Abstract
Early career academic cardiologists, whom many believe are an important component of the future of cardiovascular care, face a myriad of challenges. The Early Career Section Academic Working Group of the American College of Cardiology (ACC) along with senior leadership support, assessed the progress of this cohort from 2013–2016 with a global perspective. Data consisted of accessing National Heart Lung and Blood Institute (NHLBI) public information, American Heart Association and international organizations providing data, and a membership-wide survey. Although NHBLI increased funding of career development grants, only a small number of early career ACC members have benefited as funding of the entire cohort has decreased. Personal motivation, institutional support, and collaborators continued to be positive influential factors. Surprisingly, mentoring ceased to correlate positively with obtaining external grants. Totality of findings suggests that the status of early career academic cardiologists remain challenging; therefore, we recommend a set of attainable solutions.
Keywords: Early Career Academic Cardiologist, Mentoring, Physician-Scientist, Clinician-Scientist, Cardiology Profession
Background
Cardiovascular disease (CVD) is the number one cause of morbidity and mortality globally, and its incidence is rising at an alarming rate (1). In the United States (U.S.) alone, it is projected that by the year 2030, 45% of the population will have at least one CVD condition (2). Notably, after a long period of sustained decline in age adjusted CVD death rate (1950–2014) (3), age adjusted death rates for heart disease and stroke in the US demonstrated statistically significant increases from 2014 to 2015 (4). To address this rising burden of cardiovascular disease, society relies on academic cardiologists in all settings to drive research (basic, translational, clinical, and population) and to train the next generation of cardiologists. Thus, it is critical to maintain and renew the pipeline of early career academic cardiologists (Table 1).
Table 1.
Description of academic cardiology promotion tracks
| Academic Tracks | Roles, Efforts, Time Spent |
|---|---|
| (1) Scientist- researcher |
|
| (2) Clinician-scientist or Physician-scientist |
|
| (3) Clinician-educator |
|
| (4) Clinician-educator-administrator |
|
| (5) Pure clinician |
|
Early career academic cardiologists, defined as those within 10 years of completion of a cardiology fellowship, face enormous challenges. These challenges include limited funding, insufficient protected time, increased regulatory compliance burden, increased competition from pure Ph.D. scientists, and personal financial disincentives (5). This resulted in many cardiologists choosing to leave or never enter the academic workforce (5,6). As a response in 2014, the Early Career Section Academic Working Group of the American College of Cardiology (ACC), along with senior leadership, published a manuscript based on status of the funding environment, and inputs from staff members of the National Heart Lung and Blood Institute (NHLBI) of the National Institutes of Health (NIH), and a survey of ACC early career academic cardiologists. The manuscript summarized challenges faced by these early academicians and proposed potential solutions that could be implemented by the ACC, academic institutions, and policy makers to address these challenges (5). So how far have we come in the past 3 years? To address this question, the Early Career Section Academic Working Group of the ACC continued collaboration with staff of NHLBI, re-surveyed early career academic cardiologists, and this time, included one of the fastest growing segment of the ACC – international cardiologists.(7) Furthermore, the American Heart Association (AHA) and international representation also have joined this effort to provide a global view of the state of early career academic cardiology.
The purpose of this 2017 update is to inform the cardiovascular community, academic leadership, and policy makers on the progress of early career academic cardiologists since the previous publication (5) and present potential solutions. We hope this manuscript will serve as a catalyst for discussion and policy changes that will promote the survival and success of early career academic cardiologists and the profession as a whole.
METHODS
NHLBI personnel guided extraction of publicly accessible data. AHA provided their grant funding data. International representation (the German Center for Cardiovascular Research: Deutsches Zentrum für Herz-Kreislauf-Forschung – DZHK and ACC members working with their respective countries’ cardiology societies: Canada, India, Israel, Mexico) also provided data. Chief editors (Circulation and Journal of American College of Cardiology – Basic Translational Science) provided guidance. ACC conducted a membership-wide survey that was developed by the Academic Working Group of the Early Career Section of the ACC. Inclusion criteria consisted of self-identification as an academic cardiologist and ≤10 years from completion of cardiology fellowship.
Statistical analysis of the responses was performed using SPSS version 23. Z-tests and t-tests were used to identify significant differences for categorical and continuous variables respectively. Pearson and Spearman correlation tests were used to evaluate the strength of relationships between continuous and rank variables respectively.
RESULTS
Responses, Motivations, and Tracks
Invitations to participate were emailed to 9646 early career members of the entire ACC in January and February of 2016. Of the 1131/9646 (12%) responses, 558/1131 (49%) were included in the study, 283/1131 (25%) branched out as pure clinicians, and 290/1131(26%) did not meet inclusion criteria Majority of the respondents practiced in the US (80%). International members reside and practice outside of the US. The distributions of professional roles (i.e., academic tracks in Table-1) remained similar between 2013 and 2016 (Table 2). Thus, comparative analyses would not be confounded by different distribution of academic tracks (Figure 1).
Table-2.
Distribution of Roles
| Professional Role | 2013 Survey, n=291 | 2016 Survey, n=841 |
|---|---|---|
| 100% research | 0.7% | 0.7% |
| >75% research | 5.8% | 4.6% |
| 40–75% research | 10.0% | 9.3% |
| <40% research | 28.5% | 25.9% |
| Clinician-Educator | 18.6% | 18.5% |
| Clinician-Educator-Administrator | 11.3% | 7.3% |
| Pure Clinicians* | 25.1% | 33.7% |
Indicates early exit from survey; therefore, not included in follow-on analyses.
Figure 1. Early Career Academic Cardiologists’ Characteristics.
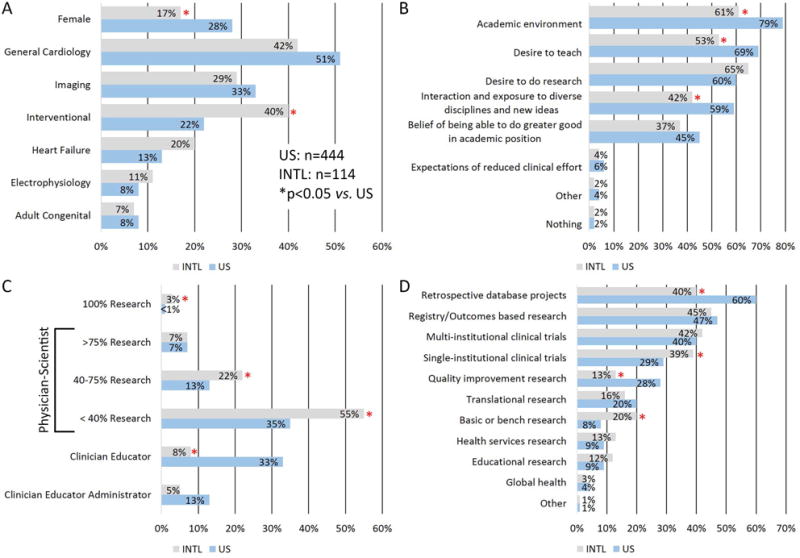
(A) Sex and practice type distribution, (B) Motivation for pursuing academic cardiology, (C) Academic track and % research effort distribution, (D) Type of research.
Key motivations for early career members to pursue academic cardiology consist of academic environment, desire to do research, desire to teach, and interaction/exposure to diverse disciplines and new ideas (Figure-1B). A significant portion of all respondents (22%) dedicated ≥40% of their professional effort in research. International members differed from US members with a greater percentage engaged in research (Figure 1C), a lesser percentage in teaching (Figure 1C), a greater proportion participating in basic science research and single-institutional clinical trial, and a lesser proportion participating in retrospective database projects and quality improvement research (Figure 1D).
Research Funding
After years of declining funding, NIH/NHLBI increased funding of career development K-grants from 2013 to 2015 (Figure 2). Mentored Clinical Scientist Development Award K-08 (e.g., basic-translation science research) success rate increased from 26% in 2013 to 51% in 2015. Mentored Patient-Oriented Research Career Development Award K-23 (e.g., clinical research) success rate increased from 30% in 2013 to 38% in 2015. In addition to funding more K-grants, NHLBI increased the amount of K-grant support from $500,000 to $625,000 (not including indirect costs) and developed a new limited competition grant for K-grant awardees to continue their development (RFA-HL-16-020)(8). NHLBI also increased funding rates of R01 grants from 14.1% in 2013 to 20.9% in 2016 (Online Figure 1). AHA fellow-to-faculty grants success rate declined (35% in 2013, 22% in 2016) and scientist development grant success rate slightly increased (16% in 2013, 19% in 2016); however, overall AHA grant success rates remained steady for last 10 years (Figure 2). Recently, ACC has established two new 1-year $70,000 grants (Keating and Presidential Awards) for early career investigators.
Figure 2. Funding Environment.
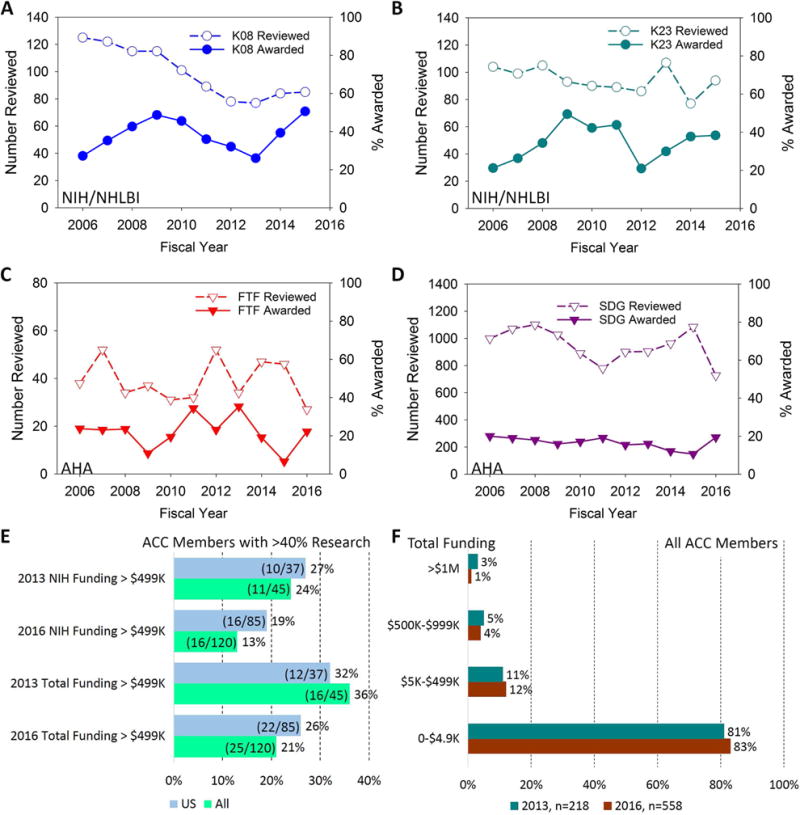
(A) National Institutes of Health/National Heart, Lung, and Blood Institute (NIH/NHLBI) funding of K-08 Mentored Clinical Scientist Development Award (Basic-Translation Research), (B) NIH/NHLBI funding of K-23 Mentored Patient-Oriented Research Career Development Award (Clinical Research), (C) American Heart Association (AHA) Fellow to Faculty transition award (three recipients declined the award in 2015 to depress the % for that year), (D) AHA Scientist Development Grant, (E) >$499K external funding for early career members with >40% research effort, (F) Funding distribution for all early career members for 2013 (only counted funding received as principal investigators (PIs)) and 2016 (counted funding received as PI, Co-PI, and Co-investigator).
With increased NHLBI funding in mind, we then evaluated a group that could have benefited from these increases. This group consists of US members who reported >40% research effort. NIH has defined >40% research as a significant research commitment(8) and the >40% threshold would likely include members who are committed to pursue research but have not yet received a K-grant. Using >75% research effort would have biased the sampling to those who likely already achieved K-grant or K-grant equivalent funding (because >75% research effort is an NIH K-grant requirement); thus, >75% research effort was not chosen. Within this group, achieving NIH funding > $499K changed from 27% (10/37) in 2013 to 19% (16/85) in 2016, and achieving NIH funding >$1.2M changed from 5.4%(2/37) in 2013 to 2.4% (2/85) in 2016 (Figure 2E). Thus, there were no increases in the combined NIH K-grant and R01-grant funding among early career ACC members despite the increased funding by the NHLBI.
To gain a global perspective, we then tallied total funding for all ACC members (Figure-2F). Despite the attempt to increase representation by including co-principal investigators and co-investigators that were not counted in the 2013 study, the percentage of members who do not receive external grant support edged upward from 81% in 2013 to 83% in 2016. There was 1% improvement for the $5K–$499K category. However, both top categories trended downward ($500K–$999K: 5% in 2013 to 4% in 2016; >$1M 3% in 2013 to 1% in 2016). Thus, external grant funding for the entire ACC early career population is likely to have decreased from 2013 to 2016 (Online Tables 1 and 2).
Matching publicly available NHLBI database of active K-grant awardees to the ACC database identified ACC early career academic cardiologists who successfully competed for NHLBI K-grants. Although the numbers are small, latest trends for ACC early career members achieving K-grants are encouraging (Figure 3). Among active K-grant awardees who achieved cardiovascular board certification, 25/90 (28%) are not members of the ACC.
Figure 3. K-Grant Awards for ACC Early Career Members.
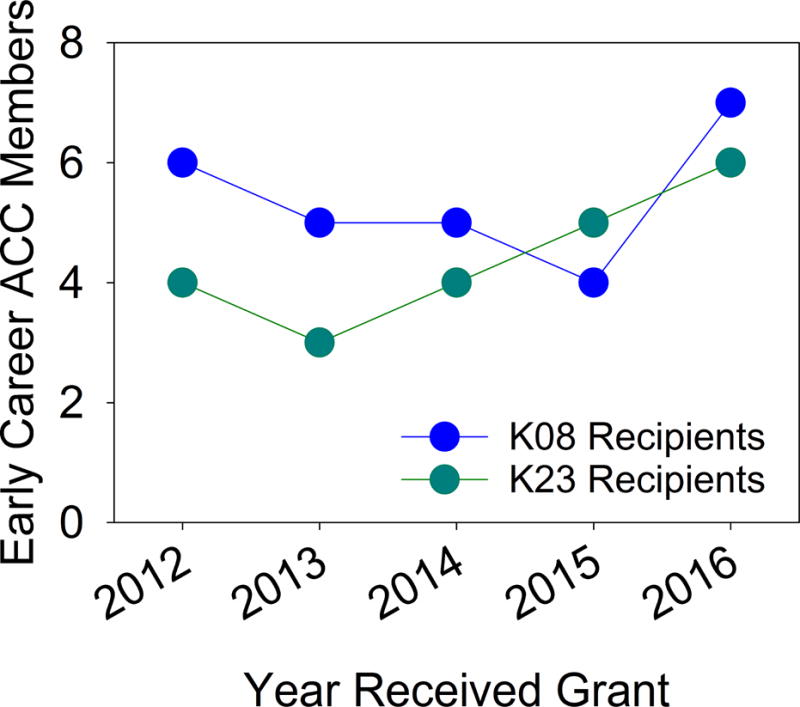
All fiscal year 2017 active NHLBI K-grants were extracted from NIH RePORTer. Principal investigators for these active K-grants were matched against ACC Membership database with ≤ 10 years from completing fellowship at the time of grant activation. The match showed number of ACC early career academic cardiologists successfully completing for K-grant by year. Of note, some of the K-grant recipients have aged out of the early career range at the time of 2016 survey.
We performed analyses by US states. The amount of fiscal year 2017 NIH research funding correlated with number of hospital beds and number of teaching hospitals (Figure 4A and B). Number of early career academic cardiologists (ECACs) also correlated with hospital beds and teaching hospitals (Figure 4C and D). However, ECAC funding did not correlate with amount of NIH research funding received by their state or number of teaching hospitals (Figure 4E and F).
Figure 4. Analyses by States of US.
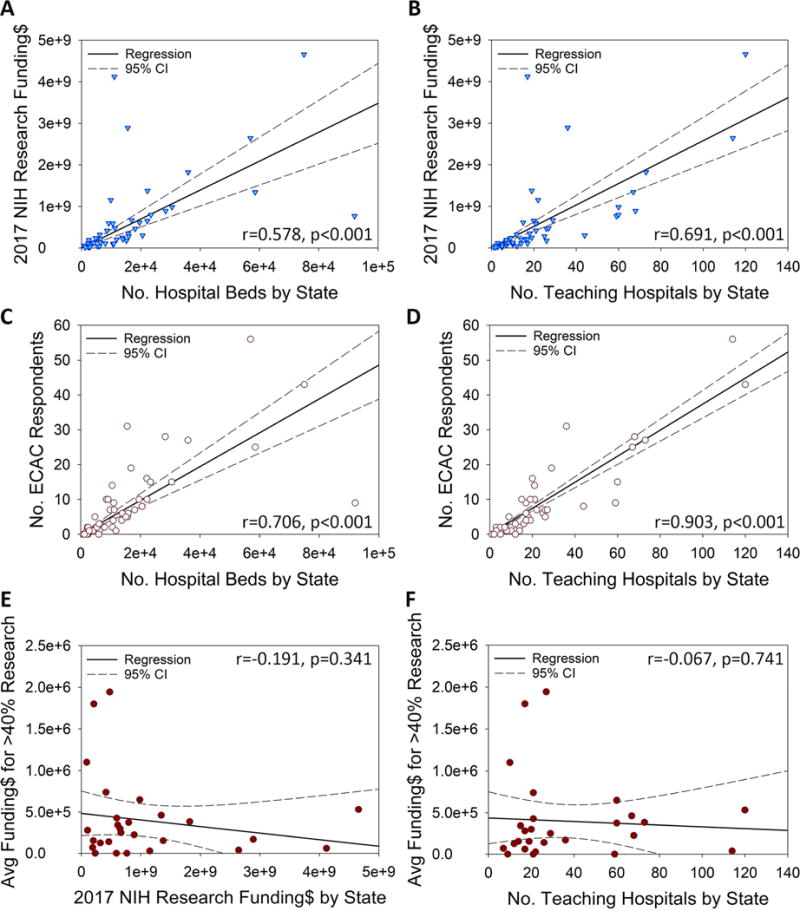
Fiscal year 2017 NIH research funding correlated with number of hospital beds (A) and number of teaching hospitals (B). Number of early career academic cardiologists (ECAC) correlated with number of hospital beds (C) and number of teaching hospitals (D). Average funding for ECACs with ≥ 40% research effort did not correlate with amount of NIH research funding received by state (E) and number of teaching hospitals by state (F). Data were extracted from NIH RePORTer,(16) Center for Medicare and Medicaid Services reporting of teaching hospitals,(17) and American Hospital Directory.(18)
Global Challenges
The vast majority (sum of top 2 affirmative response = 85% in Figure-5) of both US and international members believe that physicians should be a part of health care research, but ≥70% found lack of time as a challenge. Greater proportions of US members identified challenges of burdensome regulatory compliance, unstable external funding, and competing with pure PhDs. The use of clinical relative value units (RVU) without credit for research was also a greater challenge for U.S. members. While all members face challenges of home institutions not providing sufficient resources or funding, these challenges occur at greater proportions among international members (Figure 5).
Figure 5. Challenges and Resources.
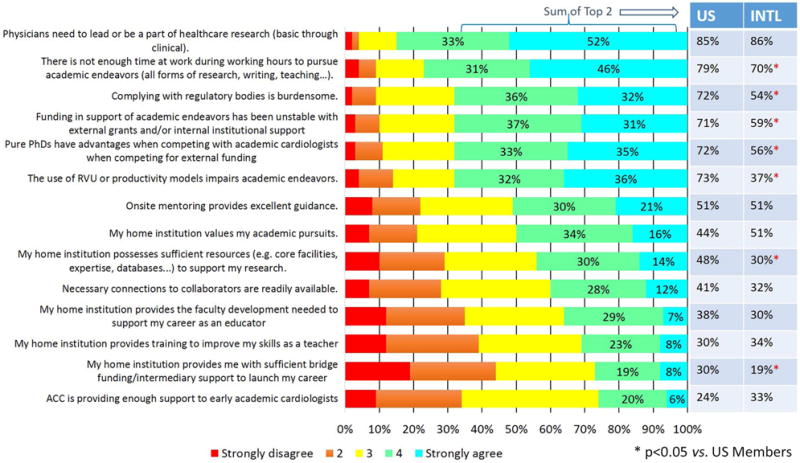
Respondents provided rating for their beliefs and experiences pertaining to academic pursuits. Comparisons were done on US vs. international members on summation of the top two agreement responses.
International members face limited external research funding streams with limited funding amounts, lack of access to international cardiovascular registries, and lack of research collaborations. For example, despite an increase in clinical trials conducted at international sites (9), international members have limited participation in large international registries such as the National Cardiovascular Data Registry (NCDR) (10), which may limit opportunities for transnational research collaborations. Additionally, many international exchange programs are mostly focused on clinical experiences rather than research collaborations (7).
Only a minority of both international and US members reported satisfaction with support for educator development (Figure 5). The status of clinician-educator will be addressed in a separate manuscript.
Factors Leading to Achieving External Grant Support
We performed correlation analyses to identify which factors were associated with achieving increasing levels of funding (Table 4). Input variables consisted of factor rankings (Figure 5) and funding range bins ($0, $1–99K, $100K–249K, $250–499K, >$500K). Spearman correlation was used because of rank data and skewed funding distribution. Positive correlation consists of resultant r > 0.1 (|r| has values 0 to 1) that reached statistical significance. The US members’ analysis identified factors that correlated with achieving increasing NIH grant amounts. The all members’ analysis (including international members) identified factors that correlated with achieving grants from any source. Personal motivation, home institution (resources, value placed on academic pursuits), and connection to collaborators correlated to increasing levels of grant funding for all years and all groups. Home institution providing sufficient bridge funding continued to be a positive correlating factor for increasing NIH funding for U.S. members.
Table-4.
Factors that correlated with increasing amount of external grant funding
| Factor | US NIH Total 2013 |
US NIH Total 2016 |
All Total 2013 |
All Total 2016 |
|---|---|---|---|---|
| [Motivation] Physicians need to lead or be a part of healthcare research | +↑ | +↑ | +↑ | +↑ |
| [Home Institution] My home institution provides me with sufficient bridge funding/intermediary support to launch my career. | +↑ | +↑ | — | +↑ |
| [Home Institution] My home institution possesses sufficient resources (e.g. core facilities, expertise, databases…) to support my research. | +↑ | +↑ | +↑ | +↑ |
| [Collaborators] Necessary connections to collaborators are readily available. | +↑ | +↑ | +↑ | +↑ |
| [Mentoring] Onsite mentoring provides excellent guidance. | +↑ | — | +↑ | — |
| [Home Institution] My home institution values my academic pursuits. | +↑ | +↑ | +↑ | +↑ |
| [Experience] Funding in support of academic endeavors has been unstable with external grants and/or internal institutional support. | — | +↑ | — | +↑ |
| [Experience] Complying with regulatory bodies is burdensome. | — | +↑ | — | +↑ |
Spearman Correlation was done between responses to challenges-resources factors (responses:1–5; 1:strongly disagree; 5:strongly agree) vs. obtained total grant amount by ranges (0, $1–99K, $100K-249K, $250–499K, ≥$500K).
 +↑ denotes positive correlation with p<0.05.
+↑ denotes positive correlation with p<0.05.
 — denotes no correlation. Mentoring changed from being a positive correlation factor for US members to obtain NIH grants to be non-contributory (2013: r=0.236, p=0.001; 2016: r=0.081, p=0.103). Mentoring changed from being a positive correlation factor for all members for all grants to be non-contributory (2013: r=0.241, p=0.001; 2016: r=0.070, p=0.115).
— denotes no correlation. Mentoring changed from being a positive correlation factor for US members to obtain NIH grants to be non-contributory (2013: r=0.236, p=0.001; 2016: r=0.081, p=0.103). Mentoring changed from being a positive correlation factor for all members for all grants to be non-contributory (2013: r=0.241, p=0.001; 2016: r=0.070, p=0.115).
Surprisingly, mentoring ceased to be a positive correlating factor for grant funding in 2016 (Table 4). We then performed a focused analysis on mentoring (Figure-6). Because US members with >40% research effort are positioned to apply for NIH K-grants, this group was analyzed. Pearson correlation of mentoring satisfaction vs. NIH grant funding showed positive correlation (r=0.333, p=0.025) in 2013 but a lack of any correlation (r= −0.05, p=0.327) in 2016. Applying this analysis to all members showed a similar pattern. Pearson correlation of mentoring satisfaction vs. total grant funding for all members showed positive correlation (r=0.225, p=0.001) in 2013 but lack of correlation (r= −0.036, p=0.349) in 2016.
Figure 6. Focused Mentor Excellence to Grant Funding Analyses.
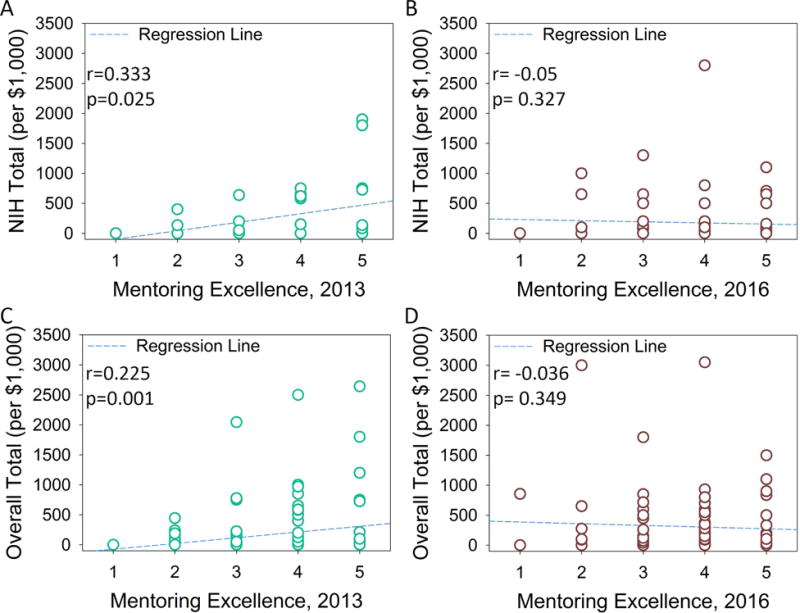
Early career members’ reported onsite mentoring provides excellent guidance 1-strongly disagree to 5-strongly agree were plotted against external grant amount received. (A) 2013 Total NIH funding for US members reporting > 40% of research effort, (B) 2016 Total NIH funding for US members reporting > 40% of research effort, (C) 2013 Total external funding for all members, (D) 2016 Total external funding for all members. Pearson correlation analyses were performed between members’ rating of mentoring to achieved grant support (correlation coefficient r and p values are listed within the figures).
US differed with international members on priority of potential research help. US members ranked seed grant and international members ranked receiving help in writing as the top useful help (Figure 7).
Figure 7. Penalties and Requested Help.

(A) Members’ reported salary reductions for pursuing academic cardiology with respect to their peers, (B) Reported application of relative value units (RVU), (C) Likelihood of leaving academic cardiology in the next 12 months, (D) Top three areas where members believe ACC can best meet their research needs.
Disincentives
Early career cardiologists suffered significant financial penalties when choosing an academic career (Figure 7). In 2013, 28% of the respondents gave up >$100,000/year to be in academics. This percentage has increased to 36% (11% internationals, 43% U.S.) in 2016. A greater percentage of international members (39%) do not incur any financial penalties for choosing academic cardiology than U.S. members (25%). The vast majority of US members (85%) are under a RVU system to receive credit for their clinical work, with 61% of these members reporting no credit for non-clinical endeavors. In contrast, only 27% of international members reported participation in a clinical revenue type of system. Similar percentages (13–14%) of international and US members reported high likelihood of leaving academics in the next 12 months. This is a slight increase from 11% in 2013. US members reported personal compensation being too low, and international members reported insufficient support for career development as the top reasons for leaving academic careers (Online Table 3).
DISCUSSION
Globally, the status of early career academic cardiologists has declined slightly since 2013; however, there were a number of positive developments as well. Negative items included: a global reduction in gaining funding for research has likely occurred (Figure 2, Online Tables 1 and 2); only a minority of respondents reported satisfaction in teaching development (Figure 5); the ability of mentoring to positively affect grant outcome has diminished (Figure 6); financial disincentives for pursuing academics is increasing (Figure 7); and 14% of early career members now reported high likelihood of leaving academics. In US, these results are consistent with a declining physician-scientist workforce as documented by NIH (6). Positive developments included: NHBLI has increased funding significantly through multiple mechanisms; ACC has provided new grants; and albeit currently small in numbers, ACC early career academic members continued to obtain NHLBI K-grants (Figure 3). In summation, continued attention needs to be directed towards the development of early career academic cardiologists.
Mentoring needs attention. A local mentor who can provide support, feedback, and when necessary hard-hitting critique, is pivotal importance in launching a physician-scientist’s career. All early career cardiologists need someone to whom “dumb questions” can be asked, someone who edits papers and grants with a fierce red pen, and someone who works through talks slide by slide. NIH has recognized the importance of the mentor; consequently, NIH formally evaluates the quality of applicants’ mentors in determining who will receive K-grants (11–13). Mentoring positively correlated with increasing grant funding in 2013 but not in 2016 while all other positive factors remain unchanged (Table 4, Figure 6). Together with ECACs’ inability to capitalize on NHBLI significantly increasing K-grant funding that specifically targets physician-scientists, mentoring appears to have lost its effectiveness. This can be caused by lost of effective mentors or mentoring ceasing to play a role. Regardless, restoring effective mentoring is crucial.
Different mentoring needs exist. NIH K-grant requirements include active R01 level funding, record of successful mentees, ability to support mentees’ research, actively publishing, and being the expert in the field (11–13). Early career members will also need guidance in career development, negotiating a faculty position, and negotiating institutional support. Conversely, those who desire to mentor also need helpful development. Mentoring does not happen spontaneously. Rather, a matchmaking process needs to occur and a beneficial relationship needs to develop. Currently, both mentoring needs and mentor development needs remain relatively unknown. Perhaps, the first step to restore effective mentoring is to gain a better understanding of the needs. Subsequently, mentor support programs can be developed.
The mixed success of early career members achieving career development level funding support needs attention. Results showed diverging trends of decreasing percentage of US early career members receiving NIH K-grant level of funding (Figure-2E), despite significant NIH/NHLBI funding increases (Figure-2A–B). However, we identified many board certified cardiologists with NIH K-grants who are not ACC members. Determining why these individuals have chosen not to join the ACC is a topic that needs to be addressed. Conversely, a very small core of members is having some success (Figure 3). We need to find ways to extend the success of this small core to others who want to pursue academic cardiology. Broadening the opportunities for protected research time can expand success to others. Trainees and early career physician-scientists must achieve first authorship in an original research paper and expertise in their selected area in order to be competitive in grant application (11) An MD-PhD has a chance to accomplish this difficult task in 2 years.(6,11) An MD with less experience will likely need ≥3 years.(6,11) Unfortunately, the current Accreditation Council for Graduate Medical Education 3-year cardiovascular disease program does not allow time for the development of this competitive portfolio.(14) Thus, the protected time to complete research training has to occur in addition to a 3-year cardiology fellowship. Paid instructor level or new faculty positions with at least 75% protected research time support the development of competitive portfolios. In fact, K-grant awardees hold these positions at the time of K-grant application.(15) Programs with active NIH T32 training grants, NIH Clinical Translational Science Awards (CTSAs), or institutional supported career development awards (Such as Vanderbilt’s Faculty Research Scholars Program) can provide these additional years of protected time. However, only a few centers currently provide these opportunties. Thus, we need to encourage interested institutions including private and community based healthcare systems to develop these early career faculty programs with protected research time outside of NIH funding to broaden opportunities.
This study also revealed that the transition from career development award (K-grant) to independent funding (R01 grant, which provides ≥ $1.25M) is a particularly vulnerable period. Early career members achieving >$1M grant support fell from 3% in 2013 to 1% in 2016. These very small and decling percentages may reflect ACC members encountering significant challenges in making the transition to independent funding. On average, it takes K-grant recipients longer than 4 years and >3 R01 proposal attempts before obtaining a R01 grant (15). K-grants require active practice licences; thus, physician-scientists are protected when competing for these grants. However, R01 grants have no such protection. With PhD-only scientists who do not have clinical responsibilities being much more numerous (11), K-grant recipients now face increased competition when applying for R01s. With the combination of financial disincentives (43% took > $100,000/yr pay reduction) and the pressure to meet clinical RVU goals (52% do not receive RVU for academic pursuits), these forces can easily push US academic cardiologists to do more clinical work instead of spending efforts on experiments and writing grants. This shift towards clinical work can reduce both the quality and quantity of proposals being submitted. Developing funding streams that support physician-scientists and minimizing the financial disincentives may help. Developing suitable methods to provide credit for academic pursuits may also alleviate the pressure for clinical productivity.
International early career members have similar characteristics but additional needs. All members chose academic cardiology for similar reasons (Figure 1). All members believe that cardiologists should participate in healthcare research (Figure 5). International members need help with expanding institutional research infrastructure, including participation in international research collaborations, cardiovascular registries, and diversification of research funding streams.
Limitations
ACC membership limitation and 12% response rate may not sufficiently represent the entire ECAC population’s progression. Life priorities will change with each ECAC generation. This study does not provide anwers on why the funding of U.S. ECACs do not reflect the resources of their respective states. As a solution, we would like to suggest the creation of a registry to follow early career academic cardiologists starting from their last year in fellowship training to 10 years of practice. Involving program directors and cardiology chiefs can increase participation. This registry potentially will provide more accurate and timely information.
CONCLUSIONS
We believe that successful development of early career academic cardiologists is critical for continued viability of cardiology as a profession as well as advancing improved cardiovascular care globally. As illustrated by our study, even with some bright developments, global status of early career academic cardiology remain uncertain. Based on our analyses, we propose a set of potentially attainable solutions (Table 5) and call on the cardiovascular medicine community’s to help implement them.
Table-5.
Recommendations
| Recommendations to ACC and Cardiovascular Professional Organizations |
|---|
| ✥ Continue to conduct studies on its members and publish results on regular basis (e.g., every 3 years) |
| ✥ Develop a registry that will follow a representative cohort of early career academic cardiologists in their progression over time (starting from last year of fellowship and follow for 10 years after completion of fellowship) |
| ✥ Conduct follow-on studies to fill in knowledge gaps |
| ➢ Mentoring needs (career development, becoming NIH funded principal investigator, contract negotiations) |
| ➢ Needs of the mentors (this can be critical to foster collegiate inter-generational communications and to ensure a base level of mentoring skills) |
| ➢ Early career members’ commitment and its associated needs (e.g. committed to academic cardiology, want to explore possibilities, committed to clinical care) |
| ✥ Promote mentoring |
| ➢ Provide mentoring workshops after identification of mentoring and mentors’ needs |
| ➢ Provide increased recognition beyond one award per year (e.g., by category: basic/translation/clinical, by stage: early-first 5 years of mentoring experience, middle-mentored from 5–15 years, senior-mentored for >15 years and has a record of mentees achieving independent faculty positions) |
| ➢ Upgrade existing mentoring database |
| ✥ Modify current early career junior faculty 1-year awards to cover at least 2 years |
| ➢ Require home institution to guarantee >50% research effort |
| ➢ As a possible no cost expanding method, funding one $70,000/yr for 2-year duration instead of two $70,000/yr grants for 1-year. |
| ➢ Consider seeking additional industry, philanthropy, and membership donation to fund this program |
| ➢ Consider expanding this program in the future after learning from results and establishing fund |
| ✥ Help to establish heart disease philanthropic foundation that will fund research and assist patients. (Susan G. Komen is a good example from breast cancer: their mission statement - “Save lives by meeting the most critical needs in our communities and investing in breakthrough research to prevent and cure breast cancer”). Unlike ACC and AHA, this foundation needs to be free from lobbying to maintain tax exemption and good will of contributing public. Better Business Bureau Wise Giving Alliance reported total program expenses for 2015: American Cancer Society $708,516,000; Susan G. Komen Foundation $217, 779,902; AHA $527,297,000. These numbers suggest that heart disease based foundation in addition to AHA is possible and needed. |
| ✥ Advocate for increased funding for NHLBI in T-32 training grants, career development grants, and research grant targeting early career physician-scientists |
| ✥ Develop workshop and exchange program to help international members in writing |
| ✥ Develop requirement statement for advanced cardiovascular research training (e.g. Level – II and Level-III) for the next iteration of ACC curriculum recommendation document COCATS |
| ➢ Writing team needs to include recent K-08, K-23, and R-01 recipients |
| ➢ NHBLI input will also be useful |
|
|
| Recommendation to Academic Centers and Clinical Institutions |
|
|
| ✥ Continue to compete for federal funding that support protected research time (i.e., T-32, CTSA) |
| ✥ Develop funding mechanisms outside of federal grant that can fund protected research time at >75% effort during the fellowship years for >2 years |
| ✥ Develop partnership with land-grant universities (e.g., tenure track professor positions) to provide funding for salary to support protected research time of faculty academic cardiologists outside of clinical revenue stream (example: Baylor Scott & White - Texas A&M University) |
| ✥ Develop partnership with philanthropic foundation to provide funding for salary to support protected research time of faculty academic cardiologists outside of clinical revenue stream (example: Vanderbilt University Medical Center Faculty Research Scholars Program) |
| ✥ Developed methods to provide credit for academic pursuits such research and teaching. The credit can be in non-monetary form such as valued components for promotion. |
ACC and Cardiovascular Professional Organizations
Professional societies provide guidance and leadership for both the profession and cardiovascular care. As illustrated by the uncertain status of early career academic cardiology, we urge the ACC and other socieities to continue evaluating the needs of the members, publishing the results, and implementing solutions. For now, restoring effective mentorship is a critical need. ACC has implemented new 1-year awards for early career members, and other societies also have provided early career support. We thank the ACC and other societies for these actions. However, as detailed earlier, 1-year duration is too short for an early career academic cardiogist to become competitive. Consequently, we urge expansion of the coverage to 2-years. Asking home institutions to provide matching funds could provide a method for expansion to 2-years. With looming budget instability at the federal level and resulting hestation of institutions in supporting non revenue generating academic infrastructure, development of new philanthropic support dedicated to fund research and patient assistance in heart disease can help alleviate signficant funding needs.
Academic Medical Centers and Clinical Institutions
Actions of these entities determine the fate of early career cardiologists and their ability to pursuit academic interests. We believe that these entities hold the key to broaden the base to support successful development of early career academic cardiologists. Besides continuing to provide core capabilities and collegiate academic enviornment, we urge development of institutional programs to provide protected research time and find equitable methods to account for the value of academic pursuits.
Current and Future Academic Cardiologists
We believe that elucidating mechanisms and developing new treatments for CVD is an important cause with a global impact. However, one needs to understand the challenges, then make a strong commitment if persuit of this career is still desired. With commitment, one needs to choose wisely where to develop based on factors that have led to success. These factors (Table 4) consist of institutional resources (funding, core capabilities), institutional commitment to academic pursuits, availability of colloborators, and effective mentoring. Table 6 provides detailed recommendations, Online Table-4 provides current institutions with active NIH T-32 grants, and the site identifies active NIH CTSA locations. Our recommendations focus on resources not on clinical setting; therefore, one needs to look beyond university based academic centers for institutions (e.g., capable private/community based healthcare systems) that can provide the resources. It is important for us to function cohesively and persevere through the ebb and flow of funding environments. We must also recognize the importance of political advocacy and the role we must play in garnering attention towards research and academic pursuits in order to improve the current status. In conclusion, we wish you success, for there is great joy in not only practicing medicine but changing the way medicine is practiced.
Table-6.
Factors for Choosing an Institution
| What to look for in a Fellowship Program | What to look for in a Cardiologist Position that can support academic pursuits |
|---|---|
|
|
CLINICAL COMPETENCIES
Identifying needs, proposing system solutions, and providing help to early career academic cardiologists addess the competencies of Professionalism, Practic-Based Learning, and System-Based Practice.
Supplementary Material
Central Illustration. Early Career Academic Cardiologist.
Personal motivation and commitment sustains drives the progress. Institutional support and mentoring help to deliver the external funding to sustain life. Successful actions provide scientific discoveries and deliver outstanding patient care.
Table-3.
Funding Sources and Barriers Among Selected International Sites
| Country | Primary Mode of Funding for Cardiovascular Research | Country-Specific Examples of Funding Streams |
|---|---|---|
| Canada | Non-Commercial | Canadian Institutes of Health Research (CIHR); Heart and Stroke Foundation of Canada |
| Germany | Non-Commercial | German Centre for Cardiovascular Research (Deutsches Zentrum für Herz-Kreislauf-Forschung, DZHK); German Research Foundation (Deutsche Forschungsgemeinschaft, DFG);German Cardiac Society (Deutsche Gesellschaft für Kardiologie – Herz- und Kreislaufforschung, DGK) |
| India | Commercial and Non-commercial | Indian council of Medical Research; Public health Foundation of India (PHFI); All India Institute of Medical Sciences (AIIMS) |
| Israel | Non-commercial | Israel Science Foundation; Israel Heart Society |
| Mexico | Non-commercial | National Council of Science and Technology; Carlos Slim Institute of Health; Mexican Education Ministry |
| Turkey | Non-commercial | Scientific and Technological Research Council of Turkey (TUBITAK) |
| United Kingdom | Commercial and Non-commercial | British Heart Foundation; Association of Medical Research Charities (AMRC); National Institute for Health Research (NIHR) |
| Barriers to Successful Academic Career: | ||
| Insufficient research infrastructure at home institution | ||
| Lack of access to cardiovascular registries and transnational research collaborations | ||
| Insufficient bridge/pilot funding at home institution | ||
| Limited research funding streams with limited research funding amounts | ||
Non-commercial: Foundations, charities, government departments, research institutes Commercial: Medical industry, for-profit companies
CONDENSED ABSTRACT.
The Early Career Section Academic Working Group of the American College of Cardiology (ACC) assessed the progress of early career academic cardiologists from 2013–2016 using reported data and a membership-wide survey. The National Heart Lung and Blood Institute significantly increased funding of career development grants. However, only a small number of early career ACC members were able to benefit while funding of the entire cohort decreased. Mentoring lost its positive correlation with obtaining grants while personal motivation, institutional support, and collaborators continued to be positive influential factors. Analyses of this challenging situation led to recommendation of attainable solutions.
Acknowledgments
Funding Sources: None
Abbreviations
- ACC
American College of Cardiology
- AHA
American Heart Association
- CVD
Cardiovascular Disease
- ECAC
Early Career Academic Cardiologist
- NHLBI
National Heart Lung and Blood Institute
- NIH
National Institutes of Health
- PI
Principal Investigator
- RVU
Relative Value Unit
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosures: Tong: NIH K08HL114877; No Industry Relationship
Madhur: NIH K08HL121671 & DP2HL137166; No Industry Relationship
Hill: NIH R01HL120732, R01HL126012, R01HL128215, T32HL125247
Mann: NIH R01HL111094, T32HL007081, U10HL110309; Consultant for Novartis – PARADISE Trial
Hira: Honoraria from Abiomed and Abbott Vascular
Raj: Canadian Institutes of Health Research (CIHR) MOP142426; Cardiac Arrhythmia Network of Canada (CANet) SRG-17-P27; Industry Consulting: GE Healthcare, Lundbeck LLC;
Research Enrollment: Medtronic Inc.
Alexanderson: None
Feldman: None
Gopinathannair: None
Leung: None
Rzeszut: None
Sivaram: None
Turner: None
Valente: None
West: None
References
- 1.Writing Group M. Mozaffarian D, Benjamin EJ, et al. Heart Disease and Stroke Statistics-2016 Update: A Report From the American Heart Association. Circulation. 2016;133:e38–360. doi: 10.1161/CIR.0000000000000350. [DOI] [PubMed] [Google Scholar]
- 2.Khavjou O, Phelps D, Leib A. Projections of Cardiovascular Disease Prevalence and Costs: 2015–2035. Technical Report. 2016 [Google Scholar]
- 3.Mensah GA, Wei GS, Sorlie PD, et al. Decline in Cardiovascular Mortality: Possible Causes and Implications. Circ Res. 2017;120:366–380. doi: 10.1161/CIRCRESAHA.116.309115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Xu J, Murphy SL, Kochanek KD, Arias E. In: Mortality in the United States, 2015. Health-and-Human-Services, editor. Hyattsville, MD: National Center for Health Statistics; 2016. pp. 1–8. [Google Scholar]
- 5.Tong CW, Ahmad T, Brittain EL, et al. Challenges facing early career academic cardiologists. J Am Coll Cardiol. 2014;63:2199–208. doi: 10.1016/j.jacc.2014.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.NIH P-SWWG. National Institute of Health Physician-Scientist Workforce Working Group Report. Advisory Committee to the Director: Physican-Scientist Workforce. 2014 doi: 10.1111/cts.12209. June 2014 ed. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Abdalla M, Kovach N, Liu C, et al. The Importance of Global Health Experiences in the Development of New Cardiologists. J Am Coll Cardiol. 2016;67:2789–97. doi: 10.1016/j.jacc.2015.10.089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.NIH, HHS. RFA-HL-16-020: Limited Competition: Small Grant Program for NHLBI K01/K08/K23 Recipients (R03) 2016 [Google Scholar]
- 9.Glickman SW, McHutchison JG, Peterson ED, et al. Ethical and scientific implications of the globalization of clinical research. N Engl J Med. 2009;360:816–23. doi: 10.1056/NEJMsb0803929. [DOI] [PubMed] [Google Scholar]
- 10.NCDR. National Cardiovascular Data Registry (NCDR) Participant Directory. American College of Cardiology; 2017. [Google Scholar]
- 11.Lindman BR, Tong CW, Carlson DE, et al. National Institutes of Health Career Development Awards for Cardiovascular Physician-Scientists: Recent Trends and Strategies for Success. J Am Coll Cardiol. 2015;66:1816–27. doi: 10.1016/j.jacc.2015.08.858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.NIH, HHS. PA-16-191: Mentored Clinical Scientist Research Development Award (Parent K08) 2016 [Google Scholar]
- 13.NIH, HHS. PA-16-198: Mentored Patient-Oriented Research Career Development Award (Parent K23) 2016 [Google Scholar]
- 14.Education ACfGM, editor. ACGME. ACGME Program Requirements for Graduate Medical Education in Cardiovascular Disease (Internal Medicine) 2016. [Google Scholar]
- 15.Carlson DE, Wang WC, Scott JD. Initial Outcomes for the NHLBI K99/R00 Pathway to Independence Program in Relation to Long-Standing Career Development Programs: Implications for Trainees, Mentors, and Institutions. Circ Res. 2016;119:904–8. doi: 10.1161/CIRCRESAHA.116.309238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.NIH. Research Portfolio Online Reporting Tools. 2017 [Google Scholar]
- 17.HHS, editor. CMS.gov. Open Payment List of Teaching Hospitals (1/1/2017–12/31/2017) Center for Medicare and Medicaid Services; 2017. [Google Scholar]
- 18.ahd.com. Hospital Statistics by State. American Hospital Directory; 2017. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


