Abstract
Objective:
To investigate changes in body ownership and chronic neuropathic pain in patients with spinal cord injury (SCI) using multisensory own body illusions and virtual reality (VR).
Methods:
Twenty patients with SCI with paraplegia and 20 healthy control participants (HC) participated in 2 factorial, randomized, repeated-measures design studies. In the virtual leg illusion (VLI), we applied asynchronous or synchronous visuotactile stimulation to the participant's back (either immediately above the lesion level or at the shoulder) and to the virtual legs as seen on a VR head-mounted display. We tested the effect of the VLI on the sense of leg ownership (questionnaires) and on perceived neuropathic pain (visual analogue scale pain ratings). We compared illusory leg ownership with illusory global body ownership (induced in the full body illusion [FBI]), by applying asynchronous or synchronous visuotactile stimulation to the participant's back and the back of a virtual body as seen on a head-mounted display.
Results:
Our data show that patients with SCI are less sensitive to multisensory stimulations inducing illusory leg ownership (as compared to HC) and that leg ownership decreased with time since SCI. In contrast, we found no differences between groups in global body ownership as tested in the FBI. VLI and FBI were both associated with mild analgesia that was only during the VLI specific for synchronous visuotactile stimulation and the lower back position.
Conclusions:
The present findings show that VR exposure using multisensory stimulation differently affected leg vs body ownership, and is associated with mild analgesia with potential for SCI neurorehabilitation protocols.
Spinal cord damage can cause permanent loss of sensorimotor functions and persistent neuropathic pain,1–4 leading to structural and functional changes in somatotopic regions of the CNS.1,5 Recently, several studies showed that multisensory processing and the related sense of body ownership6–8 are also impaired in patients with spinal cord injury (SCI),9–11 suggesting that sensory impairments in SCI extend beyond unimodal deficits in the sensorimotor system. Although pain perception and leg and global body ownership can be experimentally manipulated through body illusions using multisensory stimulation,12–21 previous SCI research only investigated ownership for the upper extremity.9,11,22 Although virtual reality (VR) is becoming increasingly used in neurorehabilitation23,24 (see appendix e-1 at Neurology.org), it has only rarely been integrated with multisensory stimulation, in particular for the legs and in SCI.
We investigated leg and global body ownership in patients with SCI employing VR technology, using adapted virtual leg illusion (VLI)12 and full body illusion (FBI),13 respectively, and tested their potential analgesic effects. In the VLI, we simultaneously stroked virtual legs and the patient's nearest body site with preserved tactile perception (lower back), investigating whether such multisensory VR exposure induces leg ownership and illusory tactile leg percepts. Based on the findings on cortical reorganization after denervation,1,17 we predicted that synchronous stimulation of the lower back would result in a stronger illusion and analgesia than stimulation of a more distant site (upper back). We further predicted finding differences between patients with SCI and healthy control participants (HCs) for leg ownership (VLI), but not for the global sense of body ownership (FBI), as tested separately with distinct multisensory stimulations.
METHODS
Participants.
A total of 20 patients (2 female; 23–71 years, mean 47.3 ± 12.0 years) with SCI participated in the study. SCI was traumatic in 18 cases and nontraumatic in 2 cases. The time since injury varied between 3.5 months and 71 years (17.1 ± 18.1 years). According to the International Standards for Neurologic Classification of Spinal Cord Injury by the American Spinal Cord Injury Association (ASIA),25 their lesions ranged from high thoracal (T2) to lumbar (L2); 15 participants had complete lesions (ASIA Impairment Scale [AIS] A), 3 sensory incomplete (AIS B), and 2 sensory and motor incomplete (AIS C) lesions. All participants with SCI had impaired tactile perception of the upper dorsal legs. None of the participants with SCI had a history of other neurologic or psychiatric disease. Eleven participants with SCI had chronic neuropathic pain at or below the SCI level (SCI-pain),26 as defined by a prior clinical assessment. Demographic and clinical data of the SCI group are summarized in table e-1. Twenty healthy age-matched participants (2 female; 23–70 years, mean 43.0 ± 11.8 years; p = 0.975) were recruited as a control sample (HCs).
Standard protocol approvals, registrations, and patient consents.
The local ethics committees approved the study protocol, which was conducted in accordance with the ethical standards of the Declaration of Helsinki. All participants were informed about the experimental procedure and gave their written informed consent prior to the study (for an example, see e-consent).
Experimental paradigms and design.
Virtual leg illusion.
We adapted the VLI protocol12 to the present investigation of patients with SCI. Due to the impaired tactile perception in legs of the patients with SCI, we applied the visuotactile conflict between the seen virtual legs and the participant's back (tactile stimulation). The participants sat in a wheelchair and wore a head-mounted display (HMD; figure 1A). Fake legs were placed on another chair, mimicking a sitting posture. A camera was mounted above, corresponding to the participant's first-person viewpoint. The real-time video recording of virtual legs was fed to the HMD, appearing as superimposed over participants' physical legs, while the experimenter simultaneously stroked the participant's lateral back and the corresponding upper dorsal part of the ipsilateral virtual leg. Thus, the participants observed the virtual legs being touched simultaneously while they received touches on their back (figure 1A). Based on the findings on cortical reorganization after SCI (i.e., shift of neighboring cortical areas towards the denervated region5), we applied tactile stimulation to the lower back (immediately above SCI level) or to the upper back (distant, control site).
Figure 1. Experimental setups.
(A) In the virtual leg illusion (VLI) paradigm, the participant sits in a wheelchair and wears a head-mounted display (HMD) and headphones. The experimenter simultaneously strokes the lower or upper part of the participant's back and the corresponding part of the dummy leg. The camera films dummy legs from the distance and angle that corresponds to the participant's first-person viewpoint, and the real-time video recording is projected onto the HMD. Thus, the participant sees touch cues applied to the virtual legs while being touched on the back. (B) In the full body illusion (FBI) paradigm, the participant sits in a wheelchair and wears headphones and an HMD. A video camera, standing 2 meters behind, films the participant's back, while the experimenter is applying tactile stimulation to the participant's back with a wooden stick. The real-time (delayed for 800 ms in asynchronous condition) video is projected onto the HMD. The participant thus sees his or her own virtual body projected in front and being touched with the stick, while at the same time feels being touched on the back.
In a 2 × 2 repeated measures design, we manipulated the synchrony between the stroking of the virtual legs (synchronous, asynchronous) and the participant's back location (lower, upper back). In the synchronous condition, the stroking of the virtual legs was synchronized with the stroking of the participant's back. In the asynchronous condition, the visuotactile stimulation was delayed (approximately 1 second of delay). Each condition lasted for 60 seconds.
Full body illusion.
We manipulated global body ownership through an adapted FBI protocol.13 The participants sat in a wheelchair and wore an HMD. A camera, positioned 2 meters behind, filmed the participant's back, which the experimenter stroked. The real-time video was projected onto the HMD. The participants thus viewed their own body projected in front (virtual body) and were simultaneously stimulated on their back (figure 1B). This visuotactile stimulation (60 seconds) was synchronous or asynchronous (800 ms of the video delay).
Assessments.
The VLI was assessed with a 9-item questionnaire, adapted from body illusions studies,13–15 with items referring to the experienced ownership for the virtual legs, illusory touch, and referred touch. The FBI was assessed with a 7-item questionnaire,13 referring to the experienced ownership for the virtual body and illusory touch on the virtual body. Both questionnaires contained control items. All items are shown in table e-2. Participants rated the questionnaires on a 7-point Likert scale (−3, completely disagree; +3, completely agree). We assessed the intensity of actual neuropathic pain with a visual analogue scale (VAS) ranging from 0 (no pain) to 100 (worst pain imagined).27 We assessed the presence of unusual body experiences with the Cambridge Depersonalization Scale (CDS).28
Procedure.
We first conducted a short semi-structured interview with the SCI participants about their SCI, related pain, and bodily sensations, followed by the CDS administration. Before the experiment started, the experimenter carefully defined the level above which each patient had intact tactile perception on the back to ascertain the detectability of tactile stimulations. All patients with SCI with neuropathic pain rated the intensity of current pain on the VAS (baseline). The VLI and FBI protocol were then carried out in a counterbalanced order across participants. After each experimental condition, the participants rated the current neuropathic pain (only SCI-pain), the VLI, or FBI questionnaire (all participants). The order of the VLI conditions was randomized across patients, and the order of the FBI conditions counterbalanced.
Statistical analyses.
The FBI and VLI illusion questionnaire ratings were first ipsatized using individual mean rating29 (appendix e-1) and then averaged based on the measured component (tables e-2 and e-3). The VLI questionnaire scores were analyzed with a mixed analysis of variance (ANOVA), with synchrony (synchronous, asynchronous) and back location (lower back, upper back) as within-subjects factors and group (SCI, HC) as a between-subjects factor. The FBI questionnaire scores were analyzed with a mixed design ANOVA, with synchrony (synchronous, asynchronous) as a within-subjects factor and group (SCI, HC) as a between-subjects factor.
Linear and exponential curve estimations were performed for the relationship between the illusion ratings and the time since lesion or the SCI level; this was done for the synchronous–lower back and synchronous–upper back conditions in the VLI and the synchronous condition in the FBI. The questionnaire data were linearly transformed to non-zero positive values. To quantify the level of injury, we considered the SCI level as an integer ascribed to the ASIA-defined lesion level, ranging from 1 (lesion at T2) to 13 (lesion at L2).10 If the lesion was defined between 2 neurologic levels, the score was calculated as the average of 2 integers (e.g., a T6/T7 lesion was scored with 5.5).
For the subgroup of patients with SCI with neuropathic pain (n = 11), the baseline pain rating was first subtracted from the postcondition pain ratings to obtain measures of pain modulation (pain change), which were then analyzed with repeated-measures ANOVA (VLI; 2 [synchrony] × 2 [back location] factorial design) and paired sample t test (FBI). The significance (α) level used was 0.05. One-tailed one-sample t tests were used to infer whether the pain change is significantly lower than zero (using Bonferroni method for multiple comparisons correction: FBI: αcorr = α/2 = 0.025; VLI: αcorr = α/4 = 0.0125).
In addition, we analyzed differences between SCI subgroups in their experience of VLI and FBI: between SCI with and without any preserved tactile sensation, between SCI with and without neuropathic pain, and between SCI with complete and incomplete SCI. We used mixed ANOVA with synchrony and back location (in VLI) as within-subjects and respective subgroups as between-subjects factors (appendix e-1).
We scored the CDS ratings according to Sierra and Berrios.28 Based on a previous study showing increased occurrence of altered body perception in SCI,9 we focused the analyses on the items in the Anomalous Body Experience (ABE) subscale,30 using nonparametric Mann-Whitney U.
RESULTS
Virtual leg illusion.
We found significant main effects of synchrony, where synchronous visuotactile stimulation induced a stronger experience of illusory ownership for the virtual legs (p = 0.037), stronger sensations of illusory touch (p = 0.008), and stronger referred touch (p < 0.001), without significantly affecting the ratings of the control items (p = 0.112). We found a significant main effect of group on the ratings of illusory ownership (p = 0.028), showing that patients with SCI experienced weaker illusory leg ownership than HC, independently of the synchrony of stroking (interaction: p = 0.263). No such group differences were found in the ratings of illusory touch, referred touch, or control items (all p ≥ 0.153). These findings suggest that SCI experienced weaker leg ownership, but equally strong illusory touch sensations as HC. We did not find any significant main effect of back location or interaction effects (all p ≥ 0.063). We did not find any significant differences in the illusion or control ratings between the patients with SCI with and without preserved tactile leg sensations (all p ≥ 0.096; table e-4), between the participants with SCI with and without neuropathic pain (all p ≥ 0.075; table e-5), or between the participants with SCI with complete and incomplete lesions (all p ≥ 0.103; table e-6).
A significant exponentially decaying relationship was found between duration of SCI and the magnitude of illusory leg ownership (p = 0.016) and between duration of SCI and the magnitude of illusory referred touch (p = 0.036). Importantly, both findings were only observed in the condition in which the lower back was stroked synchronously (other conditions: all p ≥ 0.081). No significant correlations were found between the illusory ratings and the level of SCI (all p ≥ 0.125). Statistical results are shown in table e-3.
We did not find any significant main effects of synchrony, back location, or interactions on the pain change ratings between the postillusion and the baseline ratings (all p ≥ 0.147). However, when comparing the pain change against zero, we found a significant pain reduction when the lower back was stimulated synchronously with the virtual legs (p = 0.04), but not in any of the other conditions (all p ≥ 0.188). However, this comparison did not survive correction for multiple comparisons: αcorr = 0.0125. See table 1 for statistical reports and figure 2 for a graphic presentation of results.
Table 1.
Analysis of variance results for the questionnaire ratings in the virtual leg illusion (VLI)

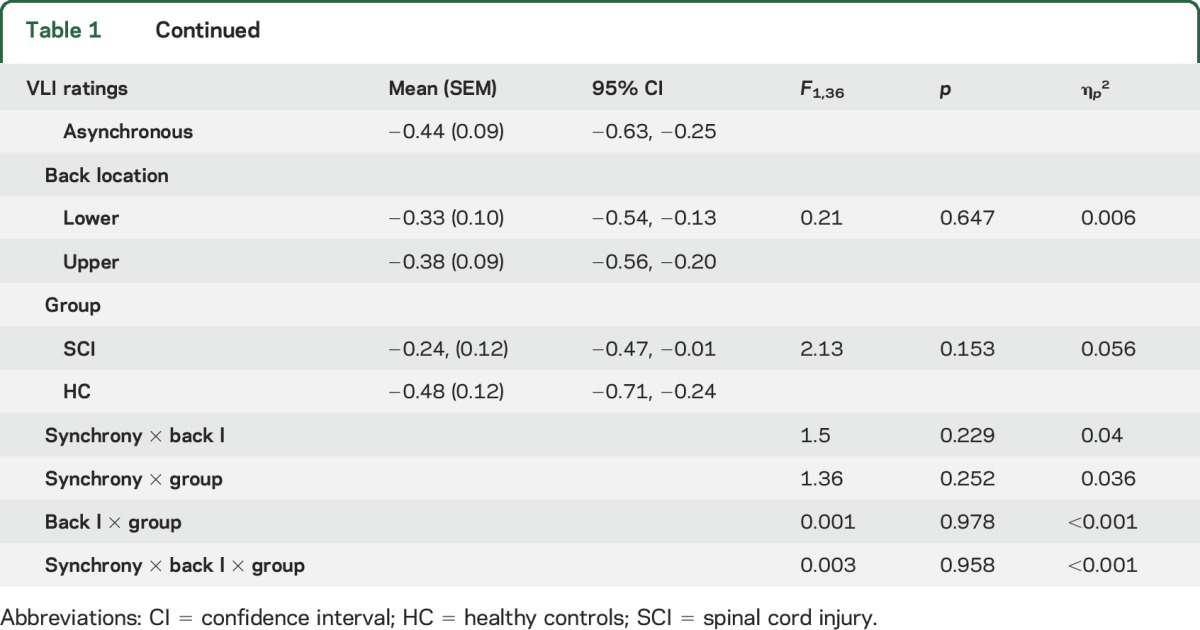
Figure 2. Virtual leg illusion (VLI) results.
(A) Mean ipsatized ratings of the VLI questionnaire items: significant main effects of synchrony were found for the ratings of ownership, illusory touch, and referred touch. Significant main effect of group was found for the ratings of ownership. (B) Mean differences in neuropathic pain between baseline and postcondition ratings in the VLI. (C) Exponential decaying relationship between the time since lesion and ratings of ownership (C.a) or referred touch (C.b) in The VLI: significant relationships between the illusion and time since lesion were found for synchronous stimulation of lower back, but not upper back. Async = asynchronous; HC = control group; L back = lower back; Sync = synchronous; SCI = spinal cord injury group; U back = upper back. SCI HC *p < 0.05, **p < 0.010, ***p < 0.001. Error bars show standard error of the mean.
Full body illusion.
We found significant main effects of synchrony, where synchronous visuotactile stimulation induced stronger illusory body ownership (p < 0.001) and stronger illusory touch (p < 0.001) as compared to asynchronous stimulation, but it did not significantly modulate the ratings of control items (p = 0.823). In contrast to the VLI, we did not find significant main effects of group (all p ≥ 0.558) or interaction effects (all p ≥ 0.146) on any of the FBI questionnaire items. No differences in the illusion or control ratings were found between participants with SCI with and without preserved tactile leg sensations (all p ≥ 0.481; table e-4), between participants with SCI with and without neuropathic pain (all p ≥ 0.332; table e-5), or between participants with SCI with complete and incomplete lesions (all p ≥ 0.173; table e-6). No significant correlations were found between ratings on body ownership and illusory touch with SCI duration or with SCI level (all p ≥ 0.052; table e-3).
Concerning pain ratings, the synchrony of visuotactile stimulation did not modulate the pain change (p = 0.920). However, the FBI significantly reduced the pain compared to baseline measurements in both the synchronous (p = 0.020) and asynchronous (p = 0.020) visuotactile stimulation conditions (table 2 and figure 3).
Table 2.
Analysis of variance results for the questionnaire items in the full body illusion (FBI) and pain change in the virtual leg illusion (VLI) and the FBI


Figure 3. Full body illusion (FBI) results.
(A) Mean ipsatized ratings of the FBI questionnaire items: significant main effects of synchrony were found for the ratings of ownership and illusory touch, but not for control items. The differences between the groups were not significant. (B) Mean differences in neuropathic pain between baseline and postcondition ratings for synchronous and asynchronous condition in the FBI: significant main effect of synchrony was found for the ratings of ownership, illusory touch, and referred touch. Significant main effect of group was found for the ownership ratings. Async = asynchronous; HC = control group; SCI = spinal cord injury group; Sync = synchronous. *p < 0.05, ***p < 0.001. Error bars show standard error of the mean.
Cambridge Depersonalization Scale.
No significant differences between the participants with SCI and HC were found for the total CDS or ABE subscale scores (all p ≥ 0.260). However, the participants with SCI rated significantly higher 2 individual items that are related to leg/body ownership: “Parts of my body feel as if they didn't belong to me” (p = 0.028) and “I have to touch myself to make sure that I have a body or a real existence” (p = 0.009) (see table e-7 for statistical results).
DISCUSSION
We investigated SCI-related alterations of bodily self-consciousness through multisensory body illusion paradigms using VR. In particular, we tested whether the sensitivity to experimental manipulations of leg and body ownership is affected by SCI, and whether such multisensory stimulation has analgesic effects.
In the VLI paradigm, participants received tactile stimulation on their back while viewing, through an HMD, the virtual legs being touched. This manipulation, when temporally synchronous, is generally associated with stronger integration (as compared to asynchronous) of visual, proprioceptive, and tactile information12; here we show for the first time that it results in the illusory sensation that touching the virtual legs is causing the touch on the back (referred touch) and to a lesser extent in illusory touch on the legs in both SCI and HC groups. Important for understanding the effect of SCI on central leg representations, the SCI group showed a general reduction across conditions in proneness to experience virtual legs as one's own, indicating that individuals with paraplegia less readily integrate the available visual and tactile information to experience illusory leg ownership. Moreover, time since injury negatively correlated with illusory leg ownership and referred touch, suggesting that with prolonged sensorimotor deficits, patients with SCI become even more resistant in their decreased sensitivity to the VLI. This may potentially be associated with alterations in central multisensory leg representations, and stronger reliance on off-line leg representations, as previously reported for upper limb amputees and the strength of the rubber hand illusion (RHI).31
We did not find any differences in the VLI between the lower and upper back stimulation conditions. Differences would have been compatible with SCI-induced changes in cortical reorganization in primary somatosensory cortex (S1), as shown for hand-face remapping effects in patients with tetraplegia during the RHI.11 This negative finding thus indirectly suggests that other, multisensory leg representations (for example, in posterior parietal cortex8) and not S1 are involved in mediating the effects of the VLI, also supported by the negative correlation between the time since SCI and VLI ratings. Alternatively, the absence of the stimulation site effect could also be due to the relatively larger receptive fields on the back in S1 (as compared to hand or face), with both stimulations activating closely similar locations in S1 and in higher-tier areas.32
In contrast to these VLI findings, we found no differences between SCI and HC in the FBI, which in comparison to paradigms where the focus of the visuotactile stimulation is a body part (RHI15 or VLI12) enables experimental manipulation of more global aspects of bodily self-consciousness, affecting ownership for the entire body.13,33 In the current study we extended earlier findings13,34 showing that synchronous (as compared to asynchronous) visuotactile stimulation induces stronger illusory ownership not just in HC but also in patients with SCI, suggesting that the chronic denervation of the lower trunk and legs in SCI does not alter the multisensory mechanisms important for global aspects of bodily self-consciousness.13,34,35 We note that visuotactile stimulation in the FBI was applied at a body site with fully preserved sensory functionality (upper trunk, above the lesion level), which, however, was also the case during all conditions of the VLI, suggesting differential recruitment of multisensory bodily integration processes in patients with SCI in both VR illusion paradigms.
We also investigated whether the present multisensory VR paradigms modulate neuropathic pain. Despite the overall mild analgesic effects in the VLI, we observed that only synchronous visuotactile stimulation in the back condition (associated with the strongest experience of the VLI) resulted in a near significant reduction of neuropathic pain. This somatotopy-related analgesia (and VLI induction) suggests that this particular experimental manipulation might activate otherwise silent cortical regions representing the lower limbs, arguing for a potential central co-representation of pain and the multisensory VLI. We speculate that the stimulation may have transiently interfered with abnormally altered leg representations in SCI, arguably involved in the central origins of neuropathic pain18,36 and previously explored using the RHI for alleviating neuropathic pain in upper limb amputees.18 We found a condition-nonspecific mild analgesic effect of the FBI, which is potentially related to so-called visual analgesia (i.e., seeing one's own body already has analgesic effects in healthy participants)21,37–39 or previously reported distraction effects of VR.40 Future work is needed to investigate these differences.
Our results need to be interpreted with caution; the SCI sample with neuropathic pain was relatively small and clinically heterogeneous. Although excluding 2 patients with nontraumatic SCI from our analyses showed only slight deviations in our results (see appendix e-1), future studies should focus on larger cohorts of different SCI subgroups with uniform clinical presentations and etiology to replicate the present findings. These studies should preferably use prolonged and repeated stimulation and test different multisensory stimulation patterns including different body locations. These changes may boost the currently observed pain reduction and enable us to draw firmer conclusions about the paradigm's analgesic effects. Nevertheless, the present findings are relevant for the design of noninvasive SCI neurorehabilitation and pain management protocols, suggesting the importance of early interventions to strengthen multisensory body representation in the SCI population. Further work may also consider testing the current VR methodology and its analgesic effects in other acute and chronic pain conditions (see appendix e-1), such as complex regional pain syndrome, diabetic neuropathy, or multiple sclerosis.
Supplementary Material
ACKNOWLEDGMENT
Dr. Andrea Serino (Laboratory of Cognitive Neuroscience, Brain Mind Institute, School of Life Sciences, Ecole Polytechnique Fédérale de Lausanne, Switzerland) contributed to the manuscript with scientific advice.
GLOSSARY
- ABE
Anomalous Body Experience
- AIS
American Spinal Cord Injury Association Impairment Scale
- ANOVA
analysis of variance
- ASIA
American Spinal Cord Injury Association
- CDS
Cambridge Depersonalization Scale
- FBI
full body illusion
- HC
healthy controls
- HMD
head-mounted display
- RHI
rubber hand illusion
- SCI
spinal cord injury
- VAS
visual analogue scale
- VLI
virtual leg illusion
- VR
virtual reality
Footnotes
Supplemental data at Neurology.org
AUTHOR CONTRIBUTIONS
Dr. Pozeg: study concept and design, acquisition of data, analysis and interpretation of data, manuscript drafting, obtaining funding. Dr. Palluel: study concept and design, acquisition of data, manuscript drafting, obtaining funding. Dr. Ronchi: interpretation of data, study supervision, manuscript drafting. Dr. Solcà: acquisition and interpretation of data. Dr. Al-Khodairy: study concept and design, acquisition of data. Dr. Jordan: acquisition and interpretation of data. Dr. Kassouha: acquisition and interpretation of data. Dr. Blanke: study concept and design, interpretation of data, obtaining funding, study supervision, critical revision of manuscript for intellectual content.
STUDY FUNDING
Supported by International Foundation for Research in Paraplegia (P143). The Article Processing Charge was funded by the International Foundation for Research in Paraplegia.
DISCLOSURE
The authors report no disclosures relevant to the manuscript. Go to Neurology.org for full disclosures.
REFERENCES
- 1.Wrigley PJ, Press SR, Gustin SM, et al. Neuropathic pain and primary somatosensory cortex reorganization following spinal cord injury. Pain 2009;141:52–59. [DOI] [PubMed] [Google Scholar]
- 2.Siddall PJ, Taylor DA, McClelland JM, Rutkowski SB, Cousins MJ. Pain report and the relationship of pain to physical factors in the first 6 months following spinal cord injury. Pain 1999;81:187–197. [DOI] [PubMed] [Google Scholar]
- 3.Melzack R, Loeser JD. Phantom body pain in paraplegics: evidence for a central “pattern generating mechanism” for pain. Pain 1978;4:195–210. [DOI] [PubMed] [Google Scholar]
- 4.Brinkhof M, Al-Khodairy A, Eriks-Hoogland I, et al. Health conditions in people with spinal cord injury: contemporary evidence from a population-based community survey in Switzerland. J Rehabil Med 2016;48:197–209. [DOI] [PubMed] [Google Scholar]
- 5.Henderson LA, Gustin SM, Macey PM, Wrigley PJ, Siddall PJ. Functional reorganization of the brain in humans following spinal cord injury: evidence for underlying changes in cortical anatomy. J Neurosci 2011;31:2630–2637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Blanke O. Multisensory brain mechanisms of bodily self-consciousness. Nat Rev Neurosci 2012;13:556–571. [DOI] [PubMed] [Google Scholar]
- 7.Serino A, Alsmith A, Costantini M, Mandrigin A, Tajadura-Jimenez A, Lopez C. Bodily ownership and self-location: components of bodily self-consciousness. Conscious Cogn 2013;22:1239–1252. [DOI] [PubMed] [Google Scholar]
- 8.Blanke O, Slater M, Serino A. Behavioral, neural, and computational principles of bodily self-consciousness. Neuron 2015;88:145–166. [DOI] [PubMed] [Google Scholar]
- 9.Lenggenhager B, Pazzaglia M, Scivoletto G, Molinari M, Aglioti SM. The sense of the body in individuals with spinal cord injury. PLoS One 2012;7:e50757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Scandola M, Aglioti SM, Pozeg P, Avesani R, Moro V. Motor imagery in spinal cord injured people is modulated by somato-topic coding, perspective taking and post-lesional chronic pain. J Neuropsychol 2016;34:603–613. [DOI] [PubMed] [Google Scholar]
- 11.Scandola M, Tidoni E, Avesani R, Brunelli G, Aglioti SM, Moro V. Rubber hand illusion induced by touching the face ipsilaterally to a deprived hand: evidence for plastic somatotopical remapping in tetraplegics. Front Hum Neurosci 2014;8:404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pozeg P, Galli G, Blanke O. Those are your legs: the effect of visuo-spatial viewpoint on visuo-tactile integration and body ownership. Front Psychol 2015;6:1749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lenggenhager B, Tadi T, Metzinger T, Blanke O. Video ergo sum: manipulating bodily self-consciousness. Science 2007;317:1096–1099. [DOI] [PubMed] [Google Scholar]
- 14.Ehrsson HH. The experimental induction of out-of-body experiences. Science 2007;24:1048. [DOI] [PubMed] [Google Scholar]
- 15.Botvinick M, Cohen J. Rubber hands “feel” touch that eyes see. Nature 1998;391:756. [DOI] [PubMed] [Google Scholar]
- 16.Romano D, Pfeiffer C, Maravita A, Blanke O. Illusory self-identification with an avatar reduces arousal responses to painful stimuli. Behav Brain Res 2014;261:275–281. [DOI] [PubMed] [Google Scholar]
- 17.Ramachandran VS, Rogers-Ramachandran DC, Cobb S. Touching the phantom limb. Nature 1995;377:489–490. [DOI] [PubMed] [Google Scholar]
- 18.Schmalzl L, Ragnö C, Ehrsson HH. An alternative to traditional mirror therapy: illusory touch can reduce phantom pain when illusory movement does not. Clin J Pain 2013;29:e8–e10. [DOI] [PubMed] [Google Scholar]
- 19.Soler MD, Kumru H, Pelayo R, et al. Effectiveness of transcranial direct current stimulation and visual illusion on neuropathic pain in spinal cord injury. Brain 2010;133:2565–2577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hänsel A, Lenggenhager B, von Känel R, Curatolo M, Blanke O. Seeing and identifying with a virtual body decreases pain perception. Eur J Pain 2011;15:874–879. [DOI] [PubMed] [Google Scholar]
- 21.Romano D, Llobera J, Blanke O. Size and viewpoint of an embodied virtual body affect the processing of painful stimuli. J Pain 2016;17:350–358. [DOI] [PubMed] [Google Scholar]
- 22.Lenggenhager B, Scivoletto G, Molinari M, Pazzaglia M. Restoring tactile awareness through the rubber hand illusion in cervical spinal cord injury. Neurorehabil Neural Repair 2013;27:704–708. [DOI] [PubMed] [Google Scholar]
- 23.Lenggenhager B, Arnold CA, Giummarra MJ. Phantom limbs: pain, embodiment, and scientific advances in integrative therapies. Wiley Interdiscip Rev Cogn Sci 2014;5:221–231. [DOI] [PubMed] [Google Scholar]
- 24.Adamovich SV, Fluet GG, Tunik E, Merians AS. Sensorimotor training in virtual reality: a review. NeuroRehabilitation 2009;25:29–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kirshblum SC, Burns SP, Biering-Sorensen F, et al. International standards for neurological classification of spinal cord injury (revised 2011). J Spinal Cord Med 2011;34:535–546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Treede RD, Jensen TS, Campbell JN, et al. Neuropathic pain: redefinition and a grading system for clinical and research purposes. Neurology 2008;70:1630–1635. [DOI] [PubMed] [Google Scholar]
- 27.Hawker GA, Mian S, Kendzerska T, French M. Measures of adult pain: visual analog scale for pain (VAS pain), Numeric Rating Scale for pain (NRS pain), McGill Pain Questionnaire (MPQ), short-form McGill Pain Questionnaire (SF-MPQ), Chronic Pain Grade Scale (CPGS), Short Form-36 bodily pain scale (SF). Arthritis Care Res (Hoboken) 2011;63(suppl 1):S240–S252. [DOI] [PubMed] [Google Scholar]
- 28.Sierra M, Berrios GE. The Cambridge Depersonalisation Scale: a new instrument for the measurement of depersonalisation. Psychiatry Res 2000;93:153–164. [DOI] [PubMed] [Google Scholar]
- 29.Fischer R, Milfont TL. Standardization in psychological research. Int J Psychol Res 2010;3:88–96. [Google Scholar]
- 30.Sierra M, Baker D, Medford N, David A. Unpacking the depersonalization syndrome: an exploratory factor analysis on the Cambridge Depersonalization Scale. Psychol Med 2005;35:1523–1532. [DOI] [PubMed] [Google Scholar]
- 31.Ehrsson HH, Rosén B, Stockselius A, Ragnö C, Köhler P, Lundborg G. Upper limb amputees can be induced to experience a rubber hand as their own. Brain 2008;131:3443–3452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Saadon-Grosman N, Tal Z, Itshayek E, Amedi A, Arzy S. Discontinuity of cortical gradients reflects sensory impairment. Proc Natl Acad Sci 2015;112:16024–16029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Blanke O, Metzinger T. Full-body illusions and minimal phenomenal selfhood. Trends Cogn Sci 2009;13:7–13. [DOI] [PubMed] [Google Scholar]
- 34.Aspell JE, Lenggenhager B, Blanke O. Keeping in touch with one's self: multisensory mechanisms of self-consciousness. PLoS One 2009;4:e6488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Noel J-P, Pfeiffer C, Blanke O, Serino A. Peripersonal space as the space of the bodily self. Cognition 2015;144:49–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ramachandran VS, Altschuler EL. The use of visual feedback, in particular mirror visual feedback, in restoring brain function. Brain 2009;132:1693–1710. [DOI] [PubMed] [Google Scholar]
- 37.Mancini F, Longo MR, Kammers MPM, Haggard P. Visual distortion of body size modulates pain perception. Psychol Sci 2011;22:325–330. [DOI] [PubMed] [Google Scholar]
- 38.Longo MR, Betti V, Aglioti SM, Haggard P. Visually induced analgesia: seeing the body reduces pain. J Neurosci 2009;29:12125–12130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Longo MR, Iannetti GD, Mancini F, Driver J, Haggard P. Linking pain and the body: neural correlates of visually induced analgesia. J Neurosci 2012;32:2601–2607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Triberti S, Repetto C, Riva G. Psychological factors influencing the effectiveness of virtual reality-based analgesia: a systematic review. Cyberpsychol Behav Soc Netw 2014;17:335–345. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.





