Abstract
71-year-old woman with progressive left-sided, monocular diplopia and ptosis. Her symptoms mimicked ocular myasthenia, but she had an indirect carotid cavernous fistula (CCF). She was diagnosed with monocular myasthenia gravis (negative acetylcholinesterase antibody) after a positive ice test and started on Mestinon and underwent a thymectomy complicated by a brachial plexus injury. Months later, she developed left-sided proptosis and ocular bruit. She was urgently referred to neuro-interventional surgery and was diagnosed with an indirect high-flow left CCF, which was treated with Onyx liquid and platinum coil embolisation. Mestinon was discontinued. Her ophthalmic symptoms resolved. However, she was left with a residual left arm and hand hemiparesis and dysmetria secondary to a brachial plexus injury. Indirect CCF usually can present with subtle and progressive symptoms leading to delayed diagnosis or misdiagnosis. It is important for ophthalmologists to consider this differential in a patient with progressive ocular symptoms.
Keywords: ophthalmology, neuro-opthalmology, cranial nerves
Background
Carotid cavernous fistula (CCF) is characterised by abnormal communications between the carotid artery and the cavernous sinus.1 2 CCFs can be classified as direct and indirect, depending on whether they are supplied by the internal, external or both carotid artery branches. Both forms can cause similar characteristic ophthalmological symptoms and signs. Direct CCF are usually high flow and present with sudden-onset symptoms, whereas indirect CCFs are generally associated with low flow and milder symptoms. Some of these symptoms can include fluctuating ocular symptoms like uni-ocular diplopia and can even mimic ocular myasthenia gravis.
Case presentation
A 71-year-old woman presented to her ophthalmologist with progressive left-sided, monocular diplopia and ptosis. Her medical history included migraine, hypercholesterolaemia, haemochromatosis, retinal detachment in the right eye and cataract surgery bilaterally. On initial ophthalmological examination, the patient had an acute-onset left-sided diplopia, decreased visual acuity, followed by complete ptosis, blown pupil, with partial third and fourth nerve palsies on December 2012. She had no history of definitive trauma or history of strabismus. She also denied any difficulty chewing or swallowing food, no shortness of breath or fatigability.
A month later, she continued to have diplopia. Physical examination revealed decreased visual acuity in the left eye 20/60 (right eye 20/40), complete left eye ptosis, blown pupil and a partial third and fourth nerve palsy. Intraocular pressures were normal in both eyes. MRI brain was significant for only a possible subtle enlargement of the left cavernous sinus without enhancement. Given the progressive nature of her symptoms, an aneurysm was ruled out with a magnetic resonance angiogram (MRA) brain.
A month later, she was diagnosed with ocular myasthenia gravis by a neuro-ophthalmologist given her delayed lid closure after onset of diplopia, a positive ice test, negative acetylcholinesterase antibody and a persistent left eye partial third and fourth nerve palsy. No anisocoria was noted at that visit. She was started on a Mestinon trial and underwent excision of a thymoma in July 2013.
Five months later, she was seen by an oculoplastic surgeon. Her diplopia and ptosis improved, but by this time she had developed left eye proptosis, chemosis of left eye inferiorly with corkscrewing of conjunctival blood vessels and a positive ocular bruit (figure 1A). She was urgently referred to neuro-interventional surgery for concerns of a left-sided CCF.
Figure 1.
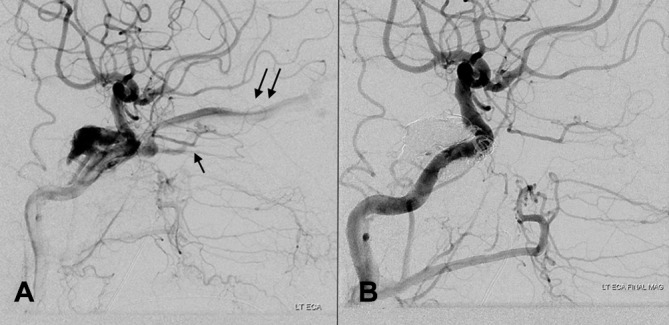
(A) Lateral angiogram showing a carotid cavernous fistula (type D). Retrograde flow into the superior (double arrow) and inferior ophthalmic veins (single arrow). (B) Lateral angiogram after coil and Onyx embolisation confirming complete occlusion of the fistula.
Investigations
A conventional cerebral angiogram confirmed an indirect high-flow left CCF (type D; supply from both ICA/ECA (external carotid artery)meningeal branches) (figure 2A,B).
Figure 2.

(A) Preoperative photograph highlighting clinical features of injection of the veins and ptosis. (B) Immediate postoperative image showing regression of dilated veins and a transient third nerve palsy.
Treatment
One year after her initial diagnosis, the patient was taken for endovascular treatment for her type D indirect CCF. Under general anaesthesia, combined transvenous and transarterial access was obtained. Using a retrograde superior ophthalmic vein approach via the left facial/angular veins, the left transverse sinus was accessed. A framework of bare platinum detachable coils was placed into the left cavernous sinus to decrease the speed of arteriovenous shunting. Using intermittent control angiograms through the left carotid artery, the left cavernous sinus was slowly injected with permanent liquid embolic material (Onyx 18, Medtronic) until both the ECA and ICA shunting was occluded (figure 1B).
Outcome and follow-up
Postoperative day 1 (figure 2B), the patient’s clinical symptoms improved and Mestinon was discontinued. Four-month and 12-month follow-up MRA examinations confirmed stable complete obliteration of the fistula. She had complete resolution of her ophthalmologic symptoms; however, she had permanent moderate left arm and hand dysmetria and hemiparesis secondary to a brachial plexus injury. At 4-year postendovascular treatment and off Mestinon, the patient has not any recurrence of her symptoms.
Discussion
CCFs can be classified based on: (1) pathogenesis: spontaneous traumatic fistulas; (2) haemodynamics: into high-flow or low-flow fistulas and (3) angiography: into direct or dural fistulas. Angiographically and anatomically, fistulas are divided into four types: type A are direct high-flow shunts between the ICA and the cavernous sinus (usually in the setting of trauma with skull base fracture), type B are dural shunts between meningeal branches of the ICA and the cavernous sinus, type C are dural shunts between meningeal branches of the external carotid artery and the cavernous sinus and type D, which are the most frequent type, are dural shunts between meningeal branches of both the internal and external carotid arteries and the cavernous sinus.1 3 Most of the direct type A CCFs are usually high-flow shunts, while indirect CCFs (types B, C and D) typically have low-flow rates. They are also called dural fistulas.3 Direct CCFs are usually associated with Dandy’s triad, a classic presentation of exophthalmos, conjunctival chemosis and ocular bruit.3
Ocular manifestations of CCF include proptosis, chemosis, orbital bruit, ptosis, vascular tortuosity, ophthalmoplegia, increased intraocular pressure/glaucoma and anterior segment ischaemia.4 Both forms can cause the similar characteristic ophthalmological symptoms and signs. Direct CCFs are usually high flow and present with acute-onset symptoms. Indirect CCFs, on the other hand, are generally associated with low flow and milder symptomatology and are hence often misdiagnosed or sometimes lead to delayed diagnosis.5 6
Some of these symptoms can include fluctuating ocular symptoms like uni-ocular diplopia and can even mimic ocular myasthenia gravis. Although ocular manifestations may be mild at initial presentation, it is important to consider an indirect CCF as a differential. Even with a thorough clinical work up, it can be missed. Our patient here was misdiagnosed with ocular myasthenia, after a positive ice test, seronegative acetylcholine antibody. It was the acute worsening of her symptoms that led to further investigation.
Neuro-imaging studies, CT, MRI and interventional radiology (IR) cerebral conventional angiography may reveal an asymmetrically enlarged superior ophthalmic vein, thick ocular muscles and evidence of an enlarged cavernous sinus with convexity of the lateral wall or asymmetric cavernous sinus (CS) widening.2 Digital subtraction angiography is the gold standard for the diagnosis and classification2 and can help determine the location, size of the fistula and venous reflux, which can help facilitate immediate treatment.7
Management is based on definitive treatment focused on reducing venous pressure along with symptomatic treatment of ocular symptoms. Barrow et al1 proposed the indication for treatment for a spontaneous CCF: (1) visual deterioration, which is contributed by combination of reduced arterial perfusion and venous hypertension with accompanying glaucoma. Intraocular pressures can increase due to venous hypertension or secondary to neovascularisation of the iris and angle of anterior segment (also known as rubeosis iridis) caused by prolonged ischaemia; (2) diplopia caused by vascular engorgement and enlargement of the extraocular muscles or by cranial nerve compression within the cavernous sinus; (3) intolerable bruit or headache and (4) ‘malignant’ proptosis with untreatable corneal exposure.
In patients with minimal symptoms and low-risk angioarchitecture, observation alone is reasonable. Endovascular treatment is considered the first-line option and includes both transarterial, transvenous approaches with a combination of n-butyl cyanoacrylate/Onyx, detachable balloons, microcoils and stents.3 In cases where transfemoral venous access fails, direct superior ophthalmic vein access can be performed. Surgical treatment is rarely performed due to incomplete occlusion and invasiveness and includes ligation of the external and/or internal carotid arteries. Although described, radiosurgery has a limited role in most cases due to high technical success of endovascular treatment.
Learning points.
Indirect carotid cavernous fistula (CCF) can present with gradual progressive ocular symptoms, whereas direct CCF usually presents with sudden-onset symptoms. It is important for ophthalmologists to consider this differential in a patient with progressive ocular symptoms like myasthenia.
This case also reflects the importance of early recognition of CCF because of the risk of irreversible vision and may help avoid unnecessary medical procedures/treatment.
CCF can be spontaneous or traumatic.
CCF can have a heterogeneous presentation that can be missed if there is not a high index of suspicion.
Footnotes
Contributors: Drafting the article: both authors. Critically revising the article: both authors. Approved the final version of the manuscript on behalf of both authors: SRS. Administrative/technical/material support: LL.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Barrow DL, Spector RH, Braun IF, et al. Classification and treatment of spontaneous carotid-cavernous sinus fistulas. J Neurosurg 1985;62:248–56. 10.3171/jns.1985.62.2.0248 [DOI] [PubMed] [Google Scholar]
- 2.Tytle TL, Punukollu PK. Carotid cavernous fistula. Seminars in Cerebrovascular Diseases and Stroke 2001;1:83–111. 10.1053/scds.2001.24080 [DOI] [Google Scholar]
- 3.Korkmazer B, Kocak B, Tureci E, et al. Endovascular treatment of carotid cavernous sinus fistula: A systematic review. World J Radiol 2013;5:143–55. 10.4329/wjr.v5.i4.143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Livi F, Ndoro S, Caird J, et al. Indirect cavernous carotid fistula in a 12-year-old girl. J Surg Case Rep 20162016;6:1–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lee KY, Kim SM, Kim DI. Isolated bilateral abducens nerve palsy due to carotid cavernous dural arteriovenous fistula. Yonsei Med J 1998;39:283–6. 10.3349/ymj.1998.39.3.283 [DOI] [PubMed] [Google Scholar]
- 6.Grumann AJ, Boivin-Faure L, Chapot R, et al. Ophthalmologic outcome of direct and indirect carotid cavernous fistulas. Int Ophthalmol 2012;32:153–9. 10.1007/s10792-012-9550-4 [DOI] [PubMed] [Google Scholar]
- 7.Halbach VV, Hieshima GB, Higashida RT, et al. Carotid cavernous fistulae: indications for urgent treatment. AJR Am J Roentgenol 1987;149:587–93. 10.2214/ajr.149.3.587 [DOI] [PubMed] [Google Scholar]


