Abstract
Introduction
Focused echocardiography is widely used to assist clinical decision-making in critically ill patients. In the UK, the Focused Intensive Care Echo protocol is recommended by the Intensive Care Society to ensure consistency of approach and guarantee training standards. Concerns remain about the reliability of information attained by non-expert clinicians in focused echocardiography, particularly when this is used to alter clinical management.
Methods
A prospective, observational evaluation of 60 consecutive patients undergoing Focused Intensive Care Echo studies in a single ICU.
Results
A complete Focused Intensive Care Echo study was possible in 43/60 scans (72%) and new diagnostic information obtained following 41/60 scans (68%), which lead to a change of clinical management in 28/60 (47%) of cases. In 24/60 (40%) of cases, a full transthoracic study was subsequently undertaken by a fully accredited sonographer. There were no cases where the results from the full study contradicted those from the limited Focused Intensive Care Echo study; additional diagnostic information was attained following 68% of full studies.
Conclusion
Focused echocardiography using the Focused Intensive Care Echo protocol is feasible and clinically useful in a high proportion of ICU patients. However, many still require additional expert echocardiographic assessment. Focused echocardiography delivered by non-experts is clinically useful in this setting but its limitations must be understood and access to expert assessment should be available.
Keywords: Intensive care, echocardiography, Focused Intensive Care Echo, haemodynamic monitoring, cardiac output
Introduction
Trans-thoracic echocardiography (TTE) is used routinely in the clinical assessment of critically ill patients.1 Undertaken by competent practitioners, it permits real-time, dynamic assessment of haemodynamic parameters, assists the diagnosis of shocked patients and permits titration of therapeutic modalities. Several prospective studies, utilising differing scanning protocols, have reported that TTE provides new diagnostic information, which can lead to a change in management in critically ill patients.2–8 Echocardiography has proven utility in the management of critically ill patients; in a study of scans undertaken in a UK intensive care unit (ICU) by clinicians fully accredited in TTE by the British Society of Echocardiography (BSE), the intensive care unit management changed in 49% of cases.9
Achieving full accreditation in echocardiography (e.g. as required by BSE or European Association of Echocardiography (EAE)) is a lengthy process involving over 2 years of sonographic training, a comprehensive logbook and examinations. It is impracticable for many UK intensive care units to train a large proportion of their intensivists to this standard. However, many life-threatening causes of shock can be diagnosed and quantified by a focused echocardiographic assessment with a significantly lower training burden. Consequently, there has been widespread support for the provision of basic-level echocardiography training to clinicians working within critical care,10–12 including Focused Intensive Care Echo (FICE),13 Focused Echo in Emergency Life Support (FEEL)14 and others.
FICE is one such training scheme which provides an achievable route to competency in conducting a focused echocardiographic assessment of the critically ill patient.13 This protocol is designed to identify clinically relevant left and right ventricular pathology, along with the presence of pericardial or pleural fluid. FICE accreditation can be realistically attained within the context of speciality training in intensive care medicine, by attending an approved course, completing an e-learning module15 and conducting a minimum of 50 focused scans under supervision, followed by a triggered assessment of scanning and interpretation ability. However, there remain concerns about the reliability of diagnostic information obtained by non-experts from focused TTE scans in a population cohort in whom it may be technically difficult to obtain high-quality images, for example due to rapidly changing physiology, the effects of positive-pressure ventilation, inotropic and mechanical cardiovascular support, tachyarrhythmias and sub-optimal patient positioning. These concerns relate most importantly to the possibility of missed echocardiographic pathology, or the misinterpretation of images leading to deleterious changes in clinical management.11,12
It currently remains unclear how focused echocardiography compares to full BSE-standard examinations in critically ill patients. We therefore undertook a service evaluation to investigate the impact of focused echocardiography utilising the FICE protocol on the management of patients in our department, the frequency with which full TTE studies were subsequently undertaken, and whether the results of the full studies contradicted those of the FICE scans or provided additional information.
Methods
We conducted a prospective, observational study evaluating the utility of the FICE protocol in the management of critically ill patients in a large university teaching hospital ICU. Our critical care department is a 30-bedded unit, which admits both medical and surgical critically ill patients, and includes quaternary services including cardiovascular surgery and solid organ transplantation. This study was reviewed by the chair of the local research ethics committee (REC) and considered to be service evaluation; a full REC submission was therefore deemed unnecessary.
All consecutive patients admitted to the intensive care unit during the study period (August 2014–June 2015) who received a FICE study as part of their management were included. This study did not include patients who had undergone cardiac surgery, who are routinely managed in a separate ICU. Scans were trans-thoracic, conducted utilising the FICE protocol and carried out using a Vivid S6 cardiovascular ultrasound system (GE Healthcare, UK) or M-Turbo ultrasound system (Sonosite, UK). Image acquisition and interpretation was performed either by or under direct supervision of FICE-accredited physicians and reported according to FICE guidelines.13 Only FICE studies required as part of the clinical management of the patient were included, and studies performed primarily for training purposes were excluded. ‘Full’ BSE standard echocardiograms were undertaken by cardiac sonographers or BSE-accredited physicians.
Data were prospectively collected and included the indication for performing echocardiography, image quality, number of satisfactory views, findings and changes in management as a result of the study. Clinical information, including the reason for ICU admission, current cardiac rhythm, diagnosis and ventilation mode was also collected.
A complete FICE study achieved all four echocardiographic windows described by the FICE protocol (parasternal long-axis, parasternal short-axis, apical four-chamber, subcostal four-chamber including IVC view) plus views of the lung bases. When a study was incomplete, the number of windows attained was recorded. Clinicians were asked to state whether the FICE scan provided an answer to the clinical question they were asking. Significant impairment of LV function, LV dilatation, RV dilatation or severely impaired function, the presence of pericardial or pleural fluid or hypovolaemia were recorded as per the FICE protocol. A change in management was defined as an alteration in the clinical care of the patient (adjustment in therapeutic interventions or initiation of new investigations other than TTE) as a direct consequence of conclusions drawn from the FICE report. Full BSE studies were undertaken when clinically indicated to fully evaluate new pathology suspected by FICE scanning, or where information not supplied by FICE was required, such as assessment of valvular function. When a full BSE examination was undertaken, any echocardiographic diagnoses misdiagnosed or missed on FICE scanning were recorded.
Results
In total, 60 FICE studies were performed during the study period. Of these, 46 (77%) were performed on patients receiving invasive positive pressure ventilation (median PEEP 5 cm H2O, IQR 5–10 cm H2O), five on patients receiving non-invasive ventilation, and nine on patients receiving no respiratory support other than facemask oxygen. Thirty-two studies were undertaken by clinicians accredited by FICE (26 by ICM consultants, 3 by ICM specialty registrars and 3 by cardiology specialty registrars) and 28 by ICM specialty registrars directly supervised by FICE mentors. The indications for requesting a FICE study are detailed in Table 1.
Table 1.
Indication for undertaking FICE scan.
| Indication | Number (%) |
|---|---|
| Diagnosis of hypotension | 16 (26.7%) |
| Assessment of volume status | 18 (30.0%) |
| Assessment of LV function in haemodynamic shock | 28 (46.7%) |
| Assessment of LV function following suspected MI | 8 (13.3%) |
| Assessment of respiratory failure | 5 (8.3%) |
| Diagnosis of suspected PE | 3 (5.0%) |
| Assessment of pericardial effusion | 3 (5.0%) |
| Assessment of RV function | 3 (5.0%) |
Indications for undertaking FICE scan. Totals do not summate to 60 as some patients had multiple indications.
A complete FICE scan was obtained in 43 studies (71.6%, all four echocardiographic windows specified by FICE plus lung bases), three windows were obtained in eight studies (13.3%), two windows in five studies (8.3%) and one window in one study (1.7%). The scanning clinician rated the quality of the view obtained as good or adequate on 52 occasions (86.6%).
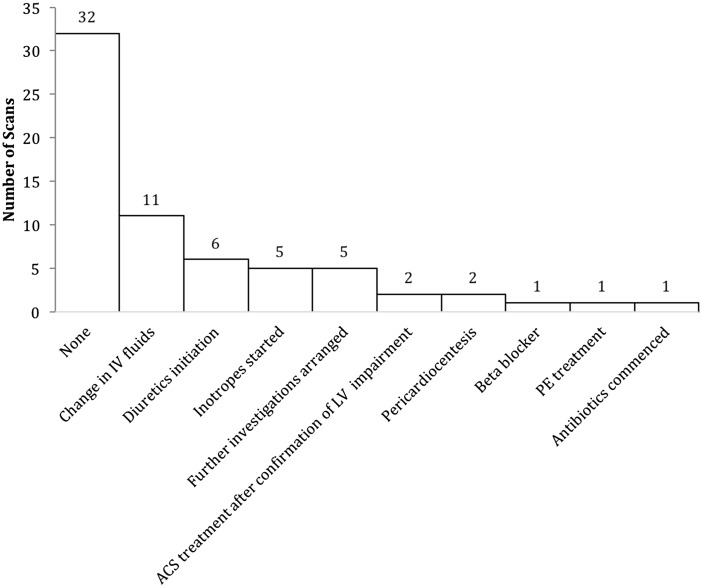
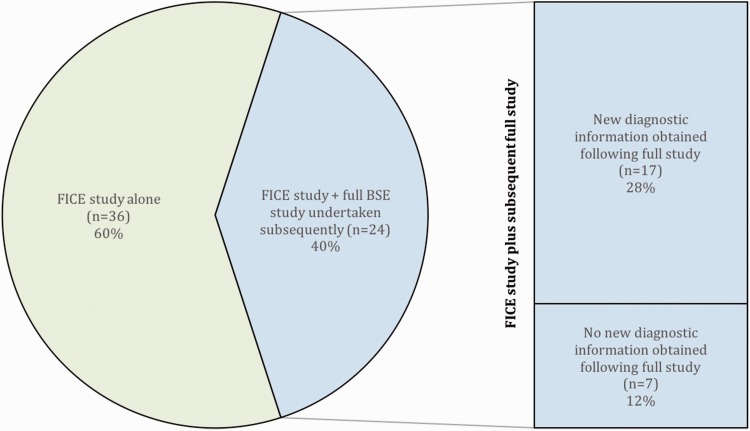
Previously unknown echocardiographic findings were diagnosed following 41 of 60 FICE studies (68.3%). The most common diagnosis was significantly impaired left ventricular function (16 studies, 26.6%), followed by hypovolaemia (15 studies, 25%), pericardial effusion (7 studies, 11.7%), pleural effusion (6 studies, 10%) and right ventricular dilatation (4 studies, 6.7%). Echocardiographic findings led to a change in management in 28 cases (47.7%, Figure 1). This included alteration of IV fluid therapy (11 cases, 18.3%), diuretic therapy (six cases, 10%), initiation of vasopressors/inotropes (five cases, 8.3%), further diagnostic procedures, e.g. CTPA (five cases, 8.3%), pericardiocentesis (two cases, 3.3%), treatment of acute coronary syndrome (two cases, 3.3%), initiation of beta-blockers (one case, 1.7%), treatment of pulmonary embolus (one case, 1.7%) and commencement of antibiotic therapy (one case, 1.7%). Scanning clinicians considered that the FICE scan sufficiently answered the clinical question they were posing in 54 cases (90%). Following 24 of the 60 FICE studies (40%), a full BSE study was subsequently undertaken (Figure 2).
Figure 1.
Change in management as a direct result of echocardiographic findings.
Figure 2.
Additional information provided by full BSE study.
There were no cases in which the results of the full BSE study contradicted those of the FICE study. RV dilatation with impaired function was diagnosed on one full study, but not recorded following the preceding FICE scan; there were no other significant findings that were missed on FICE studies. However, in 17 of the 24 full BSE studies (70.8%), additional diagnostic information was provided relating to valvular function (11 cases), assessment of endocarditis (3 cases), bubble studies for patent foramen ovale (1 study), assessment of PA pressure (1 study) and assessment of diastolic dysfunction (1 study). There were 21 patients who had new diagnoses following FICE, but who did not then undergo full BSE scanning; these new findings related to hypovolaemia (11 cases), LV impairment (6 cases), pleural effusion (5 cases), pericardial effusion (2 cases) and RV dilatation (3 cases).
Discussion
This study demonstrates that focused echocardiography delivered by FICE trained critical care clinicians in our unit provided additional clinical information leading to a change in management following almost half of conducted studies. A complete FICE protocol study was attainable in 71.6% of studies, most of which (77%) were performed in invasively ventilated patients. The quality of the view was good or adequate in the large majority of scans, even when a full series of windows could not be attained. Although a full BSE scan was only requested following fewer than half of the FICE scans, new diagnostic information was provided in a further 68% of these full studies. There were no instances recorded in which findings from the full BSE study contradicted those from the FICE study, and the additional information obtained required a level of echocardiographic interpretation, which was beyond that expected by the FICE protocol. This nonetheless suggests that specialist input from an individual accredited by the BSE or the EAE is still required in a significant number of situations.
The use of focused echocardiography in critical care and implications for clinical decision-making was summarised in a recent systematic review by Heiberg and colleagues.16 Whilst there is currently no evidence from randomised controlled trials that the use of focused echocardiography in the intensive care unit improves outcomes, six prospective observational studies (comprising a total of 1507 focused scans) have investigated its impact in clinical decision-making in the critical care setting.3–8 There is considerable heterogeneity in the inclusion criteria, sonographic expertise and scanning experience of clinicians in these studies. Importantly, none of these published full studies evaluate the FICE protocol, which is the most commonly utilised focused echocardiographic protocol in United Kingdom intensive care units and the only protocol recommended by the UK Intensive Care Society for clinicians training in the specialty.13 We were able to find one study, reported in abstract only, which specifically utilised the FICE protocol in 39 scans by FICE-accredited clinicians.17 Three of the full published studies reported a change in diagnosis following intensive care echocardiography using differing non-FICE protocols in 33–37% of cases.5,6,8 New diagnostic information was attained in a higher proportion of focused scans in our study (68.3%), which may reflect the severity of underlying critical illness and physiological derangement in our cohort, the majority of whom were invasively ventilated, the use of the FICE protocol or different echocardiography experience among our medical staff. In common with these studies, the most common new diagnosis in our study was LV dysfunction (16 studies, 26.7%). New valve disease was also diagnosed in a high proportion of cases in these studies, although assessment of valvular function is not part of the FICE protocol and would therefore not be assessed by focused echocardiography in our study. We reported a change in management following 47.7% of scans, which is comparable to the 35–51% reported by the five studies evaluating this.3–5,7,8 In common with these studies, alterations in fluid therapy and vasoactive drugs were the most common interventions following focused echocardiography.
To our knowledge, this is the first prospective evaluation to fully report the diagnostic yield and implications for clinical decision making following focused echocardiography using the FICE protocol in critically ill patients. It demonstrates that use of the FICE protocol by suitably trained critical care clinicians is able to detect diagnostic information, which leads to a change in patient-management in a critically ill cohort. We are also the first group to report the additional information attained by BSE level sonographers above that attained by a FICE scan, and to compare the findings between FICE and expert BSE sonographers. This provides some reassurance that the FICE protocol utilising non-expert clinicians does not lead to significant diagnostic error in our ICU. Our study results are broadly comparable to other observational studies of focused echocardiography using different scanning protocols. Whilst Manasia et al. report their experience of non-expert sonographers performing focused scans,5 other published studies utilised sonographers who were classed as experts. Our study therefore makes an important contribution to the evidence that non-expert clinicians can be trained to undertake clinically useful TTE in this setting.
The limitations of our study are as follows: As a single-centre, observational study of 60 focused scans, our results should be interpreted with caution. We furthermore were unable to assess for diagnostic error in the results of FICE scans when a subsequent full study was not undertaken. Twenty-one patients had new echocardiographic diagnoses but did not undergo full BSE scanning. The reasons for this include clinician satisfaction with the information provided by the FICE scan (e.g. hypovolaemia or pleural effusion); FICE protocol scanning undertaken by experienced clinicians who did not feel an additional scan was required; non-availability of expertise for full BSE scan; other clinical reasons, e.g. deterioration of patient and withdrawal of life-sustaining treatment or transfer to other facilities.
The evidence-base for the use of focused TTE in the intensive care unit is heterogenous and comprises only observational studies and expert consensus opinion.11 As the FICE protocol becomes more widely used within the setting of UK intensive care units, we hope that other groups will report their experience and contribute to an evidence base that includes the effect of focused echocardiography and specifically the FICE protocol on clinically meaningful outcome measures. A randomised-controlled trial of focused echocardiography may well be impracticable due to impossibilities of blinding, very large numbers required to detect a meaningful difference in outcomes such as mortality, and perceived lack of equipoise. However, we suggest that a prospective study in a large critically ill cohort, comparing the results from focused FICE studies with the results of a full study undertaken afterwards by a BSE or EAE-accredited sonographer, is likely to provide further confidence in the reliability of the FICE protocol.
Conclusion
In a single centre observational study, we found that focused cardiac ultrasound according to FICE protocol delivered by non-experts in a critical care setting was possible in the vast majority of patients and yielded clinically useful information. Almost half of the reported studies required further evaluation by an expert sonographer and although these studies did not contradict the initial focused study, additional information was offered in a further 68%. FICE protocol focused echocardiography is clinically useful in this setting, but its limitations must be understood and access to expert assessment should be available.
Declaration of conflicting interests
The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: MG is a Chief Scientists Office (Scotland) NHS Research Scheme Clinician.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1.Farkas JD, Anawati MK. Bedside ultrasonography evaluation of shock. Hospital Med Clin 2015; 4: 135–149. [Google Scholar]
- 2.Breitkreutz R, Price S, Steiger HV, et al. Focused echocardiographic evaluation in life support and peri-resuscitation of emergency patients: a prospective trial. Resuscitation 2010; 81: 1527–1533. [DOI] [PubMed] [Google Scholar]
- 3.Joseph MX, Disney PJS, Da Costa R, et al. Transthoracic echocardiography to identify or exclude cardiac cause of shock. Chest 2004; 126: 1592–1597. [DOI] [PubMed] [Google Scholar]
- 4.Kanji HD, McCallum J, Sirounis D, et al. Limited echocardiography-guided therapy in subacute shock is associated with change in management and improved outcomes. J Crit Care 2014; 29: 700–705. [DOI] [PubMed] [Google Scholar]
- 5.Manasia AR, Nagaraj HM, Kodali RB, et al. Feasibility and potential clinical utility of goal-directed transthoracic echocardiography performed by noncardiologist intensivists using a small hand-carried device (SonoHeart) in critically ill patients. J Cardiothorac Vasc Anesth 2005; 19: 155–159. [DOI] [PubMed] [Google Scholar]
- 6.Marcelino PA, Marum SM, Fernandes APM, et al. Routine transthoracic echocardiography in a general Intensive Care Unit: an 18 month survey in 704 patients. Eur J Intern Med 2009; 20: e37–e42. [DOI] [PubMed] [Google Scholar]
- 7.Orme RML, Oram MP, McKinstry CE. Impact of echocardiography on patient management in the intensive care unit: an audit of district general hospital practice. Br J Anaesth 2009; 102: 340–344. [DOI] [PubMed] [Google Scholar]
- 8.Stanko LK, Jacobsohn E, Tam JW, et al. Transthoracic echocardiography: impact on diagnosis and management in tertiary care intensive care units. Anaesth Intensive Care 2005; 33: 492–496. [DOI] [PubMed] [Google Scholar]
- 9.Alam S, Docherty A, Mackle I, et al. The introduction of intensive care-led echocardiography into a tertiary care unit. J Intensive Care Soc 2013; 14: 15–19. [Google Scholar]
- 10.Expert Round Table on Ultrasound in ICU. International expert statement on training standards for critical care ultrasonography. Intensive Care Med 2011; 37: 1077–1083. [DOI] [PubMed] [Google Scholar]
- 11.Via G, Hussain A, Wells M, et al. International evidence-based recommendations for focused cardiac ultrasound. J Am Soc Echocardiogr 2014; 27: 683, e1–683.e33. [DOI] [PubMed] [Google Scholar]
- 12.Levitov A, Frankel HL, Blaivas M, et al. Guidelines for the appropriate use of bedside general and cardiac ultrasonography in the evaluation of critically ill patients-part II: Cardiac ultrasonography. Crit Care Med 2016; 44: 1206–1227. [DOI] [PubMed] [Google Scholar]
- 13.Intensive Care Society. Focused Intensive Care Echo, http://www.ics.ac.uk/ICS/fice.aspx (accessed 20 October 2016).
- 14.Resuscitation Council (UK). FEEL - Focused echocardiography in emergency life support, https://www.resus.org.uk/information-on-courses/focused-echocardiography-in-emergency-life-support/ (accessed 14 November 2016).
- 15.e-learning for Healthcare. Intensive care echo and basic lung ultrasound (ICE-BLU), http://www.e-lfh.org.uk/programmes/icu-echoultrasound/ (2017, accessed 16 January 2017).
- 16.Heiberg J, El-Ansary D, Canty DJ, et al. Focused echocardiography: a systematic review of diagnostic and clinical decision-making in anaesthesia and critical care. Anaesthesia 2016; 71: 1091–1100. [DOI] [PubMed] [Google Scholar]
- 17.Strachan J. Focussed echocardiography in intensive care – A completed audit cycle implementing a standardised reporting tool. Intensive Care Society Clinical Practice Free Paper Presentations Tuesday, December 8, 2015. J Intensive Care Soc 2015; 16: 16–21.28979363 [Google Scholar]