Abstract
Mucoepidermoid carcinoma (MEC) is the most common malignant tumour of the major and minor salivary glands. Minor salivary glands are scattered in different areas of the oral cavity such as palate, retromolar area, floor of the mouth, buccal mucosa, lips and tongue, but so far, only a few lingual MEC cases have been documented in the literature and most of the studies have shown a predilection for base and dorsum of the tongue. We report a rare case of MEC involving the posterior-lateral border of the tongue.
Keywords: head and nNeck cancer, pathology
Background
Salivary gland malignancies are rare neoplasms and account for only 5% of all head and neck malignancies.1 Mucoepidermoid carcinoma (MEC) is the most common malignant salivary gland tumour representing 35% of malignant tumours from major and minor salivary glands.2 It is most common in the parotid gland and the minor salivary glands constitute the second most common site with a site predilection for palate followed by buccal mucosa. MEC of tongue is quite rare and only less than 30 cases have been documented so far.1 3 We report a rare presentation of MEC in the posterior-lateral border of the tongue and discuss the potential risk of inadequate management of such lesion as it may often be misdiagnosed as foliate papillitis.
Case presentation
A 45-year-old woman came to us complaining of swelling with intermittent pain on the left side of the tongue that had afflicted her for 2 years. It started as a small lesion and grew gradually to reach the current size. She had a history of thyroid cancer, which was removed 15 years ago. The patient was moderately built and nourished and there was no pallor, icterus, cyanosis or clubbing. There was no generalised lymphadenopathy. Intraoral examination revealed an ovoid well-circumscribed lesion measuring 2×2 cm on the posterior-lateral border of the left side of the tongue (figure 1). The overlying mucosa was erythematous and the surface was smooth. The lesion was tender on palpation and hard in consistency.
Figure 1.

An ovoid well-circumscribed swelling, measuring 2×2 cm on the posterior left lateral border of tongue.
Differential diagnosis
Foliate papillitis
Traumatic fibroma
Benign vascular/neural tumours
Metastatic thyroid cancer.
Treatment and follow-up
Excisional biopsy of the lesion was done and histopathological examination of the tissue sections showed numerous cystic spaces lined by epithelial cells and islands and sheets of epidermoid cells in the connective tissue (figure 2). The neoplasm consisted of three populations of cells: the epidermoid, and the intermediate and mucous cells. The epidermoid cells and the intermediate cells showed vesicular nuclei, prominent nucleoli, nuclear pleomorphism and increased mitosis (figure 3). The epithelial cells lining the cystic spaces and forming the solid islands were interspersed by Per iodic acid Schiff (PAS) -positive mucous cells (figure 4). Based on these features, the lesion was diagnosed as low-grade MEC. The excretory duct opening into the oral mucosa also was lined by neoplastic cells showing cellular atypia and mucous cells (figure 5). However, the tumour margins were free of neoplastic cells.
Figure 2.
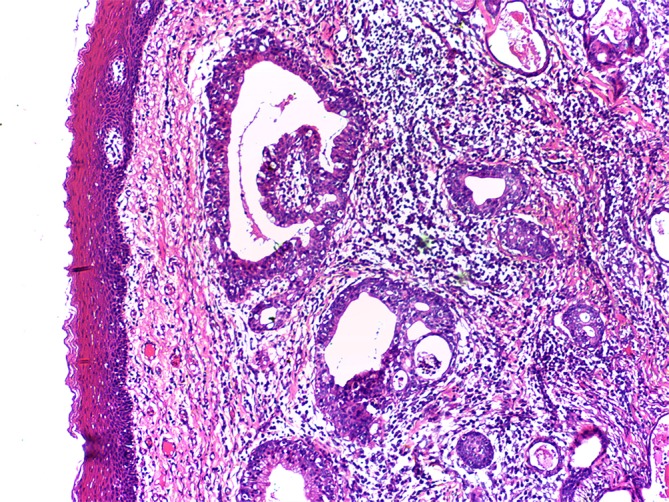
Histopathological examination of the tissue sections showing numerous cystic spaces lined by epithelial cells and solid epithelial islands in a fibrous connective tissue stroma (H&E, 10×).
Figure 3.
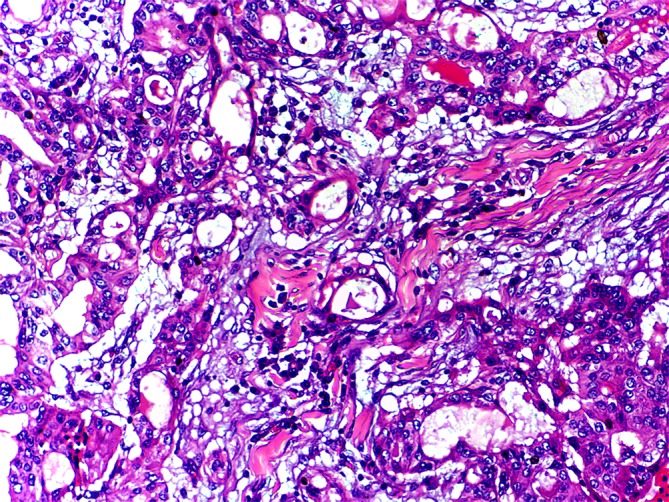
The epidermoid cells and the intermediate cells showing vesicular nuclei, prominent nucleoli, nuclear pleomorphism and increased mitosis (H&E, 20×).
Figure 4.
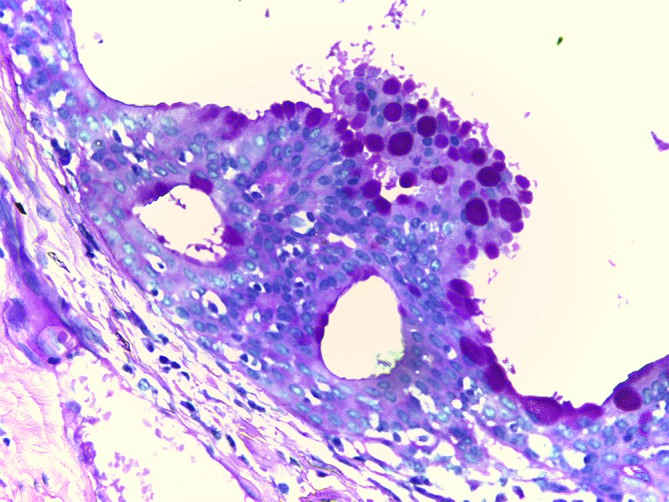
The epithelial cells lining the cystic spaces (stained blue) interspersed by PAS-positive mucous cells (stained magenta) (H&E, 40×).
Figure 5.
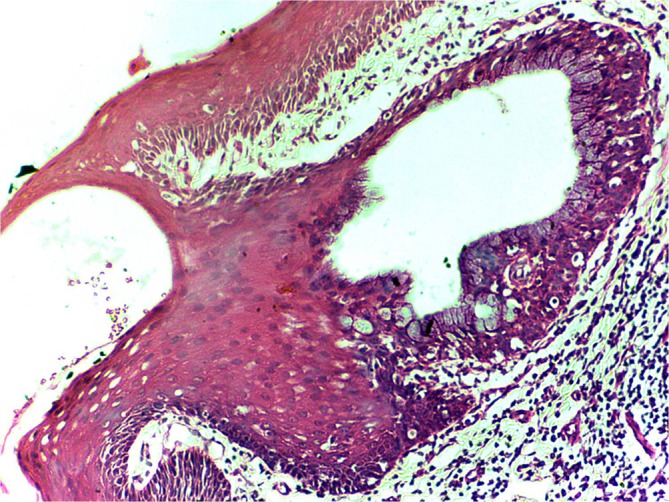
The excretory duct opening into the oral mucosa, lined by neoplastic epithelial cells showing cellular atypia and mucous cells suggestive of the origin of the neoplasm from the excretory duct (H&E, 20×).
Outcome and follow-up
Following surgical excision, the healing was uneventful and a regular follow-up of the patient for a period of 3 years did not reveal any evidence of recurrence.
Discussion
MEC was first described by Volkman in 1895, which was further elaborated on by Stewart in 1945 as mucoepidermoid tumour4 due to its highly variable biological behaviour. Later, the term ‘mucoepidermoid tumour’ was replaced by ‘mucoepidermoid carcinoma’, a more preferred designation, as it was recognised that even low-grade tumours could occasionally exhibit malignant behaviour.
MEC is the most common salivary gland malignancy with the second highest frequency of occurrence among all salivary gland tumours. Though it shows a predilection for parotid gland with 45% of the cases occurring at this site,5 it is the most common malignancy involving the minor salivary glands. Minor salivary glands are distributed throughout the oral mucosa, except in the anterior region of the hard palate and the gingiva. The minor salivary gland tumours account for 14%–22%6 of all salivary gland carcinomas with MEC being the most common type of intraoral adenocarcinoma,7 showing predilection for the palate (35.5%) followed by buccal mucosa (14%).8 Its occurrence in other intraoral sites, including tongue, are extremely rare and a PubMed search of related English-language literature revealed only 16 case reports of lingual MEC (table 1). Though lingual MEC can occur at any of the sites where salivary gland tissue is normally distributed, most cases are seen in the tongue’s base, representing more than 50% of all tumours.2 The review of previously reported cases showed that most of them developing in the base and dorsum of the tongue were, in fact, located in the tongue’s midline. Different from that, the present case occurred in the posterior-lateral border of the tongue, anterior to the circumvallate papillae, so it can be considered the first case published in the literature out there. Importantly, as this site mainly comprised foliate papilla, MEC may be mistakenly diagnosed as foliate papillitis, thus being ignored in the early stages of its development by the clinicians. Since our patient had a history of thyroid carcinoma, and as metastatic thyroid carcinoma was considered as a possible diagnosis in this case, we went ahead with excisional biopsy. As with most documented cases of lingual MECs, microscopically, the present case also showed features of low-grade mucoepidermoid carcinoma.
Table 1.
Summary of the reported cases of mucoepidermoid carcinoma of tongue
| Serial No | Authors | Gender | Site | Tumour grade |
| 1 | Heidelberger and Batsakis17 | F | Base of the tongue | High grade |
| 2 | Adkins and Putney18 | M | Base of the tongue | Low/intermediate |
| 3 | Pickell19 | M | Base of the tongue | Low grade |
| 4 | Pfendler20 | F | Base of the tongue | Low grade |
| 5 | Varghese et al21 | M | Base of the tongue | Low grade |
| 6 | Pires et al22 | F | Oral tongue (right anterior border) | Low grade |
| 7 | Andrews and Eveson23 | M | Base of the tongue | High grade |
| 8 | Leong et al3 | M | Base of the tongue | High grade |
| 9 | Liu et al24 | F | Base of the tongue | High grade |
| 10 | Sobani et al25 | M | Base of the tongue | Low grade |
| 11 | Martellucci et al26 | F | Base of the tongue | Low grade |
| 12 | Kalogirou et al7 | M | Posterior dorsal tongue | Low grade |
| 13 | Mesolella et al2 | F | Base of the tongue | Low grade |
| 14 | Bollig et al27 | F | Base of the tongue | Intermediate |
| 15 | Su et al28 | M | Base of the tongue | Low grade |
| 16 | Rubin et al29 | F | Base of the tongue | Low grade |
F, female; M, male.
MEC is thought to arise from pluripotent reserve cell of excretory duct9–11 from the salivary gland that potentially can differentiate into squamous, columnar, mucous and clear cells. In the case presented here, MEC’s tumour cells were also evident in the corresponding excretory duct opening into the superficial oral epithelium, suggestive of its origin from the excretory duct. The tumourigenesis of MEC is not clearly understood. The translocation of gene material, t(11;19) (q21;p13.1), has been identified as a solitary abnormality in some cases of MEC.12 The occurrence of MEC, among the survivors of the Hiroshima and Nagasaki atomic bomb explosions,13 and in patients after radiation therapy for thyroid carcinoma or leukaemia14 confirms the aetiological role of ionising radiation in MEC. Recently, the presence of transcriptionally active human papillomavirus (HPV) 16/18 was demonstrated in MEC, implicating high-risk HPV in its pathogenesis.15
MEC is a unique malignancy since it demonstrates a broad spectrum of aggressiveness ranging from an indolent tumour, which is cured by surgery, to aggressive neoplasm, which is prone to local invasion, recurrence and metastasis.16 Tumour location, clinical stage, tumour grade and adequacy of treatment are the main prognostic factors for MEC-affected patients. The treatment is usually surgical excision with free margins, and neck dissection is indicated in the presence of lymph node metastases or those classified as grade III.
Learning points.
Mucoepidermoid carcinomas (MECs) are rare salivary gland neoplasms showing varied biological behaviour.
Due to its typical location, MEC occurring in the posterior-lateral border of the tongue may often be misdiagnosed as foliate papillitis.
As minor salivary glands are widely distributed in the oral mucosa, MEC can occur in any locations inside the mouth; hence, it is essential that it should be considered as a differential diagnosis for all intraoral soft tissue swellings.
Footnotes
Contributors: All authors were responsible for the concept and design; definition of intellectual content; drafting/revision of intellectual content; data acquisition, analysis and interpretation; final approval of version published; agreement to be accountable for the article.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Qureshi SM, Janjua OS, Carcinoma M. A clinico-pathological review of 75 cases. International Journal of Oral & Maxillofacial Pathology 2012;3:05–9. [Google Scholar]
- 2.Mesolella M, Iengo M, Testa D, et al. Mucoepidermoid carcinoma of the base of tongue. Acta Otorhinolaryngol Ital 2015;35:58–61. [PMC free article] [PubMed] [Google Scholar]
- 3.Leong SC, Pinder E, Sasae R, et al. Mucoepidermoid carcinoma of the tongue. Singapore Med J 2007;48:272–4. [PubMed] [Google Scholar]
- 4.Ranganath MK, Matmari V, Narayanaswamy UD, et al. Mucoepidermoid carcinoma presenting as a retromolar mucocele. Ann Maxillofac Surg 2011;1:66–9. 10.4103/2231-0746.83161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ozawa H, Tomita T, Sakamoto K, et al. Mucoepidermoid carcinoma of the head and neck: clinical analysis of 43 patients. Jpn J Clin Oncol 2008;38:414–8. 10.1093/jjco/hyn045 [DOI] [PubMed] [Google Scholar]
- 6.Bansal AK, Bindal R, Kapoor C, et al. Current concepts in diagnosis of unusual salivary gland tumors. Dent Res J 2012;9(Suppl 1):S9–S19. [PMC free article] [PubMed] [Google Scholar]
- 7.Kalogirou EM, Tosios KI, Petsinis V, et al. An asymptomatic tumor on the dorsal tongue. Oral Surg Oral Med Oral Pathol Oral Radiol 2014;117:659–62. 10.1016/j.oooo.2013.10.004 [DOI] [PubMed] [Google Scholar]
- 8.Pires FR, Pringle GA, de Almeida OP, et al. Intra-oral minor salivary gland tumors: a clinicopathological study of 546 cases. Oral Oncol 2007;43:463–70. 10.1016/j.oraloncology.2006.04.008 [DOI] [PubMed] [Google Scholar]
- 9.Smitha K, Thoma S, et al. Mucoepidermoid carcinoma of the anteriormaxilla: a rare entity. Archives of Medicine and Health Sciences 2014;2:64–6. [Google Scholar]
- 10.Phasha Z, Sharma K,et al. Mucoepidermoid carcinoma of palate mimicking vascular lesion: a case report. Journal of Dental Sciences and Research 2013;4:9–12. [Google Scholar]
- 11.Jarde SJ, Das S, Narayanswamy SA, et al. Mucoepidermoid carcinoma of the palate: a rare case report. J Indian Soc Periodontol 2016;20:203–6. 10.4103/0972-124X.170828 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.El-Naggar AK, Lovell M, Killary AM, et al. A mucoepidermoid carcinoma of minor salivary gland with t(11;19)(q21;p13.1) as the only karyotypic abnormality. Cancer Genet Cytogenet 1996;87:29–33. 10.1016/0165-4608(95)00266-9 [DOI] [PubMed] [Google Scholar]
- 13.Saku T, Hayashi Y, Takahara O, et al. Salivary gland tumors among atomic bomb survivors, 1950-1987. Cancer 1997;79:1465–75. [DOI] [PubMed] [Google Scholar]
- 14.Whatley WS, Thompson JW, Rao B. Salivary gland tumors in survivors of childhood cancer. Otolaryngol Head Neck Surg 2006;134:385–8. 10.1016/j.otohns.2005.10.022 [DOI] [PubMed] [Google Scholar]
- 15.Isayeva T, Said-Al-Naief N, Ren Z, et al. Salivary mucoepidermoid carcinoma: demonstration of transcriptionally active human papillomavirus 16/18. Head Neck Pathol 2013;7:135–48. 10.1007/s12105-012-0411-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Purohit J, Desai V, Sharma R, et al. Mucoepidermoid carcinoma of parotid gland: a case report. Saudi Journal of Oral Sciences 2015;2:106–9. 10.4103/1658-6816.160781 [DOI] [Google Scholar]
- 17.Heidelberger KP, Batsakis JG. Mucoepidermoid carcinoma of the tongue. J Laryngol Otol 1973;87:1239–42. 10.1017/S0022215100078233 [DOI] [PubMed] [Google Scholar]
- 18.Adkins WY, Putney FJ. Mucoepidermoid carcinoma of the tongue. Trans Sect Otolaryngol Am Acad Ophthalmol Otolaryngol 1975;80:465–7. [PubMed] [Google Scholar]
- 19.Pickell G. Chronic glossopharyngeal neuralgic pain associated with mucoepidermoid carcinoma. CMAJ 1985;133:579–80. [PMC free article] [PubMed] [Google Scholar]
- 20.Pfendler DF. Glossopharyngeal neuralgia with tongue carcinoma. Arch Otolaryngol Head Neck Surg 1997;123:658 10.1001/archotol.1997.01900060110020 [DOI] [PubMed] [Google Scholar]
- 21.Varghese BT, Jacob MM, Madhavan J, et al. Late scar recurrence in mucoepidermoid carcinoma of base of tongue. J Laryngol Otol 2000;114:299–301. 10.1258/0022215001905409 [DOI] [PubMed] [Google Scholar]
- 22.Pires FR, Alves FA, de Almeida OP, et al. Synchronous mucoepidermoid carcinoma of tongue and pleomorphic adenoma of submandibular gland. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2003;95:328–31. 10.1067/moe.2003.7 [DOI] [PubMed] [Google Scholar]
- 23.Andrews KV, Eveson JW. Myokymia (fasciculation) of the tongue as a unique presentation of mucoepidermoid carcinoma. Int J Oral Maxillofac Surg 2007;36:79–81. 10.1016/j.ijom.2006.05.004 [DOI] [PubMed] [Google Scholar]
- 24.Liu W, Gnepp DR, de Vries E, et al. Mucoepidermoid carcinoma arising in a background of sialadenoma papilliferum: a case report. Head Neck Pathol 2009;3:59–62. 10.1007/s12105-009-0106-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sobani ZU, Junaid M, Ghaffar S, et al. Mucoepidermoid carcinoma of the base of tongue. J Pak Med Assoc 2011;61:945–7. [PubMed] [Google Scholar]
- 26.Martellucci S, Pagliuca G, de Vincentiis M, et al. Mucoepidermoid carcinoma of the tongue base mimicking an ectopic thyroid. Case Rep Otolaryngol 2013;2013:1–3. 10.1155/2013/925630 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bollig C, Huang LC, Abi-Hachem R, et al. Base of tongue mass. Mucoepidermoid carcinoma. JAMA Otolaryngol Head Neck Surg 2015;141:935–6. 10.1001/jamaoto.2015.1727 [DOI] [PubMed] [Google Scholar]
- 28.Su R, Fortson JK, Patel VG, et al. Mucoepidermoid carcinoma of the lingual tonsil. Am Surg 2016;82:269–70. [PubMed] [Google Scholar]
- 29.Rubin A, Davis J, Jreije K, et al. Case report: recurrent mucoepidermoid carcinoma of the tongue in adult female patient with lung cancer. Clin Med Insights Ear Nose Throat 2017;10:117955061772046 10.1177/1179550617720462 [DOI] [PMC free article] [PubMed] [Google Scholar]


