Abstract
Food assistance recipients are at higher risk for poor cardiovascular health given their propensity to poor dietary intake and tobacco use. This study sought to evaluate the cardiovascular health status, and determine the impact of a low-intensity smoking cessation education intervention that connected mobile food pantry participants to state quit-smoking resources. A pre-post design with a 6-week follow-up was used to evaluate the impact of a 10–12 min smoking cessation education session implemented in five food pantries in Delaware. Baseline cardiovascular health, smoking behaviors and food security status were assessed. Smoking cessation knowledge, intention to quit and use of the state quit line were also assessed at follow-up. Of the 144 participants 72.3% reported having hypertension, 34.3% had diabetes, 13.9% had had a stroke. 50.0% were current smokers. The low-intensity intervention significantly increased smoking cessation knowledge but not intention to quit at follow-up. Seven percent of current smokers reported calling the quit line. Current tobacco use was five times more likely in food insecure versus food secure adults (OR 4.98; p=0.006), even after adjustment for demographic factors. Systems based approaches to address tobacco use and cardiovascular health in low-income populations are needed. The extent to which smoking cessation could reduce food insecurity and risk for cardiovascular disease in this population warrants investigation.
Keywords: Cardiovascular disease, Smoking cessation, Community intervention, Food insecurity, Systems-approaches
Introduction
Continued tobacco use and poor dietary intake represent two leading, modifiable risk factors for cardiovascular disease that disproportionately affect low-income adults [1–3]. Despite current tobacco use reaching an all-time-low of 16.8% across all populations, low socioeconomic (SES) groups report rates of 30–40% [2]. Smokers of low SES are less likely to have access to, and use, evidence-based treatments for nicotine dependence [4, 5], and are less likely to successfully quit than those of higher income and education [6, 7]. Continued smoking among low-income groups contributes greatly to their increased odds of poor cardiovascular outcomes including stroke [8] and coronary heart disease [9].
Lower income adults are also more likely to have a diet characterized as poor, meaning lower intake of fruits and vegetables, and higher intake of energy-dense foods (i.e., foods higher in fat and sugar) [1]. Similar to smoking, poor dietary intake patterns are a risk factor for cardiovascular diseases [10]. Those who may be at greatest risk for poor dietary intake, and subsequently cardiovascular disease within the low-income population, are food insecure adults and households. Food insecurity is the uncertainty of having, or are unable to acquire enough food to meet the needs of the household members due to insufficient resources [11].
Importantly, these two risk factors for cardiovascular diseases are believed to intersect, such that current smoking is associated with food insecurity [12], even after adjustment for household income [13, 14]. Food insecure populations may represent a particularly vulnerable population for cardiovascular diseases given their propensity for tobacco use and poor dietary intake. However, the cardiovascular health status, quitting behaviors and use of evidence-based treatments among food insecure populations has yet to be elucidated.
To advance this literature, the current pilot-study reports on an academic-community partnership between the University of Delaware and the Food Bank of Delaware formed to: (a) characterize the cardiovascular health status of mobile food pantry users; (b) examine the association between food security and tobacco use; (c) develop and measure the impact of a low-intensity, portable smoking cessation educational intervention on tobacco use knowledge, intention to quit smoking and utilization of the state quit line services. Understanding the relationship of these cardiovascular disease risk factors may contribute to longer-term goal of developing efficacious, low-intensity, systems approaches to improving cardiovascular health in this group.
Methods
Design
The current study used a pre- and post-test design with a 6-week follow-up assessment to examine baseline cardiovascular health status and the impact of a low-intensity group based smoking cessation educational intervention. The intervention was designed to increase knowledge about tobacco use, quitting intentions and behaviors (including calling the state quit line) in mobile food pantry users attending events operated by the Food Bank of Delaware. This study was approved by the Institutional Review Board at the University of Delaware.
Participants
Program participants were recruited through mobile food pantries (n = 5) located in community buildings (e.g., churches, subsidized apartment complexes, resource centers and counseling services centers) in Delaware. To qualify for the mobile food pantry services, participants are required to be at least 18 years of age, provide proof of residency in Delaware (i.e., drivers license), be a current recipient of federal benefits (e.g., SNAP, WIC) and have a household income that is up to 185% of current poverty guidelines (e.g., $44,955 or less for a family of four in 2016). All participants using mobile food pantries between April and May of 2016 were invited to enroll in the current program. No additional eligibility criteria were used. 144 adults enrolled, provided written informed consent and completed the intervention.
Intervention
On arrival to the mobile food pantry, participants registered and were escorted into a large gathering room. A trained research assistant completed group informed consent procedures and participants completed a pre-test. A low-intensity (10–12 min) intervention was designed in partnership with the Food Bank of Delaware to increase knowledge about the harmful effects of cigarette smoking and second-hand-smoke, the physical and learned habit components of nicotine dependence, effective strategies for quitting smoking including pharmacotherapy and counseling, and the availability of the Delaware quit line [15]. A PowerPoint displayed key information visually, while a trained research assistant verbally shared information using a dynamic, question and answer format, to promote participant engagement and interaction. At the conclusion of the presentation, participants were provided with a state quit line handout and asked to complete a post-test evaluating the participant’s smoking cessation knowledge and quitting intention. The same evaluation was conducted by phone 6-weeks later, and in addition participants were asked to report if they had called the quit line.
Measures
All measures were collect at baseline, post-intervention and follow-up (6 weeks following post intervention) unless otherwise noted.
Demographics
Socio-demographic variables assessed were age, sex (male/female), race (coded as African American, White, Other), and education level (less than high-school, high school graduate or attended/graduated college) at baseline only.
Cardiovascular Health
Participants were asked to self-report whether they had ever been diagnosed by a healthcare provider as having coronary heart disease, a heart attack, heart failure, a stroke, vascular disease, and/or congenital heart disease, diabetes and/or high blood pressure (yes/no/don’t know). Overall health status was also assessed on a 5-point response scale (excellent, very good, good, fair and poor) by a single item: “In general, how good would you say your health is”?
Tobacco Behaviors
Tobacco use behaviors were assessed using four questions (1) Have you smoked a cigarette (even one puff) in the last 30-days? (yes/no); (2) How soon after you wake up do you have your first cigarette? (within 5, 6–30, 31–60 min, after 60-min) [16]; and (3) How many cigarettes per day do you smoke? [17].
Food Insecurity
Food security was measured using a two item scale: (1) Within the past 12 months we worried whether our food would run out before we got money to buy more; and, (2) Within the past 12 months the food we bought just didn’t last and we didn’t have money to get more. Participants responded to these items on a three-point response scale: often true, sometimes true, and never true [18].
Smoking Cessation Knowledge
Smoking cessation knowledge was measured using seven true/false questions that related specifically to the intervention content (e.g., Smoking can be harmful to non-smokers who live with smokers because of second-hand smoke). A total score corresponding to the number of correct answers (0–7) were generated and used for analysis.
Intention to Quit
Intention to quit was measured using a single item that asked participants to rate on a scale of 0 (not likely) to 10 (very likely) how likely they were to make a serious attempt to quit smoking in the next month [19]. At the 6-week follow up, participants were also asked whether they had actually called the state quit line in the past month (yes/no).
Statistical Analysis
Descriptive statistics, including mean and standard deviations for continuous variables and sample size (N) and frequencies (%) for categorical variables, were generated for all program variables. Chi square test of independence was generated to examine the association between tobacco use and food security. Paired t-tests were used to examine changes in the study outcomes across study time points (pre- vs. post-test, pre versus 6-week follow-up). Logistic regression modeling was used to examine the independent association between food security and tobacco use. Only cases with complete data were used in the bivariate analysis. All analyses were conducted using SPSS (version 24.0).
Results
Participant Characteristics
The mean age of participants (N = 144) was 62.8 years (SD 15.8). Of the total sample, 69.4% were female and 52.7% self-reported being African American. Approximately one-third (35.6%) had less than a high school education and 78.4% were on disability or retired. Almost three-quarters of the sample (72.3%) reported having hypertension, 34.3% had diabetes, and 13.9% ever had a stroke. Half of the sample (50.0%) were current smokers, with 48.3% reporting high nicotine dependence (smoked their first cigarette within 5 min of waking in the morning). The majority (46.0%) reported moderate food insecurity and 31.5% reported severe food insecurity (see Table 1).
Table 1.
Participant baseline characteristics
| M (SD) or n (%) (N = 144) | |
|---|---|
| Demographic variables | |
| Age | 62.8 (15.2) |
| Sex | |
| Male | 44 (30.6) |
| Female | 100 (69.4) |
| Race | |
| African American | 69 (52.7) |
| White | 56 (42.7) |
| Other | 6 (4.6) |
| Education | |
| Less than high school | 48 (35.6) |
| High school graduate | 60 (44.4) |
| Attended college | 27 (20.0) |
| Employment | |
| Not employed | 20 (14.4) |
| On disability/retired | 109 (78.4) |
| Employed part or full time | 10 (7.2) |
| Health status variables | |
| Food security status | |
| Severe insecure | 39 (31.5) |
| Moderate food insecure | 57 (46.0) |
| Food secure | 28 (22.6) |
| Perceived health status | |
| Poor/fair | 58 (42.0) |
| Good | 52 (37.7) |
| Very good/excellent | 28 (20.3) |
| Diagnosed health condition | |
| Diabetes (yes) | 46 (34.3) |
| Coronary heart disease (yes) | 15 (11.8) |
| Heart attack (yes) | 10 (8.0) |
| Heart failure (yes) | 6 (4.9) |
| Stroke (yes) | 17 (13.9) |
| Vascular disease (yes) | 11 (8.9) |
| Congenital heart failure (yes) | 2 (1.8) |
| Hypertension (yes) | 47 (72.3) |
| Tobacco use variables | N = 64 |
| Current smoker (N, % yes) | 64 (50.0 of entire sample) |
| High nicotine dependence (first cigarette within 5 min) | 28 (48.3 of smokers) |
| Serious quit attempt (% yes) | 40 (60.6 of smokers) |
| Called state quitline (assessed at follow-up) | 4 (8.0 of smokers) |
Association between Tobacco Use and Food Insecurity
Tobacco use was significantly more prevalent among participants who were food insecure as compared to food secure with 42.4% who reported severe food insecurity, 47.5% of smokers reporting moderate food insecurity, and 10.2% of smokers reporting being food secure (X2 = 12.34; p = 0.002; see Fig. 1). In a post-hoc multivariable binary regression model of current tobacco use, food insecure adults (moderate and severe) had a five-fold greater odds of reporting current smoking, even when race, employment, gender and education were adjusted (OR 4.98; p=0.006; Table 2).
Fig. 1.
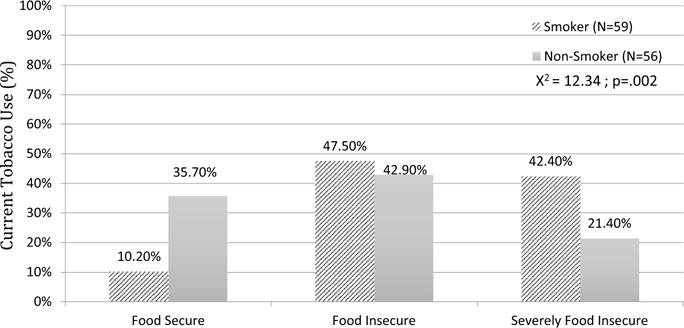
Association between current tobacco use and food security at baseline (%)
Table 2.
Regression model to show association between food insecurity and current tobacco use
| B | SE | Exp(B) | P | |
|---|---|---|---|---|
| Food insecurity (moderate and severe) | 1.61 | 0.58 | 4.98 | 0.006 |
| Education attainment | −0.36 | 0.31 | 0.70 | 0.24 |
| Job status | −0.21 | 0.43 | 0.81 | 0.62 |
| Race | −0.09 | 0.38 | 0.92 | 0.82 |
| Gender | −0.21 | 0.48 | 0.81 | 0.66 |
Impact of Intervention on Tobacco Use Knowledge and Intention to Quit
Participants’ knowledge about tobacco use and quitting based on a range of 0 (no knowledge) to 7 (complete knowledge) significantly increased between the pre- (M = 5.26; SD 1.4) and post-tests (M = 5.68; SD 1.4; t=2.340, p = 0.024) (Figs. 1, 2a) and between the pre-test (M = 5.33; SD 1.7) and the 6-week follow-up (M = 6.19, SD 0.81; t = 2.06, p = 0.052) (Fig. 2b).
Fig. 2.
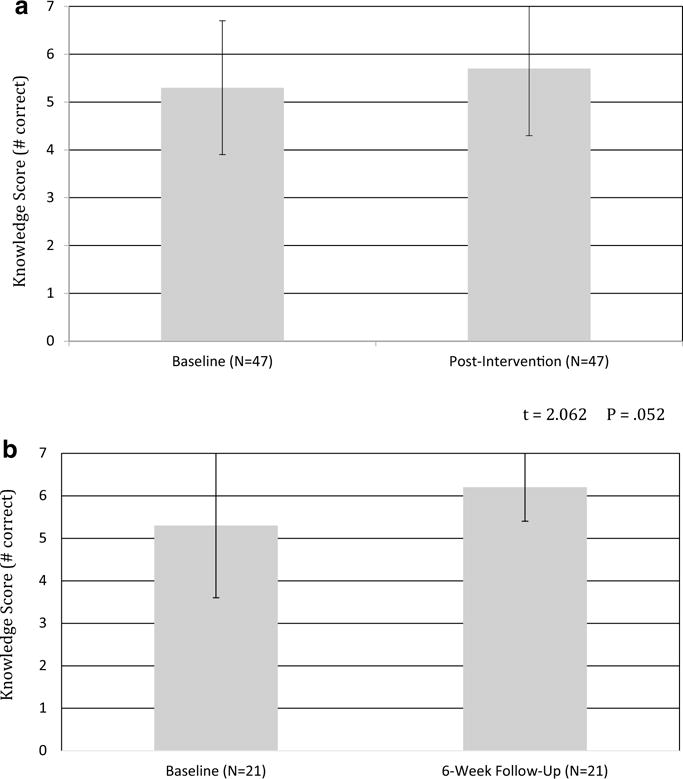
a Mean tobacco knowledge score at baseline and post intervention for smokers only (error bars represent ±1 standard deviation). b Mean tobacco knowledge score at baseline and 6-week follow-up for smokers only (error bars represent ±1 standard deviation)
Reported intention to quit on a range of 0 (not likely) to 10 (very likely), showed a non-significant increase between pre- (M=4.8; SD 3.6) and post-assessment (M = 4.9; SD 3.8; t = 0.328, p = 0.744) and between the pre-assessment (M = 4.2; SD 3.5) and the 6-week follow-up (M = 5.1, SD 3.4; t = 1.709, p = 0.100). At the 6-week follow-up 7.4% of smokers reported calling the state quit line in the last month.
Discussion
Cardiovascular disease continues to be a pervasive public health problem that disproportionately affects lower income adults [20, 21]. The findings from this study demonstrate that cardiovascular health is poor, exceeding national rates.
These data also showed that as a leading cardiovascular risk factor, current tobacco use was more prevalent in food insecure as compared to food secure adults, even after adjustment for socio-demographic factors. The low intensity educational intervention had limited impact on intention to quit and utilization of the prescribed state quit line for cessation, but knowledge did increase as hypothesized. Together these findings highlight that adults using food pantries are at an increased risk for cardiovascular disease and a more intensive intervention may be needed to increase intention to quit and connect this group with formal, evidence-based cessation programs. These data also suggest that the co-occurrence of tobacco use and food insecurity present a unique opportunity to impact food insecurity through smoking cessation or reduction.
The impact of the current low-intensity intervention on intention to quit and utilization of state quit line services was negligible. Although state quit line services have been shown to increase the odds of quitting by 60% in the general population [15], <10% of smokers who are trying to quit and are aware of quit lines, are actually using them [22]. Non-utilizers of the state quit line have been identified as those who do not have a land-line telephone, have lapses in cell phone service, and report skepticism of quit line efficacy [23]. The lack of impact of the current brief smoking cessation education program on intention to quit and quit line uptake could be attributed to the intensity of the intervention. A more intense smoking cessation session delivered directly to the self-identified smokers in the food pantry setting, that incorporate behavior change strategies and more information about the efficacy of the state quit line, may have had greater impact.
The cardiovascular disease profile of this mobile food pantry population presents much basis for concern. As stated, almost three-quarters (72%) reported being hypertensive, 34% had diabetes, 14% had a history of stroke and 12% had coronary heart disease. These rates supersede those at the national level where approximately one-third are hypertensive [24], 9.3% are diabetic [25], age adjusted prevalence of stroke was 2.7% [26], and the age adjusted prevalence of coronary heart disease was 6% [27]. In terms of cardiovascular risk behaviors, a full 50% of the sample reported being current smokers, a rate that is almost triple the national level of 16.8% [2]. That 77% of the sample reported some degree of food insecurity is not surprising given the program location at a mobile food pantry site. These cardiovascular health status data help refine food pantry recipients as a high-risk group for poor cardiovascular health.
Food insecure participants (moderate and severe) had a full five-fold greater odds of being current smokers as compared to food secure adults, even after adjustment for other socio-demographic factors (race, education, job status, gender). This result converges with a small body of work [13, 14], and advances the literature by suggesting that there may be mechanisms, other than socio-demographic factors, that make food insecure populations more vulnerable to tobacco use. Specifically, there may be shared genetic [28–30], psychosocial [31] and/or environmental factors [32–34] that may serve to perpetuate current tobacco use and poor dietary intake in low-income adults; this association may be particularly potent in food insecure adults. Further work is needed to explore the mechanisms linking tobacco use to food insecure versus secure adults.
Although the current study is one of the first to evaluate a low-intensity smoking cessation program delivered to food pantry recipients, the data presented should be considered in terms of their vulnerability to bias. Specifically, the five food pantries sampled for this program were based on convenience sampling and may not be representative of food pantry recipients in general. Relatedly, all data are self-report, and so may be subject to bias. Another limitation of the current program was the non-significant impact on the behavioral target of utilization of the state quit line; a more intensive intervention may be necessary.
Despite these limitations, the current data have several public health implications. First, the poor cardiovascular health status of this population highlights the necessity for intervention. This is underscored by the limited impact of the current low-intensity intervention on promoting use of the state quit line. Second, that food insecurity had such a strong independent relationship with current smoking presents a hypothesis that smoking cessation, or even reduction, may ameliorate food insecurity. Future work to examine the effects of smoking cessation on household food insecurity, dietary patterns, and the effects on cardiovascular health, warrants further study. The premise that smoking cessation or even reduction in food insecure adults could positively impact another potent risk factor for cardiovascular disease (i.e., food insecurity and poor dietary intake) holds much potential for transforming the cardiovascular health profile of this high-risk group.
Acknowledgments
The authors wish to thank Kai Inguito and Christina Brown for their assistance with data collection. They would also like to thank the staff at the Windsor Apartments, Brandywine Center for Counseling Services, Chelton Apartments, A.C.E. Peer Resource Center, and the Calvary Assembly of God Church for their cooperation in providing a venue for study implementation. Karen Murphy and Danielle Zack are acknowledged for their administrative support to this project.
Funding Funding for this study was provided by the American Lung Association to the Food Bank of Delaware. Research reported in this publication was also supported by an Institutional Development Award (IDeA) Center of Biomedical Research Excellence from the National Institute of General Medical Sciences of the National Institutes of Health under Grant No. P20GM113125 (FP).
Footnotes
Compliance with Ethical Standards
Conflict of interest The authors have no conflicts of interest to disclose.
Institutional Review Board The Institutional Review Board at the University of Delaware approved this study.
Informed Consent Written informed consent was obtained for all study participants.
References
- 1.Mello JA, Gans KM, Risica PM, Kirtania U, Strolla LO, Fournier L. How is food insecurity associated with dietary behaviors? An analysis with low-income, ethnically diverse participants in a nutrition intervention study. Journal of the American Dietetic Association. 2010;110(12):1906–1911. doi: 10.1016/j.jada.2010.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jamal A, Homa DM, O’Connor E, et al. Current Cigarette Smoking Among Adults—United States, 2005–2014. MMWR Morbidity and Mortality Weekly Report. 2015;64(44):1233–1240. doi: 10.15585/mmwr.mm6444a2. [DOI] [PubMed] [Google Scholar]
- 3.Lloyd-Jones DM, Hong Y, Labarthe D, et al. Defining and setting national goals for cardiovascular health promotion and disease reduction: The American Heart Association’s strategic Impact Goal through 2020 and beyond. Circulation. 2010;121(4):586–613. doi: 10.1161/CIRCULATIONAHA.109.192703. [DOI] [PubMed] [Google Scholar]
- 4.Burns EK, Deaton EA, Levinson AH. Rates and reasons: Disparities in low intentions to use a state smoking cessation quitline. American Journal of Health Promotion: AJHP. 2011;25(5 Suppl):59–65. doi: 10.4278/ajhp.100611-QUAN-183. [DOI] [PubMed] [Google Scholar]
- 5.Sheffer CE, Stitzer M, Landes R, Brackman SL, Munn T, Moore P. Socioeconomic disparities in community-based treatment of tobacco dependence. American Journal of Public Health. 2012;102(3):e8–e16. doi: 10.2105/AJPH.2011.300519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Reid JL, Hammond D, Boudreau C, Fong GT, Siahpush M, Collaboration ITC Socioeconomic disparities in quit intentions, quit attempts, and smoking abstinence among smokers in four western countries: Findings from the International Tobacco Control Four Country Survey. Nicotine & Tobacco Research. 2010;12(Suppl):S20–S33. doi: 10.1093/ntr/ntq051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fagan P, Shavers VL, Lawrence D, Gibson JT, O’Connell ME. Employment characteristics and socioeconomic factors associated with disparities in smoking abstinence and former smoking among U.S. workers. Journal of Health Care for the Poor and Underserved. 2007;18(4 Suppl):52–72. doi: 10.1353/hpu.2007.0119. [DOI] [PubMed] [Google Scholar]
- 8.Addo J, Ayerbe L, Mohan KM, et al. Socioeconomic status and stroke: An updated review. Stroke; A Journal of Cerebral Circulation. 2012;43(4):1186–1191. doi: 10.1161/STROKEAHA.111.639732. [DOI] [PubMed] [Google Scholar]
- 9.Gebreab SY, Diez Roux AV, Brenner AB, et al. The impact of lifecourse socioeconomic position on cardiovascular disease events in African Americans: The Jackson Heart Study. Journal of the American Heart Association. 2015;4(6):e001553. doi: 10.1161/JAHA.114.001553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hu FB, Rimm EB, Stampfer MJ, Ascherio A, Spiegelman D, Willett WC. Prospective study of major dietary patterns and risk of coronary heart disease in men. The American Journal of Clinical Nutrition. 2000;72(4):912–921. doi: 10.1093/ajcn/72.4.912. [DOI] [PubMed] [Google Scholar]
- 11.USDA. Food Security Status of US Households in 2014. 2015 http://www.ers.usda.gov/topics/food-nutrition-assistance/food-security-in-the-us/key-statistics-graphics.aspx-foodsecure. Accessed 5 Sept 2016.
- 12.Armour BS, Pitts MM, Lee CW. Cigarette smoking and food insecurity among low-income families in the United States, 2001. American Journal of Health Promotion: AJHP. 2008;22(6):386–392. doi: 10.4278/ajhp.22.6.386. [DOI] [PubMed] [Google Scholar]
- 13.Cutler-Triggs C, Fryer GE, Miyoshi TJ, Weitzman M. Increased rates and severity of child and adult food insecurity in households with adult smokers. Archives of Pediatrics and Adolescent Medicine. 2008;162(11):1056–1062. doi: 10.1001/archpediatrics.2008.2. [DOI] [PubMed] [Google Scholar]
- 14.Iglesias-Rios L, Bromberg JE, Moser RP, Augustson EM. Food insecurity, cigarette smoking, and acculturation among Latinos: Data from NHANES 1999–2008. Journal of Immigrant and Minority Health/Center for Minority Public Health. 2015;17(2):349–357. doi: 10.1007/s10903-013-9957-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fiore M, Jaén C, Baker T. Treating Tobacco Use and Dependence: 2008 Update Clinical Practice Guideline. Rockville, MD: Department of Health and Human Services; 2008. [Google Scholar]
- 16.Heatherton TF, Kozlowski LT, Frecker RC, Fagerstrom KO. The Fagerstrom Test for Nicotine Dependence: A revision of the Fagerstrom Tolerance Questionnaire. British Journal of Addiction. 1991;86(9):1119–1127. doi: 10.1111/j.1360-0443.1991.tb01879.x. [DOI] [PubMed] [Google Scholar]
- 17.Centers for Disease C Prevention. Brener ND, et al. Methodology of the youth risk behavior surveillance system-2013. MMWR Recomm Rep. 2013;62(RR-1):1–20. [PubMed] [Google Scholar]
- 18.Hager ER, Quigg AM, Black MM, et al. Development and validity of a 2-item screen to identify families at risk for food insecurity. Pediatrics. 2010;126(1):e26–e32. doi: 10.1542/peds.2009-3146. [DOI] [PubMed] [Google Scholar]
- 19.Biener L, Abrams DB. The Contemplation Ladder: Validation of a measure of readiness to consider smoking cessation. Health Psychology: Official Journal of the Division of Health Psychology, American Psychological Association. 1991;10(5):360–365. doi: 10.1037//0278-6133.10.5.360. [DOI] [PubMed] [Google Scholar]
- 20.Johnson NB, Hayes LD, Brown K, et al. CDC National Health Report: Leading causes of morbidity and mortality and associated behavioral risk and protective factorsUnited States, 2005–2013. MMWR Suppl. 2014;63(4):3–27. [PubMed] [Google Scholar]
- 21.Writing Group M, Mozaffarian D, Benjamin EJ, et al. Executive Summary: Heart Disease and Stroke Statistics-2016 Update: A Report From the American Heart Association. Circulation. 2016;133(4):447–454. doi: 10.1161/CIR.0000000000000366. [DOI] [PubMed] [Google Scholar]
- 22.Schauer GL, Malarcher AM, Zhang L, Engstrom MC, Zhu SH. Prevalence and correlates of quitline awareness and utilization in the United States: An update from the 2009–2010 National Adult Tobacco Survey. Nicotine & Tobacco Research: Official Journal of the Society for Research on Nicotine and Tobacco. 2014;16(5):544–553. doi: 10.1093/ntr/ntt181. [DOI] [PubMed] [Google Scholar]
- 23.Griffin JL, Segal KS, Nahvi S. Barriers to telephone quitline use among methadone-maintained smokers. Nicotine & Tobacco Research: Official Journal of the Society for Research on Nicotine and Tobacco. 2015;17(8):931–936. doi: 10.1093/ntr/ntu267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nwankwo T, Yoon SS, Burt V, Gu Q. Hypertension among adults in the United States: National Health and Nutrition Examination Survey, 2011–2012. NCHS Data Brief. 2013;(133):1–8. [PubMed] [Google Scholar]
- 25.Prevention CfDCa. National Diabetes Statistics Report: Estimates of Diabetes and Its Burden in the United States, 2014. Atlanta, GA: Department of Health and Human Services; 2014. [Google Scholar]
- 26.Centers for Disease C Prevention. Prevalence of stroke- United States, 2006–2010. MMWR Morbidity and Mortality Weekly Report. 2012;61(20):379–382. [PubMed] [Google Scholar]
- 27.Centers for Disease C Prevention. Prevalence of coronary heart disease-United States, 2006–2010. MMWR Morbidity and Mortality Weekly Report. 2011;60(40):1377–1381. [PubMed] [Google Scholar]
- 28.Comings DE, Blum K. Reward deficiency syndrome: Genetic aspects of behavioral disorders. Progress in Brain Research. 2000;126:325–341. doi: 10.1016/S0079-6123(00)26022-6. [DOI] [PubMed] [Google Scholar]
- 29.Verhagen M, Kleinjan M, Engels RC. A systematic review of the A118G (Asn40Asp) variant of OPRM1 in relation to smoking initiation, nicotine dependence and smoking cessation. Pharmacogenomics. 2012;13(8):917–933. doi: 10.2217/pgs.12.76. [DOI] [PubMed] [Google Scholar]
- 30.Hoebel BG. Brain neurotransmitters in food and drug reward. The American Journal of Clinical Nutrition. 1985;42(5 Suppl):1133–1150. doi: 10.1093/ajcn/42.5.1133. [DOI] [PubMed] [Google Scholar]
- 31.Anderson P, Butcher K, Hoynes H, Schanzenbach D. Beyond Income: What else predicts very low foo dsecurity among children? Kentucky, USA: University of Kentucky Center for Poverty Research; (Discussion Paper Series 2014). Contract No.: DP2014-06. [Google Scholar]
- 32.Bryant J, Bonevski B, Paul C. A survey of smoking prevalence and interest in quitting among social and community service organisation clients in Australia: A unique opportunity for reaching the disadvantaged. BMC Public Health. 2011;11:827. doi: 10.1186/1471-2458-11-827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Patterson F, Zaslav DS, Kolman-Taddeo D, et al. Smoking cessation in pulmonary care subjects: A mixed methods analysis of treatment-seeking participation and preferences. Respiratory Care. 2016 doi: 10.4187/respcare.04958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Edin K, Boyd M, Mabli J, et al. SNAP food security in-depth interview study. Alexandria, VA: U.S. Department of Agriculture, Food and Nutrition Service; 2013. [Google Scholar]


