Abstract
Background
The Classification for Early-onset Scoliosis (C-EOS) was developed by a consortium of early-onset scoliosis (EOS) surgeons. This study aims to examine if the C-EOS classification correlates with the speed (failure/unit time) of proximal anchor failure in EOS surgery patients.
Methods
A total of 106 EOS patients were retrospectively queried from an EOS database. All patients were treated with vertical expandable prosthetic titanium rib and experienced proximal anchor failure. Patients were classified by the C-EOS, which includes a term for etiology [C: Congenital (54.2%), M: Neuromuscular (32.3%), S: Syndromic (8.3%), I: Idiopathic (5.2%)], major curve angle [1: ≤20 degrees (0%), 2: 21 to 50 degrees (15.6%), 3: 51 to 90 degrees (66.7%), 4: >90 degrees (17.7%)], and kyphosis [“−”: ≤20 (13.5%), “N”: 21 to 50 (42.7%), “+”: >50 (43.8%)]. Outcome was measured by time and number of lengthenings to failure.
Results
Analyzing C-EOS classes with >3 subjects, survival analysis demonstrates that the C-EOS discriminates low, medium, and high speed of failure. The low speed of failure group consisted of congenital/51-90/hypokyphosis (C3−) class. The medium-speed group consisted of congenital/51-90/normal and hyperkyphosis (C3N, C3+), and neuromuscular/51-90/hyperkyphosis (M3+) classes. The high-speed group consisted of neuromuscular/51-90/normal kyphosis (M3N), and neuromuscular/>90/normal and hyperkyphosis (M4N, M4+) classes. Significant differences were found in time (P < 0.05) and number of expansions (P < 0.05) before failure between congenital and neuromuscular classes. As isolated variables, neuromuscular etiology experienced a significantly faster time to failure compared with patients with idiopathic (P < 0.001) and congenital (P = 0.026) etiology. Patients with a major curve angle >90 degrees demonstrated significantly faster speed of failure compared with patients with major curve angle 21 to 50 degrees (P = 0.011).
Conclusions
The ability of the C-EOS to discriminate the speeds of failure of the various classification subgroups supports its validity and demonstrates its potential use in guiding decision making. Further experience with the C-EOS may allow more tailored treatment, and perhaps better outcomes of patients with EOS.
Level of Evidence
Level III.
Keywords: early-onset scoliosis, scoliosis, vertical expandable prosthetic titanium rib, VEPTR, growing rod, growth friendly surgery, Classification for Early-onset Scoliosis
Early-onset scoliosis (EOS) is a heterogeneous population including congenital, neuromuscular, syndromic, and idiopathic etiologies. These etiologies have variable curve severities and differing natural histories.1–4 Communication and research with respect to EOS patients is a challenge due to this heterogeneity.5,6 In fact, numerous studies regarding the treatment of EOS have used mixed populations of patients, complicating the interpretation of such studies.7–10 EOS providers lack a common language to simplify communication regarding these patients, and in research, investigators are unable to compare management practices and outcomes.11
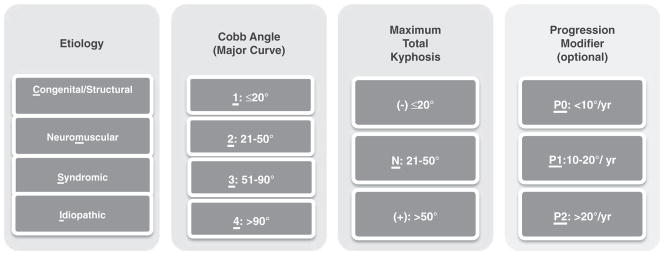
To address this issue, classification systems are essential tools that define pathology and provide the language to describe it.12 The Classification for Early-onset Scoliosis (C-EOS) (Fig. 1) was developed following a 3-step model proposed by Audigé et al.13 C-EOS facilitates the subgrouping of patients who may share natural histories and may benefit from similar treatments.12 Establishing the validity and utility of the C-EOS is crucial for the utilization of this instrument within research and clinical contexts. The purpose of this study is to establish the validity and utility of the C-EOS by evaluating its association with the speed of a common complication of EOS surgery: vertical expandable prosthetic titanium rib (VEPTR; Synthes Spine Co., West Chester, PA) proximal fixation failure.
FIGURE 1.
VEPTR relies on proximal fixation to the rib with circumferential rib “cradles” in order to support the thoracic cage. These fixation points migrate or fail with high frequency depending on the stresses on the construct, bone quality, and duration of attachment.14 This study aims to compare speed of proximal fixation failure in VEPTR constructs between classes of the C-EOS. We hypothesize that neuromuscular etiology, higher major curve angles, and higher kyphosis angles will correlate with higher speeds of VEPTR anchor failure.
METHODS
Design
This is a retrospective, multicenter study with data collected through an EOS study group registry from 2005 to 2012. Eight academic institutions contributed data: [Boston Children’s Hospital, University of Utah, Shriner’s Hospital for Children Los Angeles & Philadelphia, Children’s Hospital of Philadelphia, University of Colorado, Le Boenheur Children’s Hospital, and Children’s Hospital of New York].
Participants
Patients with a diagnosis of EOS were prospectively enrolled into an EOS study group registry. This database was queried to retrospectively gather data pertaining to patients with the following characteristics: age less than 8 years of age, underwent VEPTR implant surgery, and suffered subsequent proximal fixation failure.
Outcomes
The outcome analyzed was VEPTR proximal fixation failure speed. Failure was defined as a radiographic evidence of proximal fixation failure whether or not the patient necessitated emergent revision surgery. The speed of a failure was calculated using the formula:
For example, the speed of failure for the C3− C-EOS group was calculated by dividing the total observed failures (5) into the total months of observation for all 5 failures (250). This yielded a speed of 1 failure/50 months.
Procedures
The EOS study group registry was queried with the inclusion criteria listed above. Once study subjects were identified, data managers at contributing sites ensured data integrity and provide missing data fields. Study subject data was sent to [Children’s Hospital of New York] in order to classify patients by the C-EOS scheme and for subsequent analysis.
C-EOS classification groups with n > 3 were subjected to survivorship analysis. Speed stratification was accomplished by looking at months to <50% survival. If <50% survival occurred within 1 year of VEPTR implant, this was defined as high speed. If <50% survival occurred within 1 to 3 years of VEPTR implant, this was defined as medium speed. If <50% survival occurred beyond 3 years of VEPTR implant, this was defined as low speed.
Statistical Analysis
To analyze differences within each classification component, analysis of variance was used. Statistical significance was defined as P < 0.05. To analyze differences among classification groups, Kaplan-Meier survivorship analysis was used.
RESULTS
The registry query resulted in 106 subjects meeting inclusion with 96 having etiology, major curve angle, and kyphosis for complete classification. Of the 105 subjects, there were 51 (48.1%) males, 44 (41.5%) females, and 11 (10.4%) unknown. Mean age at index surgery was 4.7 ± 2.6 years with a mean follow-up of 6.2 ± 2.7 years. All etiology groups of the C-EOS, major curve angle classification groups 2, 3, and 4, and all kyphosis classification groups were represented by the study population (Table 1). Twenty-six classification groups were represented, 7 of which had >3 subjects (Table 2).
TABLE 1.
Demographics of Participants
| C-EOS Variables | Classification | N (%) |
|---|---|---|
| Etiology | Congenital | 52 (54.2) |
| Neuromuscular | 31 (32.3) | |
| Syndromic | 8 (8.3) | |
| Idiopathic | 5 (5.2) | |
| Cobb (deg.) | ≤20 | 0 (0) |
| 21–50 | 15 (15.6) | |
| 51–90 | 64 (66.7) | |
| > 90 | 17 (17.7) | |
| Maximum kyphosis (deg.) | ≤20 | 13 (13.5) |
| 21–50 | 41 (42.7) | |
| > 50 | 42 (43.8) |
C-EOS indicates Classification for Early-onset Scoliosis.
TABLE 2.
Frequencies of Classes
| Classification | N (%) |
|---|---|
| C2− | 2 (2.1) |
| C2N | 3 (3.1) |
| C2+ | 3 (3.1) |
| C3−* | 5 (5.2) |
| C3N* | 18 (18.8) |
| C3+* | 14 (14.6) |
| C4− | 1 (1.0) |
| C4N | 2 (2.1) |
| C4+ | 3 (3.1) |
| M2N | 1 (1.0) |
| M3− | 3 (3.1) |
| M3N* | 7 (7.3) |
| M3+* | 9 (9.4) |
| M4− | 1 (1.0) |
| M4N* | 4 (4.2) |
| M4+* | 5 (5.2) |
| S2N | 2 (2.1) |
| S2+ | 1 (1.0) |
| S3− | 1 (1.0) |
| S3N | 1 (1.0) |
| S3+ | 2 (2.1) |
| S4+ | 1 (1.0) |
| I2N | 2 (2.1) |
| I2+ | 1 (1.0) |
| I3N | 2 (2.1) |
| I3+ | 2 (2.1) |
> 3 patients present.
When subjected to Kaplan-Meier Survivorship analysis, the 7 classification groups with >3 subjects were stratified into low-speed, medium-speed, and high-speed groups. The low speed of failure group consisted of congenital/51-90 degrees/hypokyphosis (C3−) class. The medium-speed group consisted of congenital/51-90 degrees/normal and hyperkyphosis (C3N, C3+), and neuromuscular/51-90 degrees/hyperkyphosis (M3+) classes. The high-speed group consisted of neuromuscular/51-90 degrees/normal kyphosis (M3N) and neuromuscular/>90 degrees/normal and hyperkyphosis (M4N, M4+) classes (Fig. 2) and (Table 3). Time to failure was calculated as an average of months or years within classes with n > 3. Congenital curves were slower to failure than neuromuscular, and within the neuromuscular etiology, higher major curve angle classes were faster to failure than lower major curve angle classes (Table 4).
FIGURE 2.
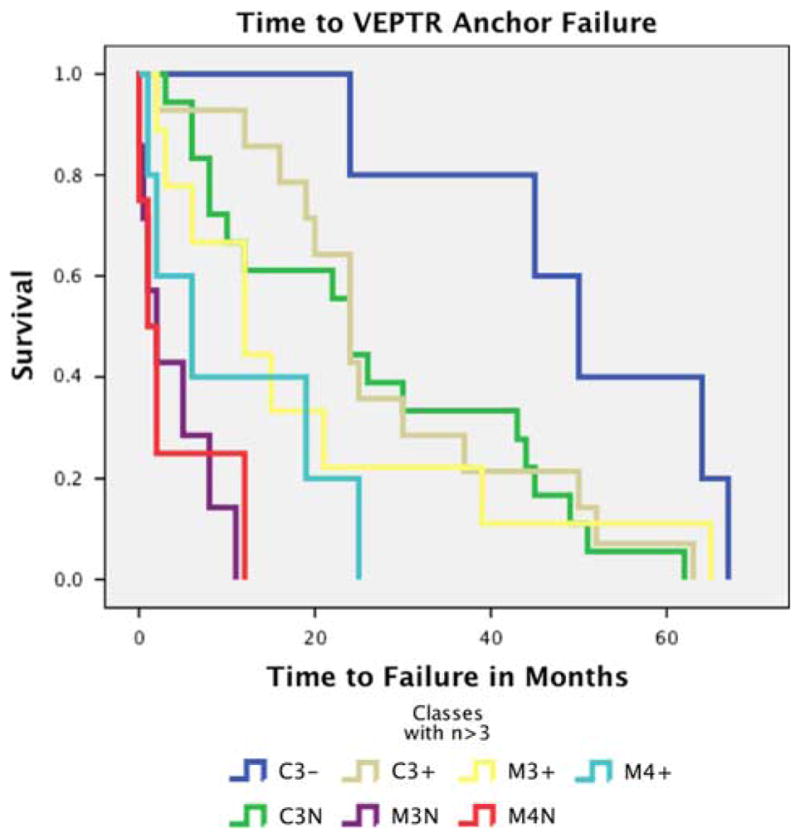
Time to vertical expandable prosthetic titanium rib proximal fixation failure.
TABLE 3.
C-EOS Classes by Speed Group
| Speed | Classification |
|---|---|
| Low speed | C3− |
| Medium speed | C3N |
| C3+ | |
| M3+ | |
| High speed | M3N |
| M4N | |
| M4+ |
C-EOS indicates Classification for Early-onset Scoliosis.
TABLE 4.
Average Months and Years to Failure in Classes With n > 3
| C-EOS | Average Months to Failure | Average Years to Failure |
|---|---|---|
| C3− | 50 | 4.17 |
| C3N | 26.28 | 2.19 |
| C3+ | 28.43 | 2.37 |
| M3N | 3.93 | 0.33 |
| M3+ | 19.44 | 1.62 |
| M4N | 3.75 | 0.31 |
| M4+ | 10.6 | 0.88 |
C-EOS indicates Classification for Early-onset Scoliosis.
Analysis of variance for speed of proximal fixation failure for individual C-EOS variables resulted in significant findings in the etiology and major curve angle variables. Subjects with neuromuscular scoliosis exhibited significantly faster speed of proximal fixation failure than idiopathic (P = 0.026) and congenital scoliosis (P < 0.001) subjects (Fig. 3). Subjects with curves >90 degrees exhibited significantly faster speed of proximal fixation failure in comparison to curves of 25 to 50 degrees (P = 0.011) and 51 to 90 degrees (P = 0.031) (Fig. 4). More failures occurred within the higher kyphosis classes (N, or +), but there were no significant differences in the speed of failure among kyphosis groups.
FIGURE 3.
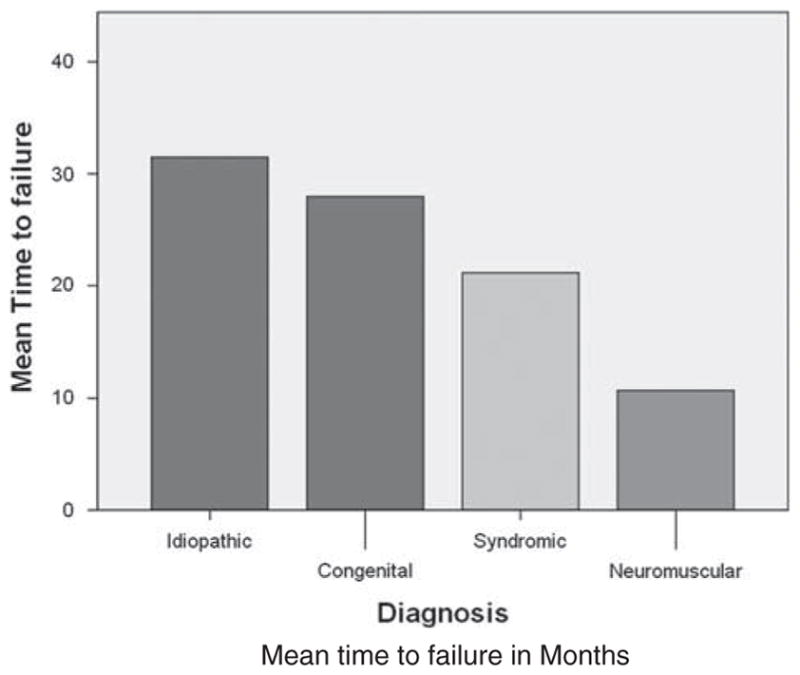
Mean time to failure by diagnosis. Neuromuscular versus idiopathic (P = 0.026). Neuromuscular versus congential (P < 0.001).
FIGURE 4.
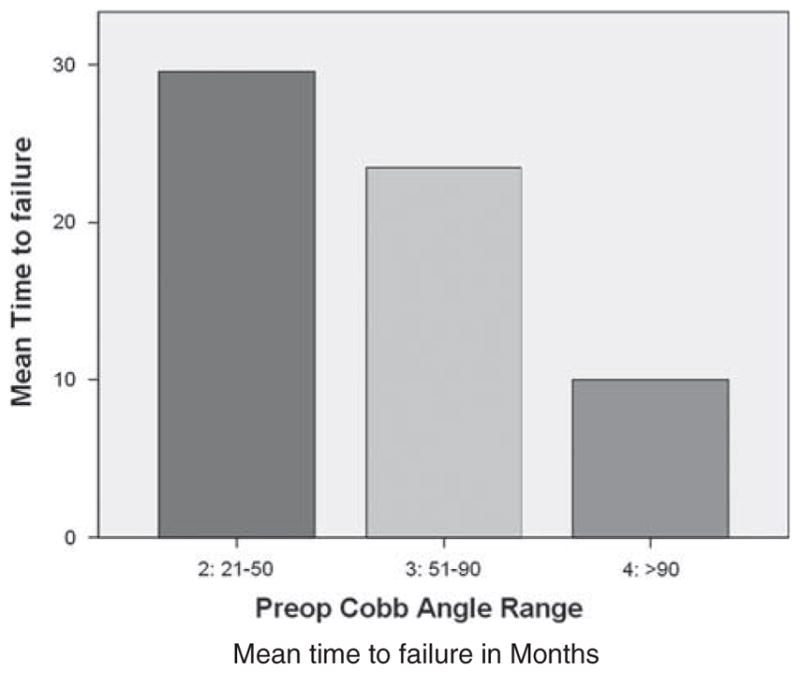
Mean time to failure by preoperative major curve angle. >90 degrees versus 21 to 50 degrees (P = 0.011). >90 degrees versus 51 to 90 degrees (P = 0.031).
DISCUSSION
Our study demonstrates that the C-EOS with combined elements of etiology, major curve angle, and kyphosis has the capability to stratify the speed of rapid VEPTR proximal anchor failure. Furthermore, the manner in which the classification groups progress toward higher speed of VEPTR anchor failure is in concert with the conceptual understanding of mechanical stress upon the surgical construct.15,16 When examining the results, neuromuscular etiology, increased major curve angle, and normokyphosis or hyperkyphosis were correlated with rapid VEPTR anchor failure. In fact, the order of classifications progressed from congenital to neuromuscular, major curve angle 51 to 90 degrees to >90 degrees, hypokyphosis to hyperkyphosis, which is in line with expectation. In terms of etiology, neuromuscular scoliosis can confer high stress to VEPTR devices as these patients often have rigid curves with associated spasticity or paralysis, factors implicated in implant-related complications of scoliosis surgery.17,18 It also follows that increased coronal and sagittal curves would also confer high stress upon VEPTR devices, factors that are also implicated in complications of growing spine surgery.19 Therefore, the progression of speed by classification group found in this study supports the validity and utility of the C-EOS.
When analyzed by individual variables, neuromuscular curves exhibited a significantly faster speed of failure than idiopathic or congenital curves. Studies have reported mixed results when examining the correlation between complications and etiology. However, there is evidence to suggest that neuromuscular scoliosis confers a high rate of complications. In a study of the Scoliosis Research Society Morbidity and Mortality database of 19,360 subjects, 4657 were neuromuscular, which was found to have a significantly greater complication rate in pediatric scoliosis surgery.20 A common complication of these patients was implant related.20 Bess et al9 found that neuromuscular patients treated with growing rods experienced the highest number of complications. However, McElroy et al21 found that the complication rate in spinal muscular atrophy subjects, a neuromuscular etiology of scoliosis, was less than that of idiopathic patients, providing evidence contrary to the notion of high rates of complications in neuromuscular scoliosis.
This study’s findings suggest that higher degree curvatures are associated with a higher speed of proximal fixation failure in VEPTR surgery. In terms of major curve angle and kyphosis, major curve angle >90 degrees and higher degrees of kyphosis correlated with speed of anchor failure. More severe preoperative major curve angles have been shown to increase the speed of general complications in scoliosis surgery.22,23 Schroerlucke et al24 found that hyperkyphosis subjects undergoing growing rods surgery had significantly more complications than normal kyphosis subjects. These findings lend support to the validity of the individual variables of the C-EOS.
The study’s strengths include its multicenter and multisurgeon experience of a known complication of VEPTR surgery. However, the retrospective nature of this study with its low study size prevents the inclusion of more C-EOS classes that have >3 subjects. Furthermore, the study size does not adequately power statistical analysis between specific C-EOS classes. Therefore, future steps for the C-EOS include validation studies that follow the outcomes of EOS patients over medium to long term with larger sample sizes.
The ability of the C-EOS to discriminate among various classification subgroups supports its validity and demonstrates its potential use in guiding decision making. Further experience with the C-EOS may allow more tailored treatment, better advice to patients, and improved outcomes for patients with EOS.
Acknowledgments
H.M. receives grant support from the Children’s Spine Foundation, Cerebral Palsy International Research Foundation, Pediatric Orthopaedic Society of North America, Scoliosis Research Society, Children’s Spine Foundation; travel support from Biomet, Medtronic, DePuy, Synthes, Stryker. D.P.R. receives grant support from Children’s Spine Foundation, Cerebral Palsy International Research Foundation, Pediatric Orthopaedic Society of North America, Scoliosis Research Society, Biomet, and OMeGA Medical Grant; Board membership with SICOT (nonfinancial) and JBJS editor (nonfinancial); consultancy with Stryker (nonfinancial); travel support from Biomet, Medtronic, DePuy, Synthes, Stryker; other support from Orthopaedic Research and Education Foundation. R.R.B. receives travel support from DePuy Synthes Spine; board membership with Children’s Spine Foundation; consultancy support from DePuy Synthes Spine, Medtronic, Orthocon, SpineGuard, Zimmer; royalties from DePuy Synthes Spine and Medtronic; stock/stock options in Orthocon, SpineGuard, Orthobond, MiMedx, Advanced Vertebral Solutions, SpineZ. P.J.C. receives support from the Children’s Spine Foundation; support for consultancy from DePuy Synthes Spine and Medtronic; support for lecture/speakers bureau from DePuy Synthes Spine and Medtronic; support for development of educational presentations from Medtronic. M.P.G. receives support from the Children’s Spine Foundation and Growing Spine Study Group. S.J.L. receives support for consultancy from Medtronic and Stryker; lecture/speaking bureau support from Medtronic and Stryker; patent with Medtronic; royalties with Globus and Lippincott. S.G. receives support for consultancy from DePuy Synthes Spine. J.R.S. receives grant support from Medicrea Spine, lectures/speaking bureau support from DePuy Synthes Spine and Medtronic Spine, Royalties from Elsivier. J.T.S. has board membership with the Children’s Spine Foundation; support for consultancy from DePuy Synthes Spine and Spineguard; royalties from DePuy. J.M.F. receives royalties from Biomet and Lippincott Williams & Wilkins. M.G.V. receives grant funding from Children’s Spine Foundation, Cerebral Palsy International Research Foundation, Pediatric Orthopaedic Society of North America, Scoliosis Research Society, OMeGA Medical Grant, Biomet, Children’s Spine Foundation, Orthopaedic Science Research Foundation; board member with Children’s Spine Foundation, Pediatric Orthopaedic Society of North America, International Pediatric Orthopaedic Symposium; support for consultancy from Stryker and Biomet; travel support from Biomet, Medtronic, DePuy, Synthes, Stryker, Fox, and Children’s Spine Foundation; other support from OMeGA, Biomet, and Orthopaedic Research and Education Foundation.
Footnotes
There are no disclosures to note regarding the National Institutes of Health, Wellcome Trust, and the Howard Hughes Medical Institute.
The remaining authors declare no conflicts of interest.
References
- 1.Fernandes P, Weinstein SL. Natural history of early onset scoliosis. J Bone Joint Surg Am. 2007;89(suppl 1):21–33. doi: 10.2106/JBJS.F.00754. [DOI] [PubMed] [Google Scholar]
- 2.Chandran S, McCarthy J, Noonan K, et al. Early treatment of scoliosis with growing rods in children with severe spinal muscular atrophy: a preliminary report. J Pediatr Orthop. 2011;31:450–454. doi: 10.1097/BPO.0b013e31821722b1. [DOI] [PubMed] [Google Scholar]
- 3.Gillingham BL, Fan RA, Akbarnia BA. Early onset idiopathic scoliosis. J Am Acad Orthop Surg. 2006;14:101–112. doi: 10.5435/00124635-200602000-00005. [DOI] [PubMed] [Google Scholar]
- 4.Hedequist D, Emans J. Congenital scoliosis: a review and update. J Pediatr Orthop. 2007;27:106–116. doi: 10.1097/BPO.0b013e31802b4993. [DOI] [PubMed] [Google Scholar]
- 5.Yang JS, McElroy MJ, Akbarnia BA, et al. Growing rods for spinal deformity: characterizing consensus and variation in current use. J Pediatr Orthop. 2010;30:264–270. doi: 10.1097/BPO.0b013e3181d40f94. [DOI] [PubMed] [Google Scholar]
- 6.Vitale MG, Gomez JA, Matsumoto H, et al. Variability of expert opinion in treatment of early-onset scoliosis. Clin Orthop Relat Res. 2011;469:1317–1322. doi: 10.1007/s11999-010-1540-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Samdani AF, Ranade A, Dolch HJ, et al. Bilateral use of the vertical expandable prosthetic titanium rib attached to the pelvis: a novel treatment for scoliosis in the growing spine. J Neurosurg Spine. 2009;10:287–292. doi: 10.3171/2008.12.SPINE08427. [DOI] [PubMed] [Google Scholar]
- 8.Thompson GH, Akbarnia BA, Kostial P, et al. Comparison of single and dual growing rod techniques followed through definitive surgery: a preliminary study. Spine. 2005;30:2039–2044. doi: 10.1097/01.brs.0000179082.92712.89. [DOI] [PubMed] [Google Scholar]
- 9.Bess S, Akbarnia BA, Thompson GH, et al. Complications of growing-rod treatment for early-onset scoliosis: analysis of one hundred and forty patients. J Bone Joint Surg Am. 2010;92:2533–2543. doi: 10.2106/JBJS.I.01471. [DOI] [PubMed] [Google Scholar]
- 10.Akbarnia BA, Marks DS, Boachie-Adjei O, et al. Dual growing rod technique for the treatment of progressive early-onset scoliosis: a multicenter study. Spine. 2005;30:S46–S57. doi: 10.1097/01.brs.0000175190.08134.73. [DOI] [PubMed] [Google Scholar]
- 11.Garbuz DS, Masri BA, Esdaile J, et al. Classification systems in orthopaedics. The Journal of the American Academy of Orthopaedic Surgeons. 2002;10:290–297. doi: 10.5435/00124635-200207000-00007. [DOI] [PubMed] [Google Scholar]
- 12.Williams BA, McCalla D, Matsumoto H, et al. Development and initial validation of the Classification of Early-Onset Scoliosis (C-EOS) J Bone Joint Surg Am. 2014;96:1359–1367. doi: 10.2106/JBJS.M.00253. [DOI] [PubMed] [Google Scholar]
- 13.Audigé L, Bhandari M, Hanson B, et al. A concept for the validation of fracture classifications. J Orthop Trauma. 2005;19:401–406. doi: 10.1097/01.bot.0000155310.04886.37. [DOI] [PubMed] [Google Scholar]
- 14.Akbarnia BA, Emans JB. Complications of growth-sparing surgery in early onset scoliosis. Spine. 2010;35:2193–2204. doi: 10.1097/BRS.0b013e3181f070b5. [DOI] [PubMed] [Google Scholar]
- 15.Reinker K, Simmons JW, Patil V, et al. Can VEPTR(®) control progression of early-onset kyphoscoliosis? A cohort study of VEPTR(®) patients with severe kyphoscoliosis. Clin Orthop Relat Res. 2011;469:1342–1348. doi: 10.1007/s11999-010-1697-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Campbell RM, Jr, Smith MD. Thoracic insufficiency syndrome and exotic scoliosis. J Bone Joint Surg Am. 2007;89(suppl 1):108–122. doi: 10.2106/JBJS.F.00270. [DOI] [PubMed] [Google Scholar]
- 17.Nectoux E, Giacomelli MC, Karger C, et al. Complications of the Luque-Galveston scoliosis correction technique in paediatric cerebral palsy. Orthop Traumatol Surg Res. 2010;96:354–361. doi: 10.1016/j.otsr.2010.01.004. [DOI] [PubMed] [Google Scholar]
- 18.Parsch D, Geiger F, Brocai DR, et al. Surgical management of paralytic scoliosis in myelomeningocele. J Pediatr Orthop B. 2001;10:10–17. [PubMed] [Google Scholar]
- 19.Schroerlucke SR, Akbarnia BA, Pawelek JB, et al. How does thoracic kyphosis affect patient outcomes in growing rod surgery? Spine. 2012;37:1303–1309. doi: 10.1097/BRS.0b013e318246d8a0. [DOI] [PubMed] [Google Scholar]
- 20.Reames DL, Smith JS, Fu KM, et al. Complications in the surgical treatment of 19,360 cases of pediatric scoliosis: a review of the Scoliosis Research Society Morbidity and Mortality database. Spine. 2011;36:1484–1491. doi: 10.1097/BRS.0b013e3181f3a326. [DOI] [PubMed] [Google Scholar]
- 21.McElroy MJ, Shaner AC, Crawford TO, et al. Growing rods for scoliosis in spinal muscular atrophy: structural effects, complications, and hospital stays. Spine. 2011;36:1305–1311. doi: 10.1097/BRS.0b013e3182194937. [DOI] [PubMed] [Google Scholar]
- 22.Master DL, Son-Hing JP, Poe-Kochert C, et al. Risk factors for major complications after surgery for neuromuscular scoliosis. Spine. 2011;36:564–571. doi: 10.1097/BRS.0b013e3181e193e9. [DOI] [PubMed] [Google Scholar]
- 23.Lipton GE, Miller F, Dabney KW, et al. Factors predicting postoperative complications following spinal fusions in children with cerebral palsy. J Spinal Disord. 1999;12:197–205. [PubMed] [Google Scholar]
- 24.Schroerlucke SR, et al. How does thoracic kyphosis affect patient outcomes in growing rod surgery? Spine. 2012;37:1303–1309. doi: 10.1097/BRS.0b013e318246d8a0. [DOI] [PubMed] [Google Scholar]