Abstract
We report a case of a 65-year-old patient with muscle invasive bladder cancer that was treated with neoadjuvant chemotherapy, followed by radical cystoprostatectomy with pelvic lymph node dissection and orthotopic neobladder according to Hautmann. Nine years later, routine follow-up showed local recurrence in the neobladder and metastatic disease of the urothelial carcinoma in the related mesenteric lymph nodes. The entire neobladder specimen was removed including the mesentery of the neobladder. Based on the anatomical lymph drainage of the ileal neobladder, we considered the metastatic disease in the mesentery lymph node as locoregional disease spread. This case shows that such locoregional lymph node metastasis may be amenable to treatment by induction chemotherapy and radical surgery.
Keywords: urological cancer, urological surgery
Background
In male patients diagnosed with muscle invasive bladder cancer, radical cystoprostatecomy with pelvic lymph node dissection and urinary diversion is standard treatment. The type of diversion is very much dependent on the patient. One of these options is an orthotopic bladder substitution (neobladder). Well-known sites for local recurrence of urothelial cancer after cystoprostatectomy are the surgical bed and pelvic lymph nodes. Distant recurrences can be found in juxtaregional lymph nodes, lungs, liver and bones.1 Local recurrences in the neobladder have been reported.2–4 However, to our knowledge, there is only one other publication that reports a local recurrence in the neobladder with mesenteric lymph node metastases of a urothelial carcinoma.2 Herewith, we report a case of urothelial carcinoma of the bladder with an unusual pattern of recurrence and treatment.
Case presentation
In February 2004, a 65-year-old male patient was diagnosed with muscle invasive bladder cancer. He was a non-smoker and had no occupational exposure to carcinogenic aromatic amines during his life. CT revealed pathological lymph nodes in the parailiac and para-aortic regions. In March 2004, neoadjuvant chemotherapy (four cycles gemcitabine/cisplatinum/taxol) was administered, followed by cystoprostatectomy with bilateral pelvic lymph node dissection and an orthotopic neobladder according to Hautmann in June 2004. Histopathology revealed complete response after neoadjuvant chemotherapy with final stage cT4aN2M1-ypT0N0Mx urothelial carcinoma of the bladder. Follow-up consisted of routine ultrasonography, urine cytology and blood examination every 3 months for the first year and biannually thereafter. Additional abdominal CT scans, intravenous CT-U scans and cystoscopy of the neobladder were performed regularly.
Outcome and follow-up
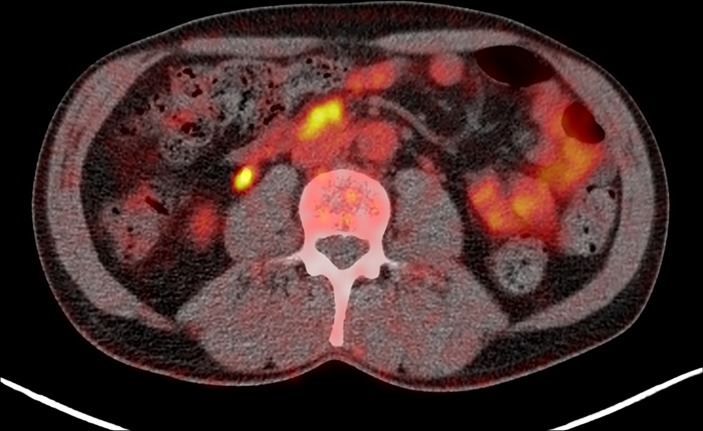
Nine years later, in January 2013, an enlarged para-aortic mesenteric lymph node was detected on a routine ultrasound. The following abdominal CT scan revealed a thickened neobladder wall at the site of the right ureteroileal anastomosis, suspicious for recurrence of urothelial carcinoma. In addition, a 18F-fluorodeoxyglucose (FDG)-PET/CT scan showed a highly suspicious pathological mesenteric lymph node (figure 1).
Figure 1.
Axial (FDG)-PET/CT reconstruction showing an enlarged FDG-positive pathological mesenteric lymph node ventral of the inferior caval vein. The hotspot on the right side is normal FDG excretion in the ureter 10 April 2013. FDG, 18F-fluorodeoxyglucose; PET, positron emission tomography.
Biopsy of the neobladder wall was performed through a transurethral resection and histopathological findings confirmed recurrence of urothelial carcinoma (grade 2–3) in the distal right ureter with infiltration of the neobladder wall. After multidisciplinary consultation, primary surgery was advised. In May 2013, the entire neobladder with its subsequent mesentery and the distal part of the right ureter were resected. Subsequently, an ileal conduit was created. Perioperatively, a suspicious lesion of the fascia of the lower right abdomen was found and resected. Pathological examination showed invasive urothelial cancer of the distal right ureter with infiltration of the neobladder wall, multiple nodal metastases in the related mesenteric lymph nodes and in the lesion on the abdominal wall.
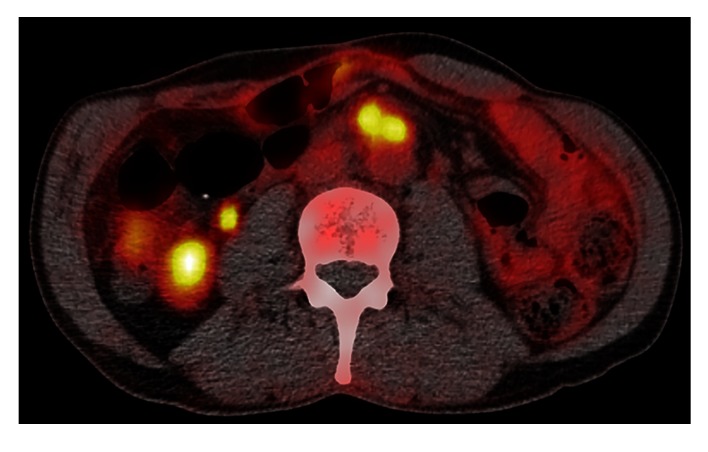
One year later (October 2014), another suspected soft tissue lesion was found at the site of the origo of the inferior mesenteric artery (figure 2).
Figure 2.
Axial (FDG)-PET/CT reconstruction showing FDG-positive lymph node ventral of the aorta at the origo of the inferior mesenteric artery 18 September 2013. FDG, 18F-fluorodeoxyglucose; PET, positron emission tomography.
Induction chemotherapy (four cycles of gemcitabine/cisplatinum) showed a good clinical response and salvage retroperitoneal lymph node dissection was performed in February 2015 revealing complete pathological response (ypN0M0). At present with a follow-up of 24 months after definitive surgery, the patient is disease free and in good health.
Discussion
Five-year survival rate of stage IV bladder cancer is 15%.5 In patients who underwent radical cystectomy for the treatment of muscle invasive bladder carcinoma, the risk of developing recurrent urothelial carcinoma depends on the stage of the initial urothelial carcinoma. Pelvic (or local) recurrence occurs in 5%–15% of patients within 6–18 months after surgery.1 Local recurrences are found in soft tissue at the surgical site and lymph nodes in the pelvic region below the aortic bifurcation.1 In addition, urethral recurrences occur in 0.5%–17.2%.2 Distant recurrence occurs in up to 50% of patients, mostly within 24 months after surgery. Common sites for distant recurrence are lymph nodes, lungs, liver and bones.1 Upper urinary tract recurrence usually occurs within a period of 3 years or longer after radical cystectomy. This includes recurrence in renal pelvis and the ureter and occurs in 1.8%–6.0% of patients following radical cystectomy for muscle invasive bladder cancer.1
Primary upper urinary tract carcinomas are uncommon. They account for 5%–10% of all urothelial carcinomas.6 Tumours of the renal pelvis are present in 58% of the cases of upper urinary tract malignancies. The ureter is affected in 35%, of which 73% are tumours of the distal ureter.7 A few case reports describe local recurrences of urothelial carcinoma in the neobladder.2–4 To our knowledge, there is only publication to report on mesenteric lymph node metastases after a urinary diversion on a patient, who developed an adenocarcinoma in an ileal conduit.2
In the present case, a tumour recurrence developed in the distal right ureter and invaded the ileal neobladder, thus initiating lymphatic spread along the related mesenteric lymph nodes.
The question arises whether the lymph node dissemination in the mesentery of the ileal neobladder should be considered as locoregional or distant lymph node metastases. Based on the anatomic lymph drainage of the ileal neobladder, we consider this to be locoregional lymph node spread. This case shows that such recurrences of urothelial cancer with locoregional lymph node metastases may be amenable to treatment by induction chemotherapy and radical surgery.
Learning points.
The pattern of disease in this case is remarkable because of the unusual lymph node metastases that were due to the invasion of the distal ureteral tumour into the ileal neobladder wall and because of long-term survivorship despite a very poor prognosis in 2004.
It is important to acknowledge the possible change in lymph drainage patterns for urothelial carcinoma invading other organs, such as the ileal urinary diversion.
Such recurrences of urothelial cancer with locoregional lymph node metastases may be amenable to treatment by induction chemotherapy and radical surgery.
Footnotes
Contributors: All persons who meet the authorship criteria are listed below as authors: identification and management of the patient of this case report: RPM. Overall guarantor: RPM. Conception and design of the work: VHG, TMTWTL, BdK, SH, RPM. Responsible for images: BdK. Drafting and revising the manuscript: VHG. Revising of the manuscript critically for important and intellectual content: TMTWTL, SH, RPM. Final approval of the version to be published: VHG, TMTWTL, BdK, SH, RPM. Authors agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved: VHG, TMTWTL, SH, RPM.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Witjes JA, Compérat E, Cowan NC, et al. EAU guidelines on muscle-invasive and metastatic bladder cancer. Limited update March 2015. [Google Scholar]
- 2.Kawamoto B, Honda M, Iwamoto H, et al. Urothelial carcinoma recurrence at an ileal orthotopic neobladder and unilateral lower ureter after surgery. Urol Case Rep 2016;9:27–9. 10.1016/j.eucr.2016.08.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hara I, Hara S, Miyake H, et al. Carcinoma in situ spread to mucosa of sigmoid colon neobladder. Urology 2003;62:145 10.1016/S0090-4295(03)00240-1 [DOI] [PubMed] [Google Scholar]
- 4.Yossepowitch O, Dalbagni G, Golijanin D, et al. Orthotopic urinary diversion after cystectomy for bladder cancer: implications for cancer control and patterns of disease recurrence. J Urol 2003;169:177–81. 10.1016/S0022-5347(05)64062-1 [DOI] [PubMed] [Google Scholar]
- 5.Survival rates for bladder cancer [Internet]. American Cancer Society 2016. (cited 7 Dec 2016). [Google Scholar]
- 6.Rouprêt M, Babjuk M, Bohle A, et al. EAU Guidelines on urothelial carcinomas of the upper urinary tract. Limited update March 2015. [Google Scholar]
- 7.Colin P, Koenig P, Ouzzane A, et al. Environmental factors involved in carcinogenesis of urothelial cell carcinomas of the upper urinary tract. BJU Int 2009;104:1436–40. 10.1111/j.1464-410X.2009.08838.x [DOI] [PubMed] [Google Scholar]