google Scholar]
- 8.Findlay-Thompson S, Mombourquette P. Evaluation of a flipped classroom in an undergraduate business course. Bus Educ Accred. 2014;6(1):63–71. [Google Scholar]
- 9.Freeman S, Eddy SL, McDonough M, et al. Active learning increases student performance in science, engineering, and mathematics. Proc Natl Acad Sci USA. . 2014 doi: 10.1073/pnas.1319030111. ;111(23):8410-8415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kim MK, Kim SM, Khera O, Getman J. The experience of three flipped classrooms in an urban university: an exploration of design principles. Internet High Educ. 2014;22:37–50. [Google Scholar]
- 11.Tune JD, Sturek M, Basile DP. Flipped classroom model improves graduate student performance in cardiovascular, respiratory, and renal physiology. Adv Physiol Educ. 2013;37(4):316–320. doi: 10.1152/advan.00091.2013. [DOI] [PubMed] [Google Scholar]
- 12.Lage MJ, Platt GJ, Treglia M. Inverting the classroom: a gateway to creating an inclusive learning environment. J Econ Educ. 2000;31(1):30–43. [Google Scholar]
- 13.Remington TL, Hershock C, Klein KC, Niemer RK, Bleske BE. Lessons from the trenches: implementing team-based learning across several courses. Curr Pharm Teach Learn. 2015;7(1):121–130. [Google Scholar]
- 14.Roth MT, Mumper RJ, Singleton SF, et al. A renaissance in pharmacy education at the University of North Carolina at Chapel Hill. N C Med J. 2014;75(1):48–52. doi: 10.18043/ncm.75.1.48. [DOI] [PubMed] [Google Scholar]
- 15.Shao X, Hufnagel P, Karp R. The effect of Clarion transitions of student academic performance and retention. J Coll Student Retent. 2010;11(4):435–457. [Google Scholar]
- 16.Berridge EJ, Freeth D, Sharpe J, Roberts CM. Bridging the gap: supporting the transition from medical student to practising doctor–a two-week preparation programme after graduation. Med Teach. 2007;29(2-3):119–127. doi: 10.1080/01421590701310897. [DOI] [PubMed] [Google Scholar]
- 17.Shreiber DI, Moghe PV, Roth CM. Multidisciplinary “boot camp” training in cellular bioengineering to accelerate research immersion for REU participants. Adv Eng Educ. 2015;4(4) [Google Scholar]