Abstract
Purpose
We conducted a prospective multicentre study in 13 Welsh intensive care units to assess what proportion of intensive care admissions relate to alcohol, and how outcomes among these patients compare with non-alcohol related admissions.
Materials and methods
Data were prospectively collected for one month between June and July 2015. Every intensive care admission was screened for alcohol associations based on ICD-10 criteria, using a pre-designed pro-forma. Follow-up data were collected at 60 days using a pre-existing database (WardWatcher; Critical Care Audit Ltd, England). Outcomes included: lengths of mechanical ventilation, intensive care units and hospital stay; intensive care units and hospital mortality.
Results
Alcohol contributed directly to 10% of all ICU admissions and to 11% of unplanned admissions. These patients were younger (52 vs. 66, p = 0.0011), more likely to be male (68% vs. 52%, p = 0.014) and had more prolonged ventilation (p = 0.019) There was no significant difference between the groups with respect to length of stay or mortality.
Conclusions
Alcohol contributes to a significant proportion of ICU admissions in Wales, a Western European country with a relatively low number of ICU beds per capita. Strategies to address this impact should be explored.
Keywords: Alcohol, alcohol-related admissions, intensive care
Introduction
Alcohol misuse is the third leading risk factor for poor health globally and kills 2.5 million people per year worldwide.1 In Wales, 1 in 20 of all deaths are attributable to alcohol and there are around 12,700 hospital admissions due to alcohol per year.2 A study of admissions to ICU in England and Wales demonstrated a threefold increase in patients with alcohol-related liver disease over the decade up to 2005.3 More recently, a study from Scotland showed that a quarter of their critical care admissions were due to alcohol misuse, representing a huge burden on resources.4
The aim of this study was to investigate the impact of alcohol on intensive care admissions in Wales, a smaller country than Scotland with a population of approximately 3,000,000,5 but with similar distribution of rural and deprived areas, shown to be related to harmful drinking behaviour.1,2 The same methods were used to allow direct comparison of findings with those of Geary et al.4
Methods and materials
This study was conducted as a service evaluation within each participating Welsh Health Board. The Wales Research Ethics Committee waived the requirement for formal ethical approval. However, participation was approved by the Clinical Audit department at each participating centre.
Local co-ordinators and data collectors were recruited from every general ICU in Wales (14 units in 6 health boards). Data were prospectively collected for a one-month period from 08.00 on 22 June 2015 to 08.00 on 21 July 2015. Every intensive care admission was screened by a member of the team for alcohol associations based on ICD-10 criteria, using a pre-designed standard pro-forma4 (see Appendix 1). The only exclusion criterion was age <16.
Prospective data collection did not occur in one unit due to unforeseen circumstances. We discounted retrospective data collection at this site since this would lead to a non-uniform methodology and could compromise data quality. Thus, results are from 13 intensive care units across five health boards.
Follow-up data were collected after 60 days using the pre-existing WardWatcher database, which is standard across Welsh ICUs. These outcomes included: number of days of mechanical ventilation; ICU and hospital length of stay; ICU outcome and hospital mortality. Data were collated into an Excel spreadsheet and analysed using the SPSS statistical package (version 22). Fisher’s Exact Chi-square test and Mann–Whitney U test were used for analysis (due to a non-parametric distribution of data).
Results
Table 1 highlights the patients’ characteristics, severity of illness and outcomes for alcohol-related and non-alcohol-related admissions to ICU.
Table 1.
Patients’ characteristics, severity of illness and outcomes.
| All patients n = 615 | Non-alcohol admissions n = 555 | Alcohol-related admissions n = 60 | P | |
|---|---|---|---|---|
| Age | 66 (51–76) | 67 (54–76) | 52 (37–63) | 0.001 |
| Male | 327 (53%) | 286 (52%) | 41 (68%) | 0.014 |
| APACHE II | 14 (10–19) | 14 (10–19) | 13 (8–18) | 0.350 |
| Unplanned admission | 507 (82%) | 452 (81%) | 55 (92%) | 0.627 |
| ICU death | 108 (18%) | 96 (17%) | 12 (20%) | 0.594 |
| All death | 150(24%) | 136 (25% | 14 (23%) | 0.492 |
| ICU length of stay | 3 (2–6) | 3 (2–6) | 4 (2–9) | 0.087 |
| (Post-ICU) Hospital length of stay | 5 (1–14) | 6 (1–14) | 4 (0–11) | 0.515 |
| Ventilator days | 0 (0–2) | 0 (0–2) | 1 (0–5) | 0.019 |
Note: Values are presented as median (interquartile range) or number (percentage).
A total of 615 patients were screened, of whom 82% were unplanned admissions. This represented an average of 20 admissions per day across 13 sites. Median length of stay was 3 days.
A total of 60 patients (9.8%) were admitted as a direct result of alcohol, for example acute intoxication; alcoholic hepatitis, alcohol-induced pancreatitis; decompensated alcoholic liver disease or bleeding varices secondary to alcoholic liver disease. These cases were significantly more likely than the non-alcohol-related admissions to be male and were younger; 81% of alcohol-related admissions were unplanned. There was no statistical difference in APACHE II score between groups; however, alcohol-related admissions had a longer median length of mechanical ventilation.
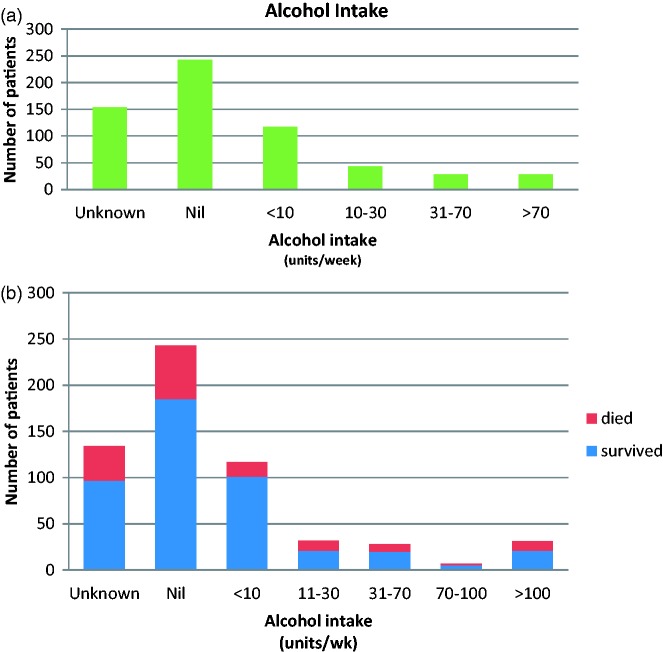
Background information on alcohol intake was sought in all cases (Figure 1); 33 patients whose primary reason for admission was not alcohol-related had evidence of alcohol-related comorbidity such as cirrhosis. If these patients were included in the alcohol cohort, there was a significant increase in ICU mortality compared to the rest of the admissions (25% vs. 14%, p = 0.02).
Figure 1.
(a) Reported alcohol intake. (b) Reported alcohol intake and outcome.
Discussion
Our study provides significant insight into the impact of alcohol on ICU services in Wales: 10% of admissions were related to alcohol, one-fifth of these patients dying in ICU and almost a quarter dying during their hospital admission.
However, taking an alcohol history appears to be problematic even during the course of a study intended to evaluate the impact of alcohol. In our study, in almost a quarter of cases, the alcohol intake was not recorded. Perhaps alcohol intake is not a routine element of history taking, or possibly it is not seen as a priority when assessing and managing a critically ill patient, or there may be doubt that inquiry will yield reliable information. It is difficult to ascertain a clear history in critically ill or unconscious patients and it may feel awkward to ask such questions of anxious relatives.
Where recorded, the most common reply for alcohol intake was nil (40%). Of course, this may not be entirely accurate. According to the Office for National Statistics,6 21% of adults report not drinking at all, and these are mainly young adults aged 16–24, which made up a minority of our ICU study population. Only 16% of our admissions reported drinking more than current national guidelines of 14 units per week. This contrasts with Welsh national data7 indicating that 40% of adults drank more than the guidelines. Additionally, when alcohol sales are compared with self-reported intake it appears that surveys may underestimate alcohol consumption by 40–45%.7,8 Possible reasons for underreporting alcohol intake may include: shame; fear of judgement; wish to ‘please’ medical staff; lack of knowledge of a relative’s alcohol intake or genuinely not realising how much one is drinking.
Despite this, we found that very high alcohol consumption was associated with worse outcome. In our study, patients who drank very excessively (more than 100 units per week) accounted for 3% of the total admissions and they had 50% mortality. Other authors have indicated that even more moderate levels of “at risk” alcohol consumption (for example,14 or more drinks per week for men aged 18 to 64 years, and 7 or more drinks for women and for men aged 65 and older) are associated with increased ICU and one-year mortality.9 Therefore, and although there are potential limitations to the accuracy of self-reported or surrogate reports of alcohol consumption, there appears to be value in estimating alcohol consumption for critical care admissions. Furthermore, in our study, two centres were able to record an answer for alcohol intake for every patient, demonstrating that it is feasible to incorporate an alcohol history into routine history-taking. Given the apparent evidence of impact of alcohol use on critical care services, this would appear to be something that other centres should aim to achieve routinely.
Evaluating the outcomes according to reason for admission, there was no significant difference between the groups in APACHE scores or mortality, although the alcohol-related admissions had a greater number of ventilated days.
Interestingly, if patients with chronic alcohol-related disease are included in the analysis, these patients were significantly more likely than those without alcohol-related disease or alcohol as a reason for admission to die in ICU (25% vs. 14%) but if they survived to ward discharge were significantly less likely to die on the ward than the rest of the cohort (10% vs. 24%). Alcohol-related patients appear to fall into one of two main subgroups: patients who are chronically unwell, e.g. with alcohol-related liver disease, who die on ICU; and younger binge-drinkers who are admitted unconscious or fitting, require a brief period of airway protection and invasive ventilation but recover quickly.
Among our patients, we found that 15% of those admitted with acute intoxication died and 47% of those admitted with chronic alcohol-related morbidity died, compared with 21% total mortality in the whole cohort of admissions.
It therefore appears that patients with a significant alcohol history are less likely to survive ICU admission even if admitted for a reason not directly related to alcohol, for example pneumonia.
Comparing our data with other published work, the recent Scottish study by Geary et al.4 identified a similar demographic (young and male) among alcohol-related admissions to ICU. However, the impact of alcohol on clinical outcomes following ICU admission appears to be somewhat inconsistent. Our study and that by Geary et al. found no difference in ICU length of stay between groups, whereas a single-centre study from Dublin showed a longer length of ICU stay for alcohol-related admissions, and another single-centre study in Finland showed shorter length of stay. McKenny et al.10 and Uusaro et al.11 showed higher ICU mortality in the alcohol-related admissions group, while the other studies demonstrated no difference.
The main strength of our study is the prospective collection across different units at the same time. Weaknesses include the fact that information on background alcohol intake was missing in 24% of cases, and that one large intensive care unit was not included in the study. This is also the neurosurgical centre, so most patients with significant head injuries as a result of alcohol would have been admitted there. As we only included general intensive care units, we may also have missed a number of alcohol-related admissions to the Welsh Centre for Burns and Plastic Surgery and the neurosurgical high dependency unit. This may mean that we have actually underestimated the impact of alcohol on intensive care admissions in Wales.
This study has also provided us with an interesting and valuable snapshot of intensive care activity across Wales, a country with among the lowest numbers of ICU beds per capita in Europe (3.2. per 100,00012). The study indicated a relatively high number of admissions during what is traditionally believed to be a ‘quiet’ time of year. Overall, there was 18% ICU mortality and 24% hospital mortality. These outcomes are comparable with a large study looking at 167 intensive care units across 17 European countries, which showed 19% ICU mortality and 24% hospital mortality.13
The vulnerability of critical care services in Wales to alcohol-related morbidity is striking. Public Health data show that alcohol is the cause of 1.5% of all hospital admissions in Wales annually,2 whereas in our study, alcohol was responsible for a 6-fold greater proportion of ICU admissions. We might hypothesise that alcohol-related admissions are more unwell than the general hospital population and more likely to require organ support. However, overall our study demonstrates the high burden alcohol abuse places on intensive care resources in Wales.
An intensive care bed costs just under £2000 per day so if we extrapolate our figures over 12 months (estimating the biggest unit to have similar numbers of admissions to the 2nd largest unit), the estimated cost to the Welsh NHS for ITU admissions due to alcohol is £6.8 million per year.
Tackling alcohol misuse is a stated priority of the Welsh Assembly Government14 but the issue remains challenging. Alcohol unit labelling and pricing appear possible options, though the World Health Organisation global strategy for tackling alcohol misuse extends beyond this to include marketing and availability, minimum unit pricing, drink driving policies, education and information, community action policies, licensing laws limiting availability of alcohol and mandatory labelling of alcoholic beverages with a health warning.1
Treatment of alcohol dependence has short- and long-term economic benefits. It is suggested that provision of alcohol treatment to 10% of the dependent drinking population in the UK would reduce public sector resource costs by between £109 million and £156 million each year, and analysis from the United Kingdom Alcohol Treatment Trial suggests that for every £1 spent on alcohol treatment, the public sector saves £5.15
Alcohol liaison teams who support patients through their admission and after discharge in the community have been shown to reduce readmission rates and bring about financial savings.14
Targeted strategies such as simple brief interventions take about 5 min and can be undertaken by any competent practitioner. The key to success is the timing of delivery during a ‘teachable moment’ and the patient can be given written self-help material, signposts to further information and support and advice on accessing follow-up help. More comprehensive methods include extended brief interventions, motivational enhancement therapy, cognitive behavioural therapy and the use of integrated care pathways, which should all be delivered by experts.15
There is much work to be done but any interventions that reduce the problem of alcohol abuse in Wales will be extremely welcome within the critical care community to reduce the huge burden on limited resources that exists currently.
Acknowledgements
We wish to thank Dr Geary and team in Scotland for kindly sharing their resources and allowing us to use their proforma for data collection.
We thank our hardworking team – Welsh Intensive Care Research Group (WICSARG) Investigators: Alison Ingham, Carys Wyn Hughes-Jones, James Hunter, Jana Anandarajah, Charlotte Draper, Lesley Bensted, Louisa Graham-Wollard, Ceri Brown, Lauren Davies, Karen James, Tom Bromfield, Richard Self, Gareth Roberts, Bethan Gibson, Karen Jones, Eloise Dawe, Ellie Powell, Edward Curtis.
Declaration of conflicting interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1.World Health Organisation. Global strategy to reduce the harmful use of alcohol, Geneva: WHO Press, 2010. [Google Scholar]
- 2.Public Health Wales Observatory. Alcohol and health in Wales, Carmarthen: Public Health Wales Observatory, 2014. [Google Scholar]
- 3.Gacouin A, Tadie J, Uhel F, et al. At-risk drinking is independently associated with ICU and one-year mortality in critically ill nontrauma patients. Crit Care Med; 42: 860–867. [DOI] [PubMed]
- 4.Geary T, O’Brien P, Ramsay S, Cook B. A national service evaluation of the impact of alcohol on admissions to Scottish intensive care units. Anaesthesia 2012; 67: 1132–1137. [DOI] [PubMed] [Google Scholar]
- 5.Office for National Statistics. Office of national statistics: Annual mid-year population estimates, London: Office for National Statistics, 2014. [Google Scholar]
- 6.Office for National Statistics. Adult drinking habits in Great Britain, London: Office for National Statistics, 2014. [Google Scholar]
- 7.Wales Centre for Health. A profile of alcohol and health in Wales, Cardiff: Public Health Wales, 2009. [Google Scholar]
- 8.Boniface S, Kneale J, Shelton N. Drinking pattern is more strongly associated with under-reporting of alcohol consumption than socio-demographic factors: Evidence from a mixed-methods study. BMC Pub Health 2014; 14: 1297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Welch C, Harrison D, Short A, et al. The increasing burden of alcoholic liver disease on United Kingdom critical care units: Secondary analysis of a high quality clinical database. J Health Serv Res Pol 2008; 13(Suppl 2): 40–44. [DOI] [PubMed] [Google Scholar]
- 10.McKenny M, O’Beirne S, Fagan C, et al. Alcohol-related admissions to an intensive care unit in Dublin. Irish J Med Sci 2010; 179: 405–408. [DOI] [PubMed] [Google Scholar]
- 11.Uusaro A, Parviainen I, Tenhunen JJ, et al. The proportion of intensive care unit admissions related to alcohol use: A prospective cohort study. Acta Anaes Scand 2005; 49: 1236–1240. [DOI] [PubMed] [Google Scholar]
- 12.Welsh Government. Together for health: Annual report for the critically Ill, Cardiff: Welsh Government, 2014. [Google Scholar]
- 13.Capuzzo M, Volta C, Tassinati T, et al. Hospital mortality of adults admitted to Intensive Care Units in hospitals with and without Intermediate Care Units: A multicentre European cohort study. Crit Care 2014; 18: 551–558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.National Assembly for Wales Health and Social Care Committee. Alcohol and substance misuse, Cardiff: National Assembly for Wales Commission, 2015. [Google Scholar]
- 15.Raistrick D, Heather N and Godfrey C. Review of the effectiveness of treatment for alcohol problems. London: National Treatment Agency for Substance Misuse, 2006.