Abstract
Introduction
Low back pain (LBP) is one of the largest and most frequent public health problems worldwide. Photobiomodulation therapy (PBMT) is a frequently used non-pharmacological therapy for the treatment of musculoskeletal disorders. However, there is little high-quality scientific evidence that demonstrates the effectiveness of PBMT in the treatment of patients with chronic LBP in the short, medium and long term. Therefore, the objective of this clinical trial is to evaluate the effects of PBMT in patients with chronic non-specific LBP in the short, medium and long term.
Methods and analyses
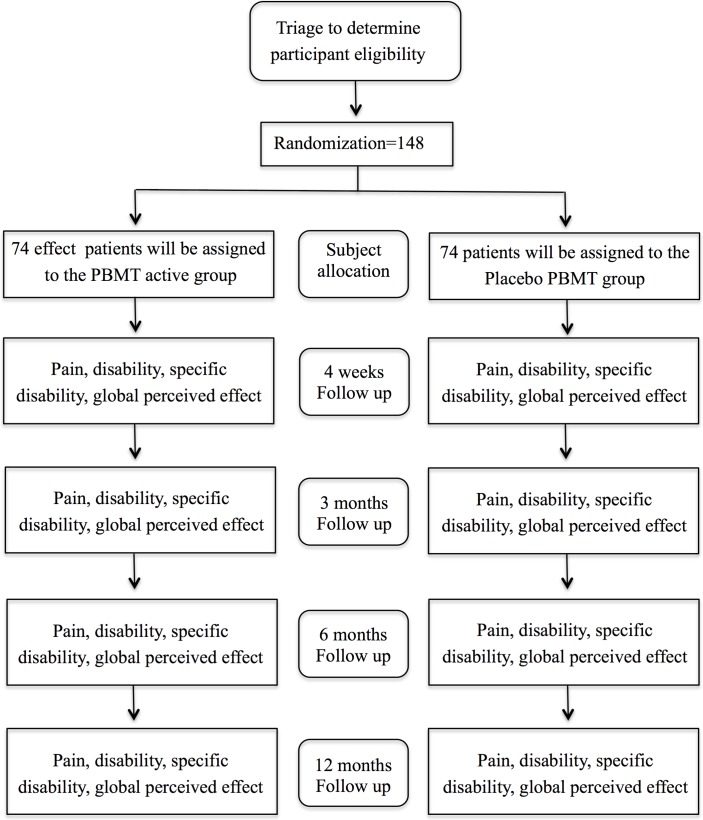
This is a prospectively registered, two-arm randomised placebo-controlled trial with blinded patients, assessors and treatment providers. One hundred and forty-eight patients with chronic non-specific LBP will be recruited. Treatment sessions will be provided three times a week for 4 weeks (totaling 12 sessions) with patients receiving either placebo or active PBMT. For ethical reasons, all patients, regardless of treatment allocation, will also receive an information booklet based on ‘The Back Book’. Clinical outcomes will be measured at baseline, at the end of treatment, as well as 3, 6 and 12 months after randomisation. The primary outcomes will be pain intensity and disability measured after 12 sessions of treatment. The secondary outcomes will be pain intensity and disability measured at 3, 6 and 12 months after randomisation, in addition to specific disability and global perceived effect in all time points.
Ethics and dissemination
The study was approved by the Research Ethics Committee of Universidade Cidade de São Paulo. The results will be disseminated through scientific publications and presentations at national and international scientific meetings.
Trial registration number
Keywords: chronic low Back pain, photobiomodulation therapy, low-level laser therapy, Lllt, pbmt
Strengths and limitations of this study.
The present study can be considered to have high methodological quality since it is a randomised, controlled and prospectively registered clinical trial.
One of the strengths of the study is that it is triple blinded, that is, outcome assessors, therapists and patients will be blinded to interventions over the course of the study.
The sample size was calculated to provide the appropriate statistical power to detect precise differences for the primary outcomes of the study.
In our study, we will test the effects of a single dose of photobiomodulation therapy (PBMT; ie, 24 Joules). PBMT is known to present a biphasic dose–response pattern, that is, within a therapeutic window (dosage range), the effects of biostimulation can be observed. However, if dosages below or above this window are used, these effects may not be observed. Therefore, the application of only one dose of PBMT may be considered a limitation of this trial. However to minimise this limitation, we based the choice of our parameters using the best available evidence.
Introduction
Low back pain (LBP) is ranked as one of the most prevalent health problems and is highly associated with disability worldwide.1–4 It is estimated that about 12% of the world’s population suffer from LBP.5 Furthermore, LBP generates high levels of work absenteeism and excessive costs to health systems.1 2 The prognosis of LBP is directly related to the duration of symptoms, with less favourable prognoses in patients with chronic LBP (ie, with a duration of symptoms longer than 3 months).6–10 Therefore, the ideal treatment for chronic LBP represents a significant challenge, since there are no treatments that cure persistent LBP. However, several interventions provide low to moderate effects in reducing pain and disability on this population.11 The existing treatments for LBP can be divided into three categories: (1) pharmacological therapies, which trigger several adverse effects with prolonged use12–14; (2) non-pharmacological therapies, which minimise undesirable effects and are moderately effective in LBP15 and surgery, used only when conservative treatment is not efficacious.16 Several therapies can be used to treat LBP by controlling symptoms, minimising disability and improving the patients' quality of life.17
Photobiomodulation therapy (PBMT) is a non-pharmacological intervention often used in the treatment of musculoskeletal disorders such as LBP.18–21 PBMT consists in applying a non-ionised form of light, which includes laser (light amplification by stimulated emission of radiation), light-emitting diodes and other lights with a broader spectrum ranging from visible to infrared.22 Recent evidence23–28 suggests that PBMT triggers positive physiological effects, such as increased microcirculation,23 increased ATP synthesis24 25 stimulation of the mitochondrial respiratory chain,24 25 stimulation of mitochondrial function26 and factors that may influence the metabolism of various pathologies. In addition, there is evidence that PBMT reduces the release of both reactive oxygen species) and creatine kinase activity and also increases the production of antioxidants and heat shock proteins.27 28
As PBMT has been successfully proven as an effective intervention for neck pain patients,29 it is likely that PBMT could also be a reasonable option for patients with LBP. A range of previous trial have shown the effects of PBMT on acute, subacute and chronic LBP. Basford et al18 and Gur et al19 observed that PBMT appears to be effective in reducing pain and disability triggered by subacute and chronic LBP, respectively. While Konstantinovic et al20 and Vallone et al21 found that PBMT combined with non-steroidal anti-inflammatory drugs (NSAIDs) and exercise were efficient in reducing pain intensity in patients with acute and chronic LBP, respectively. In a recent systematic review, Glazov et al30 found a clinically significant reduction in pain intensity in chronic LBP in patients treated with PBMT, although a reliable conclusion was hindered by the high heterogeneity in the parameters of therapy application. Furthermore, a recent clinical practice guidelines31 recommended the use of the PBMT as a possible non-pharmacological treatment for chronic LBP. On the other hand, another trial32 did not detected differences between PBMT and placebo treatments on pain and disability in mixed sample of patients with acute and chronic LBP associated with lumbar disk degeneration. These findings show that there are still conflicts in the literature about PBMT in LBP. Therefore, high-quality and adequately powered trials are strongly needed.
Therefore, in spite of the positive results obtained in the aforementioned studies in favour of PBMT, some factors warrant further investigation with high-quality studies on the effects of PBMT applied in isolation in chronic non-specific LBP. Hence, it is necessary to conduct a high-quality, adequately powered, randomised placebo-controlled trial with outcomes have been measured at medium and long terms. Therefore, the objective of this study is to evaluate the effects of PBMT against placebo in patients with chronic non-specific LBP in the short, medium and long term for the outcomes of pain intensity, general and specific disability and global perceived effect.
Methods and analyses
Design
A randomised, triple-blinded (patients, therapists and outcome assessors), placebo-controlled trial will be performed. The protocol of this study has been prospectively registered on Clinicaltrials.gov (NCT03089424).
Study setting
The study will be conducted at the Centre for Excellence in Clinical Research in Physiotherapy of Universidade Cidade de São Paulo, Brazil.
Eligibility criteria
The study assessors will determine whether or not patients will be eligible to participate in the study based on patient history and clinical examination.
Inclusion criteria
Patients with non-specific chronic LBP, defined as pain or discomfort between the costal margins and inferior gluteal folds with or without referred pain to the lower limbs;
Persistent LBP for at least 3 months33;
Aged between 18 and 65 years;
Both genders.
Exclusion criteria
Patients with severe skin diseases (eg, skin cancer, erysipelas, severe eczema, severe dermatitis, severe psoriasis and severe hives lupus);
Patients with LBP associated with nerve root compromise (measured by clinical examination of dermatomes, myotomes and reflexes)34 35;
Serious spinal pathologies such as fractures, tumours, inflammatory and infectious diseases;
Decompensated heart disease or metabolic disorders;
Previous spinal surgery;
Pregnancy.
Interventions
For ethical reasons, on the first day of treatment, all groups will receive an information booklet on LBP called ‘The Back Book’36 based on the recommendations of the European Guidelines.35 37 The booklet can be accessed freely via internet and it has been translated into Portuguese by our research team. At each treatment session, patients will receive further explanations on the contents of the booklet. There is consistent evidence that The Back Book is useful for patients with LBP38 and it has been used in clinical trials conducted by our research group.39 40
Patients will then be randomly allocated to two groups to be submitted to the active PBMT or placebo interventions. The active and placebo PBMT will be performed using the same device and the irradiated sites will be the same in both therapies. To ensure blinding for therapists and patients, the device will emit the same sounds and the same information on the display regardless of the programmed mode (active or placebo). Furthermore, because the device produces a non-significant amount of heat,41 the patients will not be able to know if active or placebo PBMT will be administered. The device was previously coded as active or placebo modes, and only one researcher not involved in the randomisation, treatment and evaluation is aware of these codes. Patients will undergo treatment (active PBMT or placebo) according to prior randomisation, three times a week (with a minimal interval of 24 hours) for four consecutive weeks, totalling 12 therapy sessions. The choice of treatment frequency was based on Basford et al.18 The total treatment (active PBMT or placebo) time will be 27 min per patient. The patients will be positioned preferably in prone. However, in specific cases where patients do not tolerate this position due to pain, we will respect the patient’s preferred positioning. Intervention specifications:
1. Active PBMT Group: The PBMT will be performed using the Multi Radiance Medical Super Pulsed Laser MR4 console (Solon, Ohio, USA), with the SE25 (emitter with an area of 4 cm2) and LaserShower (emitter with an area of 20 cm2) cluster probes as emitters. Nine sites will be irradiated on the patient’s lumbar region. PBMT irradiation sites were chosen based on previous studies18–21 and to cover the largest possible area of the lumbar spine: three central sites on top of the spinous processes (between T11 and T12, L2 and L3, L5 and S1), using the SE25 (3000 Hz of frequency, 3 min of irradiation per site, 24.75 J per site, a totalising 74.25 J irradiated from SE25); in the same direction, but laterally, three sites on the left and three on the right (on the paravertebral muscles), using the LaserShower (1000 Hz of frequency, 3 min of irradiation per site, 24.30 J per site, a total of 145.80 J irradiated from LaserShower). At each treatment session, patients will receive a total dose of 220.05 J. At the end of the 12 treatments sessions, patients will receive a total dose of 2640.60 J. Table 1 shows parameters for SE25 and LaserShower cluster probe. This PBMT application protocol was based on the study of Leal Junior et al.42
Table 1.
Parameters for SE25 and LaserShower cluster probe
| SE25 | LaserShower | |
| Number of lasers | 1 super-pulsed infrared | 4 super-pulsed infrared |
| Wavelength (nm) | 905 (±1) | 905 (±1) |
| Frequency (Hz) | 3000 | 1000 |
| Peak power (W)— each | 25 | 12.5 |
| Average mean optical output (mW)—each | 7.5 | 1.25 |
| Power density (mW/cm2)—each | 17.05 | 2.84 |
| Energy density (J/cm2)—each | 3.07 | 0.511 |
| Dose (J) - each | 1.35 | 0.225 |
| Spot size of laser (cm2)—each | 0.44 | 0.44 |
| Number of red LEDs | 4 red | 4 red |
| Wavelength of red LEDs (nm) | 640 (±10) | 640 (±10) |
| Frequency (Hz) | 2 | 2 |
| Average optical output (mW)—each | 15 | 15 |
| Power density (mW/cm2)—each | 16.67 | 16.67 |
| Energy density (J/cm2)— each | 3 | 3 |
| Dose (J) - each | 2.7 | 2.7 |
| Spot size of red LED (cm2)—each | 0.9 | 0.9 |
| Number of infrared LEDs | 4 infrared | 4 infrared |
| Wavelength of infrared LEDs (nm) | 875 (±10) | 875 (±10) |
| Frequency (Hz) | 16 | 16 |
| Average optical output (mW)—each | 17.5 | 17.5 |
| Power density (mW/cm2)—each | 19.44 | 19.44 |
| Energy density (J/cm2)—each | 3.5 | 3.5 |
| Dose (J)—each | 3.15 | 3.15 |
| Spot Size of LED (cm2)—each | 0.9 | 0.9 |
| Magnetic field (mT) | 35 | 35 |
| Irradiation time per site (s) | 180 | 180 |
| Total dose per site (J) | 24.75 | 24.30 |
| Aperture of device (cm2) | 4 | 20 |
| Application mode | Cluster probe held stationary in skin contact with a 90-degree angle and slight pressure | Cluster probe held stationary in skin contact with a 90-degree angle and slight pressure |
LED, light-emitting diode.
2. Placebo PBMT Group: The placebo PBMT will be delivered using the same device that activates PBMT but without any emission of therapeutic dose. Patients will receive a total dose of 0 J in placebo mode. The placebo mode simulates the pragmatism of clinical practice and increases the credibility of the use of the equipment in relation to the treated patients. The placebo technique has already been widely used in other studies with patients with LBP,40 43–48 as well as in studies using PBMT.41 49 50
Figure 1 shows the PBMT irradiation sites.
Figure 1.
Photobiomodulation therapy irradiation sites.
We will use two different emitters in PBMT (active or placebo) because we have different objectives in each application area, which consequently require different mechanisms of action. We will use the SE25 emitter on the spinous processes to inhibit pain. Considering the smaller area of this emitter (4 cm2), the power density will be increased, which will consequently induce the triggering of inhibitory effects, such as a decrease in the axonal flow and thus analgesic effects.51 52 In addition, the higher frequency used in this emitter will also increase the number of photons that will reach the target tissue, which will also promote the triggering of inhibitory effects and consequent analgesic effect. For the erector spinae muscles, we will use the LaserShower 50 (LS50) emitter to promote photobiostimulatory effects, considering the larger area of the device (20 cm2), with consequent lower power density. In addition, this emitter has a lower frequency, which will consequently decrease the number of photons delivered to the target tissue. With these factors, we believe that we will promote an increase in the production of ATP,24 25 an increase in microcirculation23 and consequently a decrease in muscle fatigue and stiffness. This therapeutic strategy using different emitters and different frequencies showed positive effects in the reduction of non-specific knee pain in a previous study that used this same PBMT device and these same emitters42; however, the frequencies and doses were adapted for back pain patients.
Outcomes and blinding
Primary outcomes of the study will be obtained at baseline and immediately after the last treatment session (4 weeks). Secondary outcomes of the study will be obtained at baseline, at the end of treatment (4 weeks) and 3, 6 and 12 months after randomisation. These outcomes will be collected by an assessor who will not be aware of patient allocation to their treatment groups.
The primary outcomes of the study will be
Pain intensity measured by the Pain Numerical Rating Scale.53 Pain Numerical Rating Scale evaluates pain intensity levels perceived by the patient on an 11-point scale ranging from 0 to 10, with 0 being ‘no pain’ and 10 ‘the worst possible pain’.53 Patients will be instructed to score the level of pain intensity based on the last 7 days.
Disability associated with LBP, as measured by the Roland-Morris Disability Questionnaire.54 55 The questionnaire consists of 24 items that describe situations that patients may have difficulty performing on a daily basis due to LBP. The greater the number of affirmative answers is, the higher the level of functional disability associated with LBP.53 55 Patients will be instructed to answer according to their condition on the day of administration of the questionnaire.
The secondary outcomes of the study will be
Specific disability, as measured by the Patient-Specific Functional Scale.53 The Patient-Specific Functional Scale is global and can be used for any part of the body. The measurement is done on an 11-point Likert scale for each activity, and the higher the average score is (ranging from 0 and 10 points), the better the patient’s ability to perform the activities. The patients will be asked to identify up to three activities that they consider they are incapable of performing or that they have some difficulty performing.53 56 57
Global perceived effect as measured by the Global Perceived Effect Scale.53 Global Perceived Effect Scale is an 11-point Likert scale, ranging from −5 to +5, that compares the patient’s current condition to the onset of symptoms.53 Positive scores represent improvement, while the negative scores represent worsening in relation to the onset of symptoms. Values closer to 5 mean greater intensity of this perception.53
Pain intensity measured by the Pain Numerical Rating Scale.53
Disability associated with LBP, as measured by the Roland-Morris Disability Questionnaire.54 55
Participant timeline
The Consolidated Standards of Reporting Trials flowchart summarising experimental procedures and patients are shown in figure 2.
Figure 2.
Flow diagram of the study. PBMT, photobiomodulation therapy.
Sample size
The sample calculation of the study was performed to detect a 1-point difference for the outcome pain intensity (as measured by the Pain Numerical Rating Scale),53 with an estimated SD of 1.84 points and 4 points for the outcome disability associated with LBP (measured by the Roland-Morris Disability Questionnaire),54 55 with an estimated SD of 4.9 points. A statistical power of 80% was considered for the two outcomes, with α of 5% and a possible sample loss of up to 15%. Therefore, a total of 148 patients will be required for the study.
Recruitment
Patients seeking treatment for chronic LBP will be recruited at primary or secondary care health services. We will partner with supervising clinicians at primary and secondary health services so that they will refer chronic non-specific LBP patients to our study for treatment.
Randomisation
Prior to initiation of treatment, patients will be randomised into their respective intervention groups. The randomisation will be generated by a computer program (Excel Office 2010) and performed by a participating researcher not involved with the recruitment or evaluation of patients. This same researcher will be responsible for programming the PBMT device according to the result of the randomisation. The PBMT device used in the present study will make the same sounds regardless of the programmed dose and mode (active PBMT or placebo PBMT). This researcher will be instructed not to disclose the programmed intervention to the therapist or any of the patients and other researchers involved in the study until its completion. Patient and therapist will be blinded throughout the treatment. Concealed allocation will be achieved through the use of sequentially numbered, sealed and opaque envelopes.
Data collection
The patients will be welcomed by the study’s blinded assessor who will determine whether they will be eligible to participate in the study. Subsequently, a file will be completed with the patient’s sociodemographic data and clinical history. Next, the primary outcomes and the secondary outcomes of the study will be collected. Then, all eligible patients will be randomised and allocated into two treatment groups: active PBMT or placebo PBMT. At the end of the 12 treatment sessions, the primary and secondary outcomes of the study participants will be reassessed by the same evaluator who performed the baseline assessment. The 3, 6 and 12-month follow-ups will be performed by telephone by the same evaluator who carried out the other evaluations. All of the questionnaires that will be used in the present study have been fully tested for their measurement properties.53 55 These measurement properties were also tested over the phone. Therefore, we are confident that the assessments are reliable.
Statistical analysis
The statistical analysis will be conducted following the principles of intention-to-treat analysis.58 The normality of the data will be tested by visual inspection of histograms and the characterisation of the participants will be calculated using descriptive statistical tests. The between-group differences (treatment effects) and their respective 95% CIs will be calculated by using mixed linear models59 using the group-by-time interaction terms. The analyses will be performed using SPSS V.19.
Ethics
The present study was approved by the Research Ethics Committee of Universidade Cidade de São Paulo under number 1.964.094. All patients eligible for the study will be informed by study assessors of the objectives and will be required to complete the informed consent form (see online supplementary appendix 1), as determined by Brazilian National Health Council Resolution 196/96.
bmjopen-2017-017202supp001.pdf (71.5KB, pdf)
Research personnel will take all appropriate and customary steps to ensure that data remain secure and that patient privacy and confidentiality will be maintained.
Dissemination policy
The study will be disseminated through publication in peer-reviewed international journals, as well as presentations at national and international conferences.
Discussion
Chronic LBP is a condition that is often associated with disability, emotional alterations and absenteeism from work.8 Since chronic LBP is very prevalent,11 it has a great financial impact, generating high costs, both direct and indirect.60 This fact demonstrates the importance of the constant investigation of more suitable treatments for LBP, aiming at the well-being of the patient and the reduction of expenses for health systems.
PBMT is one of the interventions recommended for the treatment of chronic LBP,31 however, it is a relatively recent therapy given that the first clinical trial investigating its effects on LBP was published in 1999.18 Since then, there are still conflicts in the literature about PBMT in LBP. Although there is evidence that PBMT is no better than placebo treatment on pain and disability in a mixed sample of patients with acute and chronic LBP,32 some studies have demonstrated the efficacy of PBMT in chronic and acute LBP.18–21 Nevertheless, there are still issues to be clarified about its efficacy, as there are no high-quality methodological studies that test PBMT versus placebo in LBP patients. To date, studies evaluating the effects of PBMT on chronic non-specific LBP have not been prospectively registered18–21 32; have a small sample size18 19 21 32 and have high risk of bias. In addition, none of the studies were either triple blinded or were analysed using intention-to-treat principles.
It is extremely important to carry out studies with high methodological quality aimed at contributing to a better understanding of the effects of PBMT on LBP. Only then will it be possible to determine whether PBMT can be used as one of the treatments of choice for LBP. If the effectiveness of PBMT in LBP is confirmed, it could be used as an alternative method to NSAIDs or opioids, for example, since it causes similar or superior effects to these drugs, shown in other chronic musculoskeletal disorders,61 62 without the presence of known adverse effects at present. We believe that, by providing relevant and compelling information about PBMT, we will contribute to a safer and more effective clinical practice.
Nevertheless, it is important to highlight that PBMT presents a biphasic dose–response pattern, that is, within a therapeutic window (dose range) the biostimulation effects can be seen. Very low doses may not trigger responses in the irradiated tissue, whereas very high doses may cause inhibition.52 In addition, the power and time of irradiation are also extremely important parameters to obtain better results with the PBMT.63 Therefore, the choice of PBMT parameters is essential for obtaining positive results and represents an important challenge in treating any musculoskeletal disorder. To date, there is great heterogeneity in the parameters of PBMT used for the treatment of LBP, and it is not possible to conclude the best dose for the treatment of this disorder. Thus, our parameters were adapted from the best evidence available42 and took into consideration the dosage recommended by World Association for Laser Therapy.63 Therefore, although we believe that the dosage chosen for the present study is the most likely to be effective in triggering the expected results, a limitation of our study is that we will test only one dose of PBMT.
The present study can be considered to have high methodological quality, since it is a randomised, controlled and prospectively registered clinical trial. In addition, one of the strengths of the study is that it is triple blinded, that is, evaluators, therapists and patients will be blinded to interventions over the course of the study. Finally, the sample size was calculated to provide the appropriate statistical power to detect precise differences in the primary outcomes of the study. Therefore, we believe that this study will contribute to the evidence-based practice of PBMT in patients with chronic LBP.
Supplementary Material
Footnotes
Contributors: SST and LOPC contributed to the concept and design of the study and established the hypothesis and wrote the original proposal. SST, LCMC, LSG, ACA, DPN, FCM, MAA and LOPC contributed significantly in creating the manuscript. LCMC and LOPC performed critical revisions of the manuscript. SST, LCMC and LOPC wrote the final version of the manuscript. All authors read and approved the final version of the manuscript.
Funding: This work was supported by FAPESP (postdoctoral scholarship of Shaiane Silva Tomazoni) grant number 2016/10265-0.
Competing interests: None declared.
Ethics approval: Research Ethics Committee of Universidade Cidade de São Paulo (UNICID) under number 1.964.094.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. Tulder MV. Chapter 1. European guidelines. Eur Spine J 2006;15:134–5. [Google Scholar]
- 2. American Academy Of Orthopaedic Surgeons. US Bone and Joint Decade - The Burden of Musculoskeletal Diseases in the United States. Rosemont, IL, USA 2008. [Google Scholar]
- 3. Dagenais S, Caro J, Haldeman S. A systematic review of low back pain cost of illness studies in the United States and internationally. Spine J 2008;8:8–20. 10.1016/j.spinee.2007.10.005 [DOI] [PubMed] [Google Scholar]
- 4. Murray CJ, Lopez AD. Measuring the global burden of disease. N Engl J Med 2013;369:448–57. 10.1056/NEJMra1201534 [DOI] [PubMed] [Google Scholar]
- 5. Hoy D, Bain C, Williams G, et al. . A systematic review of the global prevalence of low back pain. Arthritis Rheum 2012;64:2028–37. 10.1002/art.34347 [DOI] [PubMed] [Google Scholar]
- 6. Henschke N, Maher CG, Refshauge KM, et al. . Prognosis in patients with recent onset low back pain in Australian primary care: inception cohort study. BMJ 2008;337:a171 10.1136/bmj.a171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Costa LC, Maher CG, McAuley JH, et al. . Prognosis for patients with chronic low back pain: inception cohort study. BMJ 2009;339:b3829 10.1136/bmj.b3829 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Da C Menezes Costa L, Maher CG, Hancock MJ, Mcauley JH, Herbert RD, Costa LO. The prognosis of acute and persistent low-back pain: a meta-analysis. CMAJ 2012;184:E613–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Beattie PF, Silfies SP, Jordon M. The evolving role of physical therapists in the long-term management of chronic low back pain: longitudinal care using assisted self-management strategies. Braz J Phys Ther 2016;20:580–91. 10.1590/bjpt-rbf.2014.0180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Medeiros FC, Costa LOP, Added MAN, et al. . Longitudinal monitoring of patients with chronic low back pain during physical therapy treatment using the STarT back screening tool. J Orthop Sports Phys Ther 2017;47:314–23. 10.2519/jospt.2017.7199 [DOI] [PubMed] [Google Scholar]
- 11. Maher C, Underwood M, Buchbinder R. Non-specific low back pain. Lancet 2017;389:736–47. 10.1016/S0140-6736(16)30970-9 [DOI] [PubMed] [Google Scholar]
- 12. Bjordal JM, Ljunggren AE, Klovning A, et al. . Non-steroidal anti-inflammatory drugs, including cyclo-oxygenase-2 inhibitors, in osteoarthritic knee pain: meta-analysis of randomised placebo controlled trials. BMJ 2004;329:1317 10.1136/bmj.38273.626655.63 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Chou R. Pharmacological management of low back pain. Drugs 2010;70:387–402. 10.2165/11318690-000000000-00000 [DOI] [PubMed] [Google Scholar]
- 14. Dagenais S, Tricco AC, Haldeman S. Synthesis of recommendations for the assessment and management of low back pain from recent clinical practice guidelines. Spine J 2010;10:514–29. 10.1016/j.spinee.2010.03.032 [DOI] [PubMed] [Google Scholar]
- 15. Van Middelkoop M, Rubinstein SM, Kuijpers T, et al. . A systematic review on the effectiveness of physical and rehabilitation interventions for chronic non-specific low back pain. Eur Spine J 2011;20:19–39. 10.1007/s00586-010-1518-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Bertagnoli R. Disc surgery in motion. SpineLine 2004;5:23–8. [Google Scholar]
- 17. Sanders SH, Rucker KS, Anderson KO, et al. . Clinical practice guidelines for chronic non-malignant pain syndrome patients. J Back Musculoskelet Rehabil 1995;5:115–20. 10.3233/BMR-1995-5204 [DOI] [PubMed] [Google Scholar]
- 18. Basford JR, Sheffield CG, Harmsen WS. Laser therapy: a randomized, controlled trial of the effects of low-intensity Nd:YAG laser irradiation on musculoskeletal back pain. Arch Phys Med Rehabil 1999;80:647–52. 10.1016/S0003-9993(99)90167-3 [DOI] [PubMed] [Google Scholar]
- 19. Gur A, Karakoc M, Cevik R, et al. . Efficacy of low power laser therapy and exercise on pain and functions in cParameters for SE25™ and LaserShower™ cluster probehronic low back pain. Lasers Surg Med 2003;32:233–8. 10.1002/lsm.10134 [DOI] [PubMed] [Google Scholar]
- 20. Konstantinovic LM, Kanjuh ZM, Milovanovic AN, et al. . Acute low back pain with radiculopathy: a double-blind, randomized, placebo-controlled study. Photomed Laser Surg 2010;28:553–60. 10.1089/pho.2009.2576 [DOI] [PubMed] [Google Scholar]
- 21. Vallone F, Benedicenti S, Sorrenti E, et al. . Effect of diode laser in the treatment of patients with nonspecific chronic low back pain: a randomized controlled trial. Photomed Laser Surg 2014;32:490–4. 10.1089/pho.2014.3715 [DOI] [PubMed] [Google Scholar]
- 22. Anders JJ, Lanzafame RJ, Arany PR. Low-level light/laser therapy versus photobiomodulation therapy. Photomed Laser Surg 2015;33:183–4. 10.1089/pho.2015.9848 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Tullberg M, Alstergren PJ, Ernberg MM. Effects of low-power laser exposure on masseter muscle pain and microcirculation. Pain 2003;105:89–96. 10.1016/S0304-3959(03)00166-0 [DOI] [PubMed] [Google Scholar]
- 24. Silveira PC, Silva LA, Fraga DB, et al. . Evaluation of mitochondrial respiratory chain activity in muscle healing by low-level laser therapy. J Photochem Photobiol B 2009;95:89–92. 10.1016/j.jphotobiol.2009.01.004 [DOI] [PubMed] [Google Scholar]
- 25. Albuquerque-Pontes GM, Vieira RP, Tomazoni SS, et al. . Effect of pre-irradiation with different doses, wavelengths, and application intervals of low-level laser therapy on cytochrome c oxidase activity in intact skeletal muscle of rats. Lasers Med Sci 2015;30:59–66. 10.1007/s10103-014-1616-2 [DOI] [PubMed] [Google Scholar]
- 26. Xu X, Zhao X, Liu TC, et al. . Low-intensity laser irradiation improves the mitochondrial dysfunction of C2C12 induced by electrical stimulation. Photomed Laser Surg 2008;26:197–202. 10.1089/pho.2007.2125 [DOI] [PubMed] [Google Scholar]
- 27. Avni D, Levkovitz S, Maltz L, et al. . Protection of skeletal muscles from ischemic injury: low-level laser therapy increases antioxidant activity. Photomed Laser Surg 2005;23:273–7. 10.1089/pho.2005.23.273 [DOI] [PubMed] [Google Scholar]
- 28. Rizzi CF, Mauriz JL, Freitas Corrêa DS, et al. . Effects of low-level laser therapy (LLLT) on the nuclear factor (NF)-kappaB signaling pathway in traumatized muscle. Lasers Surg Med 2006;38:704–13. 10.1002/lsm.20371 [DOI] [PubMed] [Google Scholar]
- 29. Chow RT, Johnson MI, Lopes-Martins RAB, et al. . Efficacy of low-level laser therapy in the management of neck pain: a systematic review and meta-analysis of randomised placebo or active-treatment controlled trials. The Lancet 2009;374:1897–908. 10.1016/S0140-6736(09)61522-1 [DOI] [PubMed] [Google Scholar]
- 30. Glazov G, Yelland M, Emery J. Low-level laser therapy for chronic non-specific low back pain: a meta-analysis of randomised controlled trials. Acupunct Med 2016;34:328–41. 10.1136/acupmed-2015-011036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Qaseem A, Wilt TJ, McLean RM, et al. . Clinical Guidelines Committee of the American College of Physicians. Noninvasive Treatments for Acute, Subacute, and Chronic Low Back Pain: A Clinical Practice Guideline From the American College of Physicians. Ann Intern Med 2017;166:514–30. [DOI] [PubMed] [Google Scholar]
- 32. Ay S, Dogan SK, Evcik D. Is low-level laser therapy effective in acute or chronic low back pain? Clin Rheumatol 2010;29:905–10. 10.1007/s10067-010-1460-0 [DOI] [PubMed] [Google Scholar]
- 33. Airaksinen O, Brox JI, Cedraschi C, et al. . Chapter 4. European guidelines for the management of chronic nonspecific low back pain. Eur Spine J 2006;15:s192–s300. 10.1007/s00586-006-1072-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Magee DJ. Orthopedic physical assessment. 6 Edn Alberta, Canada: Elsevier, 2008:569–618. [Google Scholar]
- 35. Delitto A, George SZ, Van Dillen L, et al. . Low Back Pain. Clinical practice guidelines linked to the international classification of functioning, disability, and health from the orthopaedic section of the American Physical Therapy Association. J Orthop Sports Phys Ther 2012;42:A1–A57. [DOI] [PubMed] [Google Scholar]
- 36. Manchester MR, Glasgow GW, York JKM, et al. . The Back Book. Clinical guidelines for the management of acute low back pain. 2002:1–-28.
- 37. Van Tulder M, Becker A, Bekkering T, et al. . Chapter 3. European guidelines for the management of acute nonspecific low back pain in primary care. Eur Spine J 2006;15:s169–s191. 10.1007/s00586-006-1071-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Engers A, Jellema P, Wensing M, et al. . Individual patient education for low back pain. Cochrane Database Syst Rev 2008;23:CD004057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Garcia AN, Costa LC, Hancock MJ, et al. . Efficacy of the McKenzie method in patients with chronic nonspecific low back pain: a protocol of randomized placebo-controlled trial. Phys Ther 2015;95:267–73. 10.2522/ptj.20140208 [DOI] [PubMed] [Google Scholar]
- 40. Garcia AN, Hancock M, Costa LCM, et al. . Efficacy of the mechanical diagnosis and therapy in patients with chronic nonspecific low back pain: a randomized placebo controlled trial. 2017. Brit J Sports Med. In Press. [Google Scholar]
- 41. Grandinétti VS, Miranda EF, Johnson DS, et al. . The thermal impact of phototherapy with concurrent super-pulsed lasers and red and infrared LEDs on human skin. Lasers Med Sci 2015;30:1575–81. 10.1007/s10103-015-1755-0 [DOI] [PubMed] [Google Scholar]
- 42. Leal-Junior EC, Johnson DS, Saltmarche A, et al. . Adjunctive use of combination of super-pulsed laser and light-emitting diodes phototherapy on nonspecific knee pain: double-blinded randomized placebo-controlled trial. Lasers Med Sci 2014;29:1839–47. 10.1007/s10103-014-1592-6 [DOI] [PubMed] [Google Scholar]
- 43. Costa LO, Maher CG, Latimer J, et al. . Motor control exercise for chronic low back pain: a randomized placebo-controlled trial. Phys Ther 2009;89:1275–86. 10.2522/ptj.20090218 [DOI] [PubMed] [Google Scholar]
- 44. Kumar SP. Efficacy of segmental stabilization exercise for lumbar segmental instability in patients with mechanical low back pain: a randomized placebo controlled crossover study. N Am J Med Sci 2011;3:456–61. 10.4297/najms.2011.3456 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Ebadi S, Ansari NN, Naghdi S, et al. . The effect of continuous ultrasound on chronic non-specific low back pain: a single blind placebo-controlled randomized trial. BMC Musculoskelet Disord 2012;13:192 10.1186/1471-2474-13-192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Balthazard P, de Goumoens P, Rivier G, et al. . Manual therapy followed by specific active exercises versus a placebo followed by specific active exercises on the improvement of functional disability in patients with chronic non specific low back pain: a randomized controlled trial. BMC Musculoskelet Disord 2012;13:162 10.1186/1471-2474-13-162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Parreira PC, Costa LC, Takahashi R, et al. . Kinesio taping to generate skin convolutions is not better than sham taping for people with chronic non-specifc low back pain: a randomised trial. J Physiother 2014;60:90–6. 10.1016/j.jphys.2014.05.003 [DOI] [PubMed] [Google Scholar]
- 48. Luz Júnior MA, Sousa MV, Neves LA, et al. . Kinesio Taping® is not better than placebo in reducing pain and disability in patients with chronic non-specific low back pain: a randomized controlled trial. Braz J Phys Ther 2015;19:482–90. 10.1590/bjpt-rbf.2014.0128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Antonialli FC, De Marchi T, Tomazoni SS, et al. . Phototherapy in skeletal muscle performance and recovery after exercise: effect of combination of super-pulsed laser and light-emitting diodes. Lasers Med Sci 2014;29:1967–76. 10.1007/s10103-014-1611-7 [DOI] [PubMed] [Google Scholar]
- 50. Miranda EF, de Oliveira LV, Antonialli FC, et al. . Phototherapy with combination of super-pulsed laser and light-emitting diodes is beneficial in improvement of muscular performance (strength and muscular endurance), dyspnea, and fatigue sensation in patients with chronic obstructive pulmonary disease. Lasers Med Sci 2015;30:437–43. 10.1007/s10103-014-1690-5 [DOI] [PubMed] [Google Scholar]
- 51. Chow R, Armati P, Laakso EL, et al. . Inhibitory effects of laser irradiation on peripheral mammalian nerves and relevance to analgesic effects: a systematic review. Photomed Laser Surg 2011;29:365–81. 10.1089/pho.2010.2928 [DOI] [PubMed] [Google Scholar]
- 52. Huang YY, Sharma SK, Carroll J, et al. . Biphasic dose response in low level light therapy - an update. Dose Response 2011;9:602–618. 10.2203/dose-response.11-009.Hamblin [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Costa LO, Maher CG, Latimer J, et al. . Clinimetric testing of three self-report outcome measures for low back pain patients in Brazil: which one is the best? Spine 2008;33:2459–63. 10.1097/BRS.0b013e3181849dbe [DOI] [PubMed] [Google Scholar]
- 54. Nusbaum L, Natour J, Ferraz MB, et al. . Translation, adaptation and validation of the Roland-Morris questionnaire--Brazil Roland-Morris. Braz J Med Biol Res 2001;34:203–10. 10.1590/S0100-879X2001000200007 [DOI] [PubMed] [Google Scholar]
- 55. Costa LO, Maher CG, Latimer J, et al. . Psychometric characteristics of the Brazilian-Portuguese versions of the functional rating index and the Roland Morris disability questionnaire. Spine 2007;32:1902–7. 10.1097/BRS.0b013e31811eab33 [DOI] [PubMed] [Google Scholar]
- 56. Chatman AB, Hyams SP, Neel JM, et al. . The Patient-Specific Functional Scale: measurement properties in patients with knee dysfunction. Phys Ther 1997;77:820–9. 10.1093/ptj/77.8.820 [DOI] [PubMed] [Google Scholar]
- 57. Pengel LH, Refshauge KM, Maher CG. Responsiveness of pain, disability, and physical impairment outcomes in patients with low back pain. Spine 2004;29:879–83. 10.1097/00007632-200404150-00011 [DOI] [PubMed] [Google Scholar]
- 58. Elkins MR, Moseley AM. Intention-to-treat analysis. J Physiother 2015;61:165–7. 10.1016/j.jphys.2015.05.013 [DOI] [PubMed] [Google Scholar]
- 59. Twisk JWR. Applied longitudinal data analysis for epidemiology: a practical guide, 2003:. ISBN: 0521819768. [Google Scholar]
- 60. Walker BF, Muller R, Grant WD. Low back pain in Australian adults: the economic burden. Asia Pac J Public Health 2003;15:79–87. 10.1177/101053950301500202 [DOI] [PubMed] [Google Scholar]
- 61. Tomazoni SS, Leal-Junior EC, Frigo L, et al. . Isolated and combined effects of photobiomodulation therapy, topical nonsteroidal anti-inflammatory drugs, and physical activity in the treatment of osteoarthritis induced by papain. J Biomed Opt 2016;21:108001 10.1117/1.JBO.21.10.108001 [DOI] [PubMed] [Google Scholar]
- 62. Tomazoni SS, Leal-Junior EC, Pallotta RC, et al. . Effects of photobiomodulation therapy, pharmacological therapy, and physical exercise as single and/or combined treatment on the inflammatory response induced by experimental osteoarthritis. Lasers Med Sci 2017;32:101–8. 10.1007/s10103-016-2091-8 [DOI] [PubMed] [Google Scholar]
- 63. World Association for Laser Therapy - WALT (2010): Dosage recommendations Recommended treatment doses for low level laser therapy. http://www.walt.nu/dosage-recommendations.html (accessed 30 May 2017).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2017-017202supp001.pdf (71.5KB, pdf)