Abstract
Objective
To examine the prevalence and trends in overweight and obesity among non-pregnant urban women in Africa over the past two and a half decades.
Design
Cross-sectional surveys conducted between 1991 and 2014.
Settings
Demographic and Health Surveys (DHS), repeated cross-sectional data collected in 24 African countries.
Participants
Adult non-pregnant women aged 15–49 years. The earlier DHS collected anthropometric data on only those women who had children aged 0–5 years. The main analyses were limited to this subgroup. The participants were classified as overweight (25.0–29.9 kg/m2) and obese (≥30.0 kg/m2).
Results
The prevalence of overweight and obesity among women increased in all the 24 countries. Trends were statistically significant in 17 of the 24 countries in the case of obesity and 13 of the 24 for overweight. In Ghana, overweight almost doubled (p=0.001) while obesity tripled (p=0.001) between 1993 and 2014. Egypt has the highest levels of overweight and obesity at 44% (95% CI 42%, 46.5%) and 39% (95% CI 36.6%, 41.8%), respectively, in 2014 and the trend showed significant increase (p=0.005) from 1995 levels. Also, obesity doubled in Kenya, Benin, Niger, Rwanda, Ivory Coast and Uganda, while tripled in Zambia, Burkina Faso, Mali, Malawi and Tanzania. Ethiopia and Madagascar had the lowest prevalence of both obesity and overweight, with overweight ranging from 7% to 12% and obesity from 1% to 4%.
Conclusions
Overweight and obesity are increasing among women of reproductive age in urban Africa, with obesity among this age group having more than doubled or tripled in 12 of the 24 countries. There is an urgent need for deliberate policies and interventions to encourage active lifestyles and healthy eating behaviour to curb this trend in urban Africa.
Keywords: Overweight, Obesity, Africa, Prevalence, Trends, Urban
Strengths and limitations of this study.
Use of nationally representative data sets, thereby enhancing the generalisability of the findings.
Height and weight used in the calculation of body mass index was objectively measured, possibly reducing misclassification.
Analysis limited to women with children under 5 years of age and may affect the generalisability of the findings to all women.
Lack of uniformity in the definition of urban and rural settings across countries.
Introduction
Overweight and obesity are global public health problems, especially among women in urban settings.1 2 Worldwide, it is estimated that 2.8 million people die each year as a result of being overweight or obese, and that 35.8 million of global disability-adjusted life years (DALYs) are caused by overweight and obesity.3 There is also evidence that the risks of coronary heart disease, ischaemic stroke and type 2 diabetes mellitus increase steadily with increasing body mass index (BMI), a measure of weight relative to height.3 4 Furthermore, high BMI is found to elevate the risk of breast, colon, prostate, endometrium, kidney and gall bladder cancers.3 A recent study showed that overweight and obesity are linked to 13 different cancers.5
The consequences of overweight and obesity on women of reproductive age are more serious, especially during pregnancy. Studies have shown that maternal obesity can result in negative outcomes in both mothers and fetuses, including gestational diabetes, pre-eclampsia, an increased miscarriage rate,6 7 stillbirth and congenital anomalies. Obesity in pregnancy can also affect health later in life for both mother and child, including increased risk of heart disease, hypertension and diabetes.6 Children also have a risk of future obesity. Overweight and obesity are associated with decreased contraceptive efficacy and ovulatory disorders in women of reproductive age,7 and increasing maternal BMI exerts a progressive adverse effect on vaginal delivery rates for both primigravid and multigravid women.8 Obese mothers were more likely than other mothers to terminate breast feeding when the infant showed satiation cues.9 Obese mothers with higher BMI were also reported using more restrictive feeding practices, limiting the quantity and quality of foods provided to their toddlers, and were observed to use more pressure in getting their children to eat during mealtimes.10 11 Together, these findings show the varied effects of overweight and obesity on women of reproductive age and their children.
The literature demonstrates that the magnitude of the effect of BMI on health is largely linked to the level of BMI. For instance, there is an increased risk of comorbidities for individuals with a BMI of 25.0 to 29.9 kg/m2 (defined as overweight), and moderate to severe risk of comorbidities for individuals with a BMI greater than 30 kg/m2 (defined as obesity).3 6 WHO3 6 recommends that for optimum health, the median BMI for an adult population should be in the range of 21 to 23 kg/m2, while the goal for individuals should be to maintain BMI in the range of 18.5 to 24.9 kg/m2. This is often difficult to achieve as evidence shows that global overweight and obesity trends are on the rise, with the developing world now bearing the brunt of the surge.7 This dynamic calls for more studies to systematically document these trends over time, especially in developing country contexts.
Hitherto, overweight and obesity were not public health issues on the African continent. However, rapid changes have been observed, and many countries in Africa are currently confronted with overweight and obesity, particularly among women, coupled with a resulting increase in the prevalence of non-communicable diseases (NCDs).4 12 13 In Africa, women had approximately double the obesity prevalence of men,3 with urban settings being the most affected. Thus, the burden of overweight and obesity among urban women is increasing at an alarming rate in developing countries, and particularly in Africa for that matter.1 14 In Ghana, for example, systematic review and meta-analysis revealed that overweight among urban women was 11 percentage points higher than rural women, while obesity was two times higher in urban relative to rural women.15 Similar trends were obtained using data from 42 countries in Asia, the Middle East, Africa (East, West, Central and Southern) and Latin America, with a combined overweight/obesity prevalence of 37.2% among urban women compared with 19% of rural women.16 The study however noted regional differences, with rural women in Latin America, the Middle East and North Africa having much higher increases in the prevalence of overweight/obesity compared with their urban counterparts. Conversely, in different multicountry analysis, overweight was increasing more quickly in urban areas than in rural areas of lower-income countries such as Bangladesh and Uganda, but increasing more quickly in rural areas compared with urban areas of upper-middle-income countries, such as Jordan and Peru.17
The trend observed above may be attributable to an increased intake of energy-dense foods that are high in fat; and an increase in physical inactivity due to the increasing sedentary nature of many occupations, increased use of motorised transportation and urbanisation.1 18 19 Increasingly, sedentary lifestyles and high consumption of energy-dense diets account for the increasing burden of overweight and obesity in urban settings of low-income and middle-income countries (LMICs).20–22 Various other studies have argued that the association between urban residence and obesity in LMICs is driven largely by higher individual-level and community-level socioeconomic status (SES) in urban areas, suggesting that urban residence alone may not cause increased body weight in developing countries. However, recent studies suggest that the distribution of overweight by SES is changing in developing countries.4 23 24 For example, lower SES populations in some of these countries now have higher prevalence of overweight, mimicking long-standing associations between low SES and poorer health in LMICs.4 23–25 This changing trend is particularly widespread among the urban population. A study in urban poor settlements in Nairobi, Kenya confirmed high levels of overweight and obesity among women.26 Another study using data from seven African countries showed that the increase in overweight and obesity was higher among the poorest urban dwellers compared with the richest population subgroup.20
Despite the emerging and worrying trend of increased overweight and obesity, and recognition of the potential rise in chronic diseases in recent times in Africa, little effort has been made in addressing overweight and obesity in the continent.27 Consequently, an analysis of overweight and obesity in this study across several countries in the region is a critical step in the provision of insights into the extent of the problem over time, especially in urban settings, which is needed to inform policy and programme interventions to address the challenge in urban Africa.
It is worth noting that while there are a number of studies that investigated overweight and obesity in Africa; most either focused on one country,13 lumped urban and rural data together in their analyses,2 13 analysed overweight and obesity together25 or used one data point.28 These attempts may mask the seriousness of the problem in urban settings and the important differences in the trends and prevalence of overweight and obesity over time. Also, the presentation of the results in some of these studies makes it difficult for policy-makers to appreciate the extent of the problem. The present study elucidates the prevalence and time trends in overweight and obesity separately, and presents the results in a way that makes it easier for policy-makers to understand the extent of the problem in urban settings.
Methods
Data sources and participants
The study used data from the Demographic and Health Surveys (DHS) Program. These are nationally representative, repeated cross-sectional household surveys collected primarily in LMICs approximately every 5 years and standardised to enable cross-country comparisons.29 30 We restricted our analysis to data collected in 24 sub-Saharan African countries between 1991 and 2014 and containing individual anthropometric data. There were a total of 137 survey cycles in the 24 countries, and the number of survey cycles per country ranged between three (11/137), four (8/137) and five (5/137) in the time period under consideration. These countries were selected solely based on the number of data points (at least three) and the availability of anthropometric data. Data from a total of 29 countries that met the minimum requirement in terms of data points were downloaded. The second stage was to examine the data for the availability of anthropometric data. All data sets missing anthropometric data were excluded in the analysis. For example, the very first DHS, conducted between 1987 and 1990, did not collect maternal anthropometric data. Hence, the data set for this period was excluded in the analysis. Second, countries with three data sets, but reduced to two data points due to one of the data sets not having anthropometric data, were also excluded in the analysis.
The DHS employs a multistage sampling design. The first stage involves selecting sample points or clusters from an updated master sampling frame constructed from the National Population and Housing Census data of the respective countries. The clusters are then selected using systematic sampling with probability proportional to size. A household listing operation is then conducted in all the selected clusters to provide a sampling frame for the second-stage selection of households. The second stage of selection involves the systematic sampling of households listed in each cluster. The primary objective of the second stage of selection is to ensure adequate numbers of completed individual interviews to provide estimates for key indicators with acceptable precision.30 We limited our analyses to adult non-pregnant women of reproductive age, 15–49 years in all countries. This is because pregnant women naturally gain weight during the cause of their pregnancy, including them in the analysis may present a misleading picture about the issue of overweight and obesity among women. Since the earlier DHS collected anthropometry data on only those women who had children aged 0–5 years,25 31 we further restricted our main analyses to this subgroup. For the total of 224 940 urban women who met eligibility criteria, anthropometric data were available for 191 836 (85.3%).
Ethics statement
The DHS obtained ethical clearance from the ethical committees of the respective countries before the surveys were conducted. Written informed consent was obtained from the women before participation. The authors of this paper sought and obtained permission from the DHS Program for the use of the data. The data were completely anonymised and therefore the authors did not seek further ethical clearance before their use.
Variables
Height and weight were measured objectively by trained field technicians using standard techniques.30 Weight measurements were taken using electronic Seca scales with a digital screen. Height measurements were taken using a measuring board produced by Shorr Productions. Height and weight measurements were then used to estimate the study participants’ BMI. BMI, also referred to as Quetelet’s Index,32 was derived by dividing weight in kilograms by the squared height in metres. Based on the BMI (kg/m2) estimates and according to WHO guidelines,33 the participants were classified as overweight (25.0–29.9 kg/m2) and obese (≥30.0 kg/m2). Trends and prevalence of overweight and obesity were estimated for each country. Place of residence was designated as rural and urban according to country-specific definitions; however, the present analyses were restricted to the urban sample only. This is based on the evidence that the bane of overweight and obesity in Africa is more prevalent in the urban settings relative to other settings.18 20
Analytical strategy
We used STATA V.13 to perform the data analyses. A data file was constructed by using place of residence, country, survey year and sample size. The analyses were conducted in three key steps. Initially, prevalence of overweight and obesity in selected countries in Africa with at least three DHS data points was graphed. In this step, only point estimates were reported. We then computed, at 95% CIs, the outcomes of interest by year of survey for each country in the second step. Because CIs are affected by the sampling design, we took into account the complex survey design (CSD) of DHS within the svyset and svy procedures in STATA. In STATA, this is achieved with the ‘subpop’ in svy procedures. In the third step, we examined statistical significance of the trends of overweight and obesity. To achieve this, we performed a multinomial logistic regression with time (year of survey) as the key independent variable using BMI <25 kg/m2 category as the base outcome and taking into account the CSD. While in Steps 1 and 2 the time point data sets were treated independently, we pooled the data sets for trend analyses. To account for sampling weight, the weight in the pooled data was divided by the number of surveys available for the respective countries.
Results
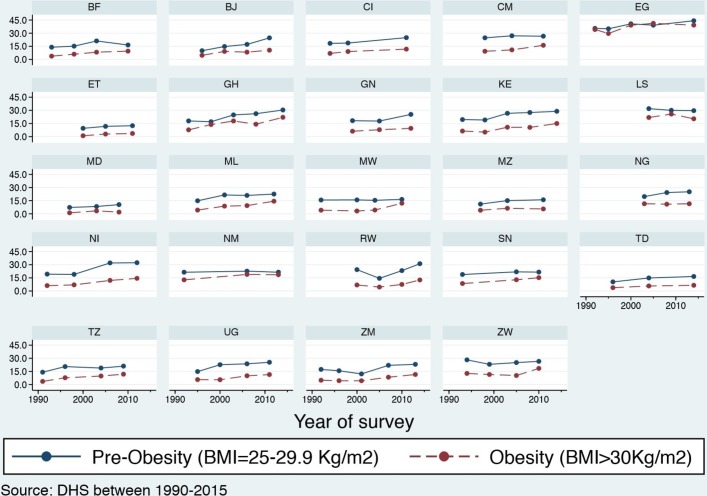
Table 1 presents results of the samples in the selected countries. Both table 2 and table 3 present the results of prevalence and trend analyses. Whereas table 2 presents results for countries with four or more data points, table 3 presents results of countries with three data points. The rationale for dividing the results into two separate tables is to ease interpretation of the results for the reader. Figure 1 displays the results for all the 24 countries included in the study.
Table 1.
Results of samples used in the analysis
| Country | Total | |||||
| Ghana | 1993 | 1998 | 2003 | 2008 | 2014 | |
| Samples | 583 | 656 | 966 | 2023 | 2130 | 6358 |
| Egypt | 1992 | 1995 | 2000 | 2005 | 2014 | |
| Samples | 3090 | 3779 | 4279 | 4595 | 5842 | 21 555 |
| Kenya | 1993 | 1998 | 2003 | 2008 | 2014 | |
| Samples | 623 | 500 | 1398 | 1342 | 6369 | 10 232 |
| Zambia | 1992 | 1996 | 2001 | 2007 | 2013 | |
| Samples | 2329 | 2099 | 1591 | 1867 | 4636 | 12 522 |
| Burkina Faso | 1993 | 1998 | 2003 | 2010 | – | |
| Samples | 1774 | 873 | 3136 | 3006 | – | 8789 |
| Benin | 1996 | 2001 | 2006 | 2011 | – | |
| Samples | 702 | 1403 | 5097 | 4480 | – | 11 682 |
| Mali | 1995 | 2001 | 2006 | 2011 | – | |
| Samples | 1630 | 2395 | 3673 | 2323 | – | 10 021 |
| Malawi | 1992 | 2000 | 2004 | 2010 | – | |
| Samples | 999 | 1864 | 1022 | 1801 | – | 5686 |
| Niger | 1992 | 1998 | 2006 | 2012 | – | |
| Samples | 2253 | 1069 | 2267 | 2453 | – | 8042 |
| Rwanda | 2000 | 2005 | 2010 | 2014 | – | |
| Samples | 1528 | 1524 | 1112 | 1604 | – | 5768 |
| Tanzania | 1991 | 1996 | 2004 | 2009 | – | |
| Samples | 1128 | 1247 | 1336 | 1404 | – | 5115 |
| Uganda | 1995 | 2000 | 2006 | 2011 | – | |
| Samples | 1462 | 1510 | 826 | 1539 | – | 4593 |
| Zimbabwe | 1994 | 1999 | 2005 | 2010 | – | |
| Samples | 508 | 1685 | 1298 | 1500 | – | 4991 |
| Senegal | 1993 | 2005 | 2010 | – | – | |
| Samples | 1683 | 3180 | 3373 | – | – | 8236 |
| Ivory Coast | 1994 | 1998 | 2011 | – | – | |
| Samples | 1470 | 1040 | 2344 | – | – | 4854 |
| Cameroon | 1998 | 2004 | 2011 | – | – | |
| Samples | 838 | 2819 | 4161 | – | – | 7818 |
| Ethiopia | 2000 | 2005 | 2011 | – | – | |
| Samples | 1550 | 1299 | 1817 | – | – | 4666 |
| Guinea | 1999 | 2005 | 2012 | – | – | |
| Samples | 1415 | 1263 | 1818 | – | – | 4496 |
| Lesotho | 2004 | 2009 | 2014 | – | – | |
| Samples | 640 | 648 | 761 | – | – | 2049 |
| Madagascar | 1997 | 2003 | 2008 | – | – | |
| Samples | 722 | 2708 | 2079 | – | – | 5509 |
| Mozambique | 1997 | 2003 | 2011 | – | – | |
| Samples | 949 | 3320 | 3308 | – | – | 7577 |
| Nigeria | 2003 | 2008 | 2013 | – | – | |
| Samples | 1831 | 6659 | 8976 | – | – | 17 466 |
| Namibia | 1992 | 2006 | 2013 | – | – | |
| Samples | 1090 | 1854 | 2142 | – | – | 5086 |
| Chad | 1996 | 2004 | 2014 | – | – | |
| Samples | 2443 | 2112 | 3396 | – | – | 7951 |
| Total sample | 191 836 |
Table 2.
Analysis of trends in overweight and obesity for countries with four or more data points
| Country | p Value | Nature of trend | |||||
| Ghana | 1993 | 1998 | 2003 | 2008 | 2014 | ||
| Overweight | |||||||
| (%) | 17.9 | 17.0 | 24.8 | 26.2 | 30.4 | <0.05 | ↗ |
| (95% CI) | 17.9, 18.2 | 13.6, 21.1 | 21.3, 28.7 | 24.2, 28.3 | 26.3, 34.9 | ||
| Obesity | |||||||
| (%) | 7.7 | 13.8 | 17.9 | 14.2 | 22.0 | <0.05 | ↗ |
| (95% CI) | 7.0, 8.5 | 10.6, 17.8 | 14.7, 21.5 | 12.7, 15.8 | 18.3, 26.3 | ||
| Egypt | 1995 | 2000 | 2005 | 2008 | 2014 | ||
| Overweight | |||||||
| (%) | 35.5 | 35.0 | 40.6 | 39.1 | 44.2 | <0.05 | ↗ |
| (95% CI) | 32.9, 38.2 | 32.7, 37.3 | 38.2, 43.2 | 36.7, 41.6 | 42.0, 46.5 | ||
| Obesity | |||||||
| (%) | 34.2 | 29.6 | 39.1 | 41.2 | 39.2 | <0.05 | ↗ |
| (95% CI) | 31.0, 37.6 | 26.7, 32.7 | 36.4, 42.0 | 38.6, 43.9 | 36.6, 41.8 | ||
| Kenya | 1993 | 1998 | 2003 | 2008 | 2014 | ||
| Overweight | |||||||
| (%) | 19.5 | 19.0 | 26.6 | 27.5 | 28.9 | <0.05 | ↗ |
| (95% CI) | 15.0, 24.9 | 15.4, 23.3 | 23.3, 30.3 | 22.8, 32.9 | 26.1, 31.9 | ||
| Obesity | |||||||
| (%) | 6.4 | 5.1 | 10.7 | 10.5 | 15.0 | <0.05 | ↗ |
| (95% CI) | 4.1, 9.8 | 3.3, 7.9 | 8.1, 14.1 | 7.7, 14.3 | 12.7, 17.6 | ||
| Zambia | 1992 | 1996 | 2001 | 2007 | 2013 | ||
| Overweight | |||||||
| (%) | 17.3 | 15.7 | 12.1 | 22.0 | 23.1 | <0.05 | ↗ |
| (95% CI) | 15.2, 19.6 | 13.8, 17.9 | 10.3, 14.2 | 18.9, 25.4 | 21.2, 25.2 | ||
| Obesity | |||||||
| (%) | 4.9 | 4.4 | 4.3 | 8.4 | 11.5 | <0.05 | ↗ |
| (95% CI) | 3.8, 6.4 | 3.4, 5.7 | 3.2, 5.9 | 6.6, 10.5 | 9.8, 13.5 | ||
| Burkina Faso | 1993 | 1998 | 2003 | 2010 | – | ||
| Overweight | – | ||||||
| (%) | 14.0 | 15.2 | 21.1 | 16.5 | – | >0.05 | → |
| (95% CI) | 12.0, 16.3 | 12.2, 18.7 | 18.2, 24.3 | 13.8, 19.5 | – | ||
| Obesity | – | ||||||
| (%) | 3.8 | 6.0 | 8.3 | 9.5 | – | <0.05 | ↗ |
| (95% CI) | 2.7, 5.2 | 4.3, 8.4 | 5.7, 11.8 | 7.2, 12.3 | – | ||
| Benin | 1996 | 2001 | 2006 | 2011 | – | ||
| Overweight | – | ||||||
| (%) | 9.9 | 14.8 | 17.2 | 24.6 | – | <0.05 | ↗ |
| (95% CI) | 7.3, 13.4 | 12.3, 17.6 | 15.5, 18.9 | 22.7, 26.7 | – | ||
| Obesity | – | ||||||
| (%) | 4.7 | 9.1 | 8.3 | 10.5 | – | <0.05 | ↗ |
| (95% CI) | 3.1, 7.0 | 7.4, 11.3 | 7.1, 9.7 | 8.9, 12.4 | – | ||
| Mali | 1995 | 2001 | 2006 | 2011 | – | ||
| Overweight | – | ||||||
| (%) | 14.9 | 21.6 | 21.0 | 22.5 | – | <0.05 | ↗ |
| (95% CI) | 12.6, 17.4 | 18.4, 25.1 | 18.3, 23.9 | 19.1, 26.4 | – | ||
| Obesity | – | ||||||
| (%) | 4.3 | 8.8 | 9.4 | 14.4 | – | <0.05 | ↗ |
| (95% CI) | 3.1, 5.8 | 6.9, 11.1 | 7.7, 11.4 | 11.7, 17.5 | – | ||
| Malawi | 1992 | 2000 | 2004 | 2010 | – | ||
| Overweight | – | ||||||
| (%) | 15.8 | 15.9 | 15.4 | 16.4 | – | >0.05 | → |
| (95% CI) | 12.3, 20.0 | 13.1, 19.1 | 12.1, 19.5 | 12.7, 21.1 | – | ||
| Obesity | – | ||||||
| (%) | 4.1 | 3.2 | 4.3 | 12.1 | – | <0.05 | ↗ |
| (95% CI) | 2.6, 6.4 | 2.0, 5.1 | 2.8, 6.7 | 8.2, 17.5 | – | ||
| Niger | 1992 | 1998 | 2006 | 2012 | – | ||
| Overweight | – | ||||||
| (%) | 19.2 | 19.0 | 32.0 | 32.23 | – | <0.05 | ↗ |
| (95% CI) | 16.8, 22.0 | 15.5, 23.0 | 27.8, 36.6 | 28.5, 36.3 | – | ||
| Obesity | – | ||||||
| (%) | 6.1 | 7.0 | 12.1 | 14.4 | – | <0.05 | ↗ |
| (95% CI) | 4.9, 7.6 | 5.2, 9.3 | 9.4, 15.4 | 11.7, 17.6 | – | ||
| Rwanda | 2000 | 2005 | 2010 | 2014 | – | ||
| Overweight | – | ||||||
| (%) | 24.4 | 14.4 | 23.3 | 31.1 | – | <0.05 | ↗ |
| (95% CI) | 23.1,25.6 | 11.0, 18.8 | 19.4, 27.6 | 26.5, 36.1 | – | ||
| Obesity | – | ||||||
| (%) | 6.8 | 4.5 | 7.5 | 12.6 | – | <0.05 | ↗ |
| (95% CI) | 6.1,7.3 | 2.6, 7.8 | 4.9, 11.4 | 10.0, 15.7 | – | ||
| Tanzania | 1991 | 1996 | 2004 | 2009 | – | ||
| Overweight | – | ||||||
| (%) | 14.1 | 20.5 | 18.9 | 21.0 | – | <0.05 | ↗ |
| (95% CI) | 11.1, 17.8 | 20.1, 20.9 | 18.5, 19.3 | 20.4, 22.2 | – | ||
| Obesity | – | ||||||
| (%) | 3.6 | 7.8 | 9.7 | 11.8 | – | <0.05 | ↗ |
| (95% CI) | 2.4, 5.3 | 7.2, 7.9 | 9.4, 10.1 | 11.1, 12.1 | – | ||
| Uganda | 1995 | 2000 | 2006 | 2011 | – | ||
| Overweight | – | ||||||
| (%) | 14.1 | 22.7 | 23.7 | 25.4 | – | <0.05 | ↗ |
| (95% CI) | 11.1, 17.8 | 18.9, 26.9 | 16.9, 32.2 | 20.0, 31.7 | – | ||
| Obesity | – | ||||||
| (%) | 5.6 | 5.5 | 10.0 | 11.4 | – | <0.05 | ↗ |
| (95% CI) | 4.2, 7.6 | 4.0, 7.6 | 5.2, 18.3 | 7.8, 16.4 | – | ||
| Zimbabwe | 1994 | 1999 | 2005 | 2010 | – | ||
| Overweight | – | ||||||
| (%) | 28.2 | 23.1 | 25.1 | 26.5 | – | >0.05 | → |
| (95% CI) | 23.3, 33.7 | 21.0, 25.4 | 22.0, 28.5 | 23.5, 29.7 | – | ||
| Obesity | – | ||||||
| (%) | 12.7 | 11.5 | 10.3 | 18.5 | – | >0.05 | ↗ |
| (95% CI) | 9.6, 16.7 | 10.0, 13.2 | 8.6, 12.4 | 15.5, 21.9 | – |
p denotes significance level.
↗, increasing; ↘, decreasing; →, stable.
Table 3.
Analysis of trends in overweight and obesity for countries with three data points
| Country | p Value | Nature of trend | |||
| Senegal | 1993 | 2005 | 2010 | ||
| Overweight | |||||
| (%) | 18.8 | 21.9 | 21.6 | >0.05 | → |
| (95% CI) | 16.3, 21.6 | 17.0, 27.6 | 18.2, 25.4 | ||
| Obesity | |||||
| (%) | 8.5 | 12.8 | 15.2 | <0.05 | ↗ |
| (95% CI) | 6.7, 10.8 | 9.5, 17.1 | 11.9, 19.3 | ||
| Ivory Coast | 1994 | 1998 | 2011 | ||
| Overweight | |||||
| (%) | 18.4 | 18.8 | 24.9 | >0.05 | → |
| (95% CI) | 16.1, 20.8 | 16.1, 21.7 | 21.4, 28.8 | ||
| Obesity | |||||
| (%) | 6.9 | 9.0 | 11.8 | >0.05 | → |
| (95% CI) | 5.1, 9.2 | 7.1, 11.4 | 9.1, 15.1 | ||
| Cameroon | 1998 | 2004 | 2011 | ||
| Overweight | |||||
| (%) | 24.7 | 27.0 | 26.7 | >0.05 | → |
| (95% CI) | 21.3, 28.3 | 23.8, 30.5 | 23.9, 29.3 | ||
| Obesity | |||||
| (%) | 9.3 | 10.9 | 16.1 | >0.05 | ↗ |
| (95% CI) | 6.7, 12.8 | 8.9, 13.4 | 14.1, 18.4 | ||
| Ethiopia | 2000 | 2005 | 2011 | ||
| Overweight | |||||
| (%) | 9.5 | 11.7 | 12.5 | >0.05 | → |
| (95% CI) | 6.9, 12.9 | 7.5, 18.0 | 9.2, 16.8 | ||
| Obesity | |||||
| (%) | 1.0 | 2.9 | 3.6 | <0.05 | ↗ |
| (95% CI) | 0.5, 1.7 | 1.5, 5.8 | 2.3, 5.4 | ||
| Guinea | 1999 | 2005 | 2012 | ||
| Overweight | |||||
| (%) | 18.2 | 17.8 | 25.4 | <0.05 | ↗ |
| (95% CI) | 15.7, 21.0 | 14.3, 22.0 | 20.9, 30.4 | ||
| Obesity | |||||
| (%) | 6.2 | 7.9 | 9.4 | <0.05 | ↗ |
| (95% CI) | 4.8, 7.9 | 4.6, 13.3 | 6.9, 12.8 | ||
| Lesotho | 2004 | 2009 | 2014 | ||
| Overweight | |||||
| (%) | 32.0 | 30.0 | 29.7 | >0.05 | → |
| (95% CI) | 25.3, 39.5 | 23.3, 37.7 | 22.9, 37.4 | ||
| Obesity | |||||
| (%) | 21.9 | 25.8 | 20.3 | >0.05 | → |
| (95% CI) | 15.5, 30.0 | 20.1, 32.4 | 14.7, 27.4 | ||
| Madagascar | 1997 | 2003 | 2008 | ||
| Overweight | |||||
| (%) | 7.3 | 8.3 | 10.5 | >0.05 | → |
| (95% CI) | 5.2, 10.1 | 6.6, 10.5 | 8.1, 13.5 | ||
| Obesity | |||||
| (%) | 1.1 | 3.4 | 1.9 | >0.05 | → |
| (95% CI) | 0.5, 2.6 | 2.4, 4.8 | 1.0, 3.5 | ||
| Mozambique | 1997 | 2003 | 2011 | ||
| Overweight | |||||
| (%) | 11.1 | 15.1 | 16.0 | <0.05 | ↗ |
| (95% CI) | 8.4, 14.6 | 13.1, 19.1 | 14.1, 18.2 | ||
| Obesity | |||||
| (%) | 4.0 | 3.2 | 6.3 | >0.05 | → |
| (95% CI) | 2.3, 6.9 | 2.0, 5.1 | 4.7, 8.6 | ||
| Nigeria | 2003 | 2008 | 2013 | ||
| Overweight | |||||
| (%) | 19.7 | 24.3 | 25.2 | >0.05 | → |
| (95% CI) | 15.2, 25.1 | 22.6, 26.1 | 23.4, 27.1 | ||
| Obesity | |||||
| (%) | 11.5 | 11.0 | 11.5 | >0.05 | → |
| (95% CI) | 8.3, 15.6 | 9.7, 12.5 | 10.3, 12.7 | ||
| Namibia | 1992 | 2006 | 2013 | ||
| Overweight | |||||
| (%) | 21.4 | 22.6 | 21.5 | >0.05 | → |
| (95% CI) | 17.9, 25.4 | 19.2, 26.5 | 18.0, 25.4 | ||
| Obesity | |||||
| (%) | 12.7 | 18.9 | 18.6 | <0.05 | ↗ |
| (95% CI) | 10.3, 15.6 | 16.1, 22.1 | 15.2, 22.5 | ||
| Chad | 1996 | 2004 | 2014 | ||
| Overweight | |||||
| (%) | 10.4 | 14.9 | 16.6 | <0.05 | ↗ |
| (95% CI) | 9.6,11.4 | 12.4, 17.7 | 13.9, 19.6 | ||
| Obesity | |||||
| (%) | 3.8 | 5.7 | 6.5 | <0.05 | ↗ |
| (95% CI) | 2.9,4.1 | 3.9, 8.4 | 4.8, 8.7 |
p denotes significance level.
↗, increasing; ↘, decreasing; →, stable.
Figure 1.
Time trends of overweight and obesity. BF, Burkina Faso; BJ, Benin; BMI, body mass index; CI, Ivory Coast; CM, Cameroon; DHS, Demographic and Health Surveys; EG, Egypt; ET, Ethiopia; GH, Ghana; GN, Guinea; KE, Kenya; LS, Lesotho; MD, Madagascar; ML, Mali; MW, Malawi; MZ, Mozambique; NG, Nigeria; NI, Niger; NM, Namibia; RW, Rwanda; SN, Senegal; TD, Chad; TZ, Tanzania; UG, Uganda; ZM, Zambia; ZW, Zimbabwe.
Table 2 provides period estimates and trends in overweight and obesity in 13 countries with four or more data points. These surveys cover periods between 14 years in Rwanda and 21 years in Ghana, Kenya and Zambia. The earliest data points in these countries were in the 1990s and the latest are after 2010. Across all 13 countries, levels of overweight reached or exceeded 20% only in Egypt (36%) and Zimbabwe (28%) in the 1990s surveys. Obesity reached a double digit of 10% or more only in Egypt (34%) and Zimbabwe (13%). In all the other countries, overweight was under 20% and obesity was under 10%. In the latest surveys conducted since 2010 in these countries, overweight exceeded 20% in all countries except Burkina Faso and Malawi where the prevalence was around 16%. The increase over time was not also statistically significant in these two countries. In four countries, the prevalence of overweight exceeded 30% (Egypt (44%), Niger (32%), Rwanda (31%) and Ghana (30%)). Obesity exceeded 10% in all countries in the 2010s surveys with Egypt (39%) and Ghana (22%) leading in levels of obesity. Only in Burkina Faso was obesity still below 10% in the most recent survey.
Table 3 shows the results for the 11 countries with only three data points. The periods covered by these surveys range from 10 years in Lesotho and Nigeria to 17 years in Senegal and Ivory Coast. Some of the earliest surveys in these countries occurred in the 2000s and given differences in timing and duration between the earliest and latest surveys, it made sense to report these surveys separately. Lesotho has the highest prevalence of overweight, which stood at 32% in 2004 and has barely changed over the subsequent 10-year period. Namibia and Cameroon also had high levels of overweight at more than 20%. On the other hand, Madagascar and Ethiopia had the lowest levels of overweight and obesity. In Madagascar and Ethiopia, overweight is varied between 7% and 12% over the period covered by the surveys, while obesity is under 5% (under 2% in Madagascar). The change of overweight over time was statistically significant only in Guinea, Mozambique, Namibia and Chad, while obesity was significant only in Senegal, Guinea and Cameroon.
Figure 1 depicts the increasing trends of overweight and obesity in all the 24 countries included in the analysis, except in Lesotho where there is semblance of a decrease.
Discussion
We set out to investigate the prevalence and time trends in overweight and obesity between 1991 and 2014 in 24 African countries. Primarily, we confirm that the prevalence of overweight and obesity among urban women has rapidly increased in the past two and a half decades. All 24 countries included in our analyses experienced an increase in overweight and obesity over the time period under consideration. However, the increase was only statistically significant in 17 of the 24 countries in the case of obesity and 13 out of the 24 for overweight. The changes over time were particularly noticeable among countries with four or more survey data points, in which case, all the 13 countries showed a statistically significant increase in obesity, while 10 showed significant increase for overweight during the period of the study. For countries with three data points, only 4 of the 11 countries had a significant increase for overweight and 3 for obesity. This suggests that length of time (number of data points) plays a role in understanding the changes in overweight and obesity over time. We also found that 18 of the 24 countries had an overweight prevalence above 20%, based on the most recent survey waves for the respective countries. This was not the case in the earlier surveys where only six countries had an overweight prevalence of 20% or above. Four countries of the 24 had an obesity prevalence that was above 20%, with the prevalence in the rest ranging between 10% and 19% based on the latest surveys. However, in the earlier surveys, only one country had obesity prevalence of 20% or more, while the rest had obesity rate ranging from 1% to 12%. This points to worsening phenomenon of obesity among urban women in the past two and a half decades. Another key finding is that in most of the countries included in our analyses, obesity increased alongside overweight. This is not unexpected, as women who are overweight (also known as pre-obesity) are naturally likely to become obese if efforts are not made by such women to control their weight. Thus, addressing overweight may, to a larger extent, curtail incidence of obesity.
Focusing on individual countries, we found significant differences in overweight and obesity across the countries included in the analysis. For example, in the most recent surveys, Egypt has the highest prevalence of overweight (44%) and obesity (39%) by far, followed by Ghana with an overweight prevalence of 30% and obesity of 22%. Niger (32%) and Rwanda (31%) were two other countries with overweight prevalence of 30% and above. The results on Egypt are not surprising as the country was previously ranked among the countries in the world with the most obese people.34 The results in Ghana are also consistent with previous findings.15 Egypt and Ghana also experienced a significant increase in overweight and obesity in the past two and a half decades. Obesity increased by 65% (7.7% to 22%) in Ghana and by 12% (34% to 39%) in Egypt. Similarly, obesity doubled in Kenya, Benin, Niger, Rwanda, Ivory Coast and Uganda, while tripled in Zambia, Burkina Faso, Mali, Malawi and Tanzania. Thus, while the prevalence of obesity in the aforementioned countries may be considered lower than that of Egypt and Ghana, the increment over time has been doubling or tripling in rates. This suggests that in the next decades, the obesity rates in these countries may catch up with Egypt and Ghana, which are currently leading in terms of the level of prevalence of both overweight and obesity. However, overweight and obesity did not show any significant changes over time in Cameroon, Lesotho, Madagascar and Nigeria. Ethiopia and Madagascar had the lowest prevalence of both obesity and overweight. Similar findings were obtained in Ethiopia and Madagascar in a recent study using the DHS data from 32 African countries.28
The increasing prevalence and trends of overweight and obesity in Africa may be attributed largely to rapid urbanisation taking place in the continent and its associated nutritional transition. For example, in 2010, the share of the African urban population was about 36% and is projected to increase to 50% and 60% by 2030 and 2050, respectively.35 Using Ghana as a case in point, for the first time, the Ghana Population and Housing Census shows that a little over half (50.9%) of country’s population live in urban areas compared with rural areas.36 The growing urbanisation comes along with lifestyle changes such as decreased physical activity and increased supply of high caloric fast foods and sugar-sweetened beverages.16 37–39 Indeed, sedentary lifestyle and high consumption of energy-dense diets are found to account for the increasing burden of overweight and obesity in urban settings of the LMICs.20–22 The consequences of which are increase in NCDs, as there is substantial evidence that the risk of NCDs such as coronary heart disease, ischaemic stroke and type 2 diabetes mellitus increases steadily with increasing BMI.3 4 39 In addition, an increased burden of DALYs is associated with overweight and obesity.3 It is imperative that strategies be implemented to address the problem of overweight and obesity, thereby curbing associated NCD risk in urban Africa. Addressing the issue of overweight and obesity will be an important step towards curbing the surge of NCDs the continent is currently experiencing, which is likely to surpass the toll of sickness and death from infectious diseases by 2030.40 This will further contribute greatly to the potential for African countries to achieve Sustainable Development Goals (SDG 3.4): reducing by one-third premature mortality from NCDs through prevention and treatment, and promote mental health and well-being by 2030.41
In the light of the findings of our study and the literature discussed above, we particularly advocate for targeted interventions to address the incidence of overweight and obesity among urban dwelling women. Intervention strategies described in the literature as ‘effective and essential’42 in addressing overweight and obesity in a developing country context include policy interventions and intersectoral partnerships; addressing food system drivers of caloric overconsumption and improving eating and physical activity environments in key community settings.42 It is believed that effective implementation of these strategies has the potential to curtail the incidence of overweight and obesity. It is important to recognise that large inequalities remain a major issue in many African countries, which may have a bearing on areas that ought to be prioritised and targeted for interventions. For example, in many African countries, it is common to see problems of undernutrition alongside increasing rates of overweight and obesity. This ‘dual burden’ of undernutrition and obesity exists at country level or community level and all the way down to households.16 43 Undernutrition persists as a significant problem44 in many African countries and interventions have been put in place to address it.45–47 However, the issue of overweight and obesity has not received adequate attention as yet in Africa.16 47 More attention of policy-makers and public health practitioners on ways to address the overweight and obesity epidemic, taking into account undernutrition, is warranted.
Strengths and limitations
The key strength of this study is the use of nationally representative data sets, thereby providing more robust estimates of the prevalence and trends of overweight and obesity in the respective countries. Further, height and weight as used in the calculation of BMI was objectively measured by well-trained technicians, reducing possible misclassification of overweight and obesity. The study is also associated with some limitations. To maintain sample comparability over time, we had to limit our sample to women with children under 5 years of age. This may, to some extent, affect the generalisability of the findings, as the sample may not be representative of the entire female population. Another limitation is the cross-sectional nature of the data. Because the surveys used in this analysis were conducted at different times across countries, we were unable to estimate the change in BMI across all countries for the entire survey period. Lack of uniformity in the definition of urban and rural settings may also affect the comparability of the findings across countries since different countries have different definitions of what constitutes urban versus rural. Last, one methodological limitation is that we pooled the data to perform the trend analysis, which may lead to an overestimation of statistical power. To address this limitation, the weight in the pooled data was divided by the number of surveys available for the country.
Conclusion
The study provided clear evidence of increase in overweight and obesity among women in the urban settings of all the countries included in the analysis, with the increase over time being statistically significant in 17 of the 24 countries in the case of obesity and 13 out of the 24 for overweight. We have supported the finding that women dwelling in urban settings are prone to overweight and obesity. The prevalence of obesity increased more than twofold in most countries and more than threefold in others. The prevalence of obesity increased alongside overweight. These findings call for deliberate strategies and interventions by policy-makers, politicians and health promotion experts, focusing on healthy diet, physical activity, weight reduction and maintenance strategies in African countries, particularly in urban areas to curb the growing proportion of unhealthy weight women of childbearing age in urban Africa. Strategies should include measures such as price reduction for healthy foods (eg, fruits and vegetables) and promotion of physical activity. For future research, we suggest the conduct of longitudinal studies to systematically elucidate cumulative changes in individual’s BMI over time. Longitudinal studies will also be able to ascertain the extent to which overweight can lead to mild-to-moderate obesity.
Supplementary Material
Acknowledgments
We wish to express our profound gratitude to The DHS Program, USA for providing us access to the data. We also wish to acknowledge institutions of respective countries that played critical roles in the data collection process.
Footnotes
Contributors: DAA conceived and designed the study, interpreted the results, wrote the first draft of the manuscript and contributed to revision of the manuscript. DAA and ZTD analysed the data. ZTD contributed to the drafting of the analytical strategy. ZTD, SM, BM and ACE contributed to study design, data interpretation and critical revision of the manuscript. All authors take responsibility of any issues that might arise from the publication of this manuscript.
Competing interests: None declared.
Ethics approval: National ethics review committees of respective countries.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: This study was a reanalysis of existing data that are publicly available from the Demographic and Health Surveys Program (DHS Program; http://dhsprogram.com/publications/publication-fr221-dhs-final-reports.cfm). Data are accessible free of charge upon a registration with the DHS Program. The registration is done on the DHS website indicated above.
References
- 1. Wang Y, Chen HJ, Shaikh S, et al. Is obesity becoming a public health problem in India? Examine the shift from under- to overnutrition problems over time. Obes Rev 2009;10:456–74. 10.1111/j.1467-789X.2009.00568.x [DOI] [PubMed] [Google Scholar]
- 2. Martorell R, Khan LK, Hughes ML, et al. Obesity in women from developing countries. Eur J Clin Nutr 2000;54:247–52. 10.1038/sj.ejcn.1600931 [DOI] [PubMed] [Google Scholar]
- 3. World Health Organization. Obesity. Situation and trends: Global Health Observatory (GHO) data. 2016. http://www.who.int/gho/ncd/risk_factors/obesity_text/en/ (accessed 1 Feb 2017).
- 4. Mokdad AH, Ford ES, Bowman BA, et al. Prevalence of obesity, diabetes, and obesity-related health risk factors, 2001. JAMA 2003;289:76–9. 10.1001/jama.289.1.76 [DOI] [PubMed] [Google Scholar]
- 5. PubMed Health. Excess body fat now linked to 13 different types of cance: PubMed Health. 2017. https://www.ncbi.nlm.nih.gov/pubmedhealth/behindtheheadlines/news/2016-08-25-excess-body-fat-now-linked-to-13-different-types-of-cancer/ (accessed 2 Feb 2017).
- 6. Leddy MA, Power ML, Schulkin J. The impact of maternal obesity on maternal and fetal health. Rev Obstet Gynecol 2008;1:170–8. [PMC free article] [PubMed] [Google Scholar]
- 7. Lash MM, Armstrong A. Impact of obesity on women’s health. Fertil Steril 2009;91:1712–6. 10.1016/j.fertnstert.2008.02.141 [DOI] [PubMed] [Google Scholar]
- 8. Lynch CM, Sexton DJ, Hession M, et al. Obesity and mode of delivery in primigravid and multigravid women. Am J Perinatol 2008;25:163–7. 10.1055/s-2008-1061496 [DOI] [PubMed] [Google Scholar]
- 9. Arianas EA, Rankin KM, Norr KF, et al. Maternal weight status and responsiveness to preterm infant behavioral cues during feeding. BMC Pregnancy Childbirth 2017;17:113 10.1186/s12884-017-1298-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Haycraft EL, Blissett JM. Maternal and paternal controlling feeding practices: reliability and relationships with BMI. Obesity 2008;16:1552–8. 10.1038/oby.2008.238 [DOI] [PubMed] [Google Scholar]
- 11. Rising R, Lifshitz F. Relationship between maternal obesity and infant feeding-interactions. Nutr J 2005;4:17 10.1186/1475-2891-4-17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Mendez MA, Monteiro CA, Popkin BM. Overweight exceeds underweight among women in most developing countries. Am J Clin Nutr 2005;81:714–21. [DOI] [PubMed] [Google Scholar]
- 13. Kinnunen TI, Neupane S. Prevalence of overweight among women of childbearing age in Nepal: trends from 2001 to 2011 and associations with socio-demographic factors. Matern Child Health J 2014;18:1846–53. 10.1007/s10995-013-1428-1 [DOI] [PubMed] [Google Scholar]
- 14. Razak F, Corsi DJ, Slutsky AS, et al. Prevalence of Body Mass Index Lower Than 16 Among Women in Low- and Middle-Income Countries. JAMA 2015;314:2164–71. 10.1001/jama.2015.15666 [DOI] [PubMed] [Google Scholar]
- 15. Ofori-Asenso R, Agyeman AA, Laar A, et al. Overweight and obesity epidemic in Ghana-a systematic review and meta-analysis. BMC Public Health 2016;16:1239 10.1186/s12889-016-3901-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Popkin BM, Adair LS, Ng SW. Global nutrition transition and the pandemic of obesity in developing countries. Nutr Rev 2012;70:3–21. 10.1111/j.1753-4887.2011.00456.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Neuman M, Kawachi I, Gortmaker S, et al. Urban-rural differences in BMI in low- and middle-income countries: the role of socioeconomic status. Am J Clin Nutr 2013;97:428–36. 10.3945/ajcn.112.045997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Yadav K, Krishnan A. Changing patterns of diet, physical activity and obesity among urban, rural and slum populations in north India. Obes Rev 2008;9:400–8. 10.1111/j.1467-789X.2008.00505.x [DOI] [PubMed] [Google Scholar]
- 19. World Health Organization. Obesity and overweight. 2016. http://www.who.int/mediacentre/factsheets/fs311/en/ (accessed 3 Apr 2017).
- 20. Ziraba AK, Fotso JC, Ochako R. Overweight and obesity in urban Africa: a problem of the rich or the poor? BMC Public Health 2009;9:1–9. 10.1186/1471-2458-9-465 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Abrha S, Shiferaw S, Ahmed KY. Overweight and obesity and its socio-demographic correlates among urban Ethiopian women: evidence from the 2011 EDHS. BMC Public Health 2016;16:636 10.1186/s12889-016-3315-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Tebekaw Y, Teller C, Colón-Ramos U. The burden of underweight and overweight among women in Addis Ababa, Ethiopia. BMC Public Health 2014;14:1126 10.1186/1471-2458-14-1126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Subramanian SV, Perkins JM, Özaltin E, et al. Weight of nations: a socioeconomic analysis of women in low- to middle-income countries. Am J Clin Nutr 2011;93:413–21. 10.3945/ajcn.110.004820 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Monteiro CA, Conde WL, Lu B, et al. Obesity and inequities in health in the developing world. Int J Obes Relat Metab Disord 2004;28:1181–6. 10.1038/sj.ijo.0802716 [DOI] [PubMed] [Google Scholar]
- 25. Jones-Smith JC, Gordon-Larsen P, Siddiqi A, et al. Is the burden of overweight shifting to the poor across the globe? Time trends among women in 39 low- and middle-income countries (1991-2008). Int J Obes 2012;36:1114–20. 10.1038/ijo.2011.179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Kimani-Murage EW, Muthuri SK, Oti SO, et al. Evidence of a Double Burden of Malnutrition in Urban Poor Settings in Nairobi, Kenya. PLoS One 2015;10:e0129943 10.1371/journal.pone.0129943 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Adeboye B, Bermano G, Rolland C. Obesity and its health impact in Africa: a systematic review. Cardiovasc J Afr 2012;23:512–21. 10.5830/CVJA-2012-040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Neupane S, Prakash KC, Doku DT. Overweight and obesity among women: analysis of demographic and health survey data from 32 Sub-Saharan African Countries. BMC Public Health 2016;16:30 10.1186/s12889-016-2698-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. The DHS Program. Demographic and Health Surveys. 2017. https://dhsprogram.com/data/dataset_admin/download-datasets.cfm (accessed 2 Feb 2017).
- 30. The DHS Program. DHS Methodology. 2017. http://dhsprogram.com/What-We-Do/Survey-Types/DHS-Methodology.cfm (accessed 2 Feb 2017).
- 31. Shireen A, Kothari MT, Pullum T. An Assessment of the Quality of DHS Anthropometric Data, 2005-2014 DHS Methodological Reports No. 16 Rockville. Maryland, USA: ICF International, 2015. [Google Scholar]
- 32. Eknoyan G, Quetelet A. (1796 –1874) - the average man and indices of obesity. Nephrol Dial Transplant 1796;2008:47–51. [DOI] [PubMed] [Google Scholar]
- 33. World Health Organization. BMI classification: WHO. 2006. http://apps.who.int/bmi/index.jsp?introPage=intro_3.html (accessed 2 Feb 2017).
- 34. Murray CTL, Ng M. Nearly one-third of the world’s population is obese or overweight, new data show 2016. 2017. http://www.healthdata.org/news-release/nearly-one-third-world%E2%80%99s-population-obese-or-overweight-new-data-show (accessed 3 Apr 2017).
- 35. African Development Bank. Urbanization in Africa. 2012. https://www.afdb.org/en/blogs/afdb-championing-inclusive-growth-across-africa/post/urbanization-in-africa-10143/ (accessed 5 Apr 2017).
- 36. Ghana Statistical Service (GHS). Population and housing census: summary report of final results. Accra: GHS, 2012. [Google Scholar]
- 37. Duda RB, Dark R, Seffah J, et al. Prevalence of Obesity in Women of Accra Ghana. Afr J Health Sci 2007;14:154–9. [Google Scholar]
- 38. Abubakari AR, Lauder W, Jones MC, et al. Prevalence and time trends in diabetes and physical inactivity among adult West African populations: the epidemic has arrived. Public Health 2009;123:602–14. 10.1016/j.puhe.2009.07.009 [DOI] [PubMed] [Google Scholar]
- 39. Mohan V, Mathur P, Deepa R, et al. Urban rural differences in prevalence of self-reported diabetes in India--the WHO-ICMR Indian NCD risk factor surveillance. Diabetes Res Clin Pract 2008;80:159–68. 10.1016/j.diabres.2007.11.018 [DOI] [PubMed] [Google Scholar]
- 40. Organization WH. Research shows higher risk of developing Non-communicable diseases in Africa: WHO. 2016. http://www.afro.who.int/en/media-centre/pressreleases/item/9285-research-shows-higher-risk-of-developing-non-communicable-diseases-in-africa.html (accessed 16 Feb 2017).
- 41. United Nations. Resolution adopted by the General Assembly on 25 September 2015-Transforming our world: the 2030 Agenda for Sustainable Development. 2015. http://www.un.org/ga/search/view_doc.asp?symbol=A/RES/70/1&Lang=E (accessed 16 Feb 2017).
- 42. Kumanyika S, Libman K, Garcia A. strategic action to combat the obesity epidemic. Report of the Obesity Working Group. 2013. http://www.wish-qatar.org/app/media/383 (accessed 28 Jul 2017).
- 43. Popkin BM. The nutrition transition and obesity in the developing world. J Nutr 2001;131:871SS-3S. [DOI] [PubMed] [Google Scholar]
- 44. Mendez MA, Monteiro CA, Popkin BM. Overweight exceeds underweight among women in most developing countries. Am J Clin Nutr 2005;81:714–21. [DOI] [PubMed] [Google Scholar]
- 45. Bosu WK. An overview of the nutrition transition in West Africa: implications for non-communicable diseases. Proc Nutr Soc 2015;74:466–77. 10.1017/S0029665114001669 [DOI] [PubMed] [Google Scholar]
- 46. Jaacks LM, Slining MM, Popkin BM. Recent underweight and overweight trends by rural-urban residence among women in low- and middle-income countries. J Nutr 2015;145:352–7. 10.3945/jn.114.203562 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Fanzo J. The Nutrition Challenge in Sub-Saharan Africa. Working paper Rome, Italy: UNDP Regional Bureau for Africa. 2012. http://www.undp.org/content/dam/rba/docs/Working%20Papers/Nutrition%20Challenge.pdf (accessed 28 Jul 2017).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.