Abstract
Young adult men-who-have-sex-with-men (YMSM) continue to have among the highest incidence of HIV infection in the United States. Pre-exposure prophylaxis (PrEP) is an effective and safe method of preventing HIV infection; however, despite US Food and Drug Administration approval, utilization remains low, in part, due to structural barriers, particularly access to healthcare. In this study, we used social media to recruit black, Hispanic, and white HIV-uninfected 18- to 24-year-old YMSM. Participants completed an online survey about their sexual behavior, healthcare access, and previous use of PrEP. Of the 2297 YMSM surveyed, only 3.4% had used PrEP. PrEP use was associated with higher levels of education, living alone, older age, higher levels of sexual activity, and greater healthcare access, specifically having healthcare insurance and a clinic or primary care provider (PCP) from whom they received care. Among PrEP nonusers, 65% met at least one of the US Centers for Disease Control and Prevention recommended indications for PrEP use, and of these, 59% had healthcare insurance and received care in a clinic and/or had a PCP. Multi-variable multi-nomial logistic regression modeling identified disparities in access to healthcare by age, race/ethnicity, education, and region. Specifically, older YMSM, blacks and Hispanics, those with fewer years of formal education, and residents of the southern and the western United States were more likely to lack healthcare access. These results demonstrate both potential opportunities and barriers to the scale-up of PrEP among YMSM.
Keywords: : HIV, YMSM, PrEP, healthcare
Introduction
The HIV epidemic continues to impact men-who-have-sex-with-men (MSM) disproportionally; in 2014, nearly two-thirds of all new HIV infections in the United States were among MSM, with increased prevalence among racial and ethnic minority MSM.1,2 Because young adult MSM (YMSM) are more likely to be undiagnosed1 and to not be virologically suppressed with antiretroviral medication,1,3 their sexual and/or injection drug partners particularly are vulnerable to infection.2 One highly effective and safe means of reducing HIV infection acquisition among YMSM is pre-exposure prophylaxis (PrEP).4–8 In 2012, the US Food and Drug Administration (FDA) approved the oral combination emtricitabine/tenofovir disoproxil fumarate as PrEP9 and in 2014, the US Public Health Service/Centers for Disease Control and Prevention (CDC) issued guidelines for the prescription of PrEP.10 Among MSM, PrEP use is indicated if they have had condomless anal intercourse (CAI) in the past 6 months and are not in a monogamous sexual partnership with a recently tested, HIV uninfected man. PrEP also is indicated for men who have sex with women if they are not in a monogamous sexual relationship, have had condomless sex with women in the past 6 months, and have also had CAI. Among injection drug users, sharing of injection or drug preparation equipment in the previous 6 months is a CDC indication for PrEP prescription.10
Despite FDA approval, CDC guidance, increasing awareness,11 and social acceptability of PrEP,11–14 its usage remains low in the United States among MSM,15,16 with lower rates especially among YMSM.17–19 Although initial research, as well as demonstration projects, largely focused on attitudes to PrEP, the need for appropriate messaging and promotion, and methods to promote adherence,14,20 there now exists a recognized need to consider the requirements for “real world” implementation of PrEP use among YMSM, particularly with regard to access to healthcare.21–23 Despite initial concerns about the appropriateness of PrEP prescriptions, particularly for men,24,25 studies have found support for PrEP among healthcare providers and have shown that healthcare providers play a critical role in awareness and uptake of PrEP among YMSM.18 Conversely, lack of health insurance coverage and limited or no engagement with the healthcare system have been identified as barriers to PrEP implementation.17,23,26–29
To fully realize the benefits of PrEP and ensure its increased use, there is a critical need to identify on a national scale YMSM who are most at risk for HIV acquisition and to assess their ability to access PrEP, particularly those YMSM who may not be engaged in the healthcare system.6 Everyday observation and research data demonstrate high levels of social media use by young adults, including YMSM, which make social media ideal vehicles for communicating with large numbers of YMSM about HIV prevention.30–32 As part of a national study of 18- to 24-year-old black, Hispanic, and white YMSM recruited through social media, we surveyed participants about their history of PrEP use, indications for PrEP use, and access to healthcare. To understand current PrEP usage patterns, potential for PrEP expansion, and possible barriers to its use, we first examined PrEP utilization and factors associated with its use among these YMSM. Among YMSM PrEP nonusers, we assessed their PrEP eligibility based on CDC guidelines and also their access to healthcare, as reflected in whether or not they had health insurance and/or a regular healthcare provider. Finally, we explored potential disparities in healthcare access among YMSM PrEP eligible nonusers; this information about access may help guide intervention efforts to expand PrEP usage for this higher HIV risk population.
Methods
Study setting and population
From August to December 2014, multiple social media platforms were used to recruit YMSM to complete an anonymous online survey. Although the parent study33 and its primary survey primarily focused on HIV testing, this study focuses on a portion of the primary survey about PrEP and associated topics. Those who were eligible to participate in the survey were English- or Spanish-speaking 18- to 24-year-old black, Hispanic, and white YMSM living in the United States, who had previously had anal sex with another man, never had an HIV positive test, and consented to the study. The sponsoring institution's institutional review board approved the study.
Survey development, content, measures, and administration
The study investigators developed the survey based on a review of existing studies on the topic. A group of 21 black, Hispanic, and white YMSM were recruited through social media for pilot testing of the survey instrument. These participants provided feedback on the survey's cultural and age appropriateness, as well as the understandability and usability of the instrument; modifications were made based on their feedback. The questions of the survey pertinent to this investigation include questions about ever using PrEP, healthcare insurance status, access to a primary care provider (PCP) or clinic, as well as previous sexual and injection drug use (IDU) history. Participants were asked, “Have you ever taken HIV PrEP (TRUVADA)?”;“Do you have a PCP (doctor, nurse practitioner, or physician assistant) or a clinic for your medical care?”; and “Do you have or are you covered by someone else's healthcare insurance?” These three questions had possible answers of yes and no. In terms of sexual history, questions included time of the most recent condomless sexual intercourse (with both men and women) with responses of time intervals of less than 1 month, 1–6 months, and over 6 months. Participants were also asked how many main, casual, and exchange male and female sexual partners with whom they had had condomless intercourse. A complete English-language copy of the questionnaire has been published previously.33
Analysis
Data analysis was completed using STATA 13 (Stata Corp, College Station, TX) and SAS 9.4 (SAS Institute, Cary, NC). Study eligibility and enrollment information were summarized. Participants who indicated they did not know, or refused to answer, if they had ever used PrEP were excluded from analysis. Missing data were not imputed. Demographic characteristics, healthcare access, and sexual behavior were compared between PrEP users and PrEP nonusers using Fisher's exact testing for discrete variables and Kruskal–Wallis testing for continuous variables. We further examined the characteristics of PrEP nonusers to assess their PrEP eligibility based on the CDC guidelines relevant to YMSM (CAI with another man in the past 6 months, sex with women in the past 6 months, or ever sharing of IDU equipment). Among PrEP-eligible participants, we calculated the proportions, with corresponding 95% confidence intervals (CIs), of those with potential ability to access PrEP as indicated by possessing healthcare insurance status and having access to a PCP/clinic. PrEP-eligible nonusers were compared to PrEP users, and PrEP-eligible nonusers were compared to non-PrEP eligible participants using the methods described above.
A multivariable multinomial model was constructed to identify demographic and social characteristics associated with decreased access to PrEP as reflected in a lack of healthcare insurance or availability of a PCP or clinic. Four groups were compared in the model: (1) those having both PCP/clinic and healthcare insurance (reference category); (2) those having neither PCP/clinic nor healthcare insurance; (3) those with a PCP/clinic, but no health insurance; and (4) those with no PCP/clinic, but health insurance. All covariates were included in a multi-variable model initially; afterward, covariates that were significant at the α = 0.05 level in this initial model were used to construct the final multi-variable model. Adjusted odds ratios with corresponding 95% CIs were estimated.
Results
Participant characteristics, PrEP use, and correlates of PrEP use
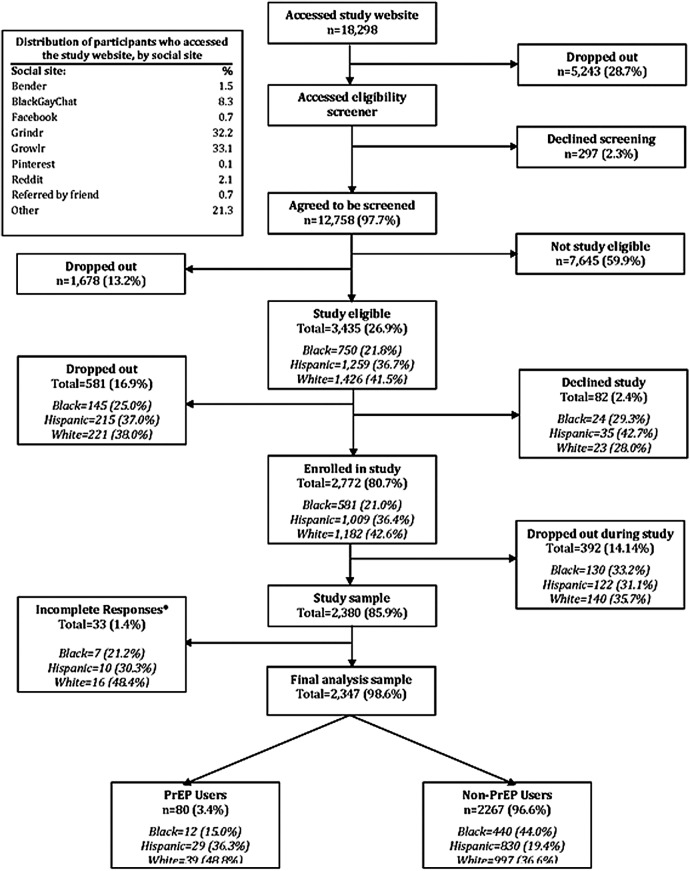
The final study sample consisted of 2347 18- to 24-year-old black, Hispanic, and white YMSM (Fig. 1). Of these participants, 80 (3.4%) reported ever using PrEP. PrEP use did not vary by racial/ethnic group: 2.7% (95% CI: 1.4–4.6%) of black participants, 3.4% (95% CI: 2.3–4.8%) of Hispanic participants, and 3.8% (95% CI: 2.7–5.1%) of white participants reported ever using PrEP. The median age of PrEP users was 23 years old; almost half were white and lived in the southern United States; and the overwhelming majority had at least some college education, lived in a large or medium city or a surrounding suburb, had a PCP or had access to a primary care clinic, and healthcare insurance (Table 1). Compared to PrEP nonusers (n = 2267), PrEP users were older, had more years of formal education, were more likely to live alone, and had greater access to healthcare (as indicated by having healthcare insurance and a PCP/clinic). PrEP users were also more likely to report prior CAI and more recent CAI, but were also more likely to perceive themselves as having no possibility of an undiagnosed HIV infection (all p < 0.05). Compared to all PrEP nonusers, PrEP users were more likely to have had CAI with exchange partners and had more main, casual, and exchange male sexual partners (all p < 0.05).
FIG. 1.
Participant enrollment. *Incomplete responses include don't know and refuse to answer responses on the PrEP question. PrEP, pre-exposure prophylaxis.
Table 1.
Participant Characteristics By Pre-Exposure Prophylaxis Use Among All Study Participants (n = 2387)
| PrEP users (n = 80) | PrEP nonusers (n = 2267) | ||
|---|---|---|---|
| n (%)a/median (IQR) | n (%)/median (IQR) | p | |
| Demographics/social background | |||
| Race/ethnicity | |||
| Black | 12 (15) | 440 (19) | 0.55 |
| Hispanic | 29 (36) | 830 (37) | |
| White | 39 (49) | 997 (44) | |
| Age | 23 (21–24) | 22 (20–23) | <0.01 |
| Education | |||
| Less than high school | 1 (1) | 128 (6) | <0.05 |
| High school/GED | 8 (10) | 304 (13) | |
| Less than bachelor degree | 44 (55) | 1383 (61) | |
| Bachelor degree or higher | 27 (34) | 447 (20) | |
| Refused/did not know | 0 | 5 (0.2) | |
| Community type | |||
| Large city or surrounding suburb | 45 (56) | 900 (38) | 0.06 |
| Medium city or surrounding suburb | 19 (24) | 738 (31) | |
| Small city | 7 (9) | 302 (13) | |
| Town | 6 (8) | 233 (10) | |
| Rural area | 3 (4) | 83 (4) | |
| Refused/did not know | 0 | 11 (0.5) | |
| US region | |||
| Midwest | 15 (19) | 510 (23) | 0.69 |
| South | 39 (49) | 954 (42) | |
| West | 14 (18) | 431 (19) | |
| Northeast | 12 (15) | 372 (16) | |
| Live alone | |||
| Yes | 30 (38) | 563 (25) | <0.05 |
| No | 50 (62) | 1697 (75) | |
| Refused/did not know | 0 | 7 (0.3) | |
| Healthcare access | |||
| Have a PCP/clinic for care | |||
| Yes | 74 (93) | 1563 (69) | <0.0001 |
| No | 6 (8) | 657 (29) | |
| Refused/did not know | 0 | 47 (2) | |
| Healthcare Insurance | |||
| Yes | 70 (88) | 1697 (75) | <0.05 |
| No | 10 (13) | 530 (23) | |
| Refused/did not know | 0 | 40 (2) | |
| Sexual behavior/perceived risk | |||
| CAI with a man | |||
| Ever | 76 (95) | 1956 (86) | 0.03 |
| Never | 4 (5) | 308 (14) | |
| Refused/did not know | 0 | 3 (0.3) | |
| Last CAI with a man | |||
| Never | 4 (5) | 308 (14) | <0.0001 |
| Less than a month ago | 50 (63) | 836 (37) | |
| Between 1 and 6 months ago | 19 (24) | 600 (26) | |
| More than 6 months ago | 7 (9) | 516 (23) | |
| Refused/did not know | 0 | 7 (0.3) | |
| Perceived risk of HIV infection | |||
| Possible | 55 (69) | 1696 (75) | <0.001 |
| Not possible at all | 24 (30) | 495 (22) | |
| Refused/did not know | 1 (1) | 76 (3) | |
| Casual CAI with a man | |||
| No CAI with a man | 4 (5) | 308 (14) | 0.08 |
| No casual CAI with a man | 7 (9) | 278 (12) | |
| Casual CAI with a man | 56 (70) | 1513 (67) | |
| Refused/did not know | 13 (16) | 168 (7) | |
| Exchange CAI with a man | |||
| No CAI with a man | 4 (5) | 308 (14) | 0.02 |
| No exchange CAI with a man | 55 (69) | 1557 (69) | |
| Exchange CAI with a man | 18 (23) | 332 (15) | |
| Refused/did not know | 3 (4) | 70 (3) | |
| Total main partners | 2 (1–5.5) | 2 (0–4) | <0.01 |
| Total casual partners | 6 (0–15) | 2 (0–7) | <0.01 |
| Total exchange partners | 0 (0) | 0 (0) | 0.03 |
Percentages may not add up to 100% due to rounding.
CAI, condomless anal intercourse; GED, general equivalency diploma; PCP, primary care provider; PrEP, pre-exposure prophylaxis.
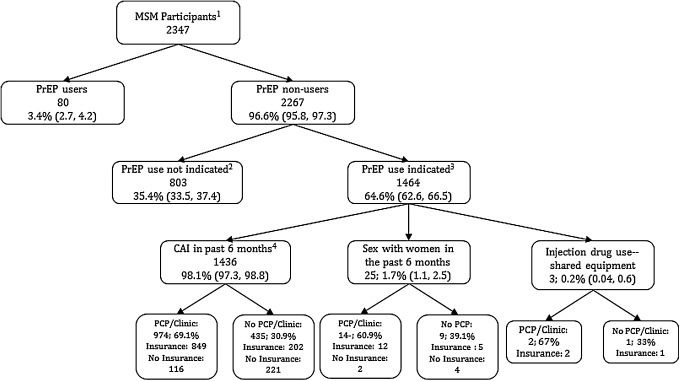
Relationship between PrEP use, PrEP eligibility, and access to healthcare
For those participants who had never used PrEP, Fig. 2 summarizes PrEP eligibility based on the 2014 CDC guidelines and healthcare provider and insurance barriers to its use. Of the 2267 PrEP nonusers, 1464 (64.6%) met at least one of the CDC criteria; among those who met at least one criteria, 94.4% met a single criterion, 5.4% met two criteria, and 0.1% met all three. The most common reason for not meeting PrEP eligibility criteria was lack of CAI in the past 6 months (Supplementary Table S1; Supplementary Data are available online at www.liebertpub.com/apc).
FIG. 2.
Identification of potential PrEP users and barriers to use. 1Characteristics of all men-who-have-sex-with-men participants are shown in Table 1. 2Supplementary Table S1 reports why participants did not meet criteria for PrEP prescription. 3Subpopulation used for analysis in Table 2; 49 of the 1464 participants did not respond to the healthcare access questions and were excluded from the analysis. Characteristics are in Supplementary Tables S2 and S3. 4One respondent also had condomless sex with women in previous 6 months and shared IDU equipment, 68 respondents had condomless sex with women, 15 respondents shared IDU equipment. CAI, condomless anal intercourse; IDU, injection drug use; MSM, men-who-have-sex-with-men; PCP, primary care provider; PrEP, pre-exposure prophylaxis.
In comparing PrEP-eligible and-ineligible nonusers, there were no differences between the groups in social and demographic factors. PrEP-eligible nonusers were somewhat less likely to have a PCP or access a clinic for care than ineligible nonusers (p < 0.05). PrEP-eligible nonusers were much more likely to report more recent CAI, more casual CAI, more exchange CAI, and a higher number of main, casual, and exchange male sexual partners; they were also more likely to perceive a possible risk of HIV infection than ineligible nonusers (all p < 0.05) (Supplementary Table S2).
Among the PrEP-eligible nonuser YMSM who answered all questions regarding healthcare (1415), 61.0% had both health insurance and a PCP or primary care clinic; 14.7% had insurance, but no PCP or clinic; 8.3% had a PCP or clinic, but lacked health insurance; and 16.0% lacked both a healthcare provider and insurance. Compared to PrEP users, the 1464 PrEP-eligible YMSM nonusers were younger, less likely to live alone, less likely to have a healthcare provider and healthcare insurance, but were more likely to perceive themselves as possibly having an undiagnosed HIV infection (Supplementary Table S2).
Demographic characteristics associated with decreased access to PrEP as a function of healthcare insurance and PCP/clinic status
Table 2 provides the results of the multivariable multinomial regression modeling used to identify demographic characteristics associated with lower access to PrEP due to lack of healthcare insurance or access to a PCP/clinic. As shown, older participants were more likely to face the barriers of having no health insurance and no PCP/clinic or having no health insurance, but having a PCP/clinic. Compared to white YMSM, both black and Hispanic YMSM were more likely to have no health insurance but have a PCP/clinic, and Hispanics were more likely to lack both health insurance and a PCP/clinic.
Table 2.
Factors Associated with Access to Healthcare Among PrEP-Eligible Nonusers (n = 1415) Using Multivariable Multinomial Modeling
| No PCP/clinic and no insurance (n = 226) | No PCP/clinic; have insurance (n = 208) | Have PCP/clinic; no insurance (n = 118) | |
|---|---|---|---|
| Adjusted OR (95% CI) | Adjusted OR (95% CI) | Adjusted OR (95% CI) | |
| Age | 1.19 (1.08–1.230) | 1.07 (0.98–1.18) | 1.18 (1.05–1.33) |
| Race | |||
| Black | 1.53 (0.96–2.42) | 1.10 (0.72–1.69) | 2.40 (1.38–4.17) |
| Hispanic | 3.47 (2.43–4.95) | 1.29 (0.91–1.82) | 2.81 (1.74–4.53) |
| White | Reference | Reference | Reference |
| Education | |||
| Less than high school | 2.69 (1.19–6.08) | 1.06 (0.45–2.49) | 6.20 (2.45–15.68) |
| High school/GED | 4.03 (2.35–6.91) | 1.37 (0.80–2.36) | 2.29 (1.01–5.18) |
| Less than bachelor degree | 1.34 (0.86–2.08) | 0.75 (0.51–1.11) | 1.91 (1.04–3.49) |
| Bachelor degree or higher | Reference | Reference | Reference |
| US Region | |||
| Midwest | 1.56 (0.91–2.68) | 1.49 (0.89–2.50) | 2.10 (0.93–4.74) |
| South | 2.08 (1.29–3.35) | 1.52 (0.94–2.44) | 3.16 (1.51–6.58) |
| West | 1.34 (0.76–2.37) | 2.13 (1.26–3.60) | 3.30 (1.49–7.31) |
| Northeast | Reference | Reference | Reference |
Among 1464 PrEP eligible nonusers, 49 did not respond to access to healthcare questions and were excluded from analyses.
Reference group is full access to healthcare: have both PCP/clinic and health insurance (n = 863)
CI, confidence interval; GED, general equivalency diploma; OR, odds ratio; PCP, primary care provider; PrEP, pre-exposure prophylaxis.
Fewer years of formal education were associated with lack of health insurance and no PCP/clinic or having a PCP/clinic, but still lacking insurance. Participants in the southern United States were less likely to have health insurance compared to those in the northeast, and participants from the west were more likely to lack access to clinical providers.
Discussion
In this investigation, we examined PrEP usage, factors associated with its use, and potential limitations to PrEP access among social media using black, Hispanic, and white YMSM living in the United States. Consistent with other recent reports, PrEP utilization was low with an overall rate of 3.4%. Three other surveys of YMSM conducted between 2013 and 2015 reported rates of usage between 8.2% and 12.2%.17–19 These three studies were focused on specific geographic areas (California or major urban areas, including Chicago, Houston, Atlanta, and New York City), included participants up to the age of 29 years old, and had varying eligibility criteria such as CAI within the past 6 months. These methodological differences might account for the slightly lower rate of reported usage in this study.
As expected, PrEP use in this investigation was associated with higher levels of condomless sex, access to health insurance, and access to a primary healthcare provider. These results are consistent with previous reports of PrEP use among YMSM as being associated with age,17 having health insurance,17 and engaging in higher levels and more recent/potentially riskier sexual activity, such as group sex or sex with HIV-infected partners.17–19 PrEP users in this current study perceived themselves as less likely to have an undiagnosed HIV infection, perhaps due to the protection against HIV that PrEP provides or the requirement for repeat HIV testing at least every 3 months, although the reasons for this belief and adherence to PrEP were not addressed in this investigation.
We found a high unmet need for PrEP among this population of racially and ethnically diverse YMSM: 65% of PrEP nonusers met at least one criterion for PrEP use, primarily CAI in the preceding 6 months. Facilitating their access to PrEP, 61% of these PrEP eligible YMSM had health insurance and a PCP/clinic for their medical care. Such YMSM constitute an apparently sizeable population already engaged in the healthcare system who might be eligible for co-pay assistance to overcome financial barriers to PrEP.34 Despite these advantages, YMSM with health insurance and providers face other barriers which might explain why they have not used PrEP, including the need for adherence to a daily medication regimen,14,17,22 continued medical visits while on PrEP,14 concerns about side effects,17,21,23,35 and PrEP related stigma from parents (especially for young adults who are still covered under their parents' insurance policies)34 and within the gay community.36
In contrast, substantial proportions of these PrEP-eligible black, Hispanic, and white YMSM reported structural barriers as follows: no healthcare insurance (15%), no PCP/clinic (8%), or both (16%). In addition, specific subgroups of YMSM may have a harder time accessing PrEP. Mirroring national trends,37 blacks and Hispanics were more likely than whites to lack health insurance and/or a PCP/clinic. Because HIV infection incidence remains highest among black and Hispanic MSM, the lack of healthcare access, and consequently PrEP access, is highly problematic. Research in Houston and Chicago among YMSM has found differences in utilization by ethnicity, with the lowest rates among blacks, suggesting that the groups most in need of PrEP may not be receiving it.19 In addition, PrEP-eligible participants in the South and West were also limited by lack of health insurance and/or PCP/clinic. These regional disparities might reflect the more limited expansion of Medicaid in the south than in the rest of the country. This finding is particularly troubling, given that the highest rates of new HIV infection are in the South, and southern blacks have a higher prevalence of HIV there than other ethnic groups.38 Also of concern is lower access to health insurance and PCPs/clinics for those with comparatively fewer years of formal education. Lower education frequently coincides with lower health literacy and reduced knowledge of preventive services such as PrEP.
There are several limitations to our study. PrEP usage is a moving target, with the number of users likely increasing since this study was conducted, so the data may be outdated. Within this study, we also do not know if participants who have indicated that they have used PrEP in the past are continuing to use PrEP, nor do we know about their adherence. We do not know if the percentage of PrEP-eligible YMSM changed over time, since patterns of sexual activity also might change over time. Although this sample of black, Hispanic, and white YMSM came from a national survey with participants from all fifty states and the District of Columbia, we cannot claim representativeness of the underlying population of these YMSM, even among social media users. We also may not have identified all potential PrEP-eligible participants since this study was designed before the issuance of CDC guidelines and there were no questions asking if participants were in monogamous sero-discordant relationships or had a sexually transmitted infection in the prior 6 months, both of which are additional indicators for PrEP use. Further, in examining access to healthcare, while a PCP/clinic is necessary for PrEP prescription and health insurance is extremely useful, there are other factors that influence access such as clinic and clinician availability, physical location of facilities and distance and transportation available to them, and health insurance limitations. Finally, all data were self reported, so veracity cannot be assured, although responses were anonymous.
In conclusion, high rates of new HIV infections among black, Hispanic, and white YMSM in the United States demonstrate the need for continued efforts to halt the spread of HIV among this population. PrEP offers an effective and safe means of intervention, but utilization remains lower than is required to curb the HIV epidemic. This investigation highlights the scope of the potential population of the YMSM who are PrEP eligible and documents significant underutilization, partially due to barriers created by a lack of healthcare providers or health providers. These findings should help guide the design and implementation of PrEP scale-up efforts, particularly in focusing efforts to reduce healthcare access barriers to PrEP use among this higher HIV risk population.
Supplementary Material
Acknowledgments
This research was supported by a grant from the National Institute of Nursing Research (R21 NR023869, ClinicalTrials.gov Identifier: NCT02369627).
The authors gratefully recognize the assistance of Mr. Ian Donaghy and Mr. Justin Romanoff in the execution of this study.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Hall HI, Song R, Tang T, et al. HIV trends in the United States: Diagnoses and estimated incidence. JMIR Public Health Surveill 2017;3:e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gay and Bisexual Men | HIV by Group | HIV/AIDS | CDC. Available at: https://www.cdc.gov/hiv/group/msm/index.html (Last accessed April29, 2017)
- 3.Men Living with Diagnosed HIV Who Have Sex with Men: Progress Along the Continuum of HIV Care—United States, 2010. Available at: https://www.cdc.gov/mmwr/preview/mmwrhtml/mm6338a2.htm (Last accessed April29, 2017) [PMC free article] [PubMed]
- 4.Fonner VA, Dalglish SL, Kennedy CE, et al. Effectiveness and safety of oral HIV preexposure prophylaxis for all populations. AIDS Lond Engl 2016;30:1973–1983 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Grant RM, Lama JR, Anderson PL, et al. Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. N Engl J Med 2010;363:2587–2599 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Baeten JM, Haberer JE, Liu AY, Sista N. Pre-exposure prophylaxis for HIV prevention: Where have we been and where are we going? J Acquir Immune Defic Syndr 1999 2013;63:S122–S129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cáceres CF, Koechlin F, Goicochea P, et al. The promises and challenges of pre-exposure prophylaxis as part of the emerging paradigm of combination HIV prevention. J Int AIDS Soc 2015;18(4 Suppl 3):19949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Grant RM, Anderson PL, McMahan V, et al. Uptake of pre-exposure prophylaxis, sexual practices, and HIV incidence in men and transgender women who have sex with men: A cohort study. Lancet Infect Dis 2014;14:820–829 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.FDA Approves First Drug for Reducing the Risk Of Sexually Acquired HIV Infection | News. Available at: https://aidsinfo.nih.gov (Last accessed April29, 2017)
- 10.US Public Health Service/Centers for Disease Control and Prevention. Preexposure Prophylaxis for the Prevention of HIV Infection in the United States—2014 Clinical Practice Guideline. May 2014. Available at: https://www.cdc.gov/hiv/pdf/PrEPguidelines2014.pdf (Last accessed December30, 2016)
- 11.Cohen SE, Vittinghoff E, Bacon O, et al. High interest in pre-exposure prophylaxis among men who have sex with men at risk for HIV-infection: Baseline data from the US PrEP Demonstration Project. J Acquir Immune Defic Syndr 1999 2015;68:439–448 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Eaton LA, Driffin DD, Smith H, Conway-Washington C, White D, Cherry C. Psycho-social factors related to willingness to use pre-exposure prophylaxis for HIV prevention among black men who have sex with men attending a community event. Sex Health 2014;11:244–251 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Young I, McDaid L. How acceptable are antiretrovirals for the prevention of sexually transmitted HIV?: A review of research on the acceptability of oral pre-exposure prophylaxis and treatment as prevention. AIDS Behav 2014;18:195–216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hosek SG, Rudy B, Landovitz R, et al. An HIV preexposure prophylaxis demonstration project and safety study for young MSM. J Acquir Immune Defic Syndr 2017;74:21–29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Burns DN, Grossman C, Turpin J, Elharrar V, Veronese F. Role of oral pre-exposure prophylaxis (PrEP) in current and future HIV prevention strategies. Curr HIV/AIDS Rep 2014;11:393–403 [DOI] [PubMed] [Google Scholar]
- 16.Dolezal C, Frasca T, Giguere R, et al. Awareness of post-exposure prophylaxis (PEP) and pre-exposure prophylaxis (PrEP) is low but interest is high among men engaging in condomless anal sex with men in Boston, Pittsburgh, and San Juan. AIDS Educ Prev 2015;27:289–297 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Holloway IW, Dougherty R, Gildner J, et al. Brief report: PrEP uptake, adherence, and discontinuation among california YMSM using geosocial networking applications. J Acquir Immune Defic Syndr 2017;74:15–20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Strauss BB, Greene GJ, Phillips G, et al. Exploring patterns of awareness and use of HIV pre-exposure prophylaxis among young men who have sex with men. AIDS Behav 2017;21:1288–1298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kuhns LM, Hotton AL, Schneider J, Garofalo R, Fujimoto K. Use of pre-exposure prophylaxis (PrEP) in young men who have sex with men is associated with race, sexual risk behavior and peer network size. AIDS Behav 2017;21:1376–1382 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mimiaga MJ, Closson EF, Battle S, et al. Reactions and receptivity to framing HIV prevention message concepts about pre-exposure prophylaxis for Black and Latino men who have sex with men in three urban US cities. AIDS Patient Care STDs 2016;30:484–489 [DOI] [PubMed] [Google Scholar]
- 21.Kubicek K, Arauz-Cuadra C, Kipke MD. Attitudes and perceptions of biomedical HIV prevention methods: Voices from young men who have sex with men. Arch Sex Behav 2015;44:487–497 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pérez-Figueroa RE, Kapadia F, Barton SC, Eddy JA, Halkitis PN. Acceptability of PrEP uptake among racially/ethnically diverse young men who have sex with men: The P18 study. AIDS Educ Prev 2015;27:112–125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bauermeister JA, Meanley S, Pingel E, Soler JH, Harper GW. PrEP awareness and perceived barriers among single young men who have sex with men in the United States. Curr HIV Res 2013;11:520–527 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mullins TLK, Zimet G, Lally M, Kahn JA. Adolescent human immunodeficiency virus care providers' attitudes toward the use of oral pre-exposure prophylaxis in youth. AIDS Patient Care STDs 2016;30:339–348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Karris MY, Beekmann SE, Mehta SR, Anderson CM, Polgreen PM. Are we prepped for preexposure prophylaxis (PrEP)? Provider opinions on the real-world use of PrEP in the United States and Canada. Clin Infect Dis 2014;58:704–712 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Doblecki-Lewis S, Jones D. Community federally qualified health centers as homes for HIV preexposure prophylaxis. J Int Assoc Provid AIDS Care 2016;15:522–528 [DOI] [PubMed] [Google Scholar]
- 27.Truvada for PrEP: Experts Weigh in on the Newest Way to Prevent HIV/AIDS. Healthline. February 7, 2014. Available at: www.healthline.com/health-news/hiv-truvada-for-hiv-prevention-experts-weight-in-020714 (Last accessed April29, 2017)
- 28.Horberg M, Raymond B. Financial policy issues for HIV pre-exposure prophylaxis: Cost and access to insurance. Am J Prev Med 2013;44(1 Suppl 2):S125–S128 [DOI] [PubMed] [Google Scholar]
- 29.King HL, Keller SB, Giancola MA, et al. Pre-exposure prophylaxis accessibility research and evaluation (PrEPARE study). AIDS Behav 2014;18:1722–1725 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lelutiu-Weinberger C, Pachankis JE, Gamarel KE, Surace A, Golub SA, Parsons JT. Feasibility, acceptability, and preliminary efficacy of a live-chat social media intervention to reduce HIV risk among young men who have sex with men. AIDS Behav 2015;19:1214–1227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Patel VV, Masyukova M, Sutton D, Horvath KJ. Social media use and HIV-related risk behaviors in young Black and Latino gay and bi men and transgender individuals in New York City: Implications for online interventions. J Urban Health 2016;93:388–399 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Landovitz RJ, Tseng C-H, Weissman M, et al. Epidemiology, sexual risk behavior, and HIV prevention practices of men who have sex with men using GRINDR in Los Angeles, California. J Urban Health 2013;90:729–739 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Merchant RC, Clark MA, Liu T, et al. Preferences for oral fluid rapid HIV self-testing among social media-using young black, Hispanic, and white men-who-have-sex-with-men (YMSM): Implications for future interventions. Public Health 2017;145:7–19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Arnold T, Brinkley-Rubinstein L, Chan PA, et al. Social, structural, behavioral and clinical factors influencing retention in pre-exposure prophylaxis (PrEP) care in Mississippi. PLoS One 2017;12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mustanski B, Johnson AK, Garofalo R, Ryan D, Birkett M. Perceived likelihood of using HIV pre-exposure prophylaxis medications among young men who have sex with men. AIDS Behav 2013;17:2173–2179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Calabrese SK, Underhill K. How stigma surrounding the use of HIV preexposure prophylaxis undermines prevention and pleasure: A call to destigmatize “Truvada Whores.” Am J Public Health 2015;105:1960–1964 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Foutz J, Cornachione E, Garfield R. Key Facts on Health and Health Care by Race and Ethnicity—Section 4: Health Coverage. Henry J Kais Fam Found. June 2016. Available at: http://kff.org/report-section/key-facts-on-health-and-health-care-by-race-and-ethnicity-section-4-health-coverage (Last accessed May22, 2017)
- 38.Prejean J, Tang T, Hall HI. HIV diagnoses and prevalence in the southern region of the United States, 2007–2010. J Community Health 2013;38:414–426 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.