Abstract
Background
Invasive fungal infections are a major cause of morbidity and mortality among solid organ transplant (SOT) and hematopoietic cell transplant (HCT) recipients, but few data have been reported on the epidemiology of endemic fungal infections in these populations.
Methods
Fifteen institutions belonging to the Transplant-Associated Infection Surveillance Network prospectively enrolled SOT and HCT recipients with histoplasmosis, blastomycosis, or coccidioidomycosis occurring between March 2001 and March 2006.
Results
A total of 70 patients (64 SOT recipients and 6 HCT recipients) had infection with an endemic mycosis, including 52 with histoplasmosis, 9 with blastomycosis, and 9 with coccidioidomycosis. The 12-month cumulative incidence rate among SOT recipients for histoplasmosis was 0.102%. Occurrence of infection was bimodal; 28 (40%) infections occurred in the first 6 months post transplantation, and 24 (34%) occurred between 2 and 11 years post transplantation. Three patients were documented to have acquired infection from the donor organ. Seven SOT recipients with histoplasmosis and 3 with coccidioidomycosis died (16%); no HCT recipient died.
Conclusions
This 5-year multicenter prospective surveillance study found that endemic mycoses occur uncommonly in SOT and HCT recipients, and that the period at risk extends for years after transplantation.
Keywords: solid organ transplant, hematopoietic cell transplant, histoplasmosis, blastomycosis, coccidioidomycosis
Histoplasma capsulatum, Blastomyces dermatitidis, and Coccidioides species are endemic fungi in the United States, and each genus is uniquely associated with human disease within a relatively restricted geographic location. Histoplasmosis occurs predominantly in the Ohio and Mississippi River valleys; blastomycosis in the upper Midwest, the Great Lakes region, and south central states; and coccidioidomycosis in the southwest. The endemic fungi often cause infection following inhalation of conidia that exist primarily in soil. Invasive infections are seen in immunosuppressed patients, particularly those with human immunodeficiency virus/acquired immunodeficiency syndrome (AIDS) or those receiving tumor necrosis factor antagonists. Recipients of solid organ transplant (SOT) or hematopoietic cell transplant (HCT) appear to acquire infection caused by endemic fungi less commonly than reported for those immunosuppressive conditions noted above (1). However, surveillance for endemic fungal infections among transplant recipients has not been performed systematically and thus, the incidence and distribution of endemic fungal infections among the transplant population is not known.
The Transplant-Associated Infection Surveillance Network (TRANSNET) was established in 2001 to perform prospective surveillance for invasive fungal infections (IFIs) among all transplant recipients at 23 selected centers throughout the United States between 2001 and 2006. The goals were to establish the burden of IFIs in the transplant population, to define the current approach to diagnosis and treatment, and to describe the outcomes of these infections. Overall incidence rates for IFIs have been reported among the SOT and HCT populations enrolled in TRANSNET (2-4). In this report, we focus on endemic fungal infections that occurred in this cohort. We sought to better define the timing of occurrence of infection post transplantation, the clinical characteristics of the population, treatment, and outcomes of histoplasmosis, blastomycosis, and coccidioidomycosis in SOT and HCT recipients.
Methods
Study sites
Fifteen of the 23 TRANSNET sites provided prospective surveillance data for endemic mycoses in SOT and HCT recipients from March 2001 through March 2006. The Surveillance Cohort comprised SOT and HCT recipients who developed an infection with an endemic mycosis during this period, regardless of when or where their transplant occurred. The Incidence Cohort comprised patients who underwent transplantation during the surveillance period at 1 of the 15 study sites. Data collected on all patients in the Incidence Cohort included demographics (age, gender, race/ethnicity), type of transplant, date of last follow-up, and outcome.
Definitions and case identification
Endemic fungal infections were identified prospectively through review of monthly logs of transplant recipients, culture data, serodiagnostic studies, and histopathology results, and by regular contact with transplant physicians and coordinators. Case data included demographics, date and type of transplant, infection type and site, method of diagnosis, co-morbid conditions, past or current infections, recent immunosuppressive treatment, rejection episodes, graft-versus-host disease (GVHD), antifungal treatment, and status 3 months after initial diagnosis of infection. Among those patients who died, the investigator determined whether death was likely due to the endemic mycosis or to another cause, and these determinations were reviewed by the Data Review Committee.
The diagnosis of histoplasmosis, blastomycosis, or coccidioidomycosis was established by growth of the organism in culture, a positive Histoplasma serum or urine antigen test in a patient who had a compatible clinical illness, or histopathologic identification of the typical yeast forms of H. capsulatum and B. dermatitidis or spherules typical of Coccidioides species. Cases were categorized as pulmonary infection when the only organ noted to be involved was the lungs; the presence of antigenemia or antigenuria did not change this categorization. Disseminated infection was manifested by evidence of non-pulmonary involvement by histopathology or culture, radiographic imaging, or antigenemia or antigenuria with no pulmonary infiltrates on imaging; only 2 patients had antigenemia or antigenuria alone as the only criterion for disseminated infection. The category of pulmonary infection with dissemination designated patients in whom infection was documented in both lungs and an extra-pulmonary site, irrespective of antigenemia or antigenuria. All cases were reviewed by the Data Review Committee to determine individual case validity.
Data analysis
Data entry and verification were performed by the Biostatistical Unit at the University of Alabama at Birmingham. Final data cleaning and data analysis were performed at the Centers for Disease Control and Prevention in Atlanta. The descriptive analysis of endemic fungal infections reflects infections occurring during the study period, independent of when or where the transplant occurred (Surveillance Cohort).
Data from the Incidence Cohort were pooled to calculate cumulative incidence curves. Cumulative incidence estimates for transplant-related infections within the first 12 months after transplant were estimated, accounting for the competing risks of infection-free death, re-transplantation, and return to chronic dialysis for renal transplant recipients. Because only a few patients had blastomycosis and coccidioidomycosis and very few HCT recipients were reported with an endemic fungal infection, the cumulative incidence was calculated only for histoplasmosis among SOT recipients.
Results
Demographic characteristics (Surveillance Cohort)
A total of 70 endemic fungal infections were reported in the Surveillance Cohort between 2001 and 2006. The mean age at diagnosis was 52 years (range 12–68), 64% were male, and the majority was Caucasian (Table 1). Of these 70 cases, 64 (91%) occurred in SOT recipients; this includes 48 cases of histoplasmosis, 9 of blastomycosis, and 7 of coccidioidomycosis. Kidney transplant recipients, including 7 who received a kidney-pancreas transplant, accounted for 40 of these 64 cases (62.5%), and liver transplant recipients accounted for an additional 24% of cases (Table 1). The distribution of infections by transplant type reflects the frequency of the types of organs transplanted.
Table 1.
Demographic characteristics of hematopoietic cell and solid organ transplant (SOT) recipients who developed endemic fungal infections
| Number (%)
|
||||
|---|---|---|---|---|
| Characteristic
|
Blastomycosis (N = 9)
|
Coccidioidomycosis (N = 9)
|
Histoplasmosis (N = 52)
|
Total (N = 70)
|
| Hematopoietic cell | 0 | 2 (22) | 4 (8) | 6 (9) |
| Autologous | 0 | 1 (11) | 3 (6) | 4 (6) |
| Allogeneic | 0 | 1 (11) | 1 (2) | 2 (3) |
| Solid organ1 | 9 (100) | 7 (78) | 48 (92) | 64 (91) |
| Heart | 1 (11) | 0 (0) | 2 (4) | 3 (4) |
| Kidney | 5 (56) | 4 (57) | 24 (50) | 33 (47) |
| Kidney-pancreas | 0 (0) | 0 (0) | 7 (15) | 7 (10) |
| Liver | 2 (22) | 3 (43) | 12 (25) | 17 (24) |
| Lung | 0 | 0 | 3 (6) | 3 (4) |
| Pancreas | 1 (11) | 0 | 0 | 1 (2) |
| Age, median (range) | 57 (38–68) | 55 (24–64) | 51 (12–68) | 52 (12–68) |
| Female | 3 (33) | 1 (11) | 21 (40) | 25 (36) |
| Male | 6 (67) | 8 (89) | 31 (60) | 45 (64) |
| Caucasian | 8 (89) | 7 (78) | 43 (83) | 58 (83) |
| African American | 0 | 1 (11) | 7 (13) | 8 (11) |
| Other2 | 1 (11) | 1 (11) | 2 (4) | 4 (6) |
Total SOT performed in the Incidence Cohort: kidney = 8672; kidney-pancreas = 746; liver = 4468; lung = 1195; pancreas = 464; heart = 1165; small bowel = 95.
Hispanic (2), Native American (1), Asian Pacific Islander (1).
HCT recipients accounted for only 9% of cases of endemic fungal infections. Six infections (4 histoplasmosis and 2 coccidioidomycosis) occurred in HCT recipients. Four patients (2 with multiple myeloma, 1 with leukemia, and 1 with medulloblastoma) had each received an autologous HCT, and 2 patients (1 each with lymphoma and leukemia) had received an allogeneic HCT.
Geographic distribution of infections with endemic mycoses
The distribution of cases from the 15 reporting centers is shown in Figure 1. Seven cases of histoplasmosis reported from Iowa were also included in a previous report (5). Notably, 1 case of histoplasmosis and 6 cases of coccidioidomycosis were reported from centers located outside of the areas considered endemic for these fungi. The patient who had histoplasmosis and 3 of the patients who developed coccidioidomycosis were known to have previously resided in or visited areas known to be endemic for these fungi. Two other patients from outside the endemic area appear to have acquired coccidioidomycosis as a result of transmission from transplanted organs, both of which came from the same donor, who had a prior history of coccidioidomycosis (6).
Fig. 1.
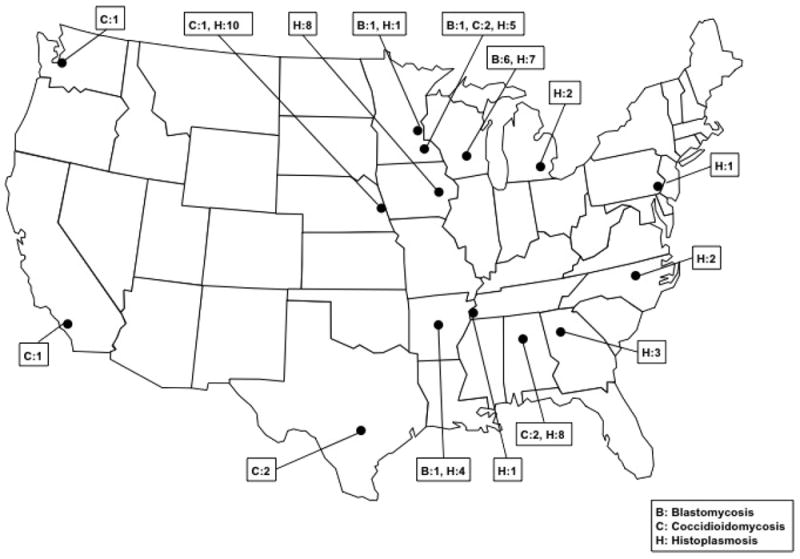
Geographic distribution of cases of histoplasmosis, blastomycosis, and coccidioidomycosis reported from 15 transplant centers in the TRANSNET network.
Rate of infection with endemic mycoses (Incidence Cohort)
A total of 36 endemic fungal infections occurred in patients who had received their transplant during the study period (Incidence Cohort). Three infections, all histoplasmosis, occurred among 16,200 patients (0.02%) who had received an HCT between March 2001 and September 2005. Among the 16,806 patients who had received an SOT in the same time period, 33 (0.2%) developed an endemic mycosis. Among these 33 patients, 23 developed infection caused by H. capsulatum, 6 by Coccidioides species, and 4 by B. dermatitidis. The 12-month cumulative incidence rate among SOT recipients for histoplasmosis, the most common infection, was 0.102% (Fig. 2).
Fig. 2.
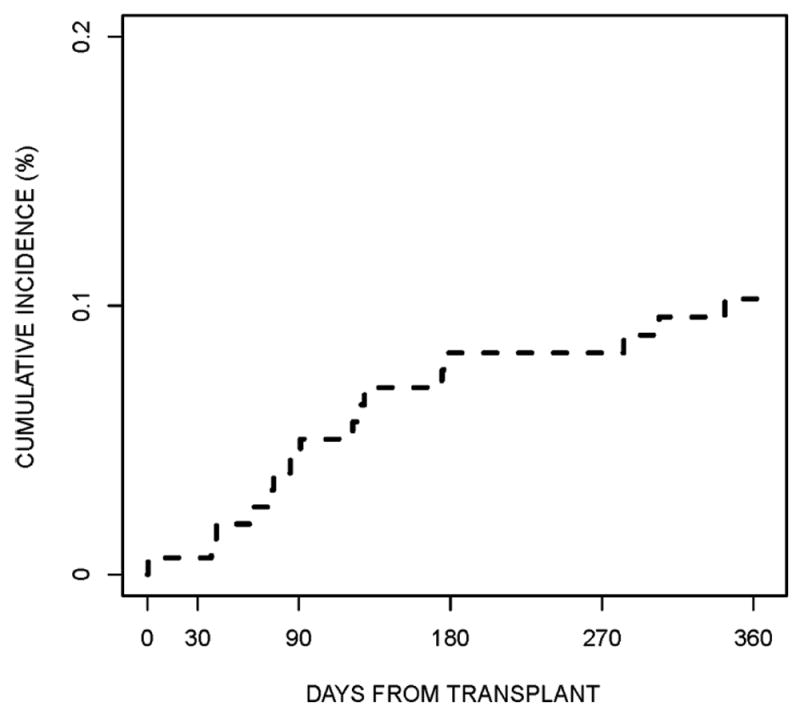
The 12-month cumulative incidence rate for histoplasmosis among solid ogan transplant recipients in the Incidence Cohort.
Time to infection post transplantation
For all 70 patients, the median time from transplantation to diagnosis of an endemic fungal infection was 274 days (range 15–3371) for HCT recipients and 343 days (range 0–4195) for SOT recipients. Figure 3 shows a box and whisker graph with the time to infection for each organism. Twenty-eight patients (40%) developed infection within 6 months post transplantation; of the remaining 42 patients, 18 developed infection within 2 years post transplantation and 24 patients experienced infection between 2 and 11 years post transplantation.
Fig. 3.
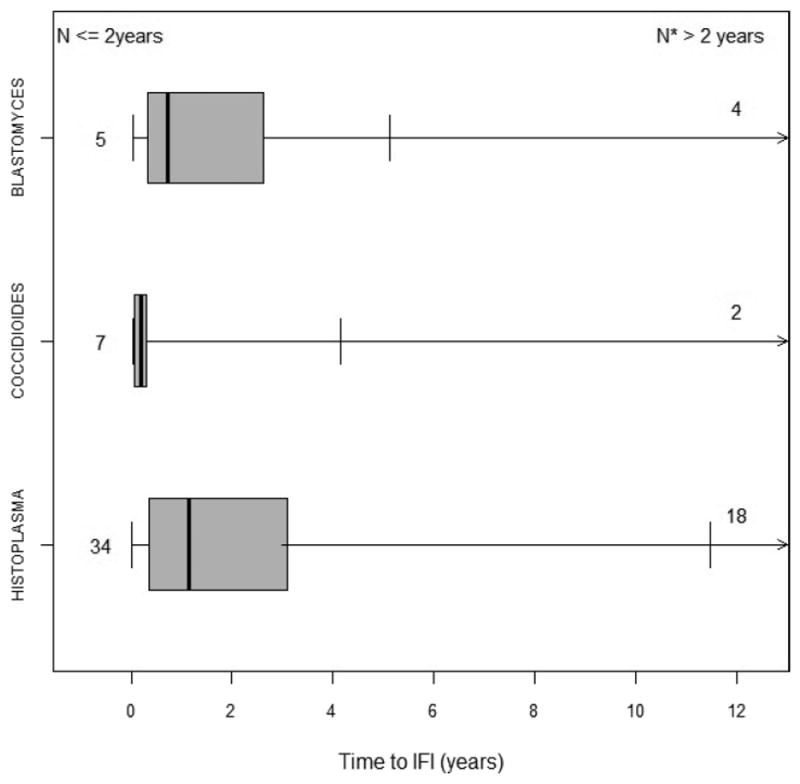
Box and whisker graph indicating time in years to the diagnosis of an endemic mycosis among SOT and HCT recipients in the Surveillance Cohort. The box represents the interquartile range (25–75%). The total number of infections occurring ≤2 years post transplantation is listed in the left-hand column, and the total number of infections occurring >2 years post transplantation is listed in the right-hand column. The median time to the diagnosis of each infection is indicated by the dark vertical line within the box, and the thin vertical lines indicate the range. SOT, solid organ transplant; HCT, hematopoietic cell transplant; IFI, invasive fungal infection.
One HCT recipient, who received an autologous HCT, was diagnosed with disseminated histoplasmosis at day 15 post transplant, but the others developed an endemic fungal infection from 60 days to 9 years after receiving a HCT.
Among 7 SOT recipients who developed infection within 30 days of transplantation, 3 definitely were thought to have acquired the organism via the transplanted organ. Histological evidence of existing Coccidioides infection was found post mortem in the donor of a liver and a kidney that were transplanted into 2 separate recipients, neither of whom had ever visited the endemic area. Both died of disseminated coccidioidomycosis within 3 weeks of transplantation (6). The third patient, in whom a biopsy of the donor liver found typical yeast forms of H. capsulatum, was begun immediately on therapy and never developed symptomatic infection. One other patient possibly acquired histoplasmosis from a donor kidney; this patient did not live in an endemic area and was found to have disseminated histoplasmosis 30 days after receiving an unrelated donor kidney; unfortunately, no further data were available regarding the donor. The remaining 3 patients (1 liver transplant recipient and 2 kidney transplant recipients) lived in the endemic area and had isolated pulmonary infection without involvement of the transplanted organ; no further donor data were available.
Underlying conditions
All patients had underlying illnesses that required transplantation, and many had other co-existing illnesses (Table 2). All patients who received an SOT had received immunosuppressive medications, predominantly calcineurin inhibitors, mycophenolate, and corticosteroids, at the time of transplantation, and most remained on immunosuppressive medications at the time of infection. A total of 19 of the 64 SOT patients had experienced an episode of rejection at some time after transplantation, but only 5 patients had an episode of rejection with 6 weeks of the diagnosis of an endemic mycosis.
Table 2.
Co-morbid conditions and immunosuppressive medications present within 30 days before the diagnosis of an endemic fungal infection in hematopoietic cell and solid organ transplant recipients
| Number (%)
|
|||
|---|---|---|---|
| Co-morbid condition/drug
|
Blastomycosis (N = 9)
|
Coccidioidomycosis (N = 9)
|
Histoplasmosis (N = 52)
|
| Diabetes mellitus | 6 (67) | 0 | 14 (27) |
| Malnutrition | 5 (56) | 0 | 3 (6) |
| Chronic lung disease | 3 (33) | 0 | 3 (6) |
| Congestive heart failure | 2 (22) | 0 | 2 (4) |
| Chronic kidney disease | 3 (33) | 3 (33) | 19 (37) |
| Hepatic insufficiency | 1 (11) | 0 | 7 (13) |
| Rheumatologic disease | 0 | 0 | 2 (4) |
| Rejection episode1 | 1 (11) | 1 (11) | 3 (6) |
| Immunosuppressive drugs | |||
| Corticosteroids2 | 9 (100) | 8 (89) | 45 (87) |
| Calcineurin inhibitors | 8 (89) | 7 (78) | 39 (75) |
| Mycophenolate | 6 (67) | 7 (78) | 27 (52) |
| Sirolimus | 0 | 0 | 5 (10) |
| Azathioprine | 0 | 0 | 1 (2) |
Within 6 weeks of the diagnosis of an endemic mycosis.
Equivalent of ≥20 mg prednisone daily (methylprednisolone, dexamethasone, prednisone).
Only 3 patients, all of whom developed histoplasmosis and all of whom had received an autologous HCT, were not on immunosuppressive agents when they developed infection. The 2 patients who had an allogeneic HCT had GVHD and were being treated with corticosteroids (>20 mg prednisone equivalent daily) when they developed pulmonary histoplasmosis.
Prophylaxis with systemic antifungal agents was used uncommonly. Two patients had received fluconazole and another had received itraconazole prior to development of coccidioidomycosis; another patient had received fluconazole prior to the development of histoplasmosis.
Concomitant infections
Concomitant infections were uncommon in transplant recipients who developed an endemic mycosis. Herpesvirus infections, primarily cytomegalovirus infections, were the most frequent concomitant infections noted within 30 days of the diagnosis of an endemic mycosis (Table 3). Five patients had another IFI (3 had candidemia and 1 each had invasive aspergillosis and Alternaria sinusitis) concomitant with or within 30 days of the diagnosis of infection with an endemic mycosis.
Table 3.
Co-infections within 30 days of diagnosis of an endemic fungal infection in hematopoietic cell and solid organ transplant recipients
| Number (%)
|
||||
|---|---|---|---|---|
| Co-infections
|
Blastomycosis (N = 9)
|
Coccidioidomycosis (N = 9)
|
Histoplasmosis (N = 52)
|
Total (N = 70)
|
| Cytomegalovirus (CMV) | 4 (44) | 1 (11) | 7 (13) | 12 (17) |
| CMV antigenemia | 2 (22) | 0 | 4 (8) | 6 (9) |
| CMV disease | 2 (22) | 1 (11) | 3 (6) | 6 (9) |
| Herpes simplex | 0 | 0 | 1 (2) | 1 (2) |
| Varicella zoster | 1 (11) | 0 | 0 | 1 (2) |
| Bloodstream infections | ||||
| Gram-positive cocci | 1 (11) | 0 | 5 (10) | 6 (9) |
| Gram-negative bacilli | 0 | 0 | 4 (8) | 4 (8) |
| Candida species | 1 (11) | 0 | 2 (4) | 3 (4) |
| Invasive mold infections | 2 (22) | 0 | 0 | 2 (3) |
Organ involvement
Pulmonary involvement was common; however, it was the sole manifestation of infection in only 25 patients (36%) (Table 4). In the other 45 patients (64%), dissemination had occurred and was present along with pulmonary infection in 24 (34%). Dissemination was seen in 71% of the 52 patients who had histoplasmosis, and in 5 (56%) of the 9 patients who had coccidioidomycosis. Three (50%) of the 6 patients who had blastomycosis had disseminated infection: numerous skin lesions in 2 and central nervous system plus pulmonary infection in 1.
Table 4.
Type of infection with endemic mycoses among hematopoietic cell and solid organ transplant recipients
| Number (%)
|
||||
|---|---|---|---|---|
| Site of infection
|
Blastomycosis (N = 9)
|
Coccidioidomycosis (N = 9)
|
Histoplasmosis (N = 52)
|
Total (N = 70)
|
| Pulmonary alone | 6 (67) | 4 (44) | 15 (29) | 25 (36) |
| Pulmonary with dissemination | 1 (11) | 3 (33) | 20 (38) | 24 (34) |
| Disseminated | 2 (22) | 2 (22) | 17 (33) | 21 (30) |
The time from transplantation to infection was not related to dissemination. Patients with infection within 6 months of transplantation (19/28, 68%) were no more likely to have disseminated infection than those who developed disease >6 months post transplant (26/42, 62%).
Sites of dissemination that yielded the organism on culture or histopathology, including those obtained at autopsy, in patients with histoplasmosis were bone marrow (in 8), liver (in 7), gastrointestinal tract (in 6), kidney (in 3), spleen (in 2), skin (in 2), and knee, thyroid, and lymph node (in 1 each).
Diagnosis
The diagnosis of fungal infection was made before death in 67 patients, and only made at autopsy for 3 patients: 2 with donor-derived coccidioidomycosis, and 1 with histoplasmosis. Among those who had a diagnosis made before death, the most useful diagnostic tests for all 3 endemic mycoses appeared to be culture of sputum, bronchoalveolar lavage fluid, or lung biopsy samples (Table 5). Histopathologic examination of lung tissue identified the organism in 33% of cases of blastomycosis and in 29% of cases of coccidioidomycosis, but cytological examination of bronchoalveloar lavage fluid was more useful for H. capsulatum (20% of cases). Blood cultures proved useful only for histoplasmosis; >50% of patients had H. capsulatum isolated from blood.
Table 5.
Diagnostic tests used to establish the pre-mortem diagnosis of endemic fungal infections in hematopoietic cell and solid organ transplant recipients
| Number (%)*
|
|||
|---|---|---|---|
| Diagnostic test
|
Blastomycosis (N = 9)
|
Coccidioidomycosis (N = 7)
|
Histoplasmosis (N = 51)
|
| Positive culture | |||
| Blood | 0 | 0 | 27 (53) |
| BAL/sputum | 5 (56) | 3 (43) | 18 (35) |
| Lung | 1 (11) | 2 (29) | 4 (8) |
| Skin | 0 | 0 | 3 (6) |
| Bone marrow | 0 | 0 | 4 (8) |
| Liver | 0 | 0 | 1 (2) |
| Urine | 0 | 0 | 2 (4) |
| Lymph node | 0 | 0 | 1 (2) |
| Pleural fluid | 0 | 0 | 1 (2) |
| Synovial fluid | 0 | 1 (14) | 1 (2) |
| Histopathology | |||
| Lung | 3 (33) | 2 (29) | 5 (10) |
| Skin | 2 (22) | 1 (14) | 1 (2) |
| Bone marrow | 0 | 0 | 4 (8) |
| Liver | 0 | 0 | 4 (8) |
| Kidney | 0 | 0 | 1 (2) |
| Bowel | 0 | 0 | 3 (6) |
| Esophagus | 0 | 0 | 1 (2) |
| Cytology | |||
| BAL | 1 (11) | 1 (14) | 10 (20) |
| Serology | |||
| Antigen, serum | 0 | 0 | 13 (25) |
| Antigen, urine | 0 | 0 | 29 (57) |
| Antibody, CF or ID | 0 | 3 (43) | 3 (6) |
Patients often had >1 positive diagnostic test.
BAL, bronchoalveolar lavage; CF, complement fixation; ID, immunodiffusion.
Among patients with histoplasmosis who underwent Histoplasma antigen testing, results were positive in 29 from urine and in 13 patients from serum. Unfortunately, data on the total number of patients who had antigen testing performed were not reported. Only 2 patients with disseminated histoplasmosis had only a positive antigen test without a positive culture or histopathologic demonstration of tissue invasion. At the time of this study, the Blastomyces antigen test was not readily available. Antibody studies were rarely obtained and were positive in only 3 patients with histoplasmosis and in 3 with coccidioidomycosis.
Treatment
Three patients, 2 of whom had coccidioidomycosis and 1 who had histoplasmosis, were not treated with antifungal agents because the diagnosis was made only at autopsy. For the remaining 67 patients, initial treatment was primarily with a lipid formulation of amphotericin B (AmB) (Table 6). Of the 43 patients who were treated with AmB at some point, 39 (91%) received a lipid formulation of AmB. Only 4 patients, all of whom had histoplasmosis, received AmB deoxycholate. Seven patients received an AmB formulation only, and 5 of these 7 patients died from 3 to 19 days after the antifungal agent was started. Most other patients, who were given AmB initially, were transitioned to oral azole therapy, usually itraconazole, at a mean of 17 days.
Table 6.
Treatment of endemic mycoses in hematopoietic cell and solid organ transplant recipients
| Number (%)
|
|||
|---|---|---|---|
| Antifungal agent
|
Blastomycosis (N = 9)
|
Coccidioidomycosis (N = 9)
|
Histoplasmosis (N = 52)
|
| AmB, then Itra | 2 (22) | 0 | 26 (50) |
| AmB, then Vori | 1 (11) | 0 | 0 |
| AmB + azole1 | 2 (22) | 0 | 1 (2) |
| AmB | 0 | 2 (22) | 5 (10) |
| Itra | 0 | 0 | 10 (19) |
| Vori | 3 (33) | 1 (11) | 1 (2) |
| Flu | 0 | 2 (22) | 1 (2) |
| Azoles2 | 1 (11) | 1 (11) | 4 (8) |
| Azole, then AmB3 | 0 | 1 (11) | 3 (6) |
| None4 | 0 | 2 (22) | 1 (2) |
Blastomycosis: AmB + vori (in 2); Histoplasmosis: AmB + Flu (in 1).
Blastomycosis: Vori, then Itra (in 1); Coccidioidomycosis: Vori, then Itra (in 1); Histoplasmosis: Vori, then Flu (in 1), Vori, then Itra (in 1), Itra then Flu then Vori (in 1), Itra then Vori then Posa (in 1).
Coccidioidomycosis: Flu then Vori then AmB (in 1); Histoplasmosis: Itra then AmB (in 3).
Diagnosis made after death.
AmB, amphotericin B; Itra, itraconazole; Flu, fluconazole; Vori, voriconazole; Posa, posaconazole.
For patients deemed to have less severe disease, half of whom had disseminated infection, therapy consisted of an azole agent alone, primarily itraconazole. However, patients who had blastomycosis were treated more frequently with voriconazole than with itraconazole. Fluconazole was rarely used to treat histoplasmosis or blastomycosis, but this agent was used for 3 of the 9 patients who had coccidioidomycosis.
Outcomes
At 3 months after an endemic fungal infection was diagnosed, no deaths occurred among the 6 patients who had received an HCT, and 10 deaths occurred among the 64 (16%) SOT recipients. Among these 64 patients, death was thought likely to be a result of the fungal infection in 7 (11%). Three of the 7 (43%) SOT recipients who had coccidioidomycosis died; 2 of these patients died of disseminated coccidioidomycosis that was derived from the donor kidney and liver, and the third patient died of bacterial pneumonia.
Seven of the 48 (15%) SOT recipients who developed histoplasmosis died within 3 months of diagnosis, and 5 of these deaths were attributed to disseminated histoplasmosis. For those 5 patients, including 1 in whom the diagnosis was made only at autopsy, death occurred within 3–19 days after they presented with symptoms of histoplasmosis. No deaths occurred at 3 months among the 9 SOT recipients who had blastomycosis, but 2 patients who had severe pulmonary blastomycosis with acute respiratory distress syndrome were left with chronic respiratory insufficiency. Mortality was not different for patients who developed infection within the first 6 months after transplantation (5/28, 18%) and those whose infection occurred >6 months after transplantation (5/42, 12%, P = 0.72).
Discussion
Endemic mycoses are an uncommon cause of IFI in SOT and HCT recipients. The strong associations noted with Candida species infections in the immediate posttransplant period and with opportunistic mold infections in patients with GVHD or rejection were not apparent for infection with the endemic mycoses (2, 3).
Among SOT recipients in the Incidence Cohort, 33 (0.2%) developed an endemic mycosis during the surveillance period, and the 1-year cumulative incidence for histoplasmosis was 0.1%. The onset of infection ranged from immediately post transplantation to 11 years post transplantation, indicating that clinicians must include endemic mycoses in their differential diagnoses even many years after transplantation. A bimodal distribution was seen, with 40% of cases occurring within the first 6 months after transplantation when immunosuppression was greatest, and 34% of infections occurring >2 years post transplantation. This bimodal distribution has been noted previously in smaller and single-center series of endemic mycoses following organ transplantation, although some reports showed a greater rate of infections occurring earlier after transplantation than what we observed (5, 7-10).
Among HCT recipients in the Incidence Cohort, only 3 (0.02%) developed histoplasmosis. The reasons for this low incidence are not known, but the rarity of endemic mycoses among HCT recipients has been noted previously (1, 11, 12). Perhaps it is because these patients are not likely to be engaged in outdoor activities before engraftment or when undergoing intensive immunosuppression for GVHD, and they are usually on antifungal prophylaxis during these periods. In addition, immune reconstitution occurs by 6 months in many HCT recipients, in contrast with SOT recipients who generally remain on continuing immunosuppression for years. This low rate also suggests infrequent reactivation infection in this population, as described in a prior retrospective review of allogeneic HCT recipients from an endemic area (12).
Rejection did not appear to have a major role in development of endemic mycoses in SOT recipients. Other investigators also have reported similar findings with histoplasmosis and blastomycosis (5, 7-9), but rejection has been associated with a higher risk of development of coccidioidomycosis (13). The role of rejection as a risk factor for endemic fungal infections differs greatly from that noted for invasive mold infections, such as fusariosis, mucormycosis, and scedosporiosis, in the TRANSNET cohort (4).
The geographic distribution of cases was similar to the areas of endemicity for each of the 3 mycoses. However, in 7 cases, the infection was reported from a transplant center outside those areas. Four of these patients had lived in or traveled to, before or after receiving the transplant, an area endemic for the infecting fungus. Thus, obtaining a precise travel history is essential in evaluating the etiology of posttransplant infections.
Three patients were documented to have received organs that contained either Coccidioides species or H. capsulatum. Blastomycosis was not documented as a donor-derived infection in this series nor in other previous reports (5, 8, 10). Donor-derived fungal infections have been identified most often among recipients of kidney transplants, but also have been reported in recipients of other organs (6, 7, 10, 13-19).
Most recipients who receive an organ containing an endemic fungus develop manifestations of infection within several weeks post transplantation. One patient in the current study received a donor liver that contained organisms thought to be H. capsulatum; with immediate therapy with an azole, she never developed active histoplasmosis. This case is similar to those of 4 patients from the Cleveland Clinic who received donor lungs with H. capsulatum and who did well post transplantation with itraconazole treatment (7). It is possible that additional donor-derived infections occurred among the 40% of patients who manifested infection within the first 6 months after transplantation. However, we do not have data on the donors or other transplant recipients who had received organs from the same donors.
Not surprisingly, histoplasmosis was manifested in three-quarters of patients as disseminated infection, with or without documented pulmonary involvement. The tendency for dissemination has also been reported previously in other series of histoplasmosis in transplant recipients (5, 7, 9). Widespread dissemination was evidenced by the fact that more than half of the patients had H. capsulatum isolated from blood cultures.
The lungs were the primary site of infection among patients who had blastomycosis; those who did have dissemination had localized disease. The limited number of cases of disseminated blastomycosis among transplant recipients was noted in a prior report (5).
Although the 2 patients who received donor organs containing Coccidioides species had widely disseminated infection, most of the other patients, including the 2 HCT recipients, had more localized coccidioidomycosis. Four had pulmonary infection only, and 3 had pulmonary involvement with dissemination documented only to skin or osteoarticular structures. In contrast, other series from endemic areas for coccidioidomycosis found a higher frequency of disseminated disease among SOT recipients (13, 20). Those reports that consist of greater numbers of patients likely, reflect more accurately the types of disease caused by Coccidioides species in the transplant population (13).
Treatment was determined by the practices at individual transplant centers. Most patients were treated in accordance with what later became the standard of therapy, as detailed in the Infectious Diseases Society of America guidelines for the respective infections (21-23). Several findings are notable. Among patients who were treated with an AmB formulation, only 9% received conventional AmB (deoxycholate formulation) and 91% received a lipid formulation, reflecting increased use of less toxic formulations and acceptance of the evidence in AIDS patients that liposomal AmB is more efficacious than the deoxycholate formulation for treating disseminated histoplasmosis (24). The higher death rate among those patients who received AmB only likely reflects the severity of infection at presentation.
Itraconazole is the agent recommended for stepdown therapy following AmB, and for initial therapy of mild-to-moderate histoplasmosis and blastomycosis (21, 22). However, more patients who had blastomycosis were treated with voriconazole than with itraconazole. Some clinicians chose to use voriconazole rather than itraconazole because it achieves higher cerebrospinal fluid levels and is better absorbed. However, clinical experience treating blastomycosis and histoplasmosis with voriconazole is limited compared to that with itraconazole, and both success and failure have been noted (8, 25).
This study has several limitations. First, the institutions in our study were not equally distributed across all geographic areas in which the endemic mycoses occur. Fewer sites were located in areas in which coccidioidomycosis is endemic than in sites in which histoplasmosis and blastomycosis are endemic. Thus, the low number of cases of coccidioidomycosis is probably not an accurate representation of the rate of occurrence of infection with this organism in the transplant population. Second, to establish more firmly whether infection was donor-derived, it is essential to have information on donors and other transplant recipients who shared organs from the same donor. These data were not accessible to us and have rarely been available in prior studies of transplant-related endemic mycoses. Third, detailed data on diagnostic testing were not collected in this surveillance study. Future studies that collect data on the height and duration of antigenemia and antigenuria, and how those tests influence the accuracy and rapidity of diagnosis of histoplasmosis, will provide useful information for the clinician.
Our large multicenter study provides comprehensive surveillance data defining the incidence of endemic mycoses among SOT and HCT recipients in the United States. We found that overall rates of infection with the endemic mycoses in the transplant population are low, but the risk continues for many years post transplantation. The response to therapy of these infections is excellent, but physicians must be vigilant in order to establish the diagnosis early and initiate appropriate antifungal treatment in this vulnerable population.
Acknowledgments
Support: This study was supported through CDC Grant 5U01CI000286-05 and grants from Merck & Co., Inc.; Astellas US, Inc.; Pfizer, Inc.; Schering-Plough Research Institute; and Enzon Pharmaceuticals, Inc.
P.G.P.: Research grants: Merck, Pfizer, Astellas, T2 Biosystems, Gilead; Ad hoc Advisory Committees: Merck, Astellas, Gilead, and T2 Biosystems. C.A.K.: Data Safety Committee: Merck; Data Review Committee: New England Research Institute. A.G.F.: Data Safety Committee: Astellas; Consultant: Merck. T.F.P.: Research grants: Merck, Pfizer, Astellas; Consultant or received honoraria: Merck, Pfizer, Astellas, Toyoma, Viamet. V.A.M.: Data Safety Committee: Celgene; Data Review Committee: Merck; Speakers Bureaus: Amgen, Celgene, Genentech. J.W.B.: Data Review Committees: Astellas, Pfizer; Consultant: Merck, Mayne Pharma. J.I.I.: Speakers Bureaus: Astellas, Merck, Sigma Tau. K.A.M.: Research grants: Astellas, Merck, Pfizer, Sigma Tau; Consultant/Advisory Boards: Astellas, Merck, Pfizer, Optimer. G.M.L.: Research grants: Astellas, T2 Biosystems. D.R.A.: Research grants: Merck, Astellas; Consultant: Merck, Astellas. B.D.A.: Research grants: Pfizer, Astellas, Charles River Laboratories.
Footnotes
Potential conflicts of interest: All others author: No conflicts.
References
- 1.Kauffman CA. Endemic mycoses after hematopoietic stem cell or solid organ transplantation. In: Bowden R, Ljungman P, Snydman DR, editors. Transplant Infections. 3. Philadelphia, PA: Lippincott, Williams, and Wilkins; 2010. pp. 607–616. [Google Scholar]
- 2.Pappas PG, Alexander BD, Andes DR, et al. Invasive fungal infections among organ transplant recipients in the United States: results of the Transplant-Associated Infection Surveillance Network (TRANSNET) Clin Infect Dis. 2010;50:1101–1112. doi: 10.1086/651262. [DOI] [PubMed] [Google Scholar]
- 3.Kontoyiannis DP, Marr KA, Park BJ, et al. Prospective surveillance for invasive fungal infections in hematopoietic stem cell transplant recipients, 2001–2006: overview of the TRANSNET database. Clin Infect Dis. 2010;50:1091–1100. doi: 10.1086/651263. [DOI] [PubMed] [Google Scholar]
- 4.Park BJ, Pappas PG, Wannemuehler KA, et al. Invasive non- Aspergillus mold infections in transplant recipients, United States, 2001–2006. Emerg Infect Dis. 2011;17:1855–1864. doi: 10.3201/eid1710.110087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Grim S, Proia L, Miller R, et al. A multicenter study of histoplasmosis and blastomycosis after solid organ transplantation. Transpl Infect Dis. 2012;14:17–23. doi: 10.1111/j.1399-3062.2011.00658.x. [DOI] [PubMed] [Google Scholar]
- 6.Wright PW, Pappagianis D, Wilson M, et al. Donor-related coccidioidomycosis in organ transplant recipients. Clin Infect Dis. 2003;37:1265–1269. doi: 10.1086/378741. [DOI] [PubMed] [Google Scholar]
- 7.Cuellar-Rodriquez J, Avery RK, Lard M, et al. Histoplasmosis in solid organ transplant recipients: 10 years of experience at a large transplant center in an endemic area. Clin Infect Dis. 2009;49:710–716. doi: 10.1086/604712. [DOI] [PubMed] [Google Scholar]
- 8.Gauthier GM, Safdar N, Klein BS, Andes DR. Blastomycosis in solid organ transplant recipients. Transpl Infect Dis. 2007;9:310–317. doi: 10.1111/j.1399-3062.2007.00227.x. [DOI] [PubMed] [Google Scholar]
- 9.Freifeld AG, Iwen PC, Lesiak BL, Gilroy RK, Stevens RB, Kalil AC. Histoplasmosis in solid organ transplant recipients at a large Midwestern university transplant center. Transpl Infect Dis. 2005;7:109–115. doi: 10.1111/j.1467-8365.2005.00105.x. [DOI] [PubMed] [Google Scholar]
- 10.Martin-Davila P, Fortun J, Lopez-Velez R, et al. Transmission of tropical and geographically restricted infections during solid-organ transplantation. Clin Microbiol Rev. 2008;21:60–96. doi: 10.1128/CMR.00021-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Glenn TJ, Blair JE, Adams RH. Coccidioidomycosis in hematopoietic stem cell transplant recipients. Med Mycol. 2005;43:705–710. doi: 10.1080/13693780500147840. [DOI] [PubMed] [Google Scholar]
- 12.Vail GM, Young RS, Wheat LJ, Filo RS, Cornetta K, Goldman M. Incidence of histoplasmosis following allogeneic bone marrow transplant or solid organ transplant in a hyperendemic area. Transpl Infect Dis. 2002;4:148–151. doi: 10.1034/j.1399-3062.2002.01016.x. [DOI] [PubMed] [Google Scholar]
- 13.Blair JE, Logan JL. Coccidioidomycosis in solid organ transplantation. Clin Infect Dis. 2001;33:1536–1544. doi: 10.1086/323463. [DOI] [PubMed] [Google Scholar]
- 14.Miller MB, Hendren R, Gilligan PH. Posttransplantation disseminated coccidioidomycosis acquired from donor lungs. J Clin Microbiol. 2004;42:2347–2349. doi: 10.1128/JCM.42.5.2347-2349.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Botterel F, Romand S, Saliba F, et al. A case of disseminated histoplasmosis likely due to infection from a liver allograft. Eur J Clin Microbiol Infect Dis. 1999;18:662–664. doi: 10.1007/s100960050369. [DOI] [PubMed] [Google Scholar]
- 16.Dierberg KL, Marr KA, Subramanian A, et al. Donor-derived organ transplant transmission of coccidioidomycosis. Transpl Infect Dis. 2011;14:300–304. doi: 10.1111/j.1399-3062.2011.00696.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Blodget E, Geiseler PJ, Larsen RA, Stapfer M, Qazi Y, Petrovic LM. Donor-derived Coccidioides immitis fungemia in solid organ transplant recipients. Transpl Infect Dis. 2011;14:305–310. doi: 10.1111/j.1399-3062.2011.00698.x. [DOI] [PubMed] [Google Scholar]
- 18.Tripathy U, Yung GL, Kriett JM, et al. Donor transfer of pulmonary coccidioidomycosis in lung transplantation. Ann Thorac Surg. 2002;73:306–308. doi: 10.1016/s0003-4975(01)02723-0. [DOI] [PubMed] [Google Scholar]
- 19.Limaye AP, Connolly PA, Sagar M, et al. Transmission of Histoplasma capsulatum by organ transplantation. N Engl J Med. 2000;343:1163–1166. doi: 10.1056/NEJM200010193431605. [DOI] [PubMed] [Google Scholar]
- 20.Antony SJ, Dummer SJ, McNeil KK, Salas I. Coccidioidomycosis in renal transplant recipients. Infect Dis Clin Pract. 2005;13:250–254. [Google Scholar]
- 21.Chapman SW, Dismukes WE, Proia LA, et al. Clinical practice guidelines for the management of patients with blastomycosis: 2008 update by the Infectious Diseases Society of America. Clin Infect Dis. 2008;46:1801–1812. doi: 10.1086/588300. [DOI] [PubMed] [Google Scholar]
- 22.Wheat LJ, Freifeld AG, Kleiman MB, et al. Clinical practice guidelines for the management of patients with histoplasmosis: 2007 update by the Infectious Diseases Society of America. Clin Infect Dis. 2007;45:807–817. doi: 10.1086/521259. [DOI] [PubMed] [Google Scholar]
- 23.Galgiani JN, Ampel NM, Blair JE, et al. Coccidioidomycosis. Clin Infect Dis. 2005;41:1217–1223. doi: 10.1086/496991. [DOI] [PubMed] [Google Scholar]
- 24.Johnson PC, Wheat LJ, Cloud GA, et al. Safety and efficacy of liposomal amphotericin B compared with conventional amphotericin B for induction therapy of histoplasmosis in patients with AIDS. Ann Intern Med. 2002;137:105–109. doi: 10.7326/0003-4819-137-2-200207160-00008. [DOI] [PubMed] [Google Scholar]
- 25.Freifeld A, Proia LA, Andes D, et al. Voriconazole use for endemic fungal infections. Antimicrob Agents Chemother. 2009;53:1648–1651. doi: 10.1128/AAC.01148-07. [DOI] [PMC free article] [PubMed] [Google Scholar]


