Abstract
Antiretroviral (ARV) adherence has largely been considered from the perspective of an individual's behavior with less attention given to potential structural causes for lapses in treatment, such as the cost of medications and care. HIV medication expense is typically covered by third party payers. However, private insurance premiums and deductibles may rise, or policies terminated such as with a change in employment. Likewise, a patient's eligibility for publicly funded coverage like state AIDS Drug Assistance Programs (ADAP) or Medicaid can also be lost. We conducted a one-time survey of a sample of 300 patients receiving HIV care at a single large academic center in the south of United States to examine lapses in HIV therapy due to financial reasons. We found that during the prior year, financial issues including medication cost or coverage led to a lapse in ARVs in 10% (n = 31) of participants. However, of the 42% (n = 125) participants who had been enrolled in ADAP at any time during the prior year, 21% (n = 26) reported an ARV lapse due to problems with ADAP or medication cost. Respondents cited ADAP's required semi-annual renewal process and other administrative issues as the cause of ARV lapses. The median duration of missed ARVs was 2 weeks (range of <1–23 weeks). Non-HIV medication and transportation to and from clinic costs were also identified as financial burdens to care by respondents. In conclusion, although conducted at a single medical center and one state, this study suggests that a significant minority of HIV-infected patients encounter financial barriers to ARV access, and this is paradoxically more common among those enrolled in the state ADAP. Streamlining, supporting, and simplifying ADAP renewal procedures will likely reduce lapses in ARV adherence and persistence.
Keywords: : access to care, drug cost, antiretroviral, patient care
Introduction
Uninterrupted adherence to antiretroviral (ARV) treatment is essential to successful long-term management of HIV infection. Continuous ARV therapy suppresses viral replication, protects CD4+ lymphocytes count, prevents disease progression, reduces the potential for drug resistance, and greatly diminishes the risk of HIV transmission.1–6 While a considerable amount of research examining the medication-taking behaviors of people living with HIV infection has been conducted, little work has been done to explore the effect of structural factors, such as the processes for procuring and paying for ARVs, as a barrier to continuous access to HIV therapy.
The annual cost of ARV medications for the treatment of HIV can easily exceed $30,000 without medication insurance coverage or other assistance.1 Private insurance will typically pay for a large proportion of the cost of HIV therapy, but policies vary considerably in the extent of coverage and most policy holders remain responsible for deductibles or co-payments. Publically funded ARV coverage, particularly the largely state funded AIDS Drug Assistance Programs (ADAP), provide ARVs, as well as many other medications for comorbid conditions, at no cost to lower income patients who meet financial criteria established by each state. Approximately, a quarter of all persons in HIV care in the United States are enrolled in ADAP, including over 7400 people in North Carolina.7 In addition, pharmaceutical companies have programs that provide co-payment assistance for those with private insurance or directly provide medication at no cost to qualifying individuals.
In this study, we sought to better understand the extent that people living with HIV fall through this safety net of medication coverage and struggle to pay for their HIV medications. We surveyed a sample of adult patients receiving HIV care at a large academic outpatient clinic in North Carolina to determine the extent that financial barriers, including medication costs and changes in health insurance coverage, result in lapses in ARV therapy. In addition, we explored the most common specific financial barriers encountered by HIV-infected patients when accessing their HIV and non-HIV medications and healthcare.
Methods
Study setting and population
Participants were recruited from the University of North Carolina at Chapel Hill (UNC) Infectious Diseases (ID) Clinic. This clinic serves ∼1800 patients with HIV infection across North Carolina. As described previously, ∼30% of clinic patients have private health insurance, 50% public/governmental insurance, and 20% are uninsured.8 To qualify for ADAP in North Carolina, recipients must have a gross income at or below 300% of the Federal Poverty Level.9 The state ADAP requires beneficiaries to renew their ADAP application every 6 months to provide evidence of continued qualification for the program.
Outpatients attending clinic visits and determined to be eligible were randomly selected for screening and those who consented were enrolled. Inclusion criteria included confirmed diagnosis of HIV infection, age 18 years and greater, prescribed ARVs in the past 12 months, and fluency in English. Individuals were excluded if they presented to the UNC ID Clinic for their first appointment as a new patient. This study was approved by the UNC Institutional Review Board.
Study procedures
Research personnel interviewed and consented patients at their routinely scheduled ID Clinic visit. Patient interviews were purposefully conducted on each weekday and during morning and afternoon clinic hours so that patients from all providers would be well represented in our sample. The questionnaire was administered via Computer Assisted Personal Interviewing and included a mix of open- and closed-ended questions. Qualtrics Survey Software was used to directly record interview responses. The survey included questions regarding participant demographics and socioeconomic status that were adapted from the 2014 Centers for Disease Control and Prevention Behavioral Risk Factor Surveillance System Questionnaire.10 To determine lapses in ARV therapy due to financial barriers all participants were asked, “Was there ever a time in the past 12 months when you did not take any of your HIV medications, even for one day, because of cost?” In addition, survey items probed the estimated costs of ARVs and non-HIV medications, duration of longest lapse in ARV therapy due to financial reasons, financial barriers to accessing medicines and healthcare, health insurance status, ADAP enrollment status, and access to non-HIV primary care. A question regarding transportation as a barrier to receiving HIV care was added subsequent to the enrollment of the first 30 participants. The complete survey can be found in Supplemental Materials. Participants received $5 in cash at the conclusion of the interview.
Data analysis
Descriptive statistics were used to summarize collected data. All data were analyzed using Microsoft Excel and Qualtrics Survey Software.
Results
Participant recruitment and characteristics
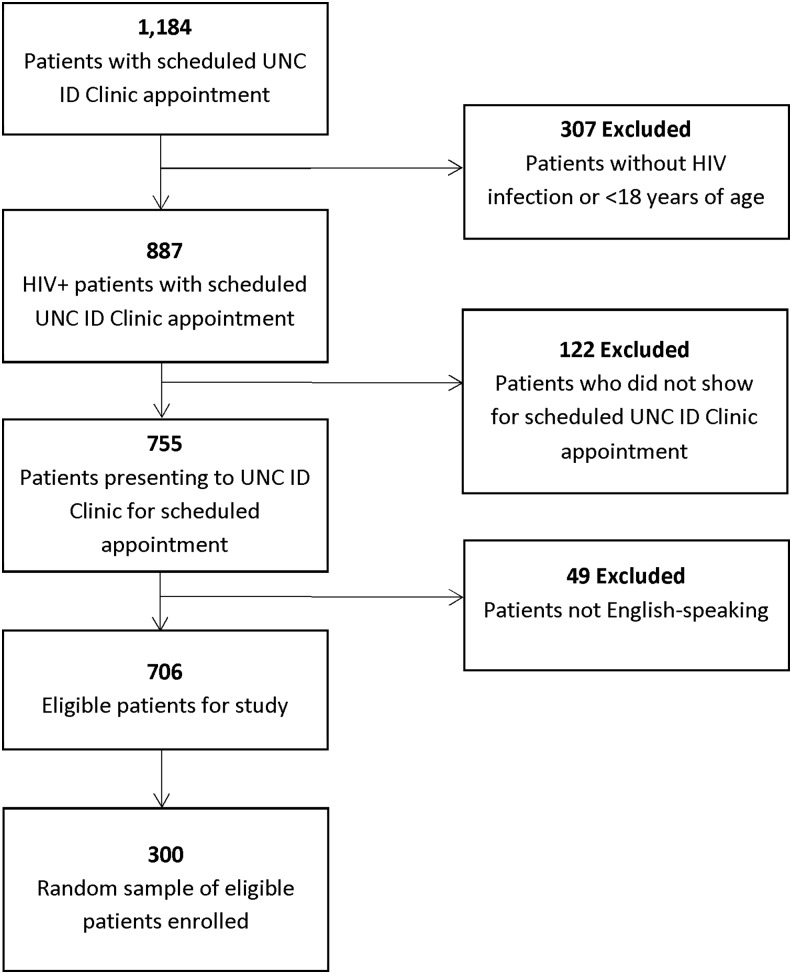
During the months of March to May 2015, all patients (n = 1184) with an appointment at the UNC ID Clinic were screened for inclusion. Of these, 706 patients were determined to meet the study eligibility criteria and presented for their appointment. A random sample of 300 of these patients distributed across each weekday and the morning and afternoon clinic sessions were enrolled (Fig. 1).
FIG. 1.
Study participant selection and recruitment. ID, Infectious Diseases; UNC, University of North Carolina at Chapel Hill.
Participants were mostly male and middle aged; approximately two-thirds self-identified as African American or black (Table 1). The median annual income stratum was $10,000–15,000 with an average household size of two and 25% of those interviewed were working full time, with most of the remainder receiving disability benefits or unemployed. During the prior year, 42% (n = 125) had been enrolled in ADAP and 35% (n = 106) reported they received the ARVs through ADAP. Other forms of ARV coverage reported included private insurance plans and Medicaid. Twenty percent reported not having any health insurance. During the prior year, 66% experienced no changes in their health insurance coverage, 5% lost their health insurance coverage, 5% gained health insurance coverage, and 4% changed health insurance plans. Approximately two-thirds received ARVs at no cost and for almost a quarter the average monthly out of pocket cost for ARVs was <$25. A co-pay card provided by an ARV pharmaceutical company was used by 17%.
Table 1.
Participant Characteristics
| Average age (years) | 47 years (range: 19–75), % |
|---|---|
| Gender | |
| Male | 68 |
| Female | 30 |
| Transgender | 1 |
| Bisexual | <1 |
| Intersex | <1 |
| Race/ethnicity | |
| African American/black | 68 |
| Non-Hispanic white | 27 |
| Hispanic/Latino | 3 |
| American Indian or Alaska Native | 3 |
| Asian | 1 |
| Native Hawaiian/Pacific Islander | <1 |
| Annual household income | |
| <$10,000 | 32 |
| $10,001–15,000 | 16 |
| $15,001–20,000 | 5 |
| $20,001–25,000 | 5 |
| $25,001–35,000 | 7 |
| $35,001–50,000 | 7 |
| $50,001–75,000 | 5 |
| $75,001–100,000 | 3 |
| >$100,001 | 3 |
| Unknown | 14 |
| Decline to answer | 2 |
| Health insurance: past year | |
| No health insurance | 20 |
| Lost health insurance | 5 |
| Gained health insurance | 5 |
| Changed health insurance plans | 4 |
| No changes in health insurance | 66 |
| Insurance/coverage for HIV medsa | |
| ADAP | 37 |
| Medicaid | 35 |
| Medicare | 26 |
| Both medicaid and medicare | 15 |
| Private insurance employer based | 20 |
| Private insurance self purchased | 6 |
| Hospital pharmacy assistance | 6 |
| Supplied through research study | 2 |
| Supplied by drug company | 1 |
| TRICARE/VA/military | <1 |
| Only self-pay/fully out of pocket | <1 |
| Other | 7 |
| Possess HIV med co-pay card | |
| Yes | 17 |
| No | 83 |
| Employment status | |
| Working full time | 25 |
| Disabled | 38 |
| Unemployed | 22 |
| Working part time | 9 |
| Retired | 6 |
| Student | 2 |
| Other | <1 |
More than one response could be selected.
ADAP, AIDS Drug Assistance Programs.
Financial barriers to continuous ARV therapy
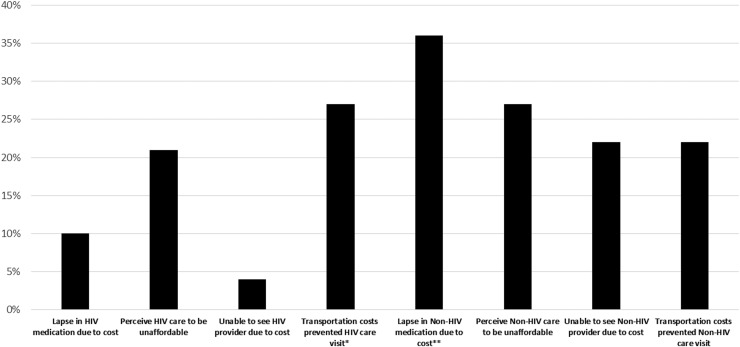
During the prior year, 10% (n = 31) of participants reported at least one lapse in ARV medication of a day or longer due to financial reasons, including the cost of medications or problems with medication coverage (e.g., ADAP). Overall, 11% of the participants indicated that their ARVs are “not at all” affordable (Fig. 2).
FIG. 2.
Reported financial barriers to HIV and Non-HIV care. *Of 270 asked about transportation barriers. **Of 185 participants reporting being prescribed non-HIV medications.
Among the 125 participants enrolled in ADAP at any time during the prior year, 21% (n = 26) reported missing at least 1 day of their ARVs due to problems with ADAP or due to medication cost, with a median 2-week duration of missed ARVs (range of <1–23 weeks). For the 22 patients citing ADAP problems as the cause of their ARV lapse, 41% (n = 9) stated their ADAP coverage was not renewed because they missed the every 6-month ADAP renewal deadline. Reasons for missing the ADAP deadline included the following: not being aware of the requirement or forgetting to reapply for ADAP coverage every 6 months, difficulty providing the information needed to renew coverage, lack of transportation to the clinic to renew their application, administrative difficulties that led to lapses in ARV therapy such as the ADAP renewal process taking longer than anticipated, lost paperwork after submission, and delays in ADAP pharmacy mailing of ARVs. Two participants also reported they became employed and briefly earned too much to qualify for ADAP coverage.
In contrast, for the 175 not enrolled in ADAP, 3% (n = 5) reported a lapse due strictly to the cost of their ARV. For these patients, the median duration of the longest lapse in ARV treatment was 1 week, with a range of 1–4 weeks. These individuals cited the following reasons for being unable to afford their ARV medications: no health insurance to pay for HIV medicines, loss of the health insurance that was paying for ARVs, a research study providing ARVs ended, problems with pharmacy/prescription renewal, the co-pay for their ARV medication increased, and unable to afford the co-pay.
Financial barriers to HIV care
Among all participants, 4% (n = 12) reported they were unable to attend an HIV clinic visit at least once in the previous 12 months due to cost. Half (n = 147) of the participants reported no clinic co-pay and for those with a co-pay the median self-reported amount was $40 (range of $0–450). Participants also cited transportation costs as a barrier to receiving HIV care, 27% (n = 73) of the 270 participants asked about transportation reporting the cost of transportation prevented them from accessing their HIV care and/or medications at least once in the previous 12 months.
Overall, 21% of participants perceived their HIV-related medication and healthcare out of pocket costs to be “not at all” or “not very” affordable, while 29% indicated these were “somewhat” affordable, and 45% responded these were “very” affordable.
Financial barriers to non-HIV medications and care
Of the 62% (n = 185) of participants who reported currently taking medicines other than ARVs at the time of the interview, 36% (n = 67) reported missing >1 day of their non-HIV medications at least once in the past year exclusively due to the cost of the medications (Fig. 2). The median duration of the longest lapse in non-HIV treatment was 3–4 weeks, with a range of <1 week to >12 months.
The median monthly cost for non-HIV medications among the cohort was $1–25, but ranged from $0 to $1000. Nearly half (46%) of the participants taking non-HIV medications obtained these at no cost and an additional 30% paid <$25 out of pocket each month for these medications.
Among those who reported being ADAP recipients who were prescribed non-HIV medications (n = 111), 32% (n = 35) had a lapse in these medications due to cost. For those not enrolled in ADAP and prescribed non-HIV medications (n = 74), 43% (n = 32) had a lapse in these medications due to cost.
An inability to see a healthcare provider at least once in the previous 12 months for their non-HIV healthcare due to cost was reported by 22% (n = 66); and 180 (60%) of participants did not have a primary care provider for non-HIV-related healthcare. Participants also cited transportation costs as a barrier to receiving non-HIV care, with 22% (n = 59) of the 270 asked about transportation reporting the cost of transportation prevented them from accessing their non-HIV care and/or medications at least once in the previous 12 months.
Overall, 27% of participants perceived their non-HIV-related medication and healthcare out of pocket costs to be “not at all” or “not very” affordable, while 32% indicated these were “somewhat” affordable, and 31% responded these were “very” affordable. Over half (54%) of the participants reported having outstanding healthcare bills for their combined HIV- and non-HIV-related medicines and healthcare, including bills for medical, dental, and/or physical therapy costs.
Discussion
HIV medication adherence has been examined largely in terms of individual medication-taking behaviors, with less attention paid to structural reasons for treatment lapses, such as financial barriers to ARVs and HIV care.11–14 We found that cost and access to treatment and care of HIV are barriers to ARV persistence for many patients, despite ADAP, medication insurance, and pharmaceutical company support programs. One in 10 people living with HIV surveyed experienced at least a single lapse in HIV therapy during the preceding year due to cost and one in five stated that they could not afford their HIV care. The lapses in ARV therapy reported by both those with and without ADAP support were not trivial. Treatment interruptions for the periods reported are sufficient for viral rebound. Resurgent viremia can have a number of consequences including an increase in transmission potential, and a small but real risk of drug resistance and CD4+ cell depletion.
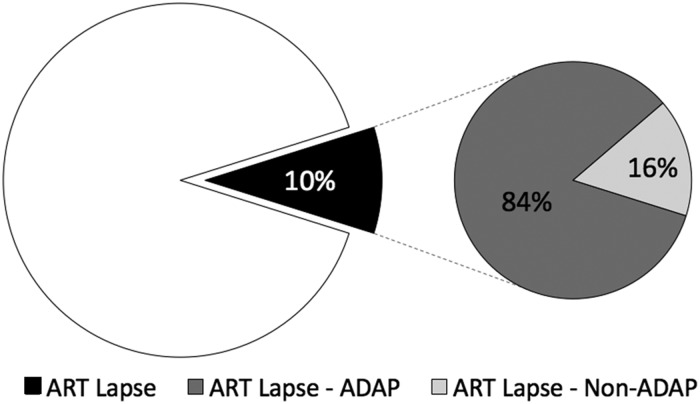
The risk of a break in taking HIV medications was paradoxically found to be substantially higher among those enrolled in the state ADAP, which provides ARVs at no cost to those who qualify based on income, compared to those not enrolled in this program. Of the 10% of the cohort who reported a lapse in ARV therapy, 84% were ADAP recipients (Fig. 3). We expected those enrolled in ADAP to have stable access to HIV medications compared to the uninsured and those with private insurance coverage, who are typically subjected to co-pays, deductibles, and changes in policy benefits; however, >20% of ADAP recipients experienced at least one lapse in ARV supply during the prior year; half had a break in treatment for two or more weeks.
FIG. 3.
Lapses in ART among overall cohort (n = 300) and proportion of those experiencing ART lapse who ADAP receipients. ADAP, AIDS Drug Assistance Programs; ART, antiretroviral therapy.
Data from the National Alliance of State and Territorial AIDS Directors (NASTAD) echo these findings.15 Of the 258,469 clients enrolled in ADAP nationwide in fiscal year 2013, 18% had not recertified twice during the prior 12-month period. Other studies have also probed for barriers to HIV care and therapy in the United States and several find that HIV-infected individuals may delay or discontinue antiretroviral therapy (ART) despite the support provided by safety-net programs.16 In Washington state, where access to ART is near universal, Dombrowski et al. found that 50% of patients enrolled in a public health HIV linkage program in Seattle reported absence of insurance as a barrier to care—and of those discontinuing ART, 31% stated that they could not afford HIV medications and 28% said they could not get access to ART for reasons other than cost.16 Ludema et al. examining viral suppression and insurance status and type among 1481 HIV-infected participants in the Women's Interagency HIV Study from 2006 to 2009 observed viral suppression to be least likely among women without insurance and also those receiving Medicaid alone.17 In that study, ADAP alone or in addition to public insurance increased the likelihood of viral suppression—highlighting the overall benefits of ADAP. Non-ADAP Ryan White HIV/AIDS Program services have also been found to be associated with positive clinical outcomes, including viral suppression, particularly among patients living in poverty, who are often individuals demonstrated to be at greater risk for under-treatment of HIV infection including younger patients, women, and African Americans.18–20
Therefore, while ADAP has been highly successful in providing crucial access to HIV therapy and services for thousands of people living with HIV infection, and has been credited with raising life expectancy and reducing racial and ethnic differences in treatment outcomes,21 it and other programs that provide ART at no cost do not completely eliminate financial barriers to HIV therapy. In the case of ADAP, aspects of the program, such as the every 6-month recertification, may lead to interruptions in ARV therapy for a substantial proportion of patients. A qualitative study of ADAP recipients in Birmingham, Alabama similarly found that the complexities of ADAP recertification act as a barrier to ARV continuity—a finding that transcended race and gender.22 As people living with HIV infection have a relatively high prevalence of comorbid medical and mental health conditions, and may also have limited healthcare literacy, they may be particularly challenged in their ability to comply with the requirements for continued participation in programs that provide for ART and HIV care.
In addition to identifying financial barriers to HIV-related healthcare, participants taking medicines for non-HIV conditions also reported financial barriers to healthcare and medicines for their non-HIV conditions. In comparison to the 21% of the study participants who stated that their HIV healthcare and medicines were not very affordable or not at all affordable, 27% of the participants felt that their non-HIV healthcare and medicines were either not very affordable or not at all affordable. Lapses in non-HIV medicines due to cost were reported by 14% of the respondents, double the proportion reporting a financially motivated break in ARV treatment. Further, a quarter reported not seeing their healthcare provider for non-HIV healthcare due to cost, suggesting that access to non-HIV healthcare remains difficult for those with limited financial means. Transportation to medical visits was also found to be a problem for many patients living with HIV infection and was a barrier to accessing both HIV and non-HIV-related care during the prior 12 months.
Overall, our results reveal a subset of HIV-infected patients who are unable to easily obtain necessary therapy and healthcare due to cost. It is notable that this study was conducted after the passage and enactment in 2010 of the Patient Protection and Affordable Care Act (ACA) which, in general, expanded health insurance and medication coverage. However, North Carolina, like the vast majority of states in the US South, opted to not expand Medicaid under the ACA. It has been estimated that Medicaid expansion in North Carolina would result in as much as an additional 400,000–500,000 people becoming insured.23 The income levels reported by the participants indicate many would be eligible for Medicaid, were North Carolina to expand this public health care program.
There are a number of important limitations to this study. Foremost, this research was conducted at a single academic center in one Southern state in the United States. The barriers to treatment and care can be expected to vary by clinic setting and locale. Selection bias could have been introduced as only patients who attended clinic visits were included and interviewed. In addition, non-English speaking patients, who make up <5% of the clinic population, were excluded and these individuals may have very different experiences paying for and accessing HIV medications and care than other patients attending the clinic. Additionally, our research was conducted at a single hospital-based outpatient clinic located within a large academic medical center. By selecting participants presenting to an ID Clinic at a major academic medical center, we likely underestimated the true prevalence of financial barriers that exist in other parts of North Carolina or among patients who miss visits or are not able present to a healthcare facility, possibly due to unsurmountable barriers to care. Further, respondents were asked about medication coverage during the prior 12 months. Those who enrolled in ADAP for <6 months before the interview would not have had an opportunity to go through the ADAP recertification process. Therefore, our estimate of the impact of ADAP recertification on ARV persistence may be conservative. Other limitations include a reliance on patient self-report. While the study survey included items that have been used in other surveys of HIV-infected patients, participants may not have always been willing and able to provide accurate answers to questions regarding financial matters.
In summary, despite the overall benefit of programs designed to provide HIV treatment that is affordable, some patients living with HIV infection still report financial barriers to continuous access to these medications. Many patients also report struggling to pay for HIV-related and non-HIV-related medical care. While ADAP has been successful in bringing people with HIV infection into care by providing them with HIV-related medicines and healthcare at no or little cost, our findings show that for some, the administrative requirements of the program may act as an obstacle to ARV access and adherence. These findings highlight the role that structural barriers can play in preventing individuals with HIV infection from maintaining optimal adherence to their ARV regimens and accessing necessary HIV-related healthcare. There is a need for corrective actions to address the structural issues within the healthcare system that act as obstacles to motivated individuals seeking HIV care. Simplification of renewal and supporting continuous participation in ADAP could be expected to reduce the risk of lapses in HIV treatment.
Acknowledgments
The authors appreciate the support received from the UNC Infectious Diseases Clinic staff, Margaret Forshag who assisted in participant recruitment, and Carol Golin, MD for her guidance during the planning of the project. This work was supported by the UNC Center for AIDS Research (CFAR), an NIH funded program (Swanstrom: P30 AI50410), and a mentoring award from the National Institutes of Drug Abuse (NIDA) at the NIH (Wohl: K24DA037101). Lastly, we thank the study participants for the generous donation of their time.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Panel on Antiretroviral Guidelines for Adults and Adolescents. Guidelines for the Use of Antiretroviral Agents in HIV-1-Infected Adults and Adolescents. Department of Health and Human Services. Available at: www.aidsinfo.nih.gov/ContentFiles/AdultandAdolescentGL.pdf (Last accessed June9, 2017)
- 2.Cohen MS, Chen YQ, McCauley M, et al. . Prevention of HIV-1 infection with early antiretroviral therapy. N Engl J Med 2011;365:493–505 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Moore RD, Keruly JC. CD4+ cell count 6 years after commencement of highly active antiretroviral therapy in persons with sustained virologic suppression. Clin Infect Dis 2007;44:441–446 [DOI] [PubMed] [Google Scholar]
- 4.Samji H, Cescon A, Hogg RS, et al. . Closing the gap: Increases in life expectancy among treated HIV-positive individuals in the United States and Canada. PLoS One 2013;8:e81355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.INSIGHT START Study Group, Lundgren JD, Babiker AG, et al. . Initiation of antiretroviral therapy in early asymptomatic HIV infection. N Engl J Med 2015;373:795–807 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.TEMPRANO ANRS Study Group, Danel C, Moh R, et al. . A trial of early antiretrovirals and isoniazid preventive therapy in Africa. N Engl J Med 2015;373:808–822 [DOI] [PubMed] [Google Scholar]
- 7.Bassett IV, Farel C, Szmuilowicz ED, Walensky RP. AIDS Drug Assistance Programs in the era of routine HIV testing. Clin Infect Dis 2008;47:695–701 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Napravnik S, Eron JJ, Jr, McKaig RG, et al. . E. Factors associated with fewer visits for HIV primary care at a tertiary care center in the Southeastern U.S. AIDS Care 2006;18:S45–S50 [DOI] [PubMed] [Google Scholar]
- 9.North Carolina Health and Human Services. Programs and Services. Available at: http://epi.publichealth.nc.gov/cd/hiv/adap.html (Last accessed June9, 2017)
- 10.Centers for Disease Control and Prevention. Behavioral Risk Factor Surveillance System. Available at: www.cdc.gov/brfss (Last accessed June9, 2017)
- 11.Thompson MA, Mugavero MJ, Amico KR, et al. . Guidelines for improving entry into and retention in care and antiretroviral adherence for persons with HIV: Evidence-based recommendations from an International Association of Physicians in AIDS Care panel. Ann Intern Med 2012;156:817–833 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rudy BJ, Murphy DA, Harris DR, et al. . Adolescent Trials Network for HIVAI. Patient-related risks for nonadherence to antiretroviral therapy among HIV-infected youth in the United States: A study of prevalence and interactions. AIDS Patient Care STDS 2009;23:185–194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Parienti JJ, Bangsberg DR, Verdon R, Gardner EM. Better adherence with once-daily antiretroviral regimens: A meta- analysis. Clin Infect Dis 2009;48:484–488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Simoni JM, Kurth AE, Pearson CR, et al. . Self-report measures of antiretroviral therapy adherence: A review with recommendations for HIV research and clinical management. AIDS Behav 2006;10:227–245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.National ADAP Monitoring Project: 2015 Annual Report. Available at: https://www.nastad.org/resource/national-adap-monitoring-project-2015-annual-report (Last accessed June9, 2017)
- 16.Dombrowski JC, Simoni JM, Katz DA, Golden MR. Barriers to HIV care and treatment among participants in a public health HIV care relinkage program. AIDS Patient Care STDS 2015;29:279–287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ludema C, Cole SR, Eron JJ Jr, et al. . Impact of health insurance, ADAP, and income on HIV viral suppression among US women in the women's interagency HIV study, 2006–2009. J Acquir Immune Defic Syndr 2016;73:307–312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Doshi RK, Milberg J, Isenberg D, et al. . High rates of retention and viral suppression in the US HIV safety net system: HIV care continuum in the Ryan White HIV/AIDS Program, 2011. Clin Infect Dis 2015;60:117–125 [DOI] [PubMed] [Google Scholar]
- 19.Weiser J, Beer L, Frazier EL, et al. . Service delivery and patient outcomes in Ryan White HIV/AIDS Program-Funded and -Nonfunded Health Care Facilities in the United States. JAMA Intern Med 2015;175:1650–1659 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Diepstra KL, Rhodes AG, Bono RS, et al. . Comprehensive Ryan White assistance and HIV clinical outcomes: Retention in care and viral suppression in a medicaid non-expansion state. Clin Infect Dis 2017. [Epub ahead of print]; DOI: 10.1093/cid/cix380 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Moore RD, Keruly JC, Bartlett JG. Improvement in the health of HIV-infected persons in care: Reducing disparities. Clin Infect Dis 2012;55:1242–1251 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Olson KM, Godwin NC, Wilkins SA, et al. . A qualitative study of underutilization of the AIDS Drug Assistance Program. J Assoc Nurses AIDS Care 2014;25:392–404 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.North Carolina Institute of Medicine. Examining the Impact of the Patient Protection and Affordable Care Act in North Carolina Medicaid Expansion Option Issue Brief. Available at: www.nciom.org/wp-content/uploads/2013/01/Medicaid-summary-FINAL.pdf (Last accessed June9, 2017)